Abstract
OBJECTIVE
To investigate the prevalence of violence involving intimate partners among women visiting Canadian family practices and to assess participants’ attitudes toward future use of computer-assisted screening for violence and other health risks.
DESIGN
Self-report via written survey.
SETTING
Group family practice clinic in inner-city Toronto, Ont.
PARTICIPANTS
Women patients at least 18 years old who were fluent in English.
MAIN OUTCOME MEASURES
Responses to questions about violence selected from the Abuse Assessment Screen and the Partner Violence Screen. Participants’ attitudes toward computer-assisted screening as measured by the Computerized Lifestyle Assessment Scale (1 to 5) in the domains of benefits, privacy—barriers, interaction—barriers, and interest.
RESULTS
Responses were received from 202 patients, 144 of whom were in current or recent relationships and completed the section on intimate-partner violence (IPV). The overall prevalence of IPV in current or recent relationships was 14.6%. Emotional abuse was reported by 10.4%, threat of violence by 8.3%, and physical or sexual violence by 7.6% of respondents. Emotional abuse was significantly associated with threat of violence and physical or sexual violence (P≤.001). Analysis of responses to questions on computerized screening revealed that participants generally perceived it would have benefits (mean score 3.6) and were very interested in it (mean score 4.3). Those who reported experiencing IPV rated the benefits of computerized screening significantly higher than respondents without IPV experiences did (t2.3, df142, P < .05). Participants were “not sure” about barriers (mean score 3.0). Responses were similar in the 2 groups for the domains of interest, privacy—barriers, and interaction—barriers.
CONCLUSION
The high rate of IPV reported by women attending family practices calls for physicians to be vigilant. Future research should examine ways to facilitate physicians’ inquiry into IPV. The positive attitudes of our participants toward interactive computer-assisted screening indicates a need for more research in this area.
RÉSUMÉ
OBJECTIF
Déterminer la prévalence de la violence entre partenaires intimes chez les femmes qui consultent les établissements de médecine familiale au Canada et évaluer l’attitude des participantes concernant l’utilisation éventuelle d’un dépistage informatisé de la violence et des autres risques pour la santé.
TYPE D’ÉTUDE
Déclaration par l’intéressée dans une enquête par écrit.
CONTEXTE
Polycliniques de médecine familiale de quartiers défavorisés de Toronto, en Ontario.
PARTICIPANTS
Patientes de 18 ans et plus parlant couramment l’anglais.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Réponses à des questions concernant la violence, tirées des outils de dépistage suivants: Abuse Assessment Screen et Partner Violence Screen. Attitude des participantes concernant un dépistage informatisé, telle que mesurée par le Computerized Lifestyle Assessment Scale, en fonction des avantages, des obstacles à la confidentialité, des obstacles à l’interaction et de l’intérêt.
RÉSULTATS
Parmi les 202 réponses reçues, 144 provenaient de patientes qui étaient en relation de couple actuelle ou récente et qui avaient répondu à la section sur la violence entre partenaires intimes (VPI). La prévalence globale de la VPI chez les couples actuels ou récents était de 14,6%. Des sévices d’ordre affectif étaient rapportés par 10,4% des participantes, des menaces de violence par 8,3% et des sévices physiques ou sexuels par 7,6% des répondantes. On notait une association significative entre les sévices d’ordre affectif d’une part et les menaces de violence et sévices physiques ou sexuels d’autre part (P≤0,001). L’analyse des réponses aux questions sur le dépistage informatisé montre que la plupart des participantes croyaient que son utilisation serait avantageuse (score moyen de 3,6) et qu’elles se disaient très intéressées par cet outil (score moyen de 4,3). Celles qui ont répondu être victimes de VPI jugeaient le dépistage informatisé significativement plus avantageux que les autres répondantes (t = 2,3 pour 142 degrés de liberté, P < 0,05). Les participantes étaient «incertaine» pour ce qui est des obstacles (score moyen de 3,0). Les 2 groupes ont répondu de la même façon aux questions sur les obstacles à la confidentialité et les obstacles à l’interaction.
CONCLUSION
Le taux élevé de VPI rapporté par les femmes qui visitent les cliniques de médecine familiale doit amener le médecin à se montrer vigilant. Des études additionnelles sont indiquées pour trouver des façons d’aider le médecin à détecter les cas de VPI. L’opinion favorable des participantes envers le dépistage interactif informatisé indique que ce domaine mérite davantage de recherche.
Intimate partner violence (IPV) involves a pattern of coercion, physical abuse, sexual abuse, or threat of violence in intimate relationships.1 In 90% of cases, women are the victims of IPV.2,3 Such violence leads to high rates of death and injury4,5 and puts physical and mental health at risk.6–8 As a result, abused women frequently visit health care settings, such as emergency departments and family practices.9
According to a recent systematic review,10 the prevalence of physical or sexual IPV in primary care ranged from 12% to 29% for current experiences and 20% to 39% for lifetime experiences. This review, however, included only 3 studies on family practice patients,11–13 and none of the studies was Canadian. Generalizations to Canadian family practice from studies conducted in the United States or the United Kingdom could be inappropriate because of the growing diversity of Canada’s population under its broad immigration policy14 and the fact that familial stress could be particularly high among recent immigrants.15,16
Canadian family physicians need to know the prevalence of IPV among their own patients. A few Canadian studies have examined IPV in family practice, but only in relation to screening tools,17,18 screening rates,19–21 and physician-patient relationships.22 Other studies have reported on IPV prevalence among pregnant women.7,23 This lack of information might be part of the reason physicians often fail to ask their patients about IPV.24–27
The College of Family Physicians of Canada endorses inquiry into relationship issues by including it on the Preventive Care Checklist Form.28 The Canadian Task Force on Preventive Health Care emphasized the need for clinicians to have a high index of suspicion regarding IPV since the evidence required to recommend universal screening was still insufficient.29 Family physicians are in a unique position to inquire about IPV because of their focus on comprehensive care, health promotion, and early detection, and the ongoing nature of physician-patient relationships. These factors make family practice an appropriate setting for inquiring about and addressing IPV.
Violence involving intimate partners is known to be a socially sensitive issue even in health care settings. Abused women seldom open up spontaneously to physicians owing to feelings of shame, embarrassment, failure, and guilt; confidentiality concerns; and fear of physicians’ reactions or rejection.30–33 Nevertheless, asking about abuse is the strongest predictor of disclosure.31,34 Physicians often miss opportunities to discuss IPV due to lack of time, feeling uncomfortable, and fear of offending patients.24–27 These barriers have led to recent use of computer-based screening for IPV. Interactive, time-efficient computer programs generate health recommendations for patients and risk reports for physicians at point of care. Although these programs are effective in emergency departments for increasing patient disclosure and physicians’ detection of IPV,35–37 the attitudes of primary care patients to these programs have yet to be studied.
Our study had 2 objectives: first, to investigate the prevalence of IPV among female patients visiting a family practice clinic in Toronto, Ont, and second, to evaluate the attitudes of family practice patients toward future use of computer-assisted screening. We hypothesized that victims of IPV would have more positive attitudes toward such screening than non-victims would.
METHODS
Study design and site
Female patients visiting a busy, inner-city, group family practice clinic affiliated with a teaching hospital in Toronto were surveyed. Patients were eligible if they were at least 18 years old, fluent in English, and able to give informed consent. All physicians on-site were provided with A Handbook Dealing with Woman Abuse and the Canadian Criminal Justice System38 before the study. The study was approved by the Research Ethics Board of St Michael’s Hospital.
Recruitment
A brief invitation letter was placed in the medical charts of all adult female patients with booked appointments. The clinic receptionist gave the invitations to patients when they checked in. Patients were then approached in the waiting area by a recruiter. After confirming eligibility, patients were invited to learn about the study in a separate room where they would be unaccompanied by family members or friends. Willing participants provided written consent and completed the 7-minute written questionnaire before seeing their physicians. All participants received a health information package with telephone numbers of counselors and a help line for assaulted women.
Survey
The survey had 3 sections. One gathered information on sociodemographic and health-related variables (Table 1). The second asked about attitudes toward future use of computer-assisted screening. The third inquired about experiences of IPV. While the first and second sections applied to all participants, the IPV section applied only to those in current or recent intimate relationships. The term “intimate partner” referred to a spouse, common-law partner, girlfriend, or boyfriend. A recent relationship was defined as an intimate relationship of at least 2 months’ duration during the last year.
Table 1. Sociodemographic characteristics (N = 202): Mean age was 45.3 years (standard deviation [SD] 15.4).
On a scale of 1–5,* respondents rated their ability to speak English at a mean of 4.5 (SD .87) and their perceived health status at a mean of 3.2 (SD 1.0). They estimated the number of visits they made to family physicians at a mean of 4.6 (SD 4.2), and their comfort level with the survey on another scale of 1–5† at a mean of 4.0 (SD 1.2).
| VARIABLE | N | % |
|---|---|---|
| Marital status | 202 | |
| • Married or common-law | 54.6 | |
| • Separated, divorced, or widowed | 13.9 | |
| • Single, in current or recent relationship | 20.3 | |
| • Single, not in relationship | 11.4 | |
| Had children | 113 | 56.2 |
| Country of birth | 202 | |
| • Canada | 63.9 | |
| • Outside Canada | 36.1 | |
| If an immigrant, years lived in Canada | 71 | |
| • <10 | 23.9 | |
| • 10–20 | 16.9 | |
| • >20 | 59.2 | |
| If an immigrant, country of birth | 72 | |
| • Europe | 36.1 | |
| • East, southeast, or south Asia | 29.1 | |
| • West Indies, Latin America, Caribbean | 20.8 | |
| • Arabia, west Asia | 6.9 | |
| • Africa | 5.6 | |
| Education | 201 | |
| • Less than high school | 3 | |
| • High school, some or complete | 19.9 | |
| • University, some or complete | 55.7 | |
| • Postgraduate training, some or complete | 21.4 | |
| Employment status | 201 | |
| • Full-time | 49.8 | |
| • Part-time | 14.4 | |
| • Unemployed | 13.9 | |
| • Retired or on disability | 21.9 | |
| Household income ($) | 181 | |
| • <20 000 | 15.5 | |
| • 20 000–40 000 | 19.9 | |
| • 40 001–60 000 | 20.5 | |
| • >60 000 | 44.2 | |
| Access to a computer at home or at work | 200 | 87 |
Scale: 1—poor, 2—fair, 3—good, 4—very good, 5—excellent.
Scale: 1—very uncomfortable, 2—uncomfortable, 3—not sure, 4—comfortable, 5—very comfortable.
Experiences of IPV were assessed using questions derived from 2 prevalidated scales, the Abuse Assessment Screen39,40 and the Partner Violence Screen,41 along with questions recommended in A Resource Manual for Health Care Providers.42 The study’s definition of IPV included emotional and physical violence and threat of violence. Emotional IPV was measured by responses to 4 items: partner is jealous, tries to control life, tries to keep me away from family or friends, and says insulting things. Threat of IPV was assessed by responses to 2 items: fear of disagreeing with partner and feeling physically threatened by partner. Physical IPV was assessed by 2 items: being pushed, hit, kicked, or otherwise physically hurt and being forced to have unwanted sex. Patients responded “yes” or “no” to each item. We defined participants as IPV victims if they responded “yes” to at least 2 items on emotional violence or 1 item on threat of violence or physical violence.
Attitudes toward use of computer-assisted screening were assessed using the 14-item Computerized Lifestyle Assessment Scale (CLAS).43 Participants read a vignette about such screening and rated each item on a scale of 1 (strongly disagree) to 5 (strongly agree), 3 being “not sure.” We assessed the psychometric properties of the CLAS (details available from the authors). The 4 attitude domains of CLAS we used were benefits, which meant patient-perceived benefits for quality of medical consultation and the means of achieving them; privacy—barriers, which covered patients’ concerns about information privacy; interaction—barriers, which meant concerns about interference during interactions with physicians; and interest, which meant patients’ interest in computer-assisted health assessments. Along with using these prevalidated questions, we pilot-tested the questionnaire for simplicity and clarity of language.
Sample size
We aimed to recruit a convenience sample of 200 participants. For the IPV section, our final sample consisted of 144 participants. To calculate the adequacy of the sample size, we used power analysis44 with the lowest IPV prevalence previously reported (ie, 12%).10 A sample size of 144 generated 96% confidence for the 12% estimate with a margin of ± 5.
Statistical analyses
Our results are based on descriptive statistics (proportions and means) and 2-group comparisons using χ2, Student’s t test, and correlation analyses. Also, 95% confidence intervals (CI) were calculated for point estimates of IPV prevalence. Data were analyzed using the Statistical Package for the Social Sciences, version 13.
RESULTS
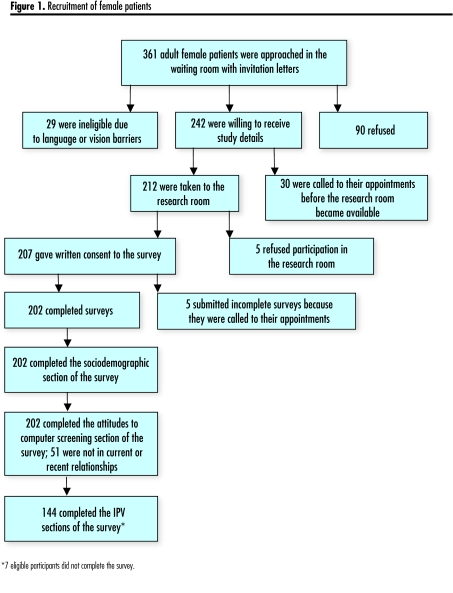
Of 212 patients receiving information on the study, 207 provided written consent to participate for a response rate of 97.6% (Figure 1). After excluding 5 incomplete surveys, we analyzed overall results for 202 patients and results from the IPV section for 144 patients.
Figure 1.
Recruitment of female patients
Sociodemographic characteristics
Participants had a mean age of 45 years (range, 19 to 86); 75% of them were in current or recent relationships (Table 1). About 36% were immigrants, and 59% of these had lived in Canada for more than 20 years. Most participants had at least some university education and were currently employed. They rated their health as “good” with a mean score of 3.2 (standard deviation ±1) on a scale of 1 to 5. They had visited family physicians during the past year a mean of 4.6 times (median 3.5, mode 1, range 0 to 30).
Experiences of IPV
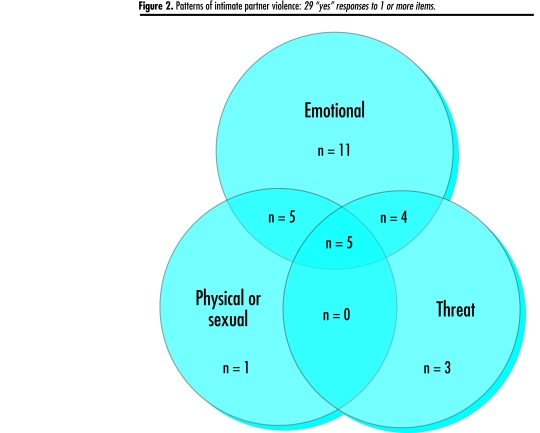
Of 144 respondents to the IPV section, 29 reported at least 1 experience of violence perpetrated by a current partner (18 women), recent partner (10 women), or current and recent partners (1 woman). Using our IPV case definition, the prevalence of emotional IPV was 10.4% (95% CI 5.4 to 15.4), threat of IPV was 8.3% (95% CI 3.8 to 12.8), and physical or sexual IPV was 7.6% (95% CI 3.3 to 11.9) (Table 2). Many patients who reported emotional IPV also reported threat of IPV (60%, Fisher’s exact test: P≤.001) or physical IPV (53%, Fisher’s exact test: P≤.001) (Figure 2). Counting IPV victims only once across 3 types of IPV gave an overall prevalence of 14.6% (95% CI 8.8 to 20.3).
Table 2. Responses to questions on intimate-partner violence in current or recent relationships (N = 144).
Overall, 21 respondents (prevalence was 14.6%) reported being victims of violence (victims were counted once across the 3 types of violence).
| QUESTIONS | N | % OF RESPONDENTS SAYING “YES” (95% CI) |
|---|---|---|
| Emotional violence* | ||
| • Is your partner very jealous? | 11 | 7.6 (3.3–11.9) |
| • Does your partner try to control your life? | 15 | 10.4 (5.4 to 15.4) |
| • Does your partner try to keep you away from family and friends? | 9 | 6.3 (2.3–10.3) |
| • Does your partner insult you or put you down? | 18 | 12.5 (7.1–18.0) |
| • Pooled responses of those saying “yes” to 2 or more Items in the emotional Domain | 10.4 (5.4–15.4) | |
| Threats | ||
| • Are you afraid to disagree with your partner? | 9 | 6.3 (2.3–10.3) |
| • Do you feel physically threatened by your partner? | 7 | 4.9 (1.4–8.4) |
| • Pooled responses of those saying “yes” to feelings of Threat | 8.3 (3.8–12.8) | |
| Physical or sexual violence | ||
| • Has your partner ever pushed, hit, kicked, or otherwise physically hurt you? | 8 | 5.6 (1.8–9.4) |
| • Has your partner ever forced you to have sex when you did not want to? | 8 | 5.6 (1.8–9.4) |
| • Pooled responses of those saying “yes” to any aspect Of physical or sexual Violence | 7.6 (3.3–11.9) | |
CI—confidence interval.
17.4% of respondents reported at least 1 experience of emotional violence (95% CI 11.2–23.6).
Figure 2.
Patterns of intimate partner violence: 29 “yes” responses to 1 or more items.
Comparison of victims and non-victims of IPV showed that victims had lower household incomes (t 2.1, df 131, P < .01), but were similar in other sociodemographic and health-related variables, including comfort level with completing the survey and Canadian-born versus immigrant status.
Attitudes toward use of computer-assisted screening
Overall, participants had positive attitudes toward computer-assisted screening (Table 3). On a scale of 1 to 5, participants agreed with the benefits of computer-assisted screening (mean score 3.6) and expressed interest in such programs (mean score 4.3). Participants were “not sure” about privacy barriers (mean score 3.1) and barriers to interaction with doctors (mean score 3.0). Victims of IPV thought computer-assisted screening had significantly higher benefits than non-victims did (t 2.3, df 142, P < .05); the 2 groups gave similar responses in the privacy—barriers, interaction—barriers, and interest domains of the CLAS.
Table 3. Patients’ attitudes toward computer-assisted screening.
Based on the Computerized Lifestyle Assessment Scale (CLAS) where 1—strongly disagree, 2—disagree, 3—not sure, 4—agree, and 5—strongly agree.
| CLAS ATTITUDE DOMAINS (CRONBACH’S α) | OVERALL RATINGS N = 202
|
RATINGS OF THOSE WHO ANSWERED THE SECTION ON IPV N = 144
|
|
|---|---|---|---|
| MEAN (SD) | THOSE NOT EXPERIENCING IPV MEAN (SD) | THOSE EXPERIENCING IPV MEAN (SD) | |
| Benefits*(.85) | 3.6 (.68) | 3.6 (.67) | 3.9 (.64) |
| Computers would help doctors with routine lifestyle questions, are a good way to ask lifestyle questions, would save doctors’ time, will help doctors make better assessments, would make patients feel comfortable answering questions, and can be trusted | |||
| Privacy—Barriers†(.81) | 3.1 (.82) | 3.1 (.73) | 3.1 (.77) |
| I would worry about confidentiality; I don’t want certain information about me on the computer; too many mistakes will be made on computers | |||
| Interaction—Barriers†(.80) | 3.0 (.82) | 2.9 (.74) | 2.8 (.76) |
| Doctors would spend less time with patients; doctors would lose the personal touch; I would find another Doctor | |||
| Interest†(.75) | 4.4 (.60) | 4.3 (.53) | 4.2 (.65) |
| I would answer honestly; I would want to read the patient information sheet |
IPV—intimate partner violence, SD—standard deviation.
Statistically significant difference between ratings of victims and non-victims of IPV (P < .05)
Adjusted reliability coefficient where each domain has 6 items.
DISCUSSION
This is one of the first Canadian studies to report on the prevalence of IPV among female patients visiting family physicians. If a family physician sees 150 patients a week, half of whom are women in relationships, our prevalence rate of 14.6% implies that a physician is likely to see 11 victims of IPV every week. Given this high prevalence and women’s reluctance to disclose,8,30–33 family physicians need to be highly vigilant to detect cases of IPV.
Family physicians could be pivotal in detecting IPV and offering empathy, support, and referral to helping agencies. Studies report that the risk of anxiety, depression, suicide attempts, and symptoms of posttraumatic stress disorder is much lower among women suffering from IPV if they have strong social support.45 Women who contacted advocacy services report that concerned nurses and physicians motivated them to seek help.46 Longitudinal research indicates that referral to specifically tailored counseling services benefits victims of abuse by helping them learn to reduce emotional or physical abuse and postpartum depression47,48 and improving their quality of life.49,50 Family physicians could empower abused women by promoting social support, self-worth, internal locus of control, decision making, and use of counseling services.
The women in our study, particularly those who were victims of IPV, had positive attitudes toward use of computer-assisted screening. Computer-based health-risk assessments provide a nonjudgmental, anonymous way of asking patients about socially sensitive health issues.51–53 This is especially important for abused women, as specific inquiries by health care providers give them permission to disclose.31 When completing computer surveys, patients are likely to learn more about and reflect on their risk before they see their physicians. Computer-generated risk reports allow physicians to shift their focus from screening to discussion.35,36 We anticipate that patients’ positive attitudes would lead to their acceptance and use of computer screening, in accordance with theories of health behaviour.54,55 Future research should examine the actual use of computer screening bypatients and providers, and assess its effectiveness in family practice.
Inquiring about emotional IPV is important. We found strong correlations between emotional and physical IPV. Traditionally, researchers and clinicians have focused on screening for physical violence, but emotional abuse is part of a larger pattern of domination and control. Emotional abuse precedes physical abuse56 or has consequences as damaging as physical abuse.57 Asking about emotional IPV would help in early detection and timely management of risk, so clinicians and health educators need to broaden their current definition of IPV.
Limitations
We acknowledge that our results might have limited generalizability because the study was conducted in only 1 clinic. This clinic, however, had several physicians on staff and served a large number of diverse patients who made an estimated 50 000 visits annually. Furthermore, we recruited patients making all types of health care visits at all kinds of clinic hours to increase generalizability. The study had a high response rate, and reassuringly, participants were similar to women residing in Toronto in terms of immigration and marital status.14 The results, therefore, can likely be generalized to similar Canadian urban family practices. Our rates of IPV, however, might underestimate the real magnitude due to under-reporting.31 In addition, we had only a few recent immigrants, which limited our ability to assess their vulnerability to IPV and attitudes toward computer-assisted screening.
Conclusion
The high rate of IPV among women in a family practice calls for physicians to be vigilant. Future research should examine ways to help physicians inquire into IPV and conflict in relationships. The positive attitudes of our participants toward interactive computer-assisted screening should encourage more research in this area.
Acknowledgment
The study contributed to doctoral and fellowship training of Farah Ahmad, funded by the Canadian Institute of Health Research, Institute of Gender and Health, and Ontario’s Women’s Health Council. We thank the Centre for Research on Inner City Health. We also thank Harvey A. Skinner, thesis advisor, and Richard H. Glazier, family physician and scientist, for their conceptual contributions, and Maureen Kelly, Program Manager, and Brenda McDowell,family physician, for their collaboration.
EDITOR’S KEY POINTS
According to a recent systematic review, the prevalence of physical and sexual violence involving intimate partners seen in primary care ranged from 12% to 29% for current relationships and 20% to 39% for lifetime relationships. Generalizing these numbers to Canadian family physicians’ experience, however, might be inappropriate.
This study had 2 objectives: to investigate the prevalence of intimate-partner violence among female patients visiting a family practice clinic in Toronto, Ont, and to evaluate patients’ attitudes toward future use of computer-assisted screening for victims of violence.
Overall prevalence of intimate-partner violence in current or recent relationships was 14.6%. Emotional abuse was reported by 10.4%, threat of violence by 8.3%, and physical or sexual violence by 7.6% of respondents.
POINTS DE REPÈRE DU RÉDACTEUR
Selon une revue systématique récente, la prévalence des sévices physiques ou sexuels entre partenaires intimes observée dans le contexte des soins de première ligne varie de 12 à 29% pour les relations de couple actuelles et de 20 à 39% pour les relations à long terme. Ces chiffres pourraient toutefois ne pas correspondre à l’expérience des médecins de famille canadiens.
Cette étude poursuivait 2 objectifs: établir la prévalence de la violence entre partenaires intimes chez des patientes visitant une clinique de médecine familiale de Toronto, en Ontario, et évaluer l’opinion de ces femmes sur l’utilisation éventuelle d’un outil informatisé pour le dépistage des victimes de violence.
La prévalence globale de violence entre partenaires intimes dans les cas de relations actuelles ou récentes était de 14,6%. Des sévices d’ordre affectif ont été rapportés par 10,4% des répondantes, des menaces de violence par 8,3% et des sévices physiques ou sexuels par 7,6%.
Footnotes
This article has been peer reviewed.
Contributors: All the authors made substantial contributions to concept and design of the study, interpretation of data, and critical revision of the article for intellectual content, and gave final approval to the version to be published. Dr Ahmad also coordinated collection of data and conducted analyses. Dr Hogg-Johnson provided feedback on the statistics. Drs Ahmad and Levinson take responsibility for the integrity of the work as a whole from inception to published article.
Competing interests
None declared
References
- 1.Krugg EG, Dahlberg LL, Mercy JA, Zwi A, Lozano R, editors. Violence—a global public health approach. World report on violence and health. Geneva, Switz: World Health Organization; 2002. pp. 3–21. [Google Scholar]
- 2.Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women. 2000;6(2):142–61. [Google Scholar]
- 3.Eisenstat SA, Bancroft L. Domestic violence. N Engl J Med. 1999;341(12):886–92. doi: 10.1056/NEJM199909163411206. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Canada. Family violence in Canada: a statistical profile 2005. Ottawa, Ont: Statistics Canada; 2005. Report no. 85–224-XIE. [Google Scholar]
- 5.United States Department of Justice. Intimate partner violence, 1993–2001. Washington, DC: US Department of Justice; 2003. Report no. NCJ-197838. [Google Scholar]
- 6.Plichta S. The effects of woman abuse on health care utilization and health status: a literature review. Womens Health Issues. 1992;2(3):154–63. doi: 10.1016/s1049-3867(05)80264-6. [DOI] [PubMed] [Google Scholar]
- 7.Stewart DE, Cecutti A. Physical abuse in pregnancy. CMAJ. 1993;149(9):1257–63. [PMC free article] [PubMed] [Google Scholar]
- 8.Plichta SB, Falik M. Prevalence of violence and its implications for women’s health. Womens Health Issues. 2001;11(3):244–58. doi: 10.1016/s1049-3867(01)00085-8. [DOI] [PubMed] [Google Scholar]
- 9.Wathen CN, MacMillan HL. Interventions for violence against women: scientific review. JAMA. 2003;289(5):589–99. doi: 10.1001/jama.289.5.589. [DOI] [PubMed] [Google Scholar]
- 10.Naumann P, Langford D, Torres S, Campbell J, Glass N. Women battering in primary care practice. Fam Pract. 1999;16(4):343–52. doi: 10.1093/fampra/16.4.343. [DOI] [PubMed] [Google Scholar]
- 11.Martin R, Holzapfel S, Baker P. Wife abuse: are we detecting it? J Womens Health. 1992;1:77–80. [Google Scholar]
- 12.Elliot BA, Johnson MM. Domestic violence in a primary care setting: patterns and prevalence. Arch Fam Med. 1995;4:113–9. doi: 10.1001/archfami.4.2.113. [DOI] [PubMed] [Google Scholar]
- 13.Hamberger LK, Saunders DG, Hovey M. Prevalence of domestic violence in community practice and rate of physician inquiry. Fam Med. 1992;24:283–7. Erratum in: Fam Med 1992;24:568. [PubMed] [Google Scholar]
- 14.Statistics Canada. Immigrant population by place of birth, by census metropolitan areas (2001 census) Ottawa, Ont: Statistics Canada; 2005. [Accessed 2006 January 25]. Available from: http://www.statcan.ca/english/Pgdb/demo47a.htm. [Google Scholar]
- 15.Cohen MM, Maclean H. Violence against Canadian women. BMC Womens Health. 2004;4(Suppl 1):S1–22. doi: 10.1186/1472-6874-4-S1-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmad F, Ali M, Stewart DE. Spousal-abuse among Canadian immigrant women. J Immigr Health. 2005;7(4):239–46. doi: 10.1007/s10903-005-5120-4. [DOI] [PubMed] [Google Scholar]
- 17.Brown JB, Lent B, Brett PJ, Sas G, Pederson LL. Development of the Woman Abuse Screening Tool for use in family practice. Fam Med. 1996;28:422–8. [PubMed] [Google Scholar]
- 18.Brown JB, Lent B, Schmidt G, Sas G. Application of the Woman Abuse Screening Tool (WAST) and WAST-short in the family practice setting. J Fam Pract. 2000;49(10):896–903. [PubMed] [Google Scholar]
- 19.Haley N, Maheux B, Rivard M, Gervais A. Lifestyle health risk assessment: do recently trained family physicians do it better? Can Fam Physician. 2000;46:1609–16. [PMC free article] [PubMed] [Google Scholar]
- 20.Ferris LE, Tudiver F. Family physicians’ approach to wife abuse: a study of Ontario, Canada, practices. Fam Med. 1992;24:276–82. [PubMed] [Google Scholar]
- 21.Ferris LE. Canadian family physicians’ and general practitioners’ perceptions of their effectiveness in identifying and treating wife abuse. Med Care. 1994;32(12):1163–72. doi: 10.1097/00005650-199412000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Woolhouse S, Brown JB, Lent B. Women marginalized by poverty and violence. How patient-physician relationships can help. Can Fam Physician. 2004;50:1388–94. [PMC free article] [PubMed] [Google Scholar]
- 23.Carroll JC, Reid AJ, Biringer A, Midmer D, Glazier RH, Wilson L, et al. Effectiveness of the Antenatal Psychosocial Health Assessment (ALPHA) form in detecting psychosocial concerns: a randomized controlled trial. CMAJ. 2005;173:253–7. doi: 10.1503/cmaj.1040610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sugg KN, Inui T. Primary care physicians’ response to domestic violence. Opening Pandora’s box. JAMA. 1992;267(23):3157–60. [PubMed] [Google Scholar]
- 25.Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse. JAMA. 1999;282(5):468–74. doi: 10.1001/jama.282.5.468. [DOI] [PubMed] [Google Scholar]
- 26.Garimella R, Plichta SB, Houseman C, Garzon L. Physician beliefs about victims of spouse abuse and about the physician role. J Womens Health Gender Based Med. 2000;9(4):405–11. doi: 10.1089/15246090050020727. [DOI] [PubMed] [Google Scholar]
- 27.Jaffee KD, Epling JW, Grant W, Ghandour RM, Callendar E. Physician-identified barriers to intimate partner violence screening. J Womens Health. 2005;18:713–20. doi: 10.1089/jwh.2005.14.713. [DOI] [PubMed] [Google Scholar]
- 28.Dubey V, Mathew R, Glazier R, Iglar K. The Evidence-Based Preventive Care Checklist Form. Mississauga, Ont: College of Family Physicians of Canada; 2004. [Accessed 2005 December 23]. Available from: http://www.cfpc.ca. [Google Scholar]
- 29.Wathen CN, MacMillan HL Canadian Task Force on Preventive Health Care. Prevention of violence against women: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2003;169:582–4. [PMC free article] [PubMed] [Google Scholar]
- 30.Bauer HM, Rodriguez MA, Quiroga SS, Flores-Ortiz YG. Barriers to health care for abused Latina and Asian immigrant women. J Health Care Poor Underserved. 2000;11(1):33–44. doi: 10.1353/hpu.2010.0590. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez MA, Sheldon WR, Bauer HM, Perez-Stable EJ. The factors associated with disclosure of intimate partner abuse to clinicians. J Fam Pract. 2001;50(4):338–44. [PubMed] [Google Scholar]
- 32.Plichta S, Duncan M, Plichta L. Spousal abuse, patient-physician communication and patient satisfaction. Am J Prev Med. 1996;12(5):297–303. [PubMed] [Google Scholar]
- 33.Feder G, Huston M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med. 2006;166(1):22–37. doi: 10.1001/archinte.166.1.22. [DOI] [PubMed] [Google Scholar]
- 34.Titus K. When physicians ask, women tell about domestic abuse and violence. JAMA. 1996;275(24):1863–5. [PubMed] [Google Scholar]
- 35.Rhodes KV, Lauderdale DS, Stocking CB, Howes DS, Roizen MF, Levinson W. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37(3):284–91. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]
- 36.Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire”. Ann Emerg Med. 2002;40(5):476–84. doi: 10.1067/mem.2002.127181. [DOI] [PubMed] [Google Scholar]
- 37.Rhodes KV, Drum M, Anliker E, Frankel RM, Howes DS, Levinson W. Lowering the threshold for discussions of domestic violence: a randomized controlled trial of computer screening. Arch Intern Med. 2006;166(10):1107–14. doi: 10.1001/archinte.166.10.1107. [DOI] [PubMed] [Google Scholar]
- 38.Ferris LE, Nurani A, Silver L. A handbook dealing with woman abuse and the Canadian criminal justice system. Guidelines for physicians. Ottawa, Ont: Family Violence Prevention Unit, Health Canada; 1999. Report no. H72–21/164–1998E. [Google Scholar]
- 39.McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267(23):3176–8. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 40.Norton LB, Peipert JF, Zierler S, Lima B, Hume L. Battering in pregnancy: an assessment of two screening methods. Obstet Gynecol. 1995;85(3):321–5. doi: 10.1016/0029-7844(94)00429-H. [DOI] [PubMed] [Google Scholar]
- 41.Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA. 1997;277(17):1357–61. [PubMed] [Google Scholar]
- 42.Warshaw C, Ganley AL. Improving the health care response to domestic violence: a resource manual for health care providers. 2. San Francisco, Calif: Family Violence Prevention Fund; 1996. [Google Scholar]
- 43.Skinner HA. Early identification of addictive behaviors using computerized life-style assessment. In: Baer JS, Marlatt GA, McMahon RJ, editors. Addictive behaviors across the lifespan. Prevention, treatment and policy issues. Newbury Park, Calif: Sage; 1993. pp. 89–110. [Google Scholar]
- 44.Hintze JL. PASS 2002 user’s guide. Kaysville, Utah: National Council for the Social Studies; 2002. [Google Scholar]
- 45.Coker AL, Smith PH, Thompson MP, McKeown RE, Bethea L, Davis KE. Social support protects against the negative effects of partner violence on mental health. J Womens Health Gender Based Med. 2002;11(5):465–76. doi: 10.1089/15246090260137644. [DOI] [PubMed] [Google Scholar]
- 46.Gerbert B, Abercrombie P, Caspers N, Love C, Bronstone A. How health care providers help battered women: the survivor’s perspective. Womens Health. 1999;29:115–35. doi: 10.1300/J013v29n03_08. [DOI] [PubMed] [Google Scholar]
- 47.Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Res Nurs Health. 1999;22:59–66. doi: 10.1002/(sici)1098-240x(199902)22:1<59::aid-nur7>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 48.Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomized controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOC. 2005;112(9):1249–56. doi: 10.1111/j.1471-0528.2005.00709.x. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan CM, Bybee DI. Reducing violence using community-based advocacy for women with abusive partners. J Consult Clin Psychol. 1999;67(1):43–53. doi: 10.1037//0022-006x.67.1.43. [DOI] [PubMed] [Google Scholar]
- 50.Bybee D, Sullivan CM. Predicting re-vitimization of battered women 3 years after exiting a shelter program. Am J Community Psychol. 2005;36(1/2):85–96. doi: 10.1007/s10464-005-6234-5. [DOI] [PubMed] [Google Scholar]
- 51.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behaviour, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 52.Locke SE, Kowaloff HB, Hoff RG, Safran C, Popovsky MA, Cotton DJ, et al. Computer-based interview for screening blood donors for risk of HIV transmission. JAMA. 1992;268(10):1301–5. [PubMed] [Google Scholar]
- 53.Skinner HA, Allen BA, McIntosh MC, Palmer WH. Lifestyle assessment: applying microcomputers in family practice. BMJ. 1985;290:212–6. doi: 10.1136/bmj.290.6463.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education. San Francisco, Calif: Jossey-Bass Inc; 1997. pp. 60–84. [Google Scholar]
- 55.Strecher VJ, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education. 2. San Francisco, Calif: Jossey-Bass Inc; 1997. pp. 41–59. [Google Scholar]
- 56.O’Leary KD. Psychological abuse: a variable deserving critical attention in domestic violence. Violence Vict. 1999;14(1):3–23. [PubMed] [Google Scholar]
- 57.Sackett LA, Saunders DG. The impact of different forms of psychological abuse on battered women. Violence Vict. 1999;14(1):105–19. [PubMed] [Google Scholar]