A 35-year-old female factory worker presented with pain and swelling at the base of her thumb, which was aggravated by use and relieved with rest. The pain was typically piercing, was exacerbated by twisting and gripping motions, and lasted only momentarily. In addition to the pain, she was having trouble performing simple tasks at work, such as opening jars or turning keys. The patient had no history of arthritis, nor family history of arthritis. Physical examination revealed swelling and tenderness around the base of the thumb. At the first carpometacarpal (CMC) joint, crepitus was present and the grind test produced pain and a crunching sound. The patient was also sent for radiographs (Figure 1).
Figure 1.
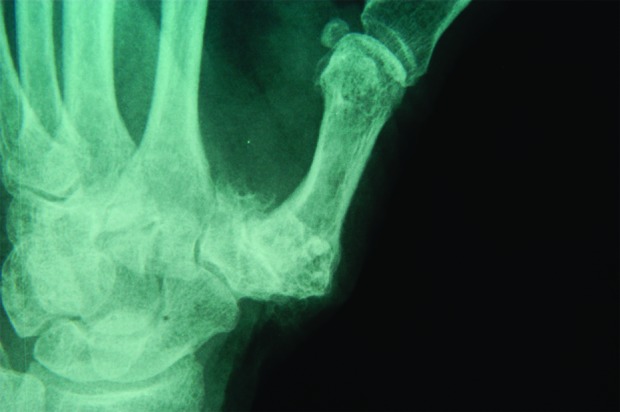
Arthritis in first carpometacarpal joint of left thumb
A clinical diagnosis of thumb CMC joint arthritis was made and confirmed by radiology. Subluxation of the CMC joint, diminished CMC joint space, osteophytes, and sclerosis of the joint surfaces were present. The thumb CMC joint is the most common joint in the hand affected by arthritis.
Tests and treatments
The grind test is performed by gripping the patient’s metacarpal bone of the thumb and moving it in a circle and loading it with a gentle axial force. A patient with thumb CMC joint arthritis generally complains of a sudden sharp pain at the CMC joint.
The patient’s Finkelstein test (radial-side wrist pain exacerbated by flexion and ulnar deviation of the wrist with the thumb adducted across the palm) results were negative, ruling out de Quervain tenosynovitis. There was no corresponding trauma or laxity of the ligaments to indicate gamekeeper’s thumb. Last, no triggering during flexion was found on clinical examination.
The options of medical therapy and surgical intervention were discussed with the patient. In general, splinting of the thumb with a CMC joint is offered as the first line of treatment. The splint supports the thumb during activity and reduces discomfort. Many patients might delay or avoid surgery by using splints; however, a downside to the use of splints over the long-term is thumb stiffness and weakness. Nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids injected directly into the involved joint are used during periods of acute exacerbations.
The patient returned after 5 weeks, complaining that the pain was much deeper and was constant and that she was unable to go to work. Physical examination revealed joint subluxation and a collapse deformity of the first metacarpal joint flexion and metacarpal phalangeal joint hyperextension.
Several surgical procedures for CMC joint arthritis are very effective in relieving pain related to this condition. These procedures involve excision of the arthritic trapezium joint (at the base of the thumb metacarpal) and filling the resulting space with a spacer, such as the flexor carpi radialis tendon, or a silicone rubber block or joint prosthesis.1,2 The postoperative regimen includes 4 to 5 weeks of splinting and physiotherapy to restore motion and strength of the affected hand.
Classification of CMC joint arthritis
Eaton and Glickel3 classify trapeziometacarpal osteoarthritis into various stages to determine appropriate treatment.
Stage I
This stage includes mild joint narrowing or subchondral sclerosis, mild joint effusion, or ligament laxity. No subluxation or osteophyte formation are present. Treatment for this stage includes NSAIDs and immobilization, which involves splinting the thumb in abduction.
Stage II
At this stage, besides CMC joint narrowing and subchondral sclerosis, there might be osteophyte formation at the ulnar side of the distal trapezial articular surface. Mild to moderate suluxation, with the base of the first metacarpal dislocated radially and dorsally, might appear. Treatment includes ligament reconstruction and tendon interposition.
Stage III
This stage includes further joint space narrowing with cystic changes and bone sclerosis. Osteophytes are prominent at the ulnar border of the distal trapezium. The first metacarpal is moderately displaced radially and dorsally. Passive reduction might not be present; the scaphotrapezial joint might show arthrosis, and there could be a hyperextension deformity of the CMC joint. Treatment includes ligament reconstruction and tendon interposition.
Stage IV
In this stage, destruction of the CMC joint is similar to that in stage III. Scaphotrapezial joint has evidence of destruction, the CMC joint is usually immobile, and often patients have little pain. Treatments are ligament reconstruction and tendon interposition.
Footnotes
Competing interests
None declared
References
- 1.Aston SJ, Beasley RW, Thorne CHM. Grabb and Smith’s plastic surgery. 5. Philadelphia, Pa: Lippincott Williams & Wilkins; 1997. pp. 975–79.pp. 999–1003. [Google Scholar]
- 2.Green DP. Operative hand surgery. 3. London, Engl: Churchill Livingstone; 1993. pp. 1969–83. [Google Scholar]
- 3.Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987;3(4):455–71. [PubMed] [Google Scholar]


