Abstract
A 10-week-old, male, border collie-cross puppy was examined for an acute onset of unilateral vestibular signs. Neurologic deterioration was rapid over the next 12 hours and the puppy was euthanized. Rabies was diagnosed by histopathologic and immunohistochemical examination.
Résumé
Rage chez un chiot de 10 semaines. Un chiot Border Collie croisé a été examiné pour une installation aiguë de signes vestibulaires unilatéraux. La détérioration neurologique a été rapide dans les 12 heures suivantes et le chiot a été euthanasié. La rage a été diagnostiquée à l’examen histopathologique et immunohistologique.
(Traduit par Docteur André Blouin)
A 10-week-old, male, border collie-cross puppy was presented to the Western College of Veterinary Medicine (WCVM) Teaching Hospital in Saskatoon, Saskatchewan, for incoordination and head tilt. The puppy had been clinically normal 4 d earlier when he was vaccinated against canine distemper virus, parainfluenza virus, canine adenovirus-2 and canine parvovirus (Vanguard® Plus 5; Pfizer Animal Health, Exton, Pennsylvania, USA) at the WCVM. He had received no previous vaccines. He had been slightly lethargic on the day following vaccination and this had become progressively worse over the 24 h prior to emergency presentation. He was presented to the emergency service, since he was moaning and had developed nystagmus and an abnormal gait.
The puppy had been born on a farm in southern Saskatchewan in a litter of 9 puppies and raised in a barn. The other puppies and the dam had appeared healthy at the time that this pup was adopted by the current owners 2 wk previously. The vaccination status of the bitch was uncertain. At his new home, the pup mainly lived outdoors with access to a garage.
Case description
On physical examination at the WCVM, the puppy was quiet, but alert and responsive and in good body condition. He was slightly ataxic but able to ambulate effectively. He had a slight head tilt to the left and would, occasionally, fall in that direction. He had a horizontal nystagmus with fast phase towards the right. Other cranial nerve responses were normal. Conscious proprioception, as assessed by knuckling and hopping, and reflexes were normal in all limbs. Palpation over his left bulla inconsistently elicited a painful response. On examination, the external ears were normal and both tympanic membranes appeared normal.
The puppy resisted restraint during jugular blood sample collection and IV catheter placement, and bit one of the restrainers. Blood collected from the puppy for immediate analysis revealed a normal hematocrit (0.42 L/L; reference range, 0.38 to 0.55 L/L) and total protein (65 g/L; reference range, 54 to 78 g/L). A chemical panel revealed a decrease in amylase (198 U/L; reference range, 300 to 1300 U/L), a mild decrease in urea (1.6 mmol/L; reference range, 2.5 to 10.4 mmol/L), mild hyperglycemia (8.88 mmol/L; reference range, 4.65 to 8.83 mmol/L), and mild hypoglobulinemia (20 g/L; reference range, 23 to 38 g/L). None of these abnormalities were considered to be significant, although there was some consideration of hepatic dysfunction causing encephalopathy, based on the low urea.
The puppy was maintained in the hospital overnight and lactated Ringer’s solution (Hospira, Montreal, Quebec) was administered, IV, at 2 mL/kg bodyweight (BW)/h. The dog’s neurological signs worsened steadily over the next 6 h. Although the puppy could still ambulate, he became more disoriented and had intermittent periods of severely depressed mentation that alternated with short episodes of extreme agitation. He wandered aimlessly and, intermittently, snapped as if to bite. The nystagmus became more pronounced and when the puppy was restrained in dorsal recumbency, the nystagmus transiently changed from horizontal to vertical. Response to stimulation of the skin of the muzzle and the nasal mucosa was diminished on the left compared with the right, suggesting decreased facial sensation on the left. Within a few hours, the puppy was unable to rise from lateral recumbency and made attempts to bite whenever handled. Due to his rapidly worsening condition, the owner elected to have the puppy euthanized; a necropsy was performed.
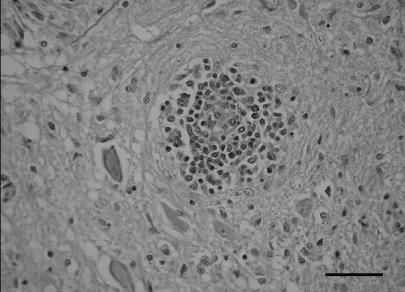
No gross abnormalities were identified during postmortem examination. Histopathological examination of the brain revealed severe nonsuppurative encephalitis with perivascular lymphocyte, plasma cell, and occasional macrophage infiltration (Figure 1). Neuronal necrosis, central chromatolysis, and moderate gliosis and astrocytosis were also noted in some areas. Intracytoplasmic inclusion bodies, or Negri bodies, were present in affected neurons in several locations but were most prominent in the medulla. The lesions were detected in all areas of the brain examined, in order of severity as follows: midbrain at the obex, brainstem at the red nucleus, hippocampus, cerebellar white matter and Purkinje cells, and cerebrum. There was a severe lymphocytic plasmacytic infiltration in the trigeminal (Gasserian) ganglion. There was congestion and edema in the lungs, but no significant pathological changes were noted in the other organs. Canine distemper virus was not detected in the brain on immunohistochemical staining. A final diagnosis of rabies was made after detection of rabies antigen in formalin fixed sections of the brain, using a 1:2000 dilution of rabbit anti-rabies polyclonal antibody by an avidin-biotin-peroxidase complex (ABC) immunohistochemical staining technique. The Canadian Food Inspection Agency (CFIA) laboratory in Nepean, Ontario, confirmed the diagnosis by a similar method. The Public Health Department was notified and the owners and veterinary clinic personnel received postexposure prophylaxis, as warranted. The dam and 5 of the 8 littermates were located and determined to be clinically normal.
Figure 1.
Photomicrograph of the brain of a rabid 10-week-old puppy illustrating lymphocytic, plasmacytic perivascular cuffing in the medulla. Hematoxylin and eosin stain, 40 × magnification. Bar = 50 microns.
Discussion
Rabies virus (RABV) is a Lyssavirus in the family Rhabdoviridae. Foxes, coyotes, and wolves are among the most susceptible to RABV infection (1,2). Skunks, raccoons, bats, cattle, and cats are considered highly susceptible, while domestic dogs, sheep, goats, and horses are only moderately susceptible (1,3). Young of every species are more susceptible than mature animals (2,3). In addition to species susceptibility, factors such as the viral variant, the bite site, and the quantity of virus inoculated affect susceptibility and incubation period (2,3).
Bites by an animal shedding virus in saliva are the most common method of transmission of the virus to other animals or humans. Contact of infected saliva with mucous membranes and open wounds or inhalation of high concentrations of virus rarely cause disease (4). The virus can remain viable in a carcass for several days at 20°C, and longer at colder temperatures, so consumption of rabid carcasses may also be an important transmission route in carnivorous species (3,5). Environmental transmission by fomites is rare (1,4).
Most dogs and cats are infected through contact with an infected wildlife reservoir host. In Saskatchewan, the primary wildlife reservoir for RABV is the skunk, although the virus has also been identified in insectivorous bats (6). Infected raccoons and foxes have rarely been identified in Saskatchewan, but in each case, they have been infected with a skunk-strain of the virus (unpublished information: Saskatchewan Agriculture and Food). Rabies surveillance data collected by the CFIA reveal that the importance of individual wildlife vectors varies regionally (Table 1) (6). Strains of RABV adapt to different host species, and most transmission occurs within species, establishing a particular virus variant at an endemic level within a population (5,7). Interspecific transmission occurs occasionally and can result in infection of domestic animals and humans (7,8). Distinct viral variants that exist in different host populations and in different geographic regions can be distinguished by demonstrating antigenic differences with monoclonal antibodies or through genetic analysis of viral RNA (1,5,8,9). Unfortunately, the RABV variant infecting this pup was not identified, but it is most likely that a skunk strain was involved.
Table 1.
Positive rabies in Canada January 1, 2001 to December 31, 2005. Positive rabies cases in each province listed by species. Compiled from annual statistics provided by the Canadian Food Inspection Agency (6)
| NWT/ Nunavut | Yukon | BC | AB | SK | MB | ON | QC | NB | NS | PEI | NL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dog | 12 | 5 | 14 | 9 | 5 | 2 | ||||||
| Cat | 1 | 2 | 8 | 9 | 1 | 1 | 1 | 1 | 1 | |||
| Skunk | 4 | 101 | 235 | 168 | 4 | |||||||
| Bat | 79 | 17 | 22 | 4 | 322 | 59 | 3 | |||||
| Fox | 42 | 10 | 79 | 24 | 33 | |||||||
| Raccoon | 1 | 88 | 1 | 49 | ||||||||
| Wolf | 2 | 2 | 3 | 2 | 3 | |||||||
| Coyote | 3 | |||||||||||
| Bear | 1 | 1 |
Striped skunks (Mephitis mephitis) are the most important species perpetuating wildlife rabies in Saskatchewan and are responsible for most infections in dogs (6,9). Infected skunks have a prolonged period of clinical illness during which they shed large quantities of virus in saliva and have a tendency to wander into locations where they can come into contact with pet or roaming dogs (1,10). The affected pup had no signs of a healing bite wound, so it is possible that the site had already healed or that exposure occurred through mucous membranes when a rabid skunk contacted the food and water bowls in the barn where this litter was raised. Bat-associated virus variants are the most common cause of rabies exposure in humans in North America, but they rarely cause rabies in dogs, so they were considered an unlikely cause of rabies in this puppy (8). Rabies virus infection in dogs can be variable in its presentation. The 2 classical clinical presentations of dogs with rabies encephalitis have been divided into the “furious or psychotic” and “dumb or paralytic” forms. The incubation period between exposure to RABV and clinical evidence of disease varies from 7 d to many months (average, 3 to 8 wk) in dogs (1,3). Some dogs will experience a prodromal phase prior to developing neurologic signs, during which they will be apprehensive, nervous, irritable, and may lick at the site of inoculation. The dog’s temperature may rise slightly, the pupils may dilate, and the nictitating membranes may cover the eyes (1,3).
Dogs with the furious form of rabies are increasingly restless and excitable. They may snap at imaginary objects and become incoordinated or disoriented. Occasionally, they will have seizures (1,3).
Dogs with the paralytic form of rabies typically experience lower motor neuron paralysis, which progresses from the site of inoculation to affect the entire nervous system (11). Brainstem involvement is common following facial inoculation, resulting in a hoarse bark, difficulty in swallowing, excessive salivation, diminished facial sensation, and a dropped jaw. Mentation is severely depressed and progression to coma and death is rapid (1,3,4). Clinical and laboratory evaluation of dogs with rabies meningoencephalomyelitis has rarely been reported due to the rapidly fatal course of infection and risks associated with human exposure (11).
The clinical diagnosis of rabies encephalitis is not always straightforward. Animals can have a misleading combination of signs or sometimes only mild neurologic signs or behavioral abnormalities, especially early in the course of disease (1,11). Systemic signs, such as vomiting, diarrhea, and stranguria, have also been reported (3,4). Some dogs will die without showing any detectable signs of illness (3).
There was no initial suspicion of rabies as a differential diagnosis in this puppy due to the mild neurologic signs at the time of presentation, resulting in potential exposure for numerous individuals in the clinic. Rapid progressive deterioration in the puppy’s mentation and behavior, and the development of an intermittent positional vertical nystagmus did prompt consideration of rabies as a potential differential diagnosis, but based on the age of the pup and no known exposure, rabies encephalitis was considered far less likely than encephalitis due to distemper, protozoal or bacterial disease, or granulomatous meningoencephalitis (GME).
Histopathological examination of this puppy’s brain revealed Negri bodies within neurons in the medulla, but cytoplasmic inclusions resembling Negri bodies can be found in the brains of some healthy animals (12,13). The diagnosis of rabies was confirmed by using an ABC immunoperoxidase technique that has been reported to have high specificity and sensitivity for the identification of RABV in formalin fixed tissues (12). The thalamus, pons, and medulla are the most reliable parts of the brain for testing (13). In this puppy, the most severe histological lesions corresponded to the clinical localization of disease to the brainstem.
The young age of this puppy and lack of known exposure to RABV steered clinicians away from a diagnosis of rabies. Rabies encephalitis, however, should always be considered as a reasonable differential diagnosis in any dog with progressive behavioral or neurologic dysfunction. Puppies with rabies can exhibit a variety of neurologic and nonneurologic signs. One recent article describes 2, 11-week-old, littermates that were presented to veterinarians for vomiting and inappetence. One puppy was euthanized due to extreme weakness and persistent vomiting. The other puppy became disoriented and depressed and a diagnosis of rabies encephalitis was made on postmortem evaluation (14).
Although the prevalence of wildlife rabies has been stable or increasing in North America, the number of cases of rabies in domestic dogs has been steadily declining because of vaccination protocols and animal control programs (1,8,15). Less than 10% of the dogs diagnosed with rabies in Canada have previously received rabies vaccines and some of those dogs may have been improperly or inadequately vaccinated (16,17). Puppies represent a uniquely susceptible group because of their age and the fact that they have not yet been vaccinated against RABV. Most rabies vaccines are licensed for administration to 12-week-old puppies. Although puppies from nonvaccinated bitches will respond to vaccination against RABV earlier (4 to 10 wk of age), puppies from well-vaccinated bitches do not respond well to rabies vaccination until 10 wk of age, even though detectable maternal RABV neutralizing antibody and rabies antiribonucleoprotein antibodies are decreased by 6 wk post-partum (18). It may be prudent to routinely recommend that puppies be kept strictly isolated from potential contact with wildlife reservoirs of RABV for the first 12 wk of life.
This case illustrates the susceptibility of puppies to rabies encephalitis and emphasizes the importance of early consideration of rabies as an important differential diagnosis in all puppies with behavioral or neurologic abnormalities. Practising veterinarians and diagnostic laboratories must be vigilant and initiate testing to rule out rabies in such cases to avoid the consequences of inadvertent human exposure to undiagnosed cases. CVJ
Footnotes
Dr. White’s current address is Department of Companion Animals, Atlantic Veterinary College, University of Prince Edward Island, 550 University Avenue, Charlottetown, Prince Edward Island C1A 4P3.
References
- 1.Greene CE, Rupprecht CE. Rabies and other Lyssavirus infections. In: Greene CE, editor. Infectious Diseases of the Dog and Cat. 3. Philadelphia: WB Saunders; 2006. pp. 167–183. [Google Scholar]
- 2.Blancou J, Aubert MFA, Artois M. Fox rabies. In: Baer GM, editor. The Natural History of Rabies. 2. Boca Raton: CRC Press; 1991. pp. 258–285. [Google Scholar]
- 3.Fekadu M. Canine rabies. In: Baer GM, editor. The Natural History of Rabies. 2. Boca Raton: CRC Press; 1991. pp. 368–375. [Google Scholar]
- 4.Jackson AC, Wunner H, editors. Rabies. San Diego: Acad Pr; 2002. pp. 165–180. [Google Scholar]
- 5.Wandeler AI. Rabies virus. In: Appel MJ, editor. Virus Infections of Carnivores. Amsterdam: Elsevier; 1987. pp. 449–461. [Google Scholar]
- 6.Canadian Food Inspection Agency [homepage on the Internet] Positive rabies in Canada. [Last accessed February 16, 2007]; [updated 2006–10–26]. Available from: http://www.inspection.gc.ca/english/anima/heasan/disemala/rabrag/statse.shtml.
- 7.Smith JS. New aspects of rabies with emphasis on epidemiology, diagnosis, and prevention of the disease in the United States. Clin Microbiol Rev. 1996;9:166–176. doi: 10.1128/cmr.9.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McQuiston JH, Yager PA, Smith JS, Rupprecht CE. Epidemiologic characteristics of rabies virus variants in dogs and cats in the United States, 1999. J Am Vet Med Assoc. 2001;218:1939–1942. doi: 10.2460/javma.2001.218.1939. [DOI] [PubMed] [Google Scholar]
- 9.Krebs JW, Mardel EJ, Swerrellow DL, Rupprecht CE. Rabies surveillance in the United States during 2004. J Am Vet Med Assoc. 2005;227:1912–1925. doi: 10.2460/javma.2005.227.1912. [DOI] [PubMed] [Google Scholar]
- 10.Charlton KM, Webster WA, Casey GA. Skunk rabies. In: Baer GM, editor. The Natural History of Rabies. 2. Boca Raton: CRC Pr; 1991. pp. 308–320. [Google Scholar]
- 11.Barnes HL, Chrisman CL, Farina L, Detrisac CJ. Clinical evaluation of Rabies virus meningoencephalomyelitis in a dog. J Am Anim Hosp Assoc. 2003;39:547–550. doi: 10.5326/0390547. [DOI] [PubMed] [Google Scholar]
- 12.Arslan A, Saglam YS, Temur A. Detection of rabies viral antigen in non-autolysed and autolysed tissues by using an immunoperoxidase technique. Vet Rec. 2004;155:550–552. doi: 10.1136/vr.155.18.550. [DOI] [PubMed] [Google Scholar]
- 13.Bingham J, van der Merwe M. Distribution of rabies antigen in infected brain material: Determining the reliability of different regions of the brain for the rabies fluorescent antibody test. J Virol Methods. 2002;101:85–94. doi: 10.1016/s0166-0934(01)00423-2. [DOI] [PubMed] [Google Scholar]
- 14.Millar K. Another litter of pups positive for rabies. News Views. 2005;227:1912–1925. [Google Scholar]
- 15.Varughese P. Rabies surveillance in Canada. CMAJ. 1986;134:617–618. [PMC free article] [PubMed] [Google Scholar]
- 16.Eng TR, Fishbein DB. Epidemiologic factors, clinical findings and vaccination status of rabies in cats and dogs in the United States in 1988. J Am Vet Med Assoc. 1990;197:201–209. [PubMed] [Google Scholar]
- 17.Gumley N. Rabies revaccination for companion animals: Canadian data. Can Vet J. 1999;40:404–407. [PMC free article] [PubMed] [Google Scholar]
- 18.Aghomo HO, Oduye OO, Rupprecht CE. The serologic response of young dogs to the Flury LEP strain of rabies virus vaccine. Vet Res Commun. 1990;14:415–425. doi: 10.1007/BF00343220. [DOI] [PubMed] [Google Scholar]