Abstract
OBJECTIVE
To investigate variations in accessibility, continuity of care, and coordination of services as experienced by patients in Quebec on the eve of major reforms, and to provide baseline information against which reforms could be measured.
DESIGN
Multilevel cross-sectional survey of practice.
SETTING
One hundred primary health care settings were randomly selected in urban, suburban, rural, and remote locations in 5 health regions in Quebec.
PARTICIPANTS
In each clinic, we chose up to 4 physicians and 20 consecutive patients consulting each physician.
MAIN OUTCOME MEASURES
Patients’ responses to a self-administered questionnaire, the Primary Care Assessment Tool, that assessed patient-provider affiliation, accessibility, relational continuity, coordination of primary and specialty care, and whether patients received health promotion and preventive services.
RESULTS
A total of 3441 patients participated (87% acceptance rate) in 100 clinics (64% response rate). Timely access was difficult; only 10% expressed confidence they could be seen by their regular doctors within a day if they became suddenly ill. Average waiting time for a doctor’s appointment was 24 days. Coordination of care with specialists was at minimally acceptable levels. Patients with family physicians recalled them addressing only 56% of the health promotion and preventive issues appropriate for their age and sex, and patients without family physicians recalled physicians addressing substantially fewer (38%). Most patients reported they were highly confident that their physicians knew them well and would manage their care beyond clinical encounters (relational continuity). The exception was the 16% of patients overall who did not have family physicians (34% of patients at walk-in clinics).
CONCLUSION
This survey highlights serious problems with accessibility. Improvement is needed urgently to avoid deterioration of patients’ confidence in the healthsystem even though patients rate their relationships with their physician highly. Health promotion, preventive services, and coordination with specialists also needed to be improved, and careful thought must be given to the plight of those without family physicians.
RÉSUMÉ
OBJECTIF
Déterminer les différences d’accessibilité, de continuité des soins et de coordination des services selon l’expérience des patients du Québec à la veillede réformes majeures, et fournir les données de base qui permettront d’évaluer les effets des réformes.
TYPE D’ÉTUDE
Enquête transversale à plusieurs niveaux portant sur la pratique.
CONTEXTE
On a choisi au hasard 100 établissements de soins primaires de divers milieux: ville, banlieue, campagne et régions éloignées dans 5 régions sanitaires du Québec.
PARTICIPANTS
Dans chaque clinique, on a choisi 4 médecins et 20 patients consécutifs de chaque médecin.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Réponses des patients à l’Outil d’évaluation des soins primaires, un questionnaire auto-administré qui évalue l’affiliation patient-soignant, l’accessibilité, la continuité relationnelle, la coordination entre soins primaires et spécialisés, et le fait que les patients sont ou non l’objet de promotion de la santé et de services préventifs.
RÉSULTATS
Au total, 3441 patients ont participé (taux d’acceptation de 87%) dans 100 cliniques (taux de réponse de 64%). L’accès au médecin habituel en temps opportun était difficile, seulement 10% se disant confiants de pouvoir être reçus en moins de 24 heures en cas de maladie soudaine. Le temps d’attente moyen pour rencontrer un médecin était de 24 jours. La coordination des soins avec les spécialistes était tout au plus acceptable. Les patients avec médecins de famille rapportaient que ceux-ci avaient abordé seulement 56% des questions de promotion et de prévention de la santé appropriées pour leur âge et leur sexe et ceux sans médecins de famille rapportaient que les médecins avaient abordé encore beaucoup moins de ces questions (38%). La plupart des patients se disaient très confiants que leur médecin les connaissaient bien et qu’il s’occuperait du suivi au-delà des rencontres cliniques (continuité relationnelle). Faisaient exception ceux qui n’avaient pas de médecin de famille (16% du total et 34% des patients des cliniques sans rendezvous).
CONCLUSION
Cette enquête révèle de sérieux problèmes d’accessibilité. Il est urgent d’apporter des correctifs pour éviter que la confiance des patients dans le système de santé ne subisse une baisse, même si les patients disent avoir une excellente relation avec leur médecin. Il y a également place à l’amélioration pour la promotion de la santé, les services préventifs et la coordination avec les spécialistes; on doit aussi accorder une attention particulière à la situation des patients sans médecin de famille.
In 2000, the Commission d’étude sur les services de santé et services sociaux1 found Quebec’s health care system deficient with regard to accessibility, continuity, and coordination of care. Like other such commissions, this one identified better organization and delivery of primary care as the key solution.1–5 The First Ministers’ Health Accord in 2000 allocated $800 million over 5 years to accelerate change in primary care,6 and in 2002, Quebec’s Ministry of Health and Social Services created and accredited family medicine groups (FMGs) to strengthen primary care.
Quebec is divided into 170 subregions, each of which is associated with a Centre local de services commun-autaires (CLSC), or local community health centre, that provides health and social services to a defined area. The scope of services varies with the needs of the population, and many metropolitan CLSCs do not offer general medical services. Approximately 15% of primary care services are provided through CLSCs and the rest are provided through physician-run clinics and private practices that are the norm elsewhere in Canada.
Although Statistics Canada has provided information on access to health services and the proportion of Canadians who have family physicians,7,8 the Canadian Community Health Survey did not provide information in enough detail to permit assessment of primary care overall. The purpose of our study was to survey primary care sites in Quebec to investigate patients’ experiences with primary care before reforms in order to establish a baseline against which reforms could be measured.
METHODS
We conducted a cross-sectional, multilevel survey of primary care settings, physicians, and patients from December 2001 to October 2002 in 5 health regions of Quebec: Montreal, Montérégie, Bas-Saint-Laurent, Côte-Nord, and Gaspésie. We used a listing of primary care clinics compiled in 20009 and the 170 CLSCs to classify sites into urban, suburban, rural, and remote geographic areas. Then we used systematic random sampling to ensure that within each geographic area our study sample had 10% solo practices, 65% group practices, and 15% CLSCs.
Eligible sites were those that offered general medical services to an undifferentiated clientele and had not undergone major changes in the last year. An additional eligibility criterion, added after data collection began, was that at least two thirds of clinic patients could respond in English or French. Within each clinic, depending on size, we selected up to 4 physicians who had practised general medicine there at least 1 day a week for at least 1 year and recruited 20 consecutive patients consulting each physician on a certain clinic day. We chose representative days; for example, if a clinic offered walk-in and scheduled care, we sampled patients from both. Data collection sometimes spanned more than 1 day; collection was stopped after 5 half-days if 20 patients were not recruited.
Eligible patients were those able to complete a self-administered questionnaire in English or French (translation validated). Parents or guardians of children younger than 18 years responded to questionnaires about their children’s care. Research technicians recruited patients on-site and administered the questionnaire face-to-face if patients had difficulty filling it in by themselves (n = 216, 6%). Most patients completed the questionnaires in the waiting room, but some (37%) opted to mail back their responses later. Sensitivity analysis showed no systematic differences in patients’ reported experiences by method or timing of administration.
Patients’ experiences were assessed principally through the Primary Care Assessment Tool (PCAT),10 which measures strength of patient-provider affiliation, degree of confidence in being seen within a day for a new problem (first-contact accessibility), confidence that providers know the medical history and personal situation and will manage care on an ongoing basis (relational continuity) and work well with specialists (coordination of care), and patients’ recall of having received preventive care. Responses on the PCAT can be valid even if patients do not have regular providers. The questionnaire included the scale for organizational accessibility from the Primary Care Assessment Survey.11 All questions related to patients’ regular care providers or, for those without regular providers, physicians or clinics being consulted that day. Conceptual and operational definitions of the constructs are listed in Table 1.12,13
Table 1.
Conceptual and operational definitions of minimum expectations for core dimensions of primary health care
| DEFINITION OF CONCEPT | OPERATIONAL DEFINITIONS OF MINIMUM EXPECTATIONS |
|---|---|
| Accessibility: The ability of a person to obtain needed care, including advice and support, from his or her practitioner of choice within a time frame appropriate to the urgency of the problem12 | First-contact accessibility: Confidence that patients could get advice or orientation within 1 day from their regular providers if they suddenly got sick and needed care at various times of day (4 items rated on a scale of 1 to 4, expected—3)
Organizational accessibility: Rating of office location, hours of operation, wait times for appointments, and ease of contacting the clinic and the regular physician (6 items rated on scale of 1 to 6, expected—4.5) |
| Relational continuity: A therapeutic relationship with a provider that spans more than 1 episode of care and leads to a sense of clinical responsibility in the provider and accumulated knowledge of a patient’s personal and medical context13 | Physician-patient affiliation: Ability to identify a regular physician who knows the patient and takes principal responsibility for his or her health care (3 items rated on a scale of 0 to 4, expected—3)
Accumulated knowledge: Confidence that a physician knows a patient’s medical history and personal situation (7 items rated on a scale of 1 to 4, expected—3) Care management: Confidence that a physician will manage care beyond the current clinical encounter (6 items rated on a scale of 1 to 4, expected—3) |
| Coordination and continuity: Delivery of services by different providers in a timely and complementary manner such that patients’ care is connected and coherent13 | Coordination with specialists: Confidence that primary care physician and specialist will collaborate and communicate in patient’s care (8 items rated on a scale of 1 to 4, expected—3) |
| Comprehensive care: Provision of a full range of services to meet patients’ health care needs, including health promotion and disease prevention and management of common conditions12 | Health promotion and preventive care: Recall of physician having addressed at least two thirds of the recommended age- and sex-appropriate strategies to maintain health (list varied for age and sex, expected—67% of strategies “probably” or “definitely” addressed) |
Responses to each PCAT item were ratings on a scale of 1 to 4: 1—definitely not, 2—probably not, 3—probably, and 4—definitely. For each dimension scale we calculated the mean of the items. To facilitate interpretation of results, we established the quality standard as a mean of 3.0 (“probably”) for each item as the minimum level that should be expected for each attribute of care. The minimum level represented a quantitative expression of patients’ expectations of care.14,15
Physicians completed the provider version of the PCAT, which assessed their usual first-contact accessibility, accumulated knowledge of patients, case management responsibility, coordination of care, and provision of preventive services. Physicians’ secretaries provided dates of their third-next available appointments.16
All descriptive results were weighted (inverse of the sampling fraction for clinics) to be representative of the regions in which clinics were sampled. We present the mean response to each attribute and the proportion of patients who rated it above or below the expected minimum level. We conducted subanalyses to look for the effects of various patient characteristics.
The study received ethical approval from the University of Montreal’s Hospital Research Centre and from several CLSCs that required local approval.
RESULTS
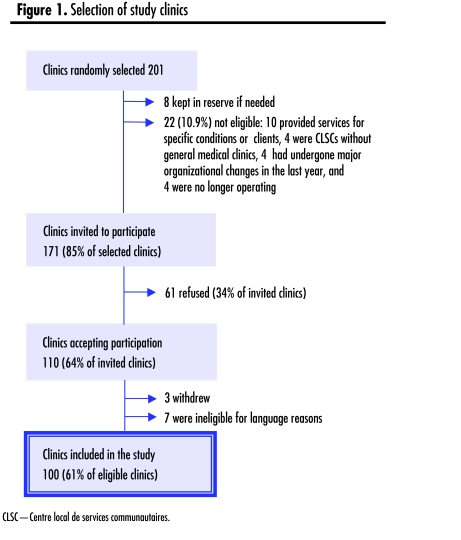
The final participation rate among eligible clinics was 61% (100 of 164) (Figure 1). The study sample included 10 clinics that identified themselves as stand-alone walk-in clinics. A total of 221 physicians contributed an average of 18 (median 20) patients in clinics and 12 patients (median 12) in CLSCs. Of the 4764 patients contacted, 93% were eligible and 89% consented to participate. Only 69% of the 1333 who chose to mail in their questionnaires did so. The final patient response rate among eligible patients was 87% (n = 3441). Table 2 shows the distribution of clinics and characteristics of patients. Patients’ characteristics were typical of those seen in primary care.
Figure 1.
Selection of study clinics
Table 2.
Characteristics of clinics and patients included in the study
| CHARACTERISTICS | % |
|---|---|
| CLINICS (N = 100) | |
| Type of clinic | 57 |
| • Group practice | |
| • Solo practice | 16 |
| • Stand-alone walk-in clinic | 10 |
| • CLSC | 17 |
| Geographic location | 38 |
| • Urban | |
| • Suburban | 22 |
| • Rural | 24 |
| • Remote | 16 |
| PATIENTS* (N = 3441) | |
| Women | 65 |
| Language spoken | |
| • French | 76 |
| • English | 13 |
| • Many or other | 11 |
| Education level | |
| • Primary | 16 |
| • Secondary incomplete | 26 |
| • Secondary complete | 16 |
| • Postsecondary | 42 |
| Self-perceived health status | |
| • Poor | 5 |
| • Fair | 22 |
| • Good | 40 |
| • Very good or excellent | 33 |
CLSC—Centre local de services communautaires
Mean age of patients was 48.9 years (SD ±18.7 years).
About 77% of patients were consulting their regular providers on the study day. Overall, 16% did not have regular physicians, but in Montreal 22% did not; in walk-in clinics 34% did not. Surprisingly, 44% of walk-in clinic patients identified clinic doctors as the physicians responsible for most of their care; in most cases (85%), these doctors shared that perception.
Table 3 shows mean patient ratings of experiences relative to minimum expected levels of care for the 7 dimensions assessed. Patients’ confidence in first-contact accessibility falls strikingly below the minimum expected level. Only 10.4% expressed confidence they could be seen within a day by their regular providers. Chances were better if patients were sick during clinics’ open hours (67% were confident they would be seen).
Table 3.
Mean level of patients’ experience of core dimensions of primary care
| ASPECT OF CARE | MEAN RATING (SD) | % WHO RATED IT BELOW EXPECTED LEVEL |
|---|---|---|
| Accessibility | ||
| • First-contact accessibility (rated on a scale of 1 to 4, expected—3) | 2.21 (0.61) | 89.9 |
| • Organizational accessibility (rated on a scale of 1 to 6, expected—4.5) | 4.61 (0.89) | 38.6 |
| Relational continuity | ||
| • Physician-patient affiliation (rated on a scale of 0 to 4, expected—3) | 3.44 (1.19) | 16.2 |
| • Accumulated knowledge (rated on a scale of 1 to 4, expected—3) | 3.28 (0.70) | 26.5 |
| • Care management (rated on a scale of 1 to 4, expected—3) | 3.26 (0.52) | 23.7 |
| Coordination | ||
| • Coordination with specialists (rated on a scale of 1 to 4, expected—3) | 3.22 (0.83) | 30.0 |
| Comprehensive care (health promotion) | ||
| • Health promotion and preventive care (each strategy rated on a scale of 1 to 4, expected—67%* of age- and sex- appropriate strategies rated as probably [3] or definitely [4] addressed) | 56.4* (29.6) | 57.4 |
Mean and expected ratings are expressed as the proportion of age- and sex-appropriate strategies rated as probably (3) or definitely (4) addressed.
Ratings of organizational accessibility were better, but ratings of individual components varied greatly. While 85% rated convenience of office location as very good or excellent, only 48% rated waiting time for an appointment as very good or excellent, and only 46% rated ease of contacting a physician by telephone as very good or excellent. Average wait to the third-next available appointment was 24 days (SD 22 days, median wait time 19 days, range 0 to 167 days); only 19% of physicians were available within 7 days. These statistics exclude the 5% of physicians never available by appointment and the 5% where delays exceeded 6 months. Study physicians largely agreed with patients’ perceptions of accessibility: only 12% reported being able to see patients within a day for sudden illness.
Relational continuity, accumulated knowledge, and care management were well within acceptable levels. Not surprisingly, patients without regular physicians had significantly less confidence in these aspects of care than those with regular physicians did (that physicians knew their personal and medical context 2.5 vs 3.4 on a scale of 4—definitely to 1—definitely not, t = 64, P < .001, or would manage their care beyond the clinical encounter 2.9 vs 3.4, t = 16.9, P < .001).
The 60% of patients who had seen specialists within the last 2 years rated coordination of care at minimum acceptable levels. Patients whose primary care providers helped make specialist appointments (almost half) rated coordination of care higher than those whose providers did not (3.4 vs 2.4 on a scale of 1 to 4, t = 34, P < .001). For 26% of patients, the last specialist visit had not been referred by their regular providers, but about two thirds of these patients were nonetheless optimistic that their providers knew of the visit and its results.
On average, patients recalled that their physicians had addressed 56% (SD 30%) of the health promotion and preventive care issues appropriate for their age and sex (eg, nutrition, vaccinations, and mental health for all; safety for children; exercise, smoking, and alcohol for adults; osteoporosis for women; and prevention of falls for the elderly).17 Among those without regular physicians, only 38% of health issues had been addressed; among those with regular physicians about 64% had been addressed (t = 13, P < .001). By contrast, physicians reported “usually” addressing each issue; only a few indicated they addressed them “occasionally.”
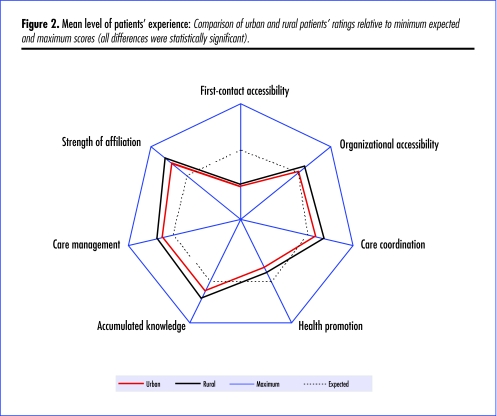
Finally, we found significant differences by geographic area (Figure 2). Rural patients reported significantly better experiences than urban patients did for all attributes of care. While there were also differences by type of clinic, geographic differences were more consistent. For instance, while urban and suburban CLSCs were similar to urban practices with respect to accessibility, CLSCs in remote areas were rated highly accessible.
Figure 2.
Mean level of patients’ experience: Comparison of urban and rural patients’ ratings relative to minimum expected and maximum scores (all differences were statistically significant).
DISCUSSION
Before this study, policy makers and the public perceived primary care in Quebec as unresponsive, fragmented, and uncoordinated with other levels of the health care system. Our study corroborates perceptions that primary care is unresponsive to the need for timely access and that coordination and health promotion barely meet minimum expectations. Patients expressed high levels of confidence in their relationships with their regular physicians, however, and these relationships translated into better coordination and comprehensiveness of care.
The large number of patients without family physicians is very worrisome (approximately 1 in 4 patients in Montreal). Patients without family physicians are less likely to get recommended preventive services and experience considerably poorer access to health care and continuity and coordination of care.18,19 The plight of those without regular physicians is critical and should be a major policy concern, especially in Quebec.
Patients are not confident they could be seen by their regular physicians or clinics within a day for sudden illness, especially at night or on weekends. While a 1-day wait might seem unreasonable to some physicians, certainly an average wait of 24 days for an appointment is not acceptable. Although most physicians have alternate arrangements for urgent care, patients depend on doctors’ secretaries for information on these, and this information varies greatly across practices.
Walk-in clinics, surprisingly, provide continuity of care for a large proportion of patients. Our results might not be generalizable, however, as some walk-in clinics were excluded from our sample because none of the rotating physicians worked a full day and others were inaccessible by telephone. Nonetheless, these clinics meet a need for patients without regular doctors, many of whom have figured out how to use them to achieve continuity of care. Studies have shown that the technical quality of care in walk-in clinics is as good or better than that in family medicine clinics.20
Has primary care changed since reforms in Quebec?
How much is primary care likely to have changed since reforms were implemented in Quebec? Family medicine groups have extended clinic hours and explicit agreements with other institutions for smooth transitions between various levels of care; accessibility and continuity are expected to improve. As of March 2006, there were 103 accredited FMGs (personal communication from Dr Jean-Guy Émond, President of the FMG Implementation Support Group), but the vast majority of Quebec’s population is not served by FMGs. It is unlikely the portrait of care we found in 2002 has changed substantially since then.
How different is Quebec’s health care system from systems in the rest of Canada? The PCAT questionnaire was also used in 4 rural communities in Nova Scotia in 1999. When asked whether they could be seen within a day if they got sick, Nova Scotians’ mean response was 2.5 (“maybe”), compared with 1.9 (“probably not”) in Quebec, according to the Nova Scotia Primary Health Care Department. Overall, the picture was more positive in Nova Scotia than in Quebec, and this could be related to physician-patient affiliation. According to the 2003 Canadian Community Health Survey,7 94% of Nova Scotians had regular doctors, while only 76% of people had them in Quebec (86% had them in Canada as a whole).
Access to health care is similar across Canada. According to the 2003 Canadian Community Health Survey,7 24% of Canadians needing immediate care for minor health problems reported having difficulty accessing care.7 Difficulty accessing care was reported by 26% of patients in Quebec, one of the highest rates, although similar to other provinces, with only Saskatchewan (17%), Alberta (22%), and British Columbia (21%) reporting lower rates. As in our survey, the most common problems across the country were difficulty contacting physicians or nurses and long waiting times for appointments.
A 2004 survey of primary care and patients’ perceptions of health systems carried out in 5 countries found that while Canada was second only to the United Kingdom in removing financial barriers, Canadians faced the greatest organizational barriers, with 25% of adult patients waiting longer than 6 days for care compared with 2% in New Zealand, 7% in Australia, 13% in the United Kingdom, and 19% in the United States.21 Only in the United States did a higher percentage of respondents believe it was very or somewhat difficult to get care on nights, weekends, or holidays without going to emergency departments (63% vs 59% in Canada).
Limitations
With a clinic response rate of 61%, there might be important biases in our sample. Most likely the study sample is biased toward good care, since clinic directors who were more secure in the quality of their services likely were more willing to participate. The actual experiences of patients might be worse that those reported here. Also, patients’ reports might not be accurate. Indeed, patients’ reports on, say, accessibility varied considerably within the same clinic, and patients with regular physicians consistently rated all aspects of services more positively. It appears that patients with good relationships with their physicians are more tolerant, so their reports might be positively biased. Finally, it is critical to keep in mind that inferences drawn from the results of the study apply only to service users, not to the population in general.
Conclusion
This survey highlights the fact that there is much room for improvement in accessibility to primary care services. People with regular primary care physicians have good continuity of care, experience acceptable coordination with specialists, and receive preventive care. Those without regular physicians have considerably worse experiences of care.
Acknowledgment
The work presented in this article should be attributed to the Department of Family Medicine at the University of Montreal in Quebec. The study was funded by the Canadian Health Services Research Foundation, the Quebec Health Research Foundation, the Regional Health Authority of Montreal-Centre, and the Dr Sadok Besrour Research Chair in Family Medicine. Direct in-kind support was provided by the Institut national de santé publique du Québec, the Collège des médecins du Québec, the Fédération des médecins omnipraticiens du Québec, the Regional Health Authorities of Bas-Saint-Laurent and Côte-Nord, and the Quebec Ministry of Health and Social Services. During the study, Dr Haggerty was appointed to the Department of Family Medicine at the University of Montreal and was supported as a research scholar (Junior 1) by the Quebec Health Research Foundation. Dr Beaulieu held the endowed Dr Sadok Besrour Research Chair in Family Medicine.
EDITOR’S KEY POINTS
This study addresses a very important step in health care reform, as it is crucial to have an understanding of the baseline in order to make the right changes and determine whether those changes have had the desired effects.
This study found that, in the Quebec health care settings studied, there was much room for improvement, particularly in the areas of accessibility to health care and provision of health promotion and preventive services. Patients who had regular family physicians fared better than those who did not.
POINTS DE REPÈRE DU RÉDACTEUR
Cette étude concerne un point très important de la réforme des soins de santé, soit la nécessité d’avoir une vue claire de la situation actuelle si on veut effectuer les bons changements et vérifier si ces changements apportent les effets désirés.
Les résultats de l’étude indiquent que dans l’organisation des soins de santé au Québec, il y a place à beaucoup d’amélioration, en ce qui concerne notamment l’accessibilité aux soins, la promotion de la santé et les services préventifs.
Footnotes
This article has been peer reviewed.
Competing interests
None declared
Contributors
Drs Haggerty, Pineault, Beaulieu, Goulet, and Rodrigue, Mr Brunelle, and Ms Gauthier contributed to concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
References
- 1.Clair M, editor. Commission d’étude sur les services de santé et les services soci-aux: les solutions émergentes. Rapport et recommandations. Quebec city, Que: Government of Quebec; 2000. [Google Scholar]
- 2.Sinclair DG, editor. Looking back, looking forward: the Ontario Health Services Restructuring Commission (1996–2000). A legacy report. Toronto, Ont: Government of Ontario; 2000. [Google Scholar]
- 3.Fyke KJ, editor. Caring for Medicare: sustaining a quality system. Regina, Sask: Policy and Planning Branch, Saskatchewan Health; 2001. [Google Scholar]
- 4.Premier’s Advisory Council on Health. A framework for reform. Report of the Premier’s Advisory Council on Health. Edmonton, Alta: Government of Alberta; 2001. [Accessed 2007 March 30]. Available from: www.health.gov.ab.ca/resources/publications/PACH_report_final.pdf. [Google Scholar]
- 5.Romanow RJ. Building on values—the future of health care in Canada. Final report. Ottawa, Ont: Commission on the Future of Health Care in Canada; 2002. [Google Scholar]
- 6.Health Canada. Primary Health Care Transition Fund. Ottawa, Ont: Health Canada; 2004. [Google Scholar]
- 7.Statistics Canada. Access to health services in Canada, 2003. Ottawa, Ont: Statistics Canada; 2004. [Google Scholar]
- 8.Sanmartin C, Berthelot J-M, White K. Access to health care services in Canada, 2001. Ottawa, Ont: Statistics Canada; 2002. Health Analysis and Measurement Group. [Google Scholar]
- 9.Demers M, Brunelle Y. Organisation de l’omnipratique au Québec entre 1994 et 1999. Quebec, Que: Ministère de la Santé et des Services sociaux; 2000. [Google Scholar]
- 10.Cassady CE, Starfield B, Hurtado MP, Berk RA, Nanda JP, Friedenberg LA. Measuring consumer experiences with primary care. Pediatrics. 2000;105(4 Pt 2):998–1003. [PubMed] [Google Scholar]
- 11.Safran DG, Kosinski M, Tarlov AR, Rogers WH, Taira DH, Lieberman N, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Haggerty J, Burge F, Gass D, Lévesque JF, Beaulieu MD, Pineault R, et al. Operational definitions of attributes of primary health care to be evaluated: results of a consensus among Canadian experts. Montreal, Que: University of Montreal; 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beaulieu MD. What do patients want from their GP? Common expectations beyond cultural differences. Br J Gen Pract. 2000;50(460):860–1. [PMC free article] [PubMed] [Google Scholar]
- 15.Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH. Direct observation of requests for clinical services in office practice: what do patients want and do they get it? Arch Intern Med. 2003;163(14):1673–81. doi: 10.1001/archinte.163.14.1673. [DOI] [PubMed] [Google Scholar]
- 16.Institute for Healthcare Improvement. Measures: primary care access. Third next available appointment. Cambridge, Mass: Institute for Healthcare Improvement; 2005. [Accessed 2005 November 15]. Available from: http://www.ihi.org/IHI/Topics/OfficePractices/Access/Measures/ [Google Scholar]
- 17.Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. Ottawa, Ont: Canada Communication Group; 1994. [Google Scholar]
- 18.Flocke S, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 Suppl):AS21–30. doi: 10.1097/00005650-199808001-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ettner SL. The relationship between continuity of care and the health behaviors of patients: does having a usual physician make a difference? Med Care. 1999;37(6):547–55. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Hutchison B, Ostbye T, Barnsley J, Stewart M, Mathews M, Campbell MK, et al. Patient satisfaction and quality of care in walk-in clinics, family practices and emergency departments: the Ontario Walk-In Clinic Study. CMAJ. 2003;168:977–83. [PMC free article] [PubMed] [Google Scholar]
- 21.Schoen C, Osborn R, Huynh PT, Doty M, Davis K, Zapert K, et al. Primary care and health system performance: adults’ experiences in five countries. Health Aff (Millwood) 2004 doi: 10.1377/hlthaff.w4.487. Suppl web exclusives:W4–487–503. [DOI] [PubMed] [Google Scholar]