Abstract
Data from 1,543 female migrants working in eight occupational clusters in Beijing and Nanjing, China were analysed to examine the association of workplace with HIV-related behaviours and perceptions. For sexually experienced women (n = 666, 43.2%), those working in entertainment establishments or personal service (e.g., nightclubs, dancing halls, barbershops, beauty salons, massage parlours, etc.) engaged in risky sexual practices twice as frequently as those working in non-entertainment establishments (e.g. restaurants, stalls, domestic service, factories, etc.). About 10% of women in the entertainment establishments reported having sold sex, 30% having multiple sexual partners and 40% having sex with men with multiple sexual partners. The rate of consistent condom use was less than 15%. They also tended to have a higher level of perceptions of both peer risk involvement and positive expectancy of risk behaviours, and lower perceptions of severity of STDs and HIV. For women who were not sexually experienced, those working in ‘stalls’ or ‘domestic service’ tended to perceive higher peer risk involvement, less severity of HIV infection, and less effectiveness of protective behaviour. The occupational pattern of sexual risk behaviours and perceptions observed in the current study indicates employment conditions are associated with HIV risk. Intervention strategies should be tailored to address occupational-related factors.
Introduction
Migrant workers have been identified as a population at risk for acquiring and transmitting HIV in many countries (Hope, 2000; Lurie et al., 2003; Li et al., 2004). For several reasons female migrants are believed to be more vulnerable than their male counterparts. First, women have greater biological susceptibility to HIV during sexual intercourse. The risk of HIV infection through unprotected vaginal sex with an infected person is estimated to be 2 to 4 times higher for women than for men (Turmen, 2003). Second, inequality in power and socioeconomic status places women at greater risk of HIV infection. In many developing countries, women are dependent on men socially, economically, and/or emotionally, thus impairing their ability to persuade their sexual partners to use condoms (Tang et al., 2001). Third, the social context of the work setting may also put female migrant workers at increased risk of exposure to various risk behaviours. Most male migrants work in labour-intensive industries, while most female migrants work in entertainment or service industries (Feng et al., 2002).
Several studies have established that high risk sexual behaviours are related to the working environment. In Tanzania, women working in bars were considered to be at high risk of HIV infection by local health authorities (Mgalla & Pool, 1997). Among commercial sex workers, potential risks of HIV infection were also found to vary substantially according to the organization of work and working conditions (Ford et al., 1998; Jachson et al., 1992). The relationship between work setting and an individual’s behaviour was also supported by the effectiveness of establishment-based HIV/STD prevention intervention activities (Ford et al., 1996; Kelly et al., 1997; Miller et al., 1998). Because female migrant workers may be a highly stratified and heterogeneous population in terms of their working environment, identifying the relationship between the workplace and HIV risk may help researchers to develop appropriately targeted prevention intervention strategies among this vulnerable subpopulation.
HIV/AIDS epidemic in China
China is experiencing an accelerating HIV epidemic (Settle, 2003). Although intravenous drug use and commercial blood/plasma donation are the predominant modes of HIV transmission, the proportion of persons infected through heterosexual intercourse is increasing, from 5.5% in 1997 to 10.9% in 2002 (UNAIDS, 2003a). The number of infected women appears to be rapidly expanding as well, with the male to female ratio falling from 9:1 in the early 1990s to 3:1 in 2001 (Settle, 2003). Several social and economic factors facilitate HIV/AIDS spread in China, including population mobility. Its about 100 million rural-to-urban migrants have been identified as the ‘tipping point’ for the HIV/AIDS epidemic in China (Anderson et al., 2003). Predominantly a rural epidemic in China, the prevalence of HIV among rural-to-urban migrants was observed to be 1.8 times higher than that among rural residents who did not migrate to cities (Xu et al., 1998).
Female migrants and their employment conditions in cities
Although males are generally more mobile than females, the overall proportion of migrants who are female in China has increased from 26% in 1986 to 40% in 1997 (Wan, 1995; Shen & Huang, 2003). In fact, among younger migrants (e.g. 15–19 years of age), the proportion of female migrants exceeds that of males (Zhang et al., 1998). Young migrant women mainly work in private (i.e. non-state-run) factories, entertainment or commercial service sectors, such as nightclubs, beauty salons, massage parlours, and retail or domestic services (Zheng, 2001).
Urban-based labour for female migrants varies greatly in terms of employment conditions. For both construction and factory workers, rigid work schedules and management regulations greatly restrict their contact with locals (Zheng, 2001). Migrant retailers supply a variety of consumable goods (e.g. food, clothes, grocery, etc.) and provide a wide range of services (e.g. dry-cleaning, appliance repairing, etc.) to urban residents. Many stalls are run by migrant husband and wife teams and are primarily patronised by housewives. The migrants typically live close to work and socialize within that area (Detels et al., 2003). Domestic service workers in cities include maids, babysitters, caregivers caring for the elder or ill patient, and those who receive payment based on completion of tasks (e.g. delivering household goods) or the amount of time spent (e.g. hourly-paid workers). Most maids, babysitters and caregivers provide full-time, live-in help (Roberts, 1997). Workers paid by the hour may be employed by several households at the same time. They usually live by themselves or with their families, relatives or friends.
Beauty salons or barbershops provide hair and facial services. They are open from 9 or 10 am and remain open until 11 pm or even later. Many young women are employed by beauty salons or barbershops to provide low-technique service such as hair-washing and head massage (requiring no more than one week of on-the-job training). Bathhouses are places where bath, massage and entertainment (e.g. chess, billiards, etc.) are available in a single location, and are primarily oriented to the needs of middle- and high-income people. These establishments are usually open 24 hours a day and are especially busy at night from late evening to early morning. Women in bathhouses/massage parlours include massage technicians who provide head, foot or body massage services to customers, and receptionists, who are responsible for welcoming customers or providing customers with drinks, snacks or towels. Women working in beauty salons or bathhouses receive a base salary, supplemented by bonuses that are proportional to the number of customers they serve. They have contact with a wide range of persons during work (Zheng, 2001) and socializing with customers during work is expected.
Dance halls or nightclubs are places for entertainment or socialization (e.g. business discussions, enhancing relationships with clients, friends gathering, or seeking excitement). Women working in such establishments include waitresses and entertainers. Waitresses, who provide drinks and snacks, are employed by the owner and have formal fixed work schedules and salaries. Most entertainers, however, are not employed by the owner but are allowed to work at the establishments because they attract clients and promote business through their escort services. Their income is mainly dependent on payments or tips from the customers.
Differing employment conditions may foster higher potential risks of HIV infection in some occupational clusters compared to others. However, little is known about the relationship between venues and risk behaviours within them. While previous studies have begun to address the issues related to workplace and risk, most of them have focused on migrant women who were identified as commercial sex workers (Pan, 1999; Rogers et al., 2002). Therefore, the current study was designed to explore the association of workplace and occupation with HIV-related sexual behaviours and perceptions among female migrant workers.
Methods
Sampling and data collection
Data in the current study were drawn from a feasibility study of an HIV/STD behavioural prevention intervention among Chinese rural-to-urban migrants, in which migrants were defined as individuals who moved from rural areas for jobs without benefit of an official household registration in the urban area. Young migrants aged 18 to 30 were eligible for the study. Ten main occupational clusters (restaurants, hotels, barbershops/beauty salons, bathhouses/massage parlours, nightclubs/karaoke/dance halls/bars, small retail shops, street vendors, domestic services, constructions and factories) which employ more than 90% of the migrants, plus job markets served as the sampling frame. Quota-sampling of occupational groups was utilized so that the number of participants in each occupational cluster was approximately proportional to the overall estimated size of the clusters.
Before starting the survey, gatekeepers, employers or workplace managers were contacted. After obtaining permission to conduct surveys at their premises, trained outreach staff went to these workplaces to recruit eligible migrants. Informed consent was obtained from individuals willing to participate. Participants completed a self-administered questionnaire in a separate room or private space at the workplace or a nearby place convenient to participants. The questionnaire, which took approximately 40–60 minutes to complete, consisted of six parts, including demographic information, working and living conditions, health status and health seeking behaviours, HIV/AIDS related knowledge, behaviours and perceptions. Participants were assured of confidentiality and anonymity and no personal identifiable information was asked on the questionnaire. Necessary assistance was provided to a few participants with limited literacy. Detailed methods for sampling and data collection have been described elsewhere (Li et al., 2004). A total of 4,301 migrants were approached for the survey. Of them, 24 (0.6%) subjects declined to participate and 69 (1.6%) missed key demographic or other substantial questions. A final sample of 4,208 (98%) was retained in the database. Among these 4,208 participants, 40% (n = 1699) were women and 60% (n = 2509) were men. Their mean age was 24.5 years (SD = 3.8). The majority of participants were Han ethnicity (97%), single (72%) and had finished at least elementary school (94%). Nearly 96% of the participants were currently employed or self-employed. The participants had an average of 4.3 years’ experience of migration, with 58% having migrated to at least two cities before participating in our study.
Measures
Several composite variables such as workplace, sexual behaviours and perceptions were created for the purpose of data analysis in the current study
Workplace
Among the 1,699 female migrants in the feasibility study sample, 54 (3.2%) reported having no jobs, 96 (5.6%) reported working in places other than the ten occupational clusters, and 6 (0.4%) provided no information regarding their current jobs. The sample in the current study consists of the 1,543 (90.8%) female migrants who were employed in the 10 defined occupational clusters. Since only a small number of female migrants were recruited from construction sites (n = 18) and retail shops (n = 46), these two venues were combined with factories and street vendors, respectively, because of the similarity of the work settings. Thus, eight occupational categories were included in the current study: ‘restaurant’, ‘hotel’, ‘hair salon’ (barbershop or beauty salon), ‘massage’ (massage centre or bathhouse), ‘nightclub’ (nightclub, karaoke, dancing hall or bar), ‘stall’ (street vendor or small retail shop), ‘factory’ (construction or factory), and ‘domestic service’.
Risk sexual behaviours
This score was created by indexing those who had initiated sex before the age of 20 (i.e. the legal age of marriage for women in China), had engaged in pre-marital sex, had had multiple sexual partners, had traded sex for money, and had partners who were having sex with others. The internal consistency of this scale, as measured with Cronbach alpha, was 0.68 and the possible score ranged from 0 to 5, with higher scores reflecting higher sexual risk.
Protective sexual behaviours
The protective score was created by indexing those who always used condoms in their sexual life, used a condom every time during the most recent three sexual intercourses, had discussed condom use with sexual partners, and knew how to use a condom correctly. The internal consistency of this scale was 0.61 and the possible score ranged from 0 to 4, with higher scores reflecting greater protective behaviour involvement.
HIV/AIDS knowledge
The AIDS knowledge score (possible range 0–11) was created by summing the correct responses to 11 items covering modes of transmission and clinical symptoms of HIV infection, with a higher score reflecting a higher level of knowledge about HIV/AIDS. The internal consistency of this scale was 0.71.
Several HIV-related perceptions were assessed, including perceived peer risk involvement, positive expectancy of risk behaviour, severity of disease, effectiveness of protective behaviour and vulnerability to HIV/STD.
Peer risk behaviour involvement
Five questions were used to assess perceived peer risk behaviour involvement. Participants were asked about how many (1 = none, 2 = few, 3 = some, and 4 = most) of their peers (including those at their home villages) had engaged in a number of HIV/STD risk behaviours, including having multiple sexual partners, having unprotected sex, trading sex (selling or buying sex), and having contracted an STD. The internal consistency of the scale was 0.85. A composite score, ranging from 1 to 20, was created by summing responses to these five questions, with a higher score reflecting a higher level of perceived peer risk involvement.
Positive expectancy of risk behaviour
Four questions were asked to assess the positive expectancy of risk behaviour, such as ‘having multiple sexual partners is cool’ and ‘Many people have extra-marital sexual behaviours because of loneliness and depression’. Each question had a 4-point response ranging from 1 = ‘strongly disagree’ to 4 = ‘strongly agree’. A composite score was calculated by summing responses to these four questions, with higher scores reflecting higher levels of positive expectancy of risk behaviours. The internal consistency of the scale was 0.65.
Severity
Perceived negative consequences of engaging in risk behaviours were measured by four questions, such as ‘if someone catches HIV/STD, he/she will lose friends’, ‘if someone is infected with HIV, his/her family member should keep away from him/her’, and ‘if someone becomes infected with HIV, his/her life is ruined’. Each question had a 4-point response option ranging from 1 = ‘strongly disagree’ to 4 = ‘strongly agree’. A composite score, ranging from 1 to 16, was created by summing responses to these four questions, with higher scores reflecting higher levels of perceived severity of the disease. The internal consistency of the scale was 0.61.
Vulnerability
Perceived vulnerability to HIV/STDs infection was measured through two items assessing the perceived likelihood of acquiring HIV or STDs. Participants were asked to rate the likelihood along a 5-point scale (1 = ‘very unlikely’, 2 = ‘unlikely’, 3 = ‘likely’, 4 = ‘very likely’ and 5 = ‘already infected’). A composite score, ranging from 1 to 10, was calculated by adding responses to these two questions. Higher scores reflect higher levels of perceived vulnerability to HIV or STD infection. The internal consistency of the scale was 0.83.
Perceived effectiveness of protective behaviour
Perceived effectiveness of protective behaviour was assessed by five items, such as ‘Using a condom is an important way to prevent STD/HIV’, ‘You can become infected with STD by having sex without protection even once’ and ‘If a woman takes contraceptive measures, there is no need to use condoms’. Each question had a 4-point response raging from 1 = ‘strongly disagree’ to 4 = ‘strongly agree. A composite score, ranging from 1 to 20, was calculated by summing responses (with necessary reverse coding) to these five questions, with a higher score reflecting a higher level of perceived effectiveness. The internal consistency of the scale was 0.63.
Analyses
All analyses were conducted with SPSS for Windows, Version 11.5 (SPSS Inc. 2002). First, Chi-square tests (for categorical variables) or ANOVA (for continuous variables) were performed to examine the relationship between work venue and sociodemographic characteristics, HIV-related behaviours and perceptions. Since information on HIV-related sexual behaviours was not available for women who had no sexual experience, the venue pattern of sexual behaviours was analysed only for sexually experienced women. Second, homogeneity of regression was performed to test the assumption for multivariate analysis of covariance (MANCOVA) through SPSS syntax (Tabachnick & Fidell, 2001). Each dependent variable in a hierarchy of dependent variables was assessed in MANCOVA with higher-priority dependent variables serving as covariates. For sexually experienced women, the hierarchy of dependent variables was perceived peer risk involvement, risk sexual behaviour, protective sexual behaviour, HIV knowledge, positive expectancy of risk behaviour, severity, perceived effectiveness of protective behaviour and vulnerability to the disease. For sexually inexperienced women, the hierarchy of dependent variables was the same as that for sexually experienced women except that risk sexual behaviour and protective sexual behaviour were omitted. Third, MANCOVA was employed to examine the relationship between workplace and HIV related behaviours and perceptions for sexually experienced women and sexually inexperienced women separately. Age, educational attainment and income were included as covariates as they may confound the relationship between workplace and sexual behaviours and perceptions. Pillais Trace was used for evaluating multivariate significance, and Roy-Bargmann stepdown F tests were run for evaluating the effect of workplace on each dependent variable with adjustment for covariates.
Results
Sample characteristics
The sociodemographic characteristics of the study sample are presented by workplace in Table I. Most of the women were in their 20s (78%), not married (78%), had received no more than 9 years of formal education (60%) and had a monthly income of less than 800 RMB, or equivalent US$ 98 (61%). About 90% had been in the cities for more than one year.
Table I.
Sociodemographic characteristics of female migrant workers by workplace.
| Sociodemographic characteristics | Total (n = 1543) | Restaurant (n = 345) | Hotel (n = 129) | Stall/shop (n = 148) | Domestic service (n = 142) | Factory/construction (n = 134) | Hair salon (n = 337) | Massage (n = 210) | Nightclub (n = 98) |
|---|---|---|---|---|---|---|---|---|---|
| Demographics: | |||||||||
| Age: <20y (%) | 17.2 | 29.4 | 17.1 | 10.8 | 20.4 | 9.7 | 15.1 | 10.5 | 11.2 *** |
| Never married (%) | 77.7 | 79.5 | 80.2 | 62.9 | 65.0 | 76.7 | 83.9 | 81.3 | 81.3 *** |
| Education: ≤9 grades (%) | 60.3 | 63.5 | 46.9 | 55.8 | 85.8 | 70.7 | 63.4 | 45.2 | 43.3 *** |
| Employment condition: | |||||||||
| Monthly income: <800 RMB (%) | 61.4 | 91.6 | 77.3 | 63.9 | 77.3 | 69.9 | 33.3 | 39.4 | 37.5 *** |
| Daily work hours: > = 10h (%) | 38.2 | 25.8 | 14.8 | 32.9 | 29.7 | 9.0 | 73.6 | 55.5 | 15.4 *** |
| Monthly rest days: <5d (%) | 87.6 | 90.1 | 77.3 | 85.7 | 90.7 | 50.0 | 96.7 | 95.7 | 93.6 *** |
| History of migration: | |||||||||
| Staying with whom in the city: | |||||||||
| Alone (%) | 10.3 | 8.1 | 7.8 | 9.5 | 25.4 | 6.0 | 9.5 | 9.5 | 11.2 *** |
| Family member(s) (%) | 26.0 | 21.2 | 22.7 | 52.7 | 30.3 | 22.4 | 23.1 | 23.3 | 22.4 *** |
| Coworker (s)/peer(s) (%) | 55.0 | 67.5 | 69.0 | 26.4 | 8.5 | 61.2 | 63.8 | 58.6 | 57.1 *** |
| Changing jobs at least twice a year (%) | 24.2 | 33.1 | 16.4 | 24.3 | 25.5 | 19.5 | 18.5 | 21.6 | 32.7 *** |
| Years of being in the city: <1y (%) | 10.8 | 15.4 | 13.3 | 8.8 | 5.6 | 5.2 | 10.4 | 9.1 | 14.3 ** |
| Having ever had sex (%) | 43.2 | 29.6 | 41.1 | 54.0 | 43.7 | 32.8 | 41.8 | 56.7 | 66.3 *** |
Notes:
P < 0.01;
P < 0.001
Socio-demographic characteristics differed by occupational category. ‘Restaurants’ had a larger proportion of women who were younger than 20 years of age (29%). Women working in ‘domestic service’ or ‘factories’ were less educated than women working in ‘massage parlours’, ‘nightclubs’ or ‘hotels’. Women in ‘stalls’ or ‘domestic service’ were more likely to be married and live with their family members or live alone. More single women were found in ‘hair salons’, ‘massage parlours’ or ‘nightclubs’; and the income of women from these three workplaces appeared to be higher. Women working in ‘nightclubs’ or ‘restaurants’ appeared to have more recently migrated to the city, with nearly 15% having been in the city for less than one year. They also tended to have less job stability, with about one-third changing their jobs at least twice a year.
Among the 1,543 female migrant workers, 666 (43.2%) had ever had sex. The proportion of sexually experienced women ranged from 66.3% among those working in ‘nightclubs’ to 29.6% among those in ‘restaurants’. After considering their marital status, 46.9% of women working in ‘nightclubs’ had ever had sex but never married. This proportion was 37.8% for women in ‘massage parlours’, 26.5% in ‘hair salons’, 21.6% in ‘hotels’, 17.1% in ‘stalls’, and about 9% in ‘factories’, ‘restaurants’ and ‘domestic service’.
Venue pattern of sexual behaviours
The sexual risk behaviour scores, ranging from 0 to 5, were significantly different by venue among sexually experienced women. As shown on the left-hand side of Figure 1, the means of the sexual-risk-behaviour score for women employed in ‘hair salons’, ‘massage parlours’ and ‘nightclubs’ (i.e., entertainment establishments or personal service) were all above 2, which were almost twice as high as those for women working in ‘restaurants’, ‘stalls’, ‘domestic service’ and ‘factories’. Each specific sexual risk behaviour varied by occupation as well (Table II). The proportion of each sexual risk behaviour for women working at ‘hair salons’, ‘massage parlours’ and ‘nightclubs’ was almost twice that seen among women from ‘restaurants’, ‘stalls’, ‘domestic service’ and ‘factories’.
Figure 1.
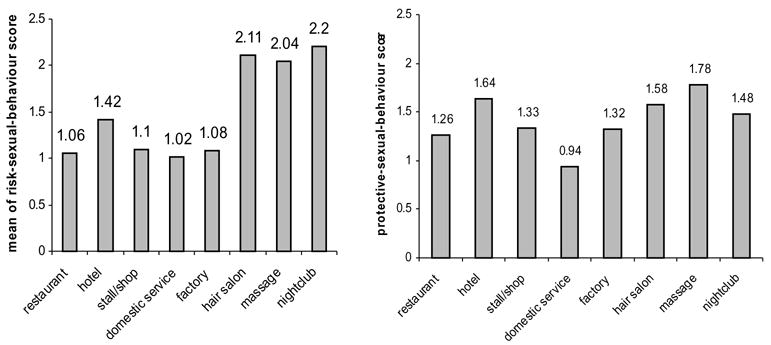
Mean of sexual behaviour scores by workplace.
Table II.
Percentage of sexual behaviour by workplace among sexually experienced women.
| Risk sexual behaviour
|
Protect sexual behaviour
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex debut <20yr | Pre-marital sex | Sex partners have sex with others | Multiple sexual partners, lifetime | Having sold sex | 100% condom use, lifetime | Discussion of condom use | Knowing correctly use condom | 100% condom use, last 3 sexes | |
| Total (n = 666) | 40.0 | 60.4 | 35.7 | 22.3 | 6.9 | 8.7 | 53.6 | 70.0 | 16.0 |
| Restaurant (n = 102) | 24.7 | 43.0 | 19.8 | 14.5 | 4.7 | 3.5 | 49.4 | 65.1 | 10.5 |
| Hotel (n = 53) | 20.0 | 56.8 | 38.6 | 22.2 | 6.7 | 11.4 | 57.8 | 71.1 | 24.4 |
| Shop/stall (n = 80) | 32.9 | 38.9 | 31.9 | 7.0 | 2.9 | 2.9 | 51.4 | 71.4 | 7.5 |
| Domestic service (n = 62) | 34.0 | 28.6 | 30.8 | 12.0 | 2.0 | 3.9 | 30.8 | 51.9 | 7.8 |
| Factory (n = 44) | 24.3 | 39.5 | 23.7 | 15.8 | 5.4 | 2.6 | 48.6 | 66.7 | 18.9 |
| Hair salon (n = 141) | 54.5 | 77.6 | 44.3 | 31.0 | 10.9 | 11.6 | 57.1 | 72.9 | 19.2 |
| Massage (n = 119) | 47.0 | 78.3 | 42.1 | 31.6 | 6.1 | 13.9 | 63.5 | 79.8 | 21.9 |
| Nightclub (n = 65) | 56.7 | 83.1 | 43.3 | 29.3 | 13.1 | 13.3 | 55.9 | 67.8 | 15.0 |
| Overall P value | <0.001 | <0.001 | 0.005 | 0.001 | 0.129 | 0.024 | 0.014 | 0.034 | 0.041 |
The relationship of protective sexual behaviour to occupation is presented on the right-hand side of Figure 1. Sexually experienced women working in ‘domestic service’ reported the lowest mean score of protective behaviours. The percentages of each specific sexual protective behaviour are presented in Table II. The highest rates of consistent condom use were found among women from ‘massage parlours’ (13.9%) and ‘nightclubs’ (13.3%). The highest rates of last-three-sexual-intercourse-condom-use were observed among women from ‘hotel’ (24.4%), ‘massage’ (21.9), ‘hair salon’ (19.2%) and ‘factory’ (18.9%).
Venue pattern of HIV-related perceptions
Mean scores of HIV/AIDS knowledge and HIV-related perceptions by sexual experience and workplace are presented in Table III. For sexually experienced women, significant differences were found in perceived peer risk involvement, positive expectancy of risk behaviour and severity across the eight occupational groups. Women in ‘hair salons’ or ‘nightclubs’ tended to have higher perceptions (e.g. higher than mean) of peer risk involvement and positive expectancy of risk behaviours, and lower perceptions of severity of HIV/STD infection. Higher perception of positive expectancy of risk behaviour and lower perception of severity were also found among women working in ‘domestic service’.
Table III.
Means and standard deviations of HIV-related perceptions by sexually experience and workplace.
| HIV knowledge
|
Peer risk involvement
|
Positive expectancy of risk behaviour
|
Vulnerability
|
Severity
|
Effectiveness of protective behaviour
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent variables | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Sexually experienced women | ||||||||||||
| Total | 7.8 | 2.5 | 7.4 | 3.1 | 8.2 | 2.3 | 7.3 | 1.2 | 10.5 | 2.1 | 10.7 | 2.4 |
| Restaurant | 7.3 | 2.5 | 7.1 | 2.6 | 7.8 | 2.2 | 7.3 | 1.3 | 11.0 | 2.0 | 11.0 | 2.4 |
| Hotel | 8.2 | 2.6 | 7.5 | 3.2 | 7.5 | 2.4 | 7.5 | 0.9 | 11.0 | 1.8 | 10.9 | 2.3 |
| Stall/shop | 8.0 | 2.3 | 6.9 | 2.7 | 7.7 | 2.1 | 7.5 | 0.8 | 10.7 | 2.3 | 11.2 | 2.6 |
| Domestic service | 7.6 | 2.6 | 7.0 | 2.9 | 8.4 | 2.5 | 7.2 | 1.4 | 9.7 | 2.4 | 10.5 | 2.7 |
| Factory/construction | 8.2 | 2.2 | 6.6 | 2.8 | 8.1 | 2.1 | 7.5 | 1.0 | 10.8 | 2.3 | 10.1 | 1.9 |
| Hair salon | 7.7 | 2.6 | 7.9 | 3.5 | 8.4 | 2.3 | 7.2 | 1.2 | 10.4 | 2.0 | 10.5 | 2.3 |
| Massage | 7.9 | 2.6 | 7.3 | 2.3 | 8.5 | 2.2 | 7.2 | 1.1 | 10.5 | 2.0 | 10.6 | 2.0 |
| Nightclub | 7.4 | 2.2 | 8.6 | 4.3 | 8.8 | 2.9 | 7.0 | 1.4 | 10.2 | 2.4 | 10.9 | 2.8 |
| F value | F(7,657) = 1.271 | F(7,654) = 3.098 | F(7,657) = 2.623 | F(7,655) = 1.725 | F(7,657) = 2.645 | F(7,657) = 1.484 | ||||||
| Omnibus P value | 0.262 | 0.003 | 0.011 | 0.100 | 0.011 | 0.170 | ||||||
| Sexually inexperienced women | ||||||||||||
| Total | 7.6 | 2.4 | 6.2 | 2.3 | 7.8 | 2.2 | 7.5 | 0.9 | 10.9 | 2.0 | 11.0 | 2.4 |
| Restaurant | 7.4 | 2.3 | 6.2 | 2.4 | 7.9 | 2.1 | 7.4 | 0.9 | 11.1 | 2.0 | 11.4 | 2.6 |
| Hotel | 7.9 | 2.6 | 5.8 | 1.6 | 7.7 | 2.0 | 7.4 | 0.8 | 11.1 | 2.0 | 11.0 | 2.4 |
| Stall/shop | 8.3 | 2.3 | 6.9 | 2.9 | 8.2 | 2.1 | 7.5 | 0.8 | 10.5 | 2.1 | 10.4 | 2.8 |
| Domestic service | 7.9 | 2.0 | 7.5 | 3.2 | 8.1 | 1.8 | 7.6 | 0.8 | 10.3 | 2.0 | 10.3 | 2.0 |
| Factory/construction | 7.6 | 2.3 | 5.6 | 1.4 | 7.5 | 2.3 | 7.5 | 1.0 | 11.2 | 1.6 | 11.2 | 1.9 |
| Hair salon | 7.4 | 2.5 | 6.2 | 2.2 | 7.6 | 2.6 | 7.5 | 0.9 | 10.9 | 2.1 | 11.1 | 2.5 |
| Massage | 7.6 | 2.3 | 6.1 | 1.8 | 7.8 | 2.0 | 7.6 | 0.8 | 10.6 | 2.0 | 10.6 | 2.1 |
| Nightclub | 7.6 | 2.2 | 6.2 | 1.8 | 8.2 | 2.7 | 7.4 | 0.9 | 10.6 | 2.3 | 10.6 | 2.9 |
| F value | F(7,850) = 1.525 | F(7,847) = 5.664 | F(7,850) = 1.127 | F(7,848) = 0.872 | F(7,850) = 2.061 | F(7,846) = 3.212 | ||||||
| Omnibus P value | 0.155 | B/0.001 | 0.344 | 0.528 | 0.045 | 0.002 | ||||||
For women who were not sexually experienced, there were significant differences in perceived peer risk involvement, severity and perceived effectiveness of protective behaviour across the eight occupational groups. Unlike the venue pattern found among sexually experienced women, sexually inexperienced women working in ‘stalls’ or ‘domestic service’ tended to perceive higher (compared to mean) peer risk involvement, less severity of HIV/STD infection, and less effectiveness of protective behaviour.
Association of workplace with HIV-related sexual behaviours and perceptions
Homogeneity of regression was established for all steps and no violation of homogeneity was found. MANCOVA results are presented in Table IV. For sexually experienced women, after adjusting for age, education attainment and income, workplace was significantly related to HIV-related sexual behaviours and perceptions (F(56,3934) = 1.78, p < 0.001). Specifically, workplace had significant association with risk sexual behaviours (p < 0.001). The associations of workplace with protective sexual behaviour, peer risk involvement, positive expectancy of risk behaviour and severity of the disease were no longer significantly different in the multivariate analyses after adjusting for age, educational attainment, and income.
Table IV.
Association of workplace with HIV-related sexual behaviours and perceptions, adjusting for age, educational attainment and income (MANCOVA).
| Sexually experienced women
|
Non-sexually experienced women
|
|||
|---|---|---|---|---|
| Effect of Workplace | P value | Effect of workplace | P value | |
| Pillais Trace Multivariate test | F(56,3934) = 1.78 | <0.001 | F(42,4938) = 2.30 | <0.001 |
| Roy-Bargmann stepdown F tests | ||||
| Perceived peer risk involvement | F(7,563) = 1.93 | 0.06 | F(7,823) = 6.86 | <0.001 |
| Risk sexual behaviour | F(7,562) = 4.81 | <0.001 | n/a | |
| Protective sexual behaviour | F(7,561) = 1.64 | 0.12 | n/a | |
| HIV/AIDS knowledge | F(7,560) = 1.70 | 0.11 | F(7,822) = 2.19 | 0.03 |
| Positive expectancy of risk behaviour | F(7,559) = 1.28 | 0.26 | F(7,821) = 0.70 | 0.67 |
| Severity of the disease | F(7,558) = 1.43 | 0.19 | F(7,820) = 1.80 | 0.08 |
| Perceived effectiveness of protective behaviour | F(7,557) = 0.86 | 0.54 | F(7,819) = 1.92 | 0.06 |
| Vulnerability to infection | F(7,556) = 0.77 | 0.61 | F(7,818) = 0.67 | 0.69 |
For sexually inexperienced women, the multivariate test was also significant (F(42,4938) = 1.95, p < 0.001). Workplace was found to be significantly related to HIV knowledge (p < 0.05) and perceptions of peer risk involvement (p < 0.001) after adjusting for age, educational attainment, and income.
Discussion
Our data indicate that workplace was significantly associated with HIV-related sexual behaviours and perceptions. For sexually experienced women, those working in entertainment establishments or personal service (e.g. massage parlours, dance halls, nightclubs, bars, barbershops, beauty salons, etc.) were more likely to engage in risk and protective sexual behaviours than women working in non-entertainment establishments (e.g., restaurants, factories, or domestic service, etc.). They also tended to have higher perceptions of both peer risk involvement and positive expectancy of risk behaviour, and lower perceptions of severity (univariate analyses). For sexually inexperienced women, the association of workplace with HIV-related perceptions existed as well. However, the venue pattern of perception differed from that for sexually experienced women. Sexually inexperienced women working in ‘stalls’ or ‘domestic service’ tended to have higher perceptions of peer risk involvement and lower perceptions of severity and perceived effectiveness of protective behaviour.
In the current study, nearly one-tenth of sexually experienced female migrant workers reported having exchanged sex for money, and nearly one-quarter reported having had multiple sexual partners. These rates are substantially higher than those among the general sexually active female population in China (around 1% and 4%, respectively) (Parish et al., 2003). This finding supports the perspective that female migrant workers in general are at higher risk of HIV/STD infection.
Nearly one-half of women working in the entertainment sector or personal service reported having sex with men with multiple sexual partners compared to only one-fifth to one-third of those in the non-entertainment establishments. Future prevention intervention activities among women should seek to heighten awareness of personal vulnerability through their sexual partner’s risk behaviours.
Consistent condom use was low in all the eight groups; similar findings have been reported among different subpopulations in China (UNAIDS, 2003b). Although consistent condom use rates were relatively higher among women in ‘hair salons’, ‘massage parlours’, ‘nightclubs’, and ‘hotels’, their condom use was inadequate given their greater involvement in sexual risk behaviours. Further study is needed to examine condom use with different types of sexual partners and reasons for non-use, and to design intervention efforts seeking to increase condom use among migrant women.
Women working in ‘hair salons’, ‘massage parlours’ and ‘nightclubs’ were more likely to report sexual risk behaviours and risk perceptions than women working in other sections. While this cross-sectional study cannot determine causality, it is possible that the workplace environment encouraged these sexual risk associations. First, women in these establishments have direct personal exposure to the local population, which may provide a greater chance for engaging in sexual activities. Second, with commercial sex reemerging in China, some establishments of these types have started to provide illegal sexual services and are gradually emerging as places for sex trading (Rogers et al., 2002; Liao et al., 2003; Pan, 1999). Young women working in such establishments may be identified as commercial sex workers regardless of the accuracy of such perceptions, so that they may often encounter sexual advances, expectations or harassment. Third, the legitimate wage which many of these women are earning is frequently inadequate to cover basic living needs. HIV intervention strategies among female migrant workers should therefore be responsive to the varying demands of their work. Given the potential risk factors related to employment type, it is necessary to include HIV/STD preventive knowledge and skills as part of their job training, especially for those working in entertainment or personal service establishments. Employers and/or managers (e.g. gatekeepers) of the establishments should be included in intervention efforts as well. Free or affordable condoms may be provided in their workplace. Policy makers should be educated about the benefits of guaranteeing a minimal income for female migrant workers that allows for a better-than subsistence existence.
Limitation
Several limitations of the current study should be addressed. First, respondents were not selected randomly, since about half of all migrants are not listed in government registers in the urban areas (Zhang, 2000). Therefore, a valid random sampling frame is not available. While efforts have been taken in recruitment to ensure the representativeness of the sample, caution is needed when generalizing results to the entire female migrant populations in Beijing and Nanjing. Second, our sample was from Beijing and Nanjing, the two major metropolitan areas in China. Since local policies and economic development vary substantially across areas in China, services and social context of each type of work setting may vary by areas. Therefore, the venue pattern found in the current study may not reflect the situation in other areas of China, particularly, townships or small cities. Third, data collection was based on self-report. Sensitive questions regarding personal sexual behaviours may be underreported due to fear of disclosure of their sexual risk behaviours. However, such bias in self-reporting may not affect the occupational pattern found in the study since there is no reason to suspect that the rates of under-reporting significantly vary by the occupational clusters.
Implication
Given the wide variation in sexual risk associated with worksite, intervention strategies should be tailored to address occupational-related factors. Activities focusing on increasing their ability to identify and avoid potential risk situations and to increase their ability to resist sexual advances and/or to negotiate condom use should be included in work orientation. A relevant policy is needed to guarantee at least minimum wages for migrant workers in urban cities. Further studies on the social context of their work, such as the characteristics of clients and owners’ attitudes toward HIV prevention and regulations in the establishments, are needed for a better understanding of these issues and for development of effective venue-specific intervention strategies.
Acknowledgments
The study is funded by NIMH/NIH (grant number R01MH64878). The authors would like to thank our participating investigators at Beijing Normal University Institute of Developmental Psychology, Nanjing University Institute of Mental Health and West Virginia University School of Medicine for their contributions to questionnaire development and data collection.
References
- Anderson AF, Qingsi Z, Hua X, Jianfeng B. China’s floating population and the potential for HIV transmission: a social-behavioural perspective. AIDS Care. 2003;15:177–185. doi: 10.1080/0954012031000068326. [DOI] [PubMed] [Google Scholar]
- Detels R, Wu Z, Rotheram MJ, Li L, Guan J, Yin Y, Liang G, Lee M, Hu L The National Institute of Mental Health (NIMH) Collaborative HIV Prevention Trial Group. Sexually transmitted disease prevalence and characteristics of market vendors in eastern China. Sexually Transmitted Diseases. 2003;30:803–808. doi: 10.1097/01.OLQ.0000086607.82667.CF. [DOI] [PubMed] [Google Scholar]
- Feng W, Zuo X, Ruan D. Rural migrants in Shanghai: living under the shadow of socialism. The International Migration Review. 2002;36:520–545. [Google Scholar]
- Ford K, Wirawan DN, Fajans P. Factors related to condom use among four groups of female sex workers in Bali, Indonesia. AIDS Education and Prevention. 1998;10:34–45. [PubMed] [Google Scholar]
- Ford K, Wirawan DN, Fajans P, Meliawan P, MacDonald K, Thorpe L. Behavioural interventions for reduction of sexually transmitted disease/HIV transmission among female commercial sex workers and clients in Bali, Indonesia. AIDS. 1996;10:213–222. doi: 10.1097/00002030-199602000-00013. [DOI] [PubMed] [Google Scholar]
- Hope KR., snr Mobile workers and HIV/AIDS in Botswana. AIDS Analysis Africa. 2000;10:6–7. [PubMed] [Google Scholar]
- Jackson L, Highcrest A, Coates RA. Varied potential risks of HIV infection among prostitutes. Social Science Medicine. 1992;35:281–286. doi: 10.1016/0277-9536(92)90024-k. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, Winett RA, Kalichman SC the Community HIV Prevention Research Collaborative. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. The Lancet. 1997;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- Liao S, Schensul J, Wolffers I. Sex-related health risks and implications for interventions with hospitality women in Hainan, China. AIDS Education and Prevention. 2003;15:109–121. doi: 10.1521/aeap.15.3.109.23834. [DOI] [PubMed] [Google Scholar]
- Li X, Fang X, Lin D, Mao R, Wang J, Cottrell L, Harris C, Stanton B. HIV/STD risk behaviours and perceptions among rural-to-urban migrants in China. AIDS Education and Prevention. 2004;16:538–556. doi: 10.1521/aeap.16.6.538.53787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, Sweat MD, Gittelsohn J, Abdool Karim SS. The impact of migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sexually Transmitted Diseases. 2003;30:149–156. doi: 10.1097/00007435-200302000-00011. [DOI] [PubMed] [Google Scholar]
- Mgalla Z, Pool R. Sexual relationships, condom use and risk perception among female bar workers in north-west Tanzania. AIDS Care. 1997;9:407–416. doi: 10.1080/713613167. [DOI] [PubMed] [Google Scholar]
- Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: Replication of an HIV preventive intervention. American Journal of Community Psychology. 1998;26:97–131. doi: 10.1023/a:1021886208524. [DOI] [PubMed] [Google Scholar]
- Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behaviour: a meta-analytic review of protection motivation theory. Journal of Applied Social Psychology. 2000;30:106–143. [Google Scholar]
- Pan SM. Reality and absurdity – Underground sex industry in China. Beijing: Qun Yan Publishing House; 1999. [Google Scholar]
- Parish WL, Laumann EO, Cohen MS, Pan S, Zheng H, Hoffman I, Wang T, Ng KH. Population-based study of Chlamydial infection in China: a hidden epidemic. Journal of American Medical Association. 2003;289:1265–1273. doi: 10.1001/jama.289.10.1265. [DOI] [PubMed] [Google Scholar]
- Roberts KD. China’s ‘tidal wave’ of migrant labor: what can we learn from Mexican undocumented migration to the United States? International Migration Review. 1997;31:2–39. [PubMed] [Google Scholar]
- Rogers RW. Cognitive and physiological processes in fear appraisals and attitude change: A revised theory of protection motivation. In: Cacioppi T, Petty RE, editors. Social Psychology. New York: Guilford Press; 1983. pp. 153–176. [Google Scholar]
- Rogers SJ, Liu Y, Yan TX, Fung K, Kaufman J. Reaching and identifying the STD/HIV risk of sex workers in Beijing. AIDS Education and Prevention. 2002;14:217–227. doi: 10.1521/aeap.14.3.217.23892. [DOI] [PubMed] [Google Scholar]
- Settle E. China AIDS survey: Current overview of HIV/AIDS in China. 2003 Available at: http://www.casy.org/index.htm.
- Shen J, Huang Y. The working and living space of the ‘floating population’ in China. Asia Pacific Viewpoint. 2003;44(1):51–62. [Google Scholar]
- SPSS Inc. SPSS for Windows Release 11.5.0 (Standard Version) Chicago, IL: SPSS Inc; 2002. [Google Scholar]
- Tabachnick B, Fidell L. Multivariate analysis of variance and covariance. In: Tabachnick B, Fidell L, editors. Using multivariate statistics. Allyn & Bacon; Needham Heights, MA: 2001. pp. 322–390. [Google Scholar]
- Tang CS, Wong C, Lee AM. Gender-related psychosocial and cultural factors associated with condom use among Chinese married women. AIDS Education and Prevention. 2001;13:329–342. doi: 10.1521/aeap.13.4.329.21426. [DOI] [PubMed] [Google Scholar]
- Turmen T. Gender and HIV/AIDS. International Journal of Gynecology & Obstetrics. 2003;82:411–418. doi: 10.1016/s0020-7292(03)00202-9. [DOI] [PubMed] [Google Scholar]
- UNAIDS. A joint assessment of HIV/AIDS prevention, treatment and care in China. 2003a. [Google Scholar]
- UNAIDS. Condoms. 2003b Available at http://www.unaids.org/html/pub/Topics/Partnership-Menus/PDF/CHINAcondoms_en_pdf.pdf.
- Wan GH. Peasant flood in China: Internal migration and its political determinants. Third World Quarterly. 1995;16(2):173–196. doi: 10.1080/01436599550036086. [DOI] [PubMed] [Google Scholar]
- Xu C, Wu Z, Zhang Y. A study on HIV prevalence among rural to urban migrants. Selected Studies Presented on Symposium on AIDS Prevention and Control in China; Beijing. 1998. pp. 23–24. [Google Scholar]
- Zhang WM, Li XR, Ye LQ, Xie G, Hu Y. Migrant population in China. Reference for Economic Research. 1998;57:2–18. [Google Scholar]
- Zhang L. The interplay of gender, space and work in China’s floating population. In: Entwisle B, Henderson GE, editors. Re-drawing boundaries: work, households, and gender in China. Berkeley: University of California Press; 2000. pp. 171–196. [Google Scholar]
- Zheng Z, Zhou Y, Zheng L, Yang Y, Zhao D, Lou C, Zhao S. Sexual behaviour and contraceptive use among unmarried, young women migrant workers in five cities in China. Reproductive Health Matters. 2001;9:118–127. doi: 10.1016/s0968-8080(01)90015-1. [DOI] [PubMed] [Google Scholar]


