Abstract
A common recommendation for youth treated for substance abuse is to attend 12-step groups. However, little is known regarding the effects of this adult-derived prescription on substance use outcomes for teens. This study examined (a) the relation between 12-step attendance and substance use outcome in the 6 months postdischarge from inpatient care and (b) a process model of how 12-step attendance during the first 3 months postdischarge affects proximal outcomes of motivation, coping, and self-efficacy, measured at 3 months, and how these, in tum, affect ultimate substance use outcome in the following 3 months. Adolescent inpatients (N = 99) were assessed during treatment and 3 and 6 months postdischarge. Results revealed modest beneficial effects of 12-step attendance, which were mediated by motivation but not by coping or self-efficacy. Findings suggest that closer attention be paid to motivational factors in the treatment of adolescent substance abuse.
It is estimated that more than 1 million individuals enter treatment for substance use problems each year in the United States (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 1993). The majority of these facilities use a 12-step1 or “Minnesota” model (McElrath, 1997). According to a national study by Roman and Blum (1998) on a representative sample of 450 private substance abuse treatment centers, 90% of the facilities based their treatment on the 12-step principles of Alcoholics Anonymous and variations of this model, with nearly one half of the remaining 10% incorporating 12-step model principles in combination with other approaches, including encouraged attendance at 12-step meetings. Furthermore, a survey carded out on substance use disorder treatment programs in the U.S. Veterans Administration system (Humphreys, 1997) indicated that the majority of patients (79.4%) were referred to AA postdischarge.
Although studies have supported the utility of the 12-step approach with adults (N. S. Miller, Ninonuevo, Klamen, & Hoffmann, 1997; Montgomery, Miller, & Tonigan, 1995; Moos, Finney, Ouimette, & Suchinsky, 1999; Morgenstern, Labouvie, McCrady, & Kahler, 1997; Project MATCH Research Group, 1997a, 1997b, 1998), comparatively little is known regarding the applicability of this treatment modality for adolescents, and even less is known regarding the use and effectiveness of 12-step groups for adolescents after treatment despite it being a commonplace recommendation (Bukstein, 1995). Swadi (1992) pointed out that developmentally specific physical and psychological attributes as well as unique environmental challenges may mean that adolescents differ from adults in the extent to which treatment approaches are able to engage them and be effective for them. Indeed, prior research has revealed that adolescents in treatment for substance use disorders differ in both qualitative and quantitative aspects of substance use behavior and consequences compared to adults as well as being a more heterogeneous group (Brown, 1993; Brown, Mott, & Myers, 1990; Tarter, Kirisci, Hegedus, Mezzich, & Vanyukov, 1994).
Investigations of substance use topography reveal that teenagers in treatment have used substances less frequently, display fewer dependence symptoms, use multiple substances concurrently, and have fewer medical complications and withdrawal symptoms than adults (e.g., Brown, 1993; Stewart & Brown, 1995). In fact, one of the criticisms of the 12-step, disease model approach for use with adolescent substance abusers has been the emphasis on the primary causative role of the substance(s) of abuse in the clinical presentation when, more typically, the substance abuse constitutes only one part of a more complicated problem behavior pattern. Adolescents entering treatment have also been found to differ from adults in their motivation to cease alcohol and drug use, because adolescents rarely enter substance abuse treatment because of an intrinsic desire to stop substance use. Instead, youth motivation could be conceived as being more extrinsic in that adolescents are usually coerced into treatment, to a lesser or greater degree, because of a variety of school, legal, or familial-interpersonal problems (Brown, Vik, & Creamer, 1989). Adolescents also face logistical barriers not encountered by adults following treatment. Most adults have the independent financial resources and available transportation to access aftercare or 12-step groups whenever and wherever they choose, whereas adolescents are more often dependent on parents for money and transportation. Furthermore, even if teens are willing and able to attend 12-step groups, the adult composition of most groups may provide a barrier to affiliation and continued attendance. A study by Kelly and Myers (1997) revealed that teens who did attend groups consisting of at least a substantial proportion of teenagers had significantly better substance use outcomes at 3 months posttreatment than those who attended predominantly adult meetings.
Despite these developmentally specific differences, the majority of treatment approaches for teens with substance abuse problems have been an extrapolation of the traditional adult model with a largely unexamined behavioral prescription of attendance at 12-step meetings. This problem is not unique to the field of substance use disorder treatment. As Garber (1984) stated, conceptualizations of psychopathology have historically been based on adult models, and thus the study of children's mental health has merely been an unjustified extension of the adult model. The treatment of adolescents as “miniature adults” is viewed as not acceptable unless empirical validation reveals it is justifiable to do so. However, a review of quantitative research on AA conducted by Emrick, Tonigan, Montgomery, and Little (1993) did not find a single study examining use of AA by individuals under 21 years of age. Furthermore, very few studies have been published since the early 1990s in this area. A study by Alford, Koehler, and Leonard (1991) revealed that posttreatment AA/NA attendance was significantly related to improved social-civil productivity and abstinence at 2-year follow-up. Also, several adolescent samples studied by Brown and colleagues (e.g., Brown, 1993; Brown et al., 1990; Vik, Grizzle, & Brown, 1992) found that 12-step group attendance was associated with more favorable outcomes at 1-year follow-up. A study by Hsieh, Hoffman, and Hollister (1998) found that in a multisite sample of 2,317 adolescents who received inpatient treatment for substance abuse problems, 12-step meeting attendance was the most powerful discriminator of abstinence from substances at 6 and 12 months posttreatment. However, given that approximately 125,000 youth enter substance abuse treatment annually (NIAAA & National Institute on Drug Abuse, 1995), more studies are needed to assess the impact of adolescent 12-step group attendance on relapse.
The most prominent and well-explicated adult model of relapse to date is the cognitive–behavioral model of Marlatt and Gordon (1985). This model emphasizes important constructs from Bandura's social–cognitive learning theory (Bandura, 1986), such as “self-efficacy” and “coping responses,” which are posited as crucial mediators in the capacity to resist using substances in a situation in which one is at high risk for relapse. A major assumption of this model is that an individual is motivated to abstain (or sustain controlled moderate use) from the use of psychoactive substances. An individual's motivation for abstinence is postulated to subsequently influence coping efforts and necessarily forms an integral part of the model. Marlatt and Gordon's model predicts that the greater an individual's commitment to abstinence, self-efficacy, and coping skills in the face of high-risk situations the more likely that individual will be to resist resumption of substance use.
Clinical recommendations to attend 12-step groups are derived from anecdotal and empirical observations that such attendance leads to improved substance use outcomes, but mechanisms through which such salutary effects are exerted for youth are not yet clear. Morgenstern et al. (1997) examined the effects of AA affiliation following inpatient 12-step treatment in an adult sample and found that attendance was related to better outcomes, which were mediated by the common change factors of cognitive and behavioral coping, measures of motivation, and self-efficacy. Of substantive theoretical and practical importance would be knowledge of how constructs such as those postulated within a social-cognitive formulation (i.e., motivation, coping, and self-efficacy) may influence, and be influenced by, 12-step attendance for adolescents and whether these effects can be used to help explain all or some of these observed relations. Prospective, multivariate, process-oriented research designs may help determine not just whether such treatment recommendations have the desired outcome effects but also help explain how or why these effects occur and for whom. Use of such models may serve to improve the specificity and efficiency of inpatient and aftercare recommendations for youth treated for substance use disorders.
The purpose of this study was twofold: first, to examine the relation between 12-step attendance and substance use in the first 6 months2 postdischarge from inpatient care, and second, to test a process model of how 12-step attendance during the first 3 months postdischarge affects proximal outcome measures of motivation for abstinence, abstinence-focused coping, and self-efficacy, measured at 3 months, and how these in turn affect ultimate substance use outcome (i.e., number of days abstinent) in the following 3 months. We predicted that more attendance at 12-step groups would be associated with the maintenance of abstinence or more abstinent days following inpatient treatment. We further predicted that this effect would be mediated by increases in abstinence-focused coping, self-efficacy, and motivation for abstinence.
Method
Setting and Sample
The current study is based on 99 adolescents recruited during inpatient treatment for substance abuse problems. These participants were drawn from a sample of 227 adolescents consecutively admitted to two private inpatient treatment programs in metropolitan San Diego, California. These treatment facilities are based broadly on a Minnesota model framework, which requires 12-step attendance during treatment and prescribes postdischarge attendance of community 12-step meetings. Some adolescents are also recommended to attend aftercare sessions at the treatment facility for support, encouragement, and psychoeducation. The average duration of inpatient treatment for this sample was 12.5 days (SD = 9.07).
Adolescents were recruited into the study if they met criteria for a psychoactive substance abuse or dependence diagnosis in accordance with the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 1994). Diagnoses were determined by structured interview using the Customary Drinking and Drug Use Record (CDDR; Brown, Myers, Lippke, Stewart, Tapert, & Vik, 1998). Other eligibility criteria were (a) the participation of a resource person who could provide corroborative information; (b) adequate ability to understand and comprehend the measures, (c) lived within 50 miles of the research facility; (d) no history of psychotic symptoms, independent of substance use; and (e) between the ages of 14 and 18.
Because opportunities for substance use are severely limited in restrictive settings such as residential treatment centers or juvenile hall/jail, participants who had spent the majority of the follow-up period in such settings (n = 20) were excluded from analyses. Of the remainder, 26 participants withdrew, and 19 individuals were unable to be contacted, leaving a total of 165. A further 25 cases were excluded because of missing data on one of the intake measures, and another 41 were excluded because they were missing measures at the 3- or 6-month follow-up, leaving a total of 99 participants. We conducted univariate analyses to examine any systematic baseline differences between included and excluded cases. The results revealed no significant differences on baseline measures of age, gender, ethnicity, number of days in inpatient treatment, number of days abstinent in the 30 days prior to treatment, substance use problem severity, motivation for abstinence, abstinence-focused coping, or self-efficacy (ps > .11). Examination of socioeconomic status revealed a trend for individuals of lower socioeconomic status to be in the excluded group (p = .07; see Table 1).
Table 1.
Comparison of Baseline Variables for Included (N = 99) and Excluded (N = 128) Cases
| Included cases |
Excluded cases |
|||
|---|---|---|---|---|
| Comparison dimension | M | SD | M | SD |
| Interval-scaled variables | ||||
| Age | 16.11 | 1.16 | 15.97 | 1.18 |
| Socioeconomic status* | 34.26 | 13.22 | 38.01 | 15.86 |
| Days in inpatient treatment | 12.52 | 9.07 | 12.93 | 11.16 |
| Abstinence-focused coping | 43.49 | 11.44 | 41.63 | 13.92 |
| Self-efficacy | 4.83 | 2.72 | 5.11 | 2.87 |
| Motivation for abstinence | 7.02 | 2.96 | 7.00 | 2.76 |
| Substance use problem severity | 61.67 | 15.79 | 62.42 | 18.04 |
| Days abstinent | 9.43 | 9.53 | 11.34 | 10.95 |
| Nominal-scaled variablesa | ||||
| Ethnicity | ||||
| White | 78 | 69 | ||
| Hispanic | 16 | 19 | ||
| Other | 6 | 12 | ||
| Gender | ||||
| Male | 40 | 45 | ||
| Female | 60 | 55 | ||
Note. Cell ns vary because of missing baseline data.
All of these values are percentages.
p < .10.
The average age of the sample was approximately 16 years (M = 16.11, SD= 1.16, range: 14–18), and just over half (60%) were female. Ethnic makeup was primarily Caucasian but consisted of a substantial proportion of Hispanics (78% Caucasian, 16% Hispanic, 4% African American, 2% Asian/Pacific Islander). Participants came from families of varying socioeconomic backgrounds, ranging from unskilled laborers to college-educated professionals (Hollingshead, 1965, socioeconomic status index: M = 34.26, SD = 13.22, range: 11–65). The sample was composed of polysubstance abusers, but the self-reported primary substances of choice were marijuana (43.6%), amphetamines (29.7%), alcohol (10.8%), hallucinogens (7.9%), opiates (4%), cocaine (2%), and inhalants (2%). The average number of days per month that participants used alcohol, other drugs, or both, in the 3 months prior to treatment entry were as follows: marijuana: M = 16.7, SD = 11.9; amphetamines: M = 7.8, SD = 10.7; beer: M = 7.1, SD = 9.1; liquor: M = 4.3, SD = 6.7; hallucinogens: M = 2.1, SD = 3.8; cocaine: M = 1.5, SD = 4.4; opiates: M = 1.1, SD = 4.5; and inhalants: M = 0.9, SD = 3.3.
Procedure
Participants were recruited during inpatient treatment if both parent and adolescent consented to the adolescent's participation. Initial interviews and baseline measures of substance involvement and common processes were completed during hospitalization by trained master's- and bachelor's-level interviewers. Corroborative resource-person interviews (usually parents) also were completed during treatment by a different interviewer so as not to bias independently obtained results. Information from the two sources was compared and combined through detailed discussions during weekly meetings with research personnel. This was done to resolve discrepant information and to arrive at the most accurate estimate of reported behaviors. This same format was used at the 3- and 6-month follow-up points. For the outcome measure (number of days abstinent) adolescent–parent discrepancies occurred in 2.5% of cases. This is consistent with previous studies (Myers et al., 1993; Myers, Brown, & Vik, 1998) showing that teens consistently self-report more substance use than parent collaterals. For 12-step attendance, adolescent reports were amended in 11% of cases. In the latter case we cannot specify the direction of discrepancies (i.e., whether parents underreported or teens overreported). Although parent reports replaced teen reports in only a minority of cases for both these variables, the value of collateral reports should not be discounted as they may serve to motivate better teen self-report and have been shown to provide valuable additional information in other domains, such as antisocial behavior (e.g., Brown, Gleghorn, Schuckit, Myers, & Mott, 1996). Also, to enhance reporting of substance use involvement during the follow-up period, saliva test strips (Alcostrip ™) were administered to detect recent use of alcohol, and urine samples for drug toxicology were obtained in cases where the adolescent denied any substance use during the follow-up period.
Measures
Demographics
Background information regarding age, ethnicity, and gender were recorded using the Structured Clinical Interview for Adolescents (Brown, 1987).
Substance involvement
Substance use frequency and quantity (alcohol only) was measured using the timeline follow-back (TLFB) procedure (Sobell & Sobell, 1992), adapted for multiple substances. Substance use problem severity was measured with the Personal Involvement scale of the Personal Experiences Inventory (Winters, Stinchfield, & Henly, 1993). This scale measures severity of substance involvement and has been shown to have excellent internal consistency as well as good construct and criterion validity for youth (Winters et al., 1993). Reliability analysis with the current sample also revealed a high internal consistency (Cronbach's α = .94).
Twelve-step attendance
Frequency of attendance at 12-step meetings was evaluated with the timeline follow-back technique. To enhance accurate recall of meeting attendance, interviewers used memory cues by reminding participants of the occurrence of significant events or holidays during the follow-up period and by inquiry into whether any significant or outstanding events had occurred in their own lives. This information was then entered onto the calendar to facilitate memory recall for the temporal topography of meeting attendance. Adolescent estimates were corroborated by a resource person using the same strategies and, where discrepancies occurred, the most conservative estimate was recorded.
Motivation for abstinence
Motivation was measured with two items taken from the Structured Clinical Interview for Adolescents (Brown, 1987). Participants gave ratings in response to the following questions: “On a scale of 1–10, how important is it for you not to use alcohol?”, and “On a scale of 1–10, how important is it for you not to use drugs?” (1 = not at all important and 10 = very important). Given that treatment goals were defined as abstinence from alcohol and other drugs, responses were averaged across both alcohol and drugs to provide a single index of motivation for abstinence.
Self-efficacy
Self-efficacy was measured with items taken from the Structured Clinical Interview for Adolescents (Brown, 1987). Two questions tapped this construct: “On a scale of 1–10, how likely is it that you will use alcohol again in the future?”, and “On a scale of 1–10, how likely is it that you will use drugs again in the future?” (1 = won't happen, 10 = happen for sure). Responses were averaged across both alcohol and drugs to provide a single index of self-efficacy. We conducted concurrent baseline correlational analyses with a validated measure of situation-specific self-efficacy: the Drug Taking Confidence Questionnaire (DTCQ; Sklar, Annis, & Turner, 1997). Results revealed a moderately strong relation, suggesting significant overlap with the full-scale score from this measure (r = .57). However, the DTCQ was developed to assess situation-specific self-efficacy for use of a particular substance of abuse, whereas the items used from the structured interview were global self-ratings about any substance use. This could have attenuated the magnitude of this relation.
Coping
Abstinence-focused coping with substance use temptations was assessed with the Adolescent Relapse Coping Questionnaire (Myers & Brown, 1995). This scale measures coping responses to a hypothetical, commonly reported substance use situation (i.e., at a party with other people, the adolescent is offered drugs and something to drink). It has been shown to have good internal consistency (Cronbach's α = .82) as well as construct and criterion validity (Myers & Brown, 1995).
Results
Preliminary Analyses
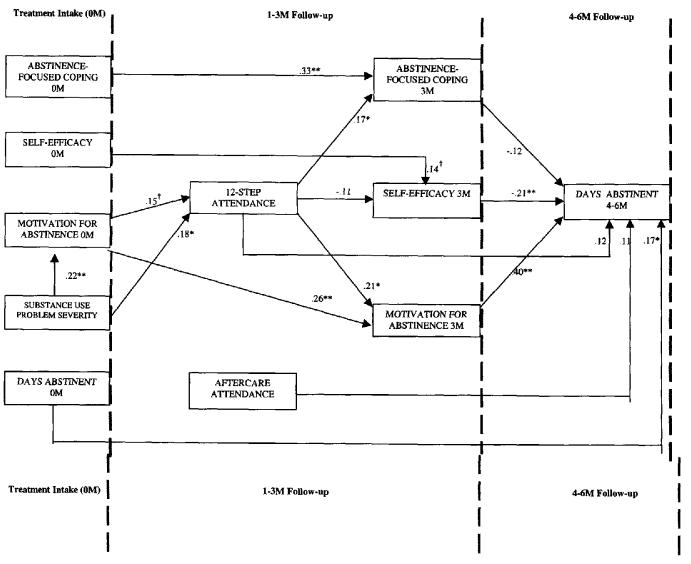
Variables were initially examined with regard to their distributional qualities in order to detect possible violations of statistical assumptions for the covariance structure model seen in Figure 1. Only one variable had an undesirably large skew ( > 1.5: number of aftercare meetings attended during the first 3 months). This was subsequently transformed (square root), dramatically reducing skewness and kurtosis. Analyses were carried out separately with the transformed and untransformed variable. The differences in magnitude of the relations between variables were small and did not alter the pattern of findings. Because of this, and inherent difficulties in interpreting results from transformed variables, results for the untransformed variables are reported and discussed herein.
Figure 1.
Path diagram depicting standardized coefficients of mediational relationships (with control variables). N = 99. M = months, †p < .10. *p < .05. **p < .01.
To control for the relation between other variables and substance use outcome, we conducted initial univariate analyses on (a) demographics (age, gender, ethnicity), (b) substance use variables (baseline substance use problem severity, frequency of baseline substance use), (c) treatment experience variables (number of days in inpatient treatment; aftercare meetings attended), and (d) intake measures of the hypothesized mediators (abstinence-focused coping, self-efficacy, and motivation for abstinence). None of the demographic variables (ps > .16), intake measures of hypothesized mediators (ps > .08), or number of days in treatment (p = .17) were related to substance use outcome. Of the substance use variables, substance use problem severity was not related to outcome (p = .32), whereas baseline frequency of substance use was modestly associated with outcome (r = .24, p = .02) and was thus retained as a control variable. Although aftercare meeting attendance only reached a significant trend (p = .06) it was nevertheless retained as a control variable because it contributed uniquely to outcome when controlling levels of baseline use (sr = .21, p = .04) and would provide a more stringent test of the proposed model.
During the first 3 months nearly one third (31%) of the participants reported complete abstinence from alcohol and other drugs, but the sample as a whole was abstinent on average on 87% of days. By the 6-month follow-up point approximately the same proportion (30.3%) reported complete abstinence, with the sample as a whole abstinent on 77% of days during the second 3-month period. Thus, although complete abstinence from alcohol and other drugs was achieved by only a minority of participants, a dramatic reduction in substance involvement occurred during the 6-month follow-up period, with participants abstinent on almost 82% of days on average (adolescents were abstinent on 32% days at intake).
Baseline Predictors of 12-Step Attendance
To begin to examine the factors that influence, and are influenced by, adolescent 12-step attendance, we analyzed baseline levels of the mediator variables, substance use problem severity, frequency of substance use at intake, and gender in regard to their relation with attendance at such groups. The analyses revealed one statistically significant baseline predictor: substance use problem severity (r = .29, p = .004), with motivation for abstinence producing a statistical trend (r = .19, p = .06). Problem severity was also related to motivation (r = .29, p = .004). These variables were incorporated into the process model illustrated in Figure 1.
Adolescent 12-Step Attendance
The current sample of adolescents attended meetings on average between two and three times per week during the first 3 months post-discharge (M = 29.2, SD = 31.9, range: 0–90); just over one fourth (25.3%) did not attend any 12-step meetings. The average attendance dropped considerably during the second 3-month period (M = 16.9, SD = 25.9, range: 0–90) with 41% of the sample not attending any 12-step meetings. Bivariate analysis of concurrent 12-step attendance and substance use outcome in the first 3 months and the second 3 months postdischarge revealed small to moderate effects (r = .32, p = .001, and r = .29, p = .003, respectively). Examination of the relation between 12-step attendance and rates of abstinence revealed that abstainers attended approximately twice as many 12-step meetings (M = 43.74, SD = 34.04), on average, during the first 3 months, as substance users did (M = 22.53, SD = 28.82), F(1, 98) = 10.28,p = .002; η2 = .10. This also held true for the 4- to 6-month follow-up period (M = 27.50, SD = 30.07, vs. M = 12.18, SD = 22.14, respectively), F(1, 98) = 7.78, p = .006; η2 = .08. A simultaneous multiple regression revealed that, after partialing out the effects of after-care attendance and number of days abstinent at baseline, 12-step meeting attendance in the first 3 months still contributed uniquely to both substance use outcome variance in the first 3 months (β = .28, p = .007) and the second 3 months postdischarge (β = .23, p = .03).
Test of the Mediational Model
To test the effects of the hypothesized mediating variables in the relation between 12-step attendance and ultimate substance use, we estimated outcome structural equations using EQS (Bentler & Wu, 1995). EQS provides both parameter estimates (βs) and a z test of the total mediated (indirect) effects. The intercorrelations between variables along with means and standard deviations of all variables are shown in Table 2.
Table 2.
Means, Standard Deviations, and Zero-Order Pearson Product–Moment Correlations of Analysis Variables
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Efficacy 0 m | 4.9 | 2.7 | — | ||||||||||||
| 2. Efficacy 3 m | 4.8 | 3.3 | .15 | — | |||||||||||
| 3. Motivation 0 m | 7.0 | 2.9 | −.37** | −.13 | — | ||||||||||
| 4. Motivation 3 m | 7.3 | 3.3 | −.27** | −.61** | .30** | — | |||||||||
| 5. Coping 0 m | 43.7 | 11.5 | −.38** | −.16 | .59** | .19 | — | ||||||||
| 6. Coping 3 m | 36.8 | 17.2 | −.31** | −.33** | .18 | .47** | .34** | — | |||||||
| 7. Substance use severity | 62.2 | 15.8 | −.07 | .05 | .29** | .16 | .33** | .23* | — | ||||||
| 8. Days abstinent 0 m | 9.6 | 9.6 | .08 | −.12 | .10 | .12 | .08 | −.03 | −.33** | — | |||||
| 9. 12-step 1–3 m | 29.2 | 31.9 | −.08 | −.12 | .19 | .26** | .05 | .18 | .29** | −.12 | — | ||||
| 10. 12-step 4–6 m | 16.9 | 25.9 | −.19 | −.26* | .19 | .34** | .13 | .37** | .26** | −.08 | .66** | — | |||
| 11. Aftercare 1–3 m | 9.3 | 12.9 | −.11 | −.02 | .07 | .19 | .11 | .22* | .23* | −.05 | .36** | .21* | — | ||
| 12. Days abstinent 1–3 m | 78.3 | 19.2 | −.06 | −.38** | .18 | .52** | .16 | .23* | −.02 | .15 | .32** | .27** | .26** | — | |
| 13. Days abstinent 4–6 m | 69.5 | 29.3 | −.08 | −.44** | .14 | .52** | .18 | .17 | −.10 | .24* | .24* | .29** | .19 | .64** | — |
Note. m = months.
p < .05, two-tailed.
p < .01, two-tailed.
Initially, the hypothesized relations were estimated and tested. Figure 1 depicts the variables that predicted 12-step attendance in the first 3 months posttreatment and the mechanisms through which attendance at 12-step meetings is hypothesized to exert its effects on ultimate substance use outcomes in the following 3 months. Baseline levels of the hypothesized mediators and other control variables (days abstinent at baseline, aftercare meeting attendance) are also shown.
The exogenous variable, substance use problem severity, had direct effects on 12-step attendance (β = . 18, p = .03) and motivation for abstinence (β = .22, p = .0l). The effect of motivation for abstinence at baseline on postdischarge 12-step attendance approached statistical significance (β = . 15, p = .06). The z test of the indirect effect of substance use problem severity, through motivation, revealed a statistical trend (z = 1.26, p = .10), suggesting that motivation for abstinence is a partial mediator of substance use problem severity and postdischarge attendance at 12-step meetings. Motivation and problem severity explained approximately 10% (8% adjusted [adj]) of the variance in 12-step attendance (R2 adj = .08), F(2, 96) = 5.09, p = .008.
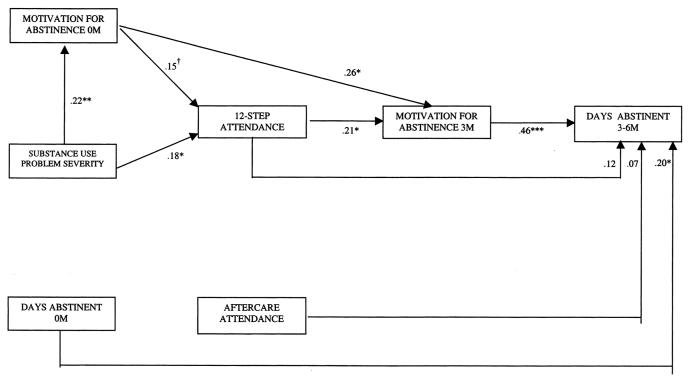
Abstinence-focused coping, self-efficacy, 3 and motivation for abstinence (measured at 3 months) together significantly mediated the relation between 12-step attendance during the first 3 months and substance use outcome in the second 3 months postdischarge (z = 1.70, p = .04). Figure 1 shows the standardized path coefficients and associated significance levels. The set of explanatory variables affecting substance use during Months 4–6 postdischarge, shown in Figure 1, accounted for 36% (32% adjusted) of the outcome variance (R2 adj = .32), F(6, 92) = 8.68, p < .001. The path from 12-step attendance to motivation for abstinence (β = .21, p = .02) and from motivation for abstinence to substance use outcome (β = .40, p < .0001) appeared to account for the majority of the indirect effects. However, as shown in Table 2, there was a considerable degree of multicollinearity among the three mediators at 3 months. Multicollinearity can cause problems in the estimation of path coefficients, tending to inflate the standard errors of the estimates, which leads to imprecise, misleading, and even paradoxical results (Pedhazur, 1992). This could have accounted for the observed negative paradoxical effect of abstinence-focused coping measured at 3 months on substance use outcome (β = −.12), which would suggest that more coping skills are associated with fewer days abstinent. This also contradicted the positive zero-order relation (r = .17). These findings warranted separate tests for each mediator. Results revealed that neither abstinence-focused coping (z = 1.04, p = .15)nor self-efficacy (z = 1.11, p = .13) significantly mediated the relation between 12-step attendance and substance use outcome (controlling for baseline levels of the mediators, days abstinent at baseline, and aftercare meeting attendance). The model testing the mediational effect of motivation for abstinence revealed a significant indirect effect (z = 2.01, p = .02). The re-estimated path coefficients for the relations in this model can be seen in Figure 2.
Figure 2.
Path diagram depicting standardized coefficients of mediational effect of motivation for abstinence (with control variables). N = 99. M = months. † p < .10. * p < .05. ** p < .01. *** p < .001.
Attendance at 12-step meetings was significantly related to motivation for abstinence (β = .21, p = .03), which in turn significantly predicted substance use outcome in the following 3 months (β = .45, p < .0001).
Discussion
The present study prospectively examined the effects of 12-step meeting attendance on substance use outcome for adolescents in the 6 months following inpatient substance abuse treatment and tested a multivariate process model of factors leading to and affected by such attendance. Attendance at 12-step meetings in the first 3 months, both when examined concurrently and when predicting future substance use behavior, was associated with significant reductions in posttreatment substance involvement. This effect held even when other formal treatment factors, such as aftercare session attendance, days in inpatient treatment, and baseline levels of substance use, were taken into account.
The major mechanism identified in our study by which attendance at 12-step meetings seems to operate is by maintaining and enhancing motivation for abstinence, which in turn is associated with abstinence and lower levels of substance use. It may be that the testimony and sharing of past and present experiences, a central component of 12-step meeting process, serves to remind those in attendance of past negative consequences resulting from their own use while emphasizing benefits of remaining abstinent. In this way cognitions supportive of continued abstinence may be reinforced.
Twelve-step meeting attendance was also found to maintain and enhance abstinence-focused coping in the first 3 months posttreatment, but greater coping skills were not associated with lower levels of substance use in the second 3 months after treatment. This may be due to differences observed between adults and adolescents in substance use topography. As mentioned earlier, adolescents have less entrenched patterns of use and present with lower levels of physical dependence compared to adults. Therefore, it may be that motivation is the principal factor that serves as the catalyst for behavioral change in adolescents, overriding the need for specific abstinence-focused skills. Adults presenting for treatment, on the other hand (who possess on average greater dependency), might possess a strong desire to remain abstinent but may be less likely to do so without the acquisition and employment of specific coping skills. Indeed, this notion is captured within the postulates of cognitive-behavioral theories of relapse for adults (e.g., Marlatt & Gordon, 1985). Findings in this study would suggest a closer fit with self-regulation theory (Kanfer, 1987) and its derivative motivational enhancement theory (Miller & Rollnick, 1991). Adolescents with briefer substance involvement histories may be better able to “self-regulate” their behavior once they reach a commitment to do so.
Attendance at 12-step meetings did not affect self-efficacy measured at 3 months. However, self-efficacy did retain unique explanatory power in the equation predicting substance use between 3 and 6 months postdischarge. It may be that testimonials and admonitions from individuals who have relapsed, often heard at 12-step meetings, initially do not enhance confidence. Instead, such dialogue may again serve to increase motivation for continued abstinence and continued attendance. These findings appear to be consistent with the study by Morgenstern and colleagues (1997) in which adult AA affiliation in the first month after inpatient treatment had strong relations with motivation and active coping efforts but only a small effect on self-efficacy. Longer term follow-up would help elucidate how self-efficacy is affected by continued 12-step attendance over time.
When examined from a temporal-process perspective, the pattern of results suggests that adolescents in treatment who display a greater degree of substance dependency are consequently more motivated to cease their substance use. Motivation for abstinence is related to an increased likelihood of postdischarge attendance at 12-step meetings, but not aftercare meetings. This may be because a greater degree of effort is necessary to find and attend 12-step meetings in the community than to find and attend aftercare meetings, which typically occur at the same facility as the inpatient treatment. Adolescents who attend 12-step groups tend to realize increases in abstinence-focused coping skills and motivation. However, it is a continued commitment to abstain that appears to have the most impact on substance use.
In the present study we measured attendance at 12-step meetings but did not assess the degree of affiliation or acculturation with such groups. Although it seems feasible to assume that attendance may serve as a reasonable proxy for affiliation, prior research with adults has shown that affiliation with 12-step groups is more predictive of successful outcome than mere attendance at meetings (e.g., Montgomery et al., 1995; Snow, Prochaska, & Rossi, 1994). Affiliation can be differentiated from attendance when it is understood as active participation in fellowship meetings (e.g., speaking at meetings, receiving and/or giving tokens) and organized activities (e.g., dances and parties) and incorporating 12-step principles and strategies into one's daily life (e.g., meditation and calling a sponsor). This has implications for estimating the effectiveness of 12-step mutual-support groups in reducing substance use problems. A parallel can be made with formal treatment, because many individuals attend but do not become engaged by the treatment process, or actively participate in it. The same has been shown to be true in studies of other psychiatric disorders requiring medication compliance, which have shown that only 50% of individuals who are prescribed medications actually comply with the treatment regimen (Haynes, McKibbon, & Kanani, 1996). Therefore, to adequately assess whether a medication is effective it would be important to know whether the patient has been actually taking it. Thus, future research would do well to examine any incremental effects of affiliation with 12-step groups and substance use outcomes for adolescents.
For several reasons, the present findings must be interpreted cautiously. The small sample size may mean that obtained estimates do not truly reflect population parameters. This work should be replicated with larger samples. Also, given the high dropout rate and missing data, there are obvious generalizability issues. However, these concerns are ameliorated by a failure to find any systematic differences on important baseline variables. The correlational nature of the study may mean that unspecified variables may account for observed relations. However, the present study did control for possible demographic, problem severity, and treatment experience confounds, which adds to the validity of the conclusions. Also, the data collected in this study relied primarily on a monomethod, self-report, which may possibly bias estimates of population parameters (Campbell & Fiske, 1959). However, other possible reporting bias was minimized through collateral informants (parents) and biological assays. The follow-up period was also relatively short (6 months). However, this initial posttreatment phase is of critical clinical importance, because it requires an acute and demanding adjustment, and prior research has shown that, during this time, relapse for both adults and adolescents is most likely to occur (e.g., Brown, 1993). More lengthy prospective follow-ups are needed, however, to help elucidate the impact of these relations in the long term. In addition, only a single outcome was measured (days abstinent). Broader psychosocial domains of functioning, such as school and work performance, interpersonal relationships, and familial and emotional difficulties, would be useful to assess in future studies to examine the relative effects of 12-step attendance in these domains. A further limitation is the measure of self-efficacy used herein. Although such measures are in keeping with the literature in general, this may nevertheless over-simplify the construct. Also, the future time frame in relation to this measure was not limited to the next 3-month period but rather to “future use.” Finally, the modest explanatory power of 12-step attendance and the specified mediators imply other factors at work not specified in this model.
Of clinical importance is the fact that just over one fourth of the individuals treated did not attend any 12-step meetings during the first 3 months, and during the second 3-month period the number of adolescents not attending any 12-step meetings increased to almost 41% while the average number of meetings attended decreased. Given the importance attributed to meeting attendance within the chronic, disease model perspective of 12-step treatment philosophy, such nonattendance may diminish its effectiveness. According to Finney (1995), this could represent a “program failure” in that a weakness in the treatment chain occurs between treatment implementation and an intended proximal outcome (attendance at 12-step meetings). It would then follow that either more intensive treatment should be offered or a different therapeutic approach be taken. Given that motivation was only indirectly related to substance use outcome by means of 12-step attendance, use of motivational enhancement strategies proposed by Miller and Rollnick (1991) may prove useful in helping adolescents reflect on their current substance use status and its relation to current difficulties creating in turn a state of internal imbalance or dissonance sufficient to increase the likelihood of attendance at 12-step meetings. Alternatively, given that participants with a less severe substance abuse problem appear less motivated for abstinence and less likely to attend 12-step meetings, a different therapeutic focus on the interpersonal consequences of use rather than on the “disease”-related aspects may be a more fitting way to effect changes in those whose substance abuse is less severe. As Tober (1991) pointed out, use of a motivational enhancement approach may increase self-esteem and give adolescents a belief in their ability to have some control in their lives. More research is needed to determine the possibility of such attribute-treatment matching effects for this age group.
As explained earlier, it is also possible that adolescent nonattendance at 12-step groups may be due to developmentally specific logistical barriers not faced by adults (e.g., dependence on other people for transportation, adult composition of most groups). Thus, the effects of initial levels of motivation on subsequent attendance may be moderated by contextual factors, such as family support and resources. Future studies are needed to assess the impact of such differences on adolescent relapse.
In summary, these findings indicate that post-discharge attendance at 12-step meetings is associated with reductions in posttreatment substance involvement for adolescents. The modest salutary effect appears to operate primarily through maintaining and enhancing motivation to remain abstinent. In spite of this, many adolescents do not attend such groups, either because they are not convinced of the need to do so or because of environmental constraints related to their developmental status. In addition, unlike adults, the acquisition of specific abstinence-focused coping skills for youth, although a consequence of attendance at 12-step meetings, is not as crucial in effecting substance use behavior change for youth, at least in the early postdischarge months.
A multitude of studies in adult populations reveal that there is no uniformly right or optimal approach to treating psychoactive substance use disorders that is suitable in every case. This may be even more evident for adolescents. These results underscore the need for further studies with larger samples to examine more complex models of moderated mediation to begin to diagnose weak links in the causal chains of substance abuse treatments and determine which individuals, in particular, are vulnerable at these junctures.
Acknowledgments
This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA-07033), the Research Service of the Department of Veterans Affairs, and the National Institute on Drug Abuse (R29DA-09181). We thank Denis McCarthy for his help in the preparation of this article.
Footnotes
The terms 12-step group and 12-step meeting refer to attendance at Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) meetings where mentioned in this article.
Because of numeric variation in calendar months the “3-month” and “6-month” time windows actually refer to 90- and 180-day periods.
Because self-efficacy, as measured herein, refers to likelihood of future substance use rather than abstinence, its relation with 12-step attendance and days abstinent is negative.
Contributor Information
John F. Kelly, Joint Doctoral Program in Clinical Psychology, University of California, San Diego, and Joint Doctoral Program in Clinical Psychology, San Diego State University
Mark G. Myers, Department of Psychiatry, University of California, San Diego, and Psychology Service, Veterans Affairs San Diego Healthcare System
Sandra A. Brown, Department Psychiatry and Department of Psychology, University of California, San Diego, and Psychology Service, Veterans Affairs San Diego Healthcare System.
References
- Alford GS, Koehler RA, Leonard J. Alcoholics Anonymous-Narcotics Anonymous model inpatient treatment of chemically dependent adolescents: A 2-year outcome study. Journal of Studies on Alcohol. 1991;52:118–126. doi: 10.15288/jsa.1991.52.118. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Bentler PM, Wu L. EQS (Version 5.7b) BMDP Statistical Software; Los Angeles: 1995. [Google Scholar]
- Brown SA. Alcohol use and type of life events experienced during adolescence. Psychology of Addictive Behaviors. 1987;1:104–107. [Google Scholar]
- Brown SA. Recovery patterns in adolescent substance abuse. In: Baer JS, Marlatt GA, McMahon RJ, editors. Addictive behaviors across the life span: Prevention, treatment, and policy issues. Sage; Newbury Park, CA: 1993. pp. 161–183. [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott M. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol. 1996;57:314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Brown SA, Mott MA, Myers MG. Adolescent alcohol and drug treatment outcome. In: Watson ERR, editor. Drug and alcohol abuse prevention: Drug and alcohol abuse reviews. Humana; Clifton, NJ: 1990. pp. 373–403. [Google Scholar]
- Brown SA, Myers MG, Lippke L, Stewart D, Tapert SF, Vik M. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Bukstein OG. Adolescent substance abuse: Assessment, prevention, and treatment. Wiley; New York: 1995. [Google Scholar]
- Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin. 1959;56:81–105. [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: What is currently known? In: McCrady EBS, Miller EWR, editors. Research on Alcoholics Anonymous: Opportunities and alternatives. Alcohol Research Documentation; New Brunswick, NJ: 1993. pp. 41–76. [Google Scholar]
- Finney JW. Enhancing substance abuse treatment evaluations: Examining mediators and moderators of treatment effects. Journal of Substance Abuse. 1995;7:135–150. doi: 10.1016/0899-3289(95)90310-0. [DOI] [PubMed] [Google Scholar]
- Garber J. Classification of childhood psychopathology: A developmental perspective. Child Development. 1984;55:30–48. [PubMed] [Google Scholar]
- Haynes RB, McKibbon KA, Kanani R. Systematic review of randomized trials of interventions to assist patients to follow prescriptions for medications. The Lancet. 1996;348:383–386. doi: 10.1016/s0140-6736(96)01073-2. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two-factor index of social position. Yale University Press; New Haven, CT: 1965. [Google Scholar]
- Hsieh S, Hoffman NG, Hollister DC. The relationship between pre-, during-, posttreatment factors, and adolescent substance abuse behaviors. Addictive Behaviors. 1998;23:477–488. doi: 10.1016/s0306-4603(98)00028-8. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Clinicians' referral and matching of substance abuse patients to self-help groups after treatment. Psychiatric Services. 1997;48:1445–1449. doi: 10.1176/ps.48.11.1445. [DOI] [PubMed] [Google Scholar]
- Kanfer FH, editor. Self-regulation and behavior. Springer-Verlag; Heidelberg, Germany: 1987. [Google Scholar]
- Kelly JF, Myers MG. Adolescent treatment outcome in relation to adolescent 12-step group attendance. Alcoholism: Clinical and Experimental Research. 1997;21:27a. [Google Scholar]
- Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- McElrath D. The Minnesota model. Journal of Psychoactive Drugs. 1997;29:141–144. doi: 10.1080/02791072.1997.10400180. [DOI] [PubMed] [Google Scholar]
- Miller NS, Ninonuevo FG, Klamen DL, Hoffmann NG. Integration of treatment and posttreatment variables in predicting results of abstinence-based outpatient treatment after one year. Journal of Psychoactive Drugs. 1997;29:239–248. doi: 10.1080/02791072.1997.10400197. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. Guilford Press; New York: 1991. [Google Scholar]
- Montgomery HA, Miller WR, Tonigan JS. Does Alcoholics Anonymous involvement predict treatment outcome? Journal of Substance Abuse Treatment. 1995;12:241–246. doi: 10.1016/0740-5472(95)00018-z. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney JW, Ouimette PC, Suchinsky RT. A comparative evaluation of substance abuse treatment: I. Treatment orientation, amount of care, and 1-year outcomes. Alcoholism: Clinical & Experimental Research. 1999;23:529–536. [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW. Affiliation with Alcoholics Anonymous after treatment: A study of its therapeutic effects and mechanisms of action. Journal of Consulting & Clinical Psychology. 1997;65:768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. The Adolescent Relapse Coping Questionnaire: Psychometric validation. Journal of Studies on Alcohol. 1995;57:40–46. doi: 10.15288/jsa.1996.57.40. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA, Mott MA. Coping as a predictor of adolescent substance abuse treatment outcome. Journal of Substance Abuse. 1993;5:15–29. doi: 10.1016/0899-3289(93)90120-z. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA, Vik PW. Adolescent substance use problems. In: Mash EEJ, Russell EA, Barkley J, editors. Treatment of childhood disorders. 2nd ed. Guilford Press; New York: 1998. pp. 692–729. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism . National Drug and Alcoholism Treatment unit survey. U. S. Government Printing Of-rice; Washington, DC: 1993. (DHHS Publication No. SMA 93–200). [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism & National Institute on Drug Abuse . State resources and services related to alcohol and other drug abuse problems, fiscal year 1992. U.S. Department of Health and Human Services; Rockville, MD: 1995. [Google Scholar]
- Pedhazur E. Multiple regression in behavioral research: Explanation and prediction. 2nd ed. Harcourt Brace Jovanovich; Orlando, FL: 1992. [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997a;58:7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group Secondary a priori hypotheses. Addiction. 1997b;92:1671–1698. [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical & Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Roman PM, Blum TC. National treatment center study. Summary report (No. 3): Second wave on-site results. University of Georgia; 1998. Unpublished manuscript. [Google Scholar]
- Sklar SM, Annis HM, Turner ME. Development and validation of the Drug-Taking Confidence Questionnaire: A measure of coping self-efficacy. Addictive Behaviors. 1997;22:655–670. doi: 10.1016/s0306-4603(97)00006-3. [DOI] [PubMed] [Google Scholar]
- Snow MG, Prochaska JO, Rossi JS. Processes of change in Alcoholics Anonymous maintenance factors in long-term sobriety. Journal of Studies on Alcohol. 1994;55:362–371. doi: 10.15288/jsa.1994.55.362. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten JR, Allen J, editors. Measuring alcohol consumption. Humana; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Stewart DG, Brown SA. Withdrawal and dependency symptoms among adolescent alcohol and drug abusers. Addiction. 1995;90:627–635. doi: 10.1046/j.1360-0443.1995.9056274.x. [DOI] [PubMed] [Google Scholar]
- Swadi H. A longitudinal perspective on adolescent substance abuse. European Child & Adolescent Psychiatry. 1992;1:156–169. doi: 10.1007/BF02091901. [DOI] [PubMed] [Google Scholar]
- Tarter RL, Kirisci L, Hegedus A, Mezzich A, Vanyukov MM. Heterogeneity of adolescent alcoholism. In: Babor TF, Hessel-brock VM, Meyer WS, editors. Annals of the New York Academy of Sciences: Vol. 708. Types of alcoholics: Evidence from clinical, experimental, and genetic research. New York Academy of Sciences; New York: 1994. pp. 172–180. [DOI] [PubMed] [Google Scholar]
- Tober G. Motivational interviewing with young people. In: Miller W, Rollnick S, editors. Motivational interviewing: Preparing people to change addictive behavior. Guilford Press; New York: 1991. pp. 248–259. [Google Scholar]
- Vik PW, Grizzle KL, Brown SA. Social resource characteristics and adolescent substance abuse relapse. Journal of Adolescent Chemical Dependency. 1992;2:59–74. [Google Scholar]
- Winters KC, Stinchfield RD, Henly GA. Further validation of new scales measuring adolescent alcohol and other drug abuse. Journal of Studies on Alcohol. 1993;54:534–541. doi: 10.15288/jsa.1993.54.534. [DOI] [PubMed] [Google Scholar]