Abstract
OBJECTIVE
To determine whether the canalith repositioning maneuver (CRM) is effective for treating benign paroxysmal positional vertigo when it is used by family physicians in primary care settings.
DESIGN
Randomized, prospective, double-blind, sham-controlled trial.
SETTING
An academic family practice in Hamilton, Ont.
PARTICIPANTS
Eighty-one patients 18 years or older whose dizziness was confirmed by the Dix-Hallpike (DH) vertigo-triggering maneuver and who had no contraindications to the CRM.
INTERVENTIONS
At the first visit, the intervention group received the CRM and the control group received a sham maneuver. Both groups received the CRM at the second and third visits 1 and 2 weeks later.
MAIN OUTCOME MEASURES
Negative results of the DH test or self-reported resolution of vertigo after the initial treatment.
RESULTS
Eighty-one patients were randomized and received the first treatment. After the first treatment, 34.2% of patients in the intervention group and 14.6% of patients in the control group had negative DH test results (relative risk 2.3, 95% confidence interval 1.03 to 5.2, P = .04); and 31.6% of patients in the intervention group and 24.4% of patients in the control group reported resolution of dizziness (relative risk 1.2, 95% confidence interval 0.7 to 1.9, P = .48). One week later, patients in both intervention and control groups received the CRM, and 61.8% and 57.1% of them, respectively, had negative DH test results (P = .81). By week 3, approximately 75% of patients in both groups had improved.
CONCLUSION
A statistically significant proportion of patients in the CRM group returned to a negative response to the DH maneuver immediately after the first treatment. Family physicians can use the CRM to treat benign paroxysmal positional vertigo and potentially avoid delays in treatment and unnecessary referrals.
TRIAL REGISTRATION NUMBER
NCT00182273 (ClinicalTrials.gov)
RÉSUMÉ
OBJECTIF
Déterminer si la manœuvre de déplacement de la canalolithiase (MDC) est efficace pour traiter le vertige positionnel paroxystique bénin, quand elle est exécutée par des médecins de famille en milieu de soins de première ligne.
CONCEPTION
Étude prospective randomisée avec groupe témoin fictif, à double insu.
CONTEXTE
Une pratique familiale universitaire à Hamilton, en Ontario.
PARTICIPANTS
Quelque 81 patients de 18 ans et plus dont les étourdissements étaient confirmés à l’aide de la manœuvre de déclenchement du vertige Dix-Hallpike (DH) et chez qui il n’était pas contre-indiqué d’exécuter la manœuvre.
INTERVENTIONS
À la première visite, le groupe d’intervention subissait une MDC et le groupe témoin faisait l’objet d’une manœuvre fictive. On effectuait ensuite la MDC chez les deux groupes lors d’une deuxième et d’une troisième visites, 1 et 2 semaines plus tard.
PRINCIPALES MESURES DES RÉSULTATS
Des résultats négatifs à l’épreuve DH ou la disparition du vertige signalée par l’intéressé à la suite du premier traitement.
RÉSULTATS
On a divisé les 81 patients en deux groupes au hasard et ils ont reçu leur premier traitement. Après le premier traitement, 34,2% des patients dans le groupe d’intervention et 14,6% des patients dans le groupe témoin ont obtenu des résultats négatifs à l’épreuve DH (risque relatif 2,3, intervalle de confiance à 95% de 1,03 à 5.2, P = .04); et 31,6% des patients dans le groupe d’intervention et 24,4% des patients du groupe témoin signalaient la disparition de leurs étourdissements (risque relatif 1,2, intervalle de confiance à 95% de 0,7 à 1,9, P = .48). Une semaine plus tard, les patients dans le groupe d’intervention et dans le groupe témoin ont fait l’objet de la MDC et 61,8%et 57,1% ont obtenu respectivement des résultats négatifs à l’épreuve DH (P = .81). À la troisième semaine, le problème d’environ 75% des patients dans les deux groupes s’était amélioré.
CONCLUSION
Une proportion statistiquement significative des patients dans le groupe ayant subi une MDC a obtenu des résultats négatifs au test de la manœuvre DH immédiatement après le premier traitement. Les médecins de famille peuvent utiliser la MDC pour traiter le vertige positionnel paroxystique bénin et ainsi éviter des délais dans le traitement et des demandes de consultation inutiles.
NUMÉRO D’ENREGISTREMENT DE L’ÉTUDE
NCT00182273 (ClinicalTrials.gov)
Benign paroxysmal positional vertigo (BPPV) is a common cause of peripheral vertigo.1 Its patho-physiology is consistent with a vestibular disorder in which floating particles in the posterior semicircular canals activate the hair cell receptors and disrupt endolymph flow.1
Estimates suggest that vertigo of undifferentiated cause accounts for 2.2% of patient complaints in primary care each year,2 and BPPV has been estimated to account for approximately 10% to 30% of these complaints.3,4 Prevalence is highest in the sixth decade, and BPPV is nearly twice as common among women as among men.3
Benign paroxysmal positional vertigo is usually transient. It frequently resolves spontaneously but frequently also recurs. Benign paroxysmal positional vertigo resolves spontaneously in one third to two thirds of untreated patients within 1 week to 1 month.5 Symptoms recur in up to 50% of patients within several years of treatment, and untreated patients have reported 3 to 20 exacerbations during up to 7 years of follow-up.5 The burden of illness of BPPV is considerable, owing to its disabling effects on patients’ lives and its unpredictable nature. There is evidence that, compared with patients, physicians underestimate its effect on quality of life.6 Deferred diagnosis and treatment, as a result of referrals to specialists, extends waiting times and engenders financial costs and the unnecessary use of prescribed medication known to be ineffective.5
The currently accepted treatment for BPPV is the canalith repositioning maneuver (CRM) described by Epley in 1992,7 in which particulate material is displaced away from the posterior semicircular canal using a 5-position cycle through which patients’ heads are moved sequentially. The CRM has demonstrated rates of improvement ranging from 67% to 89%.8 These studies, however, were carried out by otolaryngology, neurology, and internal medicine specialists.8 The effectiveness of CRM when carried out by family physicians was unknown.
The objective of this study was to test the CRM when carried out by trained family physicians in family practice. We conducted a randomized, prospective, double-blind, sham-controlled trial of the CRM, as described by Epley,7 for treatment of BPPV in family practice. Outcomes of interest were negative results on the diagnostic Dix-Hallpike (DH) test or self-reported resolution of vertigo.
METHODS
Setting and participants
Patients 18 years or older with vertigo were referred by community family physicians in the Hamilton, Ont, area to McMaster Family Practice in Hamilton between July 2001 and July 2005. The study was also advertised in various waiting areas of Hamilton hospitals and community practices, and patients were invited to participate. Patients were eligible if they reported positional vertigo and had positive unilateral results on the DH diagnostic maneuver.9 Patients with positive diagnoses of BPPV but evidence of ongoing central nervous system disease, otitis media, otosclerosis, inability to tolerate the diagnostic maneuver, severe degenerative disc disease of the cervical spine, or severe angina or hypertension were excluded.
All candidates for participation in the study provided written informed consent before being interviewed and assessed. The study was approved by the Research Ethics Committee of Hamilton Health Sciences.
Randomization and intervention
Eligible patients were randomly allocated by a concealed central randomization procedure to immediate intervention with the CRM or to a sham maneuver. The first treatment was administered at the baseline enrolment visit.
Three family physicians were involved in the project. All were male full-time faculty in the Department of Family Medicine at McMaster University in Hamilton with 5 to 30 years’ family practice experience. One (J.E.M.) had previously been a neurologist for 10 years. The other 2 physicians received a 1-hour training session from J.E.M. The physicians were also given an instruction manual on performing the maneuvers. For the first few patients, J.E.M. observed the newly trained physicians to ensure they were performing the maneuvers consistently. Data on these test patients were not included in the analyses.
One physician (J.T.M.), blinded to the treatment allocation group, administered the DH test to determine eligibility and administered the test again after the intervention to determine the effectiveness of the intervention; he did not carry out the intervention or sham maneuvers on any patients. Depending on availability at the time of patients’ visits, 1 of the other 2 physicians (J.E.M. or R.S.) administered the intervention or sham maneuver but did not assess any patients’ outcomes.
Outcome assessment for resolution of symptoms and the diagnostic DH test were conducted immediately after the intervention. Patients returned for subsequent treatments approximately 7 and 14 days later. Participants who received the sham maneuver at the first visit and CRM patients who still had symptoms or who had positive results of the DH test were given the CRM at the next 2 visits.
The CRM described by Epley7 is a 5-position cycle of the head and upper body aimed at displacing particulate matter away from the posterior semicircular canal. The patient sits on an examination table. The patient’s upper body is then moved to the supine position, with the head hanging over the end of the table and turned at a 45° angle with the affected side down. Then the hyper-extended head is rotated to the opposite side through a 90° angle until the unaffected side of the head is toward the floor. The patient is then rolled over onto that side so that his or her face is looking down at the floor. Finally, the patient is returned to the sitting position with the chin tilted down into the chest.10 Patients spend 1 minute in each of the 5 positions. The maneuver is applied to the side that had a positive result on the diagnostic DH test. The sham maneuver was the CRM performed on the non-affected side. After each treatment, patients in both groups were asked to rate their level of dizziness on a 10-point Likert-type scale from “same or worse” to “completely resolved.”
Statistical methods
The main outcomes were reversal of DH test results to negative after the first treatment or self-reported improvement in dizziness, defined as a score of 8 or higher on the 10-point scale.
Based on a between-group difference in the rate of resolution of 40% and a spontaneous rate of resolution of 30% to 50%, a sample size of 28 patients per group was required to detect a difference of 40% in self-reported resolution of symptoms or negative results of the DH test (2-tailed α of .05), with a power of 80%; P values for differences between proportions were calculated using the Fisher exact test (2-sided) and Intercooled Stata, version 8.1.
RESULTS
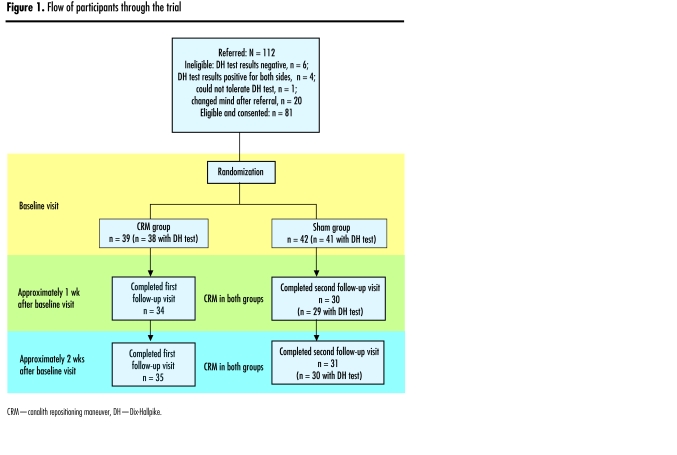
Figure 1 shows the flow of participants through the trial. Eighty-one patients were randomized and received the CRM or sham maneuver at the first visit. Thirty-four patients in the CRM group and 35 in the sham group completed the first follow-up 1 week later, and of these 69 patients, 59 completed the second follow-up 1 week after that.
Figure 1.
Flow of participants through the trial
Table 1 shows the baseline characteristics of patients in the 2 groups. The groups were similar except in sex and self-reported health. The CRM group was 81.6% (31/38) women; the sham group was 61.0% (25/41) women. In the CRM group, 28.9% (11/38) of patients reported fair or poor health, compared with 10.0% (4/40) in the sham group.
Table 1.
Characteristics of patients in the CRM and sham groups at baseline: Mean age of patients was 54.9 (17.5) years in the CRM group and 54.1 (15.3) years in the sham group; mean years since onset was 6.2 (5.9) in the CRM group and 6.0 (7.1) in the sham group.
| CHARACTERISTIC | CRM GROUP (N=38)* % (n/N) | SHAM GROUP (N=41)* % (n/N) |
|---|---|---|
| Female | 81.6 (31/38) | 61.0 (25/41) |
| First episode | 52.6 (20/38) | 40.0 (16/40) |
| Dizziness interferes with life a great deal | 29.7 (11/37) | 35.0 (14/40) |
| Fair or poor self- reported health | 28.9 (11/38) | 10.0 (4/40) |
CRM—canalith repositioning maneuver.
Divisors vary because of missing information.
After the first treatment at the baseline visit, 34.2% (13/38) of patients in the CRM group had negative results of the DH test, compared with 14.6% (6/41) in the sham group (relative risk [RR] for improvement 2.34, 95% confidence interval [CI] 1.03 to 5.33, P = .04) (Table 2). At that time, 31.6% (12/38) of intervention patients and 24.4% (10/41) of control patients reported their dizziness had resolved (RR 1.2, 95% CI 0.7 to 1.9, P = .48). After treatment at the follow-up visit 1 week later, 61.8% of CRM patients and 57.1% of control patients (also given CRM at this visit) had negative results of the DH test (RR 1.08, 95% CI 0.73 to 1.60, P = .81). By week 3, approximately 75% of patients in both groups had improved (Table 2).
Table 2.
Proportions of patients in the CRM group and the sham group who had negative DH test results or self-reported resolution of dizziness after treatments
| RESULTS | CRM GROUP% (n/N) | SHAM GROUP% (n/N) | P VALUE |
|---|---|---|---|
| TREATMENT 1 | |||
| DH test result negative | 34.2 (13/38) | 14.6 (6/41) | .04 |
| Dizziness resolved | 31.6 (12/38) | 24.4 (10/41) | .48 |
| Either resolved | 52.6 (20/38) | 36.6 (15/41) | .18 |
| TREATMENT 2 (both groups received CRM) | |||
| DH test result negative | 61.8 (21/34) | 57.1 (20/35) | .81 |
| Dizziness resolved | 40.0 (14/35) | 41.2 (14/34) | .92 |
| Either resolved | 73.5 (25/34) | 65.7 (23/35) | .48 |
| TREATMENT 3 (both groups received CRM) | |||
| DH test result negative | 75.0 (21/28) | 66.7 (20/30) | .55 |
| Dizziness resolved | 66.7 (20/30) | 67.7 (21/31) | .93 |
| Either resolved | 75.9 (22/29) | 76.7 (23/30) | .94 |
CRM—canalith repositioning maneuver, DH—Dix-Hallpike.
Divisors vary because of missing information.
Patients who completed follow-up assessment were more likely to report that BPPV interferes with their lives a great deal (50.8% versus 18.2%, P=.01) and to have had BPPV for fewer years on average (mean 5.5 years versus 11.5, P=.005 than patients who did not complete follow-up).
DISCUSSION
Results of our randomized, prospective, double-blind, sham-controlled trial of the effectiveness of the CRM in a primary care setting suggest that it is an appropriate and suitable procedure for treatment of BPPV in primary care. Results in this setting are comparable to those achieved by specialists.
A statistically significant proportion of patients in the CRM group returned to a negative response to the vertigo-triggering DH test immediately after the first treatment. In the subsequent weeks, when both groups received the active treatment, differences between groups were not significant due to improvements in the control group. In both groups, however, there was a cumulative increase in negative response to the DH test and in self-reported improvement in vertigo, suggesting repetitive application of the CRM at the second and third follow-up sessions might have maintained the beneficial effects observed after the first treatment. The apparent discordance between objective and subjective assessment of BPPV resolution has been reported previously; nearly one third of patients with negative DH test results have been reported to continue to have feelings of imbalance and vertigo.11
Limitations
A limitation of this study was that the CRM was performed by 3 family physicians in 1 academic practice, and the results need to be tested in other settings. Appropriate training of family physicians would be required before widespread use of the CRM. It was challenging to reach our recruitment target, as many people did not complete all 3 visits, likely because their symptoms resolved spontaneously or they improved after the first treatment. Although unlikely, it is possible that patients could have guessed their treatment group if they were familiar with the CRM and knew their affected side.
Conclusion
The improvement rates observed in our study after the first application of the CRM are within the range of those reported in otolaryngology, neurology, and internal medicine settings.8 We foresee 2 further directions for our research: training family physicians in the community and studying the clinical results derived from this training; and studying the effectiveness of the treatment when conducted by patients on themselves at home.
The results of this study and the innocuous nature of the CRM when basic clinical precautions have been taken support use of the CRM as first-line treatment for BPPV in primary care. Widespread use of the procedure by family physicians could benefit patients, avoid delays in treatment, and considerably reduce the number of referrals.
Acknowledgment
We dedicate this paper to the memory of Shawn Ling, our research assistant for the study. This study was funded by the Physicians’ Services Incorporated Foundation.
EDITOR’S KEY POINTS
Benign paroxysmal positional vertigo resolves spontaneously in one third to two thirds of untreated patients within 1 week to 1 month; symptoms recur in up to 50% of treated patients within several years.
Studies assessing the effectiveness of the canalith repositioning maneuver administered by specialists have shown improvement rates of 67% to 89% in patients with benign paroxysmal positional vertigo.
This study demonstrates that the canalith repositioning maneuver can be administered effectively by family physicians and that improvement can be seen within the first week.
POINTS SAILLANTS
Le vertige positionnel paroxystique bénin se règle spontanément chez un à deux tiers des patients non traités dans un délai d’une semaine à un mois; les symptômes reviennent chez jusqu’à 50% des patients traités dans les quelques années qui suivent.
Des études portant sur l’efficacité de la manœuvre de déplacement de la canalolithiase effectuée par des spécialistes ont démontré des taux d’amélioration de 67% à 89% chez les patients atteints de vertige positionnel paroxystique bénin.
Cette étude fait valoir que la manœuvre de déplacement de la canalolithiase peut être effectuée efficacement par les médecins de famille et que des améliorations peuvent être constatées en l’espace d’une semaine.
Footnotes
This article has been peer reviewed.
Drs Munoz, Miklea, and Kaczorowski contributed to study concept and design, collection and interpretation of data, and preparing the article for submission. Dr Springate contributed to collection and interpretation of data and preparing the article for submission. Ms Howard contributed to analysis and interpretation of data and preparing the article for submission.
Competing interests
None declared
References
- 1.Lanska DJ, Remler B. Benign paroxysmal positional vertigo: classic description, origins of the provocative positioning technique, and conceptual developments. Neurology. 1997;48:1167–77. doi: 10.1212/wnl.48.5.1167. [DOI] [PubMed] [Google Scholar]
- 2.Bird JC, Beynon GJ, Prevost AT, Baguely DM. An analysis of referral patterns for dizziness in the primary care setting. Br J Gen Pract. 1998;48:1828–32. [PMC free article] [PubMed] [Google Scholar]
- 3.Kentala E. Characteristics of six otological diseases involving vertigo. Am J Otol. 1996;17:883–92. [PubMed] [Google Scholar]
- 4.Madlon-Kay D. Evaluation and outcome of the dizzy patient. Fam Pract. 1985;21:109–13. [PubMed] [Google Scholar]
- 5.Sakaida M, Takeuchi K, Ishinaga H, Adachi M, Majima Y. Long-term outcome of benign paroxysmal positional vertigo. Neurology. 2003;60:1532–4. doi: 10.1212/01.wnl.0000061477.03862.4d. [DOI] [PubMed] [Google Scholar]
- 6.Honrubia V, Bell TS, Harris MR, Baloh RW, Fisher LM. Quantitative evaluation of dizziness characteristics and impact on quality of life. Am J Otol. 1996;17:595–602. [PubMed] [Google Scholar]
- 7.Epley JM. The canalith repositioning procedure for treatment of benign paroxysmal positioning vertigo. Otolaryngol Head Neck Surg. 1992;107:399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 8.Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2004;(2):CD003162. doi: 10.1002/14651858.CD003162.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Hain TC. Dix-Hallpike test. Chicago, Ill: Northwestern University; 2006. [Accessed 2007 April 24]. Available from: www.dizziness-and-balance.com/disorders/bppv/dix%20hallpike.htm. [Google Scholar]
- 10.Hain TC. The Epley maneuver. Chicago, Ill: Northwestern University; 1998. [Accessed 2007 April 24]. Available from: www.dizziness-and-balance.com/disorders/bppv/epley/first.html. [Google Scholar]
- 11.Magliulo G, Bertin S, Ruggiera M, Gagliardi M. Benign paroxysmal positional vertigo and post-treatment quality of life. Eur Arch Otorhinolaryngol. 2005;262:627–30. doi: 10.1007/s00405-004-0784-2. [DOI] [PubMed] [Google Scholar]