Abstract
Many barriers, including being uninsured or having less than comprehensive health insurance coverage, reduce access to palliative and end-of-life care by inner city minorities. Medicaid or Medicare coverage alone can limit options for pain and symptom management, especially when late referrals make it more difficult to achieve symptom control. Patient affiliation with a religion could offset perceived difficulties with pain medication as well as negative pain and symptom attitudes. Data were analyzed from the most recent assessments of 146 African Americans and Latinos enrolled in an outpatient palliative care unit of an inner city hospital. Fifty-seven percent were receiving palliative care for cancer. Compared with other patients, patients with a religious affiliation did not differ regarding pain medication stress. Uninsured patients with a religious affiliation reported more hopeful pain and symptom attitudes, while patients with a religious affiliation covered only by Medicaid reported less hopeful pain and symptom attitudes. More hopeful pain and symptom attitudes by religious-affiliated, uninsured patients may reveal adequate coping, yet also conceal problem domains. Conversely, less hopeful attitudes by religious-affiliated patients covered only by Medicaid serve as clues to coping difficulties and problem domains. Palliative care programs should carefully consider how to integrate religious support networks as pipelines for program referrals and potential partners for care.
Keywords: religious affiliation, uninsured, Medicaid, pain and symptom attitudes, palliative care
Race and ethnicity critically shape the experience of coping with chronic conditions and the experience of dying, with a considerable portion of these processes mediated by low socioeconomic status, a powerful predictor of health and well-being.1 In cancer, for instance, variations in morbidity and mortality rates by age and social class encompass a distinctive pattern of increased risk of terminal illness that disproportionately affects poor and minority populations.2 African Americans and Latinos are more likely to be undertreated for pain than are white patients, and pharmacies in minority neighborhoods are less likely to carry opioids.3,4 Similarly, African American patients with AIDS are less likely to use pain medications and more likely to die in hospitals.5
Minority patients deprived of appropriate health care and symptom management earlier during the course of their illness may be less receptive to palliative care when their conditions become more advanced. However, for many minority patients and caregivers, the dense social ties of extended family and church communities provide alternative sources of support, which should be carefully integrated into palliative and end-of-life programs.6
BARRIERS TO PALLIATIVE CARE
Lack of insurance, late referrals, and mistrust
Barriers to palliative care among ethnic minorities are closely tied to barriers limiting access to health care.7 Inability to pay for care and lack of insurance are major barriers, and ethnic minorities are at least twice as likely to be uninsured as whites.8 Among minorities with cancer, uninsured patients are more likely to be treated at late stages and to die from cancer.9 Inability to obtain health care in a timely fashion often has much to do with the presence of social constraints; submission to the demands of serious illness is rarely an option for poor patients and their families, because it interferes with the capacity to make a living and care for dependents.
The timely decision to refer a patient depends largely on the physician’s knowledge and perception of the value of palliative care; often referring doctors had a cultural background similar to their patients.10 In a study of Japanese family caregivers’ perceptions about whether the timing of referrals to palliative care was appropriate,11 factors contributing to late referrals were the family belief that palliative care shortens the patient’s life, insufficient advance discussion about palliative care, and lack of preparation for the changes in the patient’s condition(s). The Japanese caregivers considered effective communication among parties to be a critical factor for timely referrals to palliative care.
Empirical evidence for the prevalence and importance of culturally based mistrust in end-of-life care remains quite limited. In 1 qualitative study, African Americans stated that doctors could not always be trusted about stopping life support because they may remove life support for economic reasons.12 These reactions are not surprising, considering the American history of unethical experiments that exploited minorities, especially African Americans. It is also possible that some religious leaders in minority communities may have similar attitudes towards the medical care system, which could contribute to fewer, or later, referrals to palliative care as well.
Religion and culture
The church historically has served as a major vehicle for black patients and family caregivers to alleviate burden and gain access to social and health resources that were denied because of discrimination and poverty. African Americans facing death and bereavement issues were more likely to seek help from clergy.13 Clergy are qualified to address these issues by integrating religious beliefs and practices so that dying persons and their family can find meaning in suffering and death. Since social and cultural forces attract African Americans to black ministers for counseling, it is recommended that mental health professionals and black clergy exchange information so as to increase access to health and mental health care. Conversely, the importance of clergy and religious institutions in helping Latinos gain access to health and mental health care appears less well documented.
Education and advocacy about pain management by African American and Latino religious leaders may be an untapped approach for increasing referrals to palliative care. Religious beliefs may play a significant role in the willingness of some patients to accept palliative care. Some patients may believe that pain should be endured and pain medications avoided because they believe that patiently accepting God’s will, including suffering, is desirable or pleasing to God, or because they believe that they deserve to suffer because of past behavior. Clergy may help some patients consider that they may also choose to allow family and caregivers’ efforts to relieve suffering, which may be another means of honoring God’s will.
Research Questions
The quality of care minorities receive may be affected not only by lack of health insurance, as discussed previously, but by type of insurance. Indeed, less comprehensive insurance may result in lower quality or incomplete care due to underinsurance. African Americans and Latinos are much less likely to be privately insured than white Americans, and health insurance limited only to Medicaid or Medicare coverage may constrain options for pain and symptom management.14 Many uninsured patients are referred to palliative care late in the course of illness, and while exacerbated pain and symptoms may now qualify them for Medicaid, a long-standing history of mismanaged pain and symptoms may mean that full-blown conditions have become more difficult to control. Thus, more hopeful pain and symptom attitudes by uninsured patients anticipating Medicaid coverage could diminish over time once on Medicaid. Other patients covered only by Medicare could experience difficulty affording prescription drugs (although Medicare began covering these out-of-pocket costs in 2006).
When minority patients face challenges because of their insurance status, how do they try to resolve these problems? Although managing pain and symptoms was identified as one of the most important factors in end-of-life care,15 little empirical work has been conducted with minorities. Pain medication stress could be associated, in part, with not being able to afford medications. Medicaid patients do not have out-of-pocket costs for pain medications, but other patients, including those who are uninsured or underinsured, need to pay for them. Therefore, economically disadvantaged patients experiencing pain who do not qualify for Medicaid may experience more financial stress in managing pain medications. Conversely, economically disadvantaged patients with a need for prescription medication to manage pain or other symptoms may become more likely to qualify for Medicaid.
In the current study, we will explore whether African American and Latino palliative care outpatients without Medicaid are less likely to be taking pain medication and encounter pain medication stress. We will also investigate whether the presence of a religious affiliation in these outpatients buffers negative impacts from being medically uninsured or underinsured. The negative impacts are 1) pain medication stress and 2) less hopeful overall pain and symptom attitude.
Within the overall sample, we hypothesize that religious affiliation predicts more hopeful overall pain and symptom attitude, while being uninsured, or underinsured with Medicaid or Medicare coverage alone, predicts less hopeful overall pain and symptom attitude. We further hypothesize that religious affiliation will offset the extent of stress with pain medication as well as less hopeful pain and symptom attitudes within patient subgroups that are uninsured or covered only by Medicaid or Medicare.
MATERIALS AND METHODS
Data Collection
The study participants were 146 African American and Latino patients from an outpatient palliative care unit of an inner city hospital who were seen during the period between December 2000 and late March 2002. Most data were from patients receiving ongoing palliative care for more than 3 months. A community network in contact with patients and families contending with life-threatening illnesses served as a referral base; this network was comprised to a large extent by health care providers, pharmacists, and religious leaders, but also included community organizations and social service agencies. The major categories of primary diagnosis were cancer (57%), followed by congestive heart failure (7%), AIDS (6%), and end stage renal disease (5%). Patient ages ranged from 32 to 97 (mean 62.4) years; 59.4% were women. The hospital IRB board exempted the study from full review because the data collection was already part of routine care, patient data were coded so that they could not be used to identify individual patients, and the researcher had no contact with patients or other patient data that could be used to identify individual patients. Informed consent by patients was not required.
An African American nurse and bilingual Latino social worker conducted a comprehensive assessment upon admission that was updated every 3 months during a case conference with the patient, and if available, caregiver or family member. Only the latest assessment information was available for our analyses. The initial referral form (completed by the referring physician or other provider, such as clergy) and the initial and any follow-up comprehensive palliative care assessments were used by the nurse and social worker every 3 months to monitor, record, and update several variables within the program database (see Table 1).
TABLE 1.
Descriptive Statistics (n = 146)
| Variables | Frequency | % | Variables | Frequency | % |
|---|---|---|---|---|---|
| Predisposing factors | DNR | ||||
| Age >65 y | Unknown | 135 | 92.5 | ||
| No | 80 | 54.8 | Yes | 11 | 7.5 |
| Yes | 66 | 45.2 | Living Will | ||
| Gender | Unknown | 127 | 87.0 | ||
| Female | 91 | 62.3 | Yes | 19 | 13.0 |
| Male | 55 | 37.7 | Need Factors | ||
| Race | Lost insurance | ||||
| Hispanic/Latino | 45 | 30.8 | No | 130 | 89.0 |
| Black/African American | 101 | 69.2 | Yes | 16 | 11.0 |
| Religious affiliation | Cancer | ||||
| No | 56 | 38.4 | No | 63 | 43.2 |
| Yes | 90 | 61.6 | Yes | 83 | 56.8 |
| Catholic | Comorbidity | ||||
| No | 121 | 82.9 | No | 134 | 91.8 |
| Yes | 24 | 16.4 | Yes | 12 | 8.2 |
| Enabling factors | Length of stay | ||||
| Medicaid only | Less than 3 months | 40 | 27.4 | ||
| No | 114 | 78.1 | 3 months or more | 106 | 72.6 |
| Yes | 32 | 21.9 | Patient unaware of prognosis | ||
| Medicare only | No | 102 | 69.9 | ||
| No | 110 | 75.3 | Unknown | 28 | 19.2 |
| Yes | 36 | 24.7 | Yes | 16 | 11.0 |
| Medicaid and Medicare | Receiving pain medication | ||||
| No | 114 | 78.1 | No | 63 | 43.2 |
| Yes | 32 | 21.9 | Yes | 83 | 56.8 |
| Uninsured | Difficulty with pain medication | ||||
| Insured | 114 | 78.1 | No | 11 | 13.4 |
| Uninsured | 32 | 21.9 | Some | 69 | 84.1 |
| Formal support | A lot | 2 | 2.4 | ||
| No | 108 | 74.0 | Depression | ||
| Yes | 38 | 26.0 | No | 94 | 64.4 |
| Informal support | Unknown | 43 | 29.5 | ||
| No | 103 | 70.5 | Yes | 9 | 6.2 |
| Yes | 43 | 29.5 | Pain and symptom attitude index | ||
| Health care proxy | 2 = most hopeful | 71 | 69.0 | ||
| Unknown | 98 | 67.1 | 3 | 25 | 17.2 |
| Yes | 48 | 32.9 | 4 = neutral | 45 | 31.0 |
| Private insurance | 5 | 2 | 1.4 | ||
| No | 140 | 95.9 | 6 = most pessimistic | 2 | 1.4 |
| Yes | 6 | 4.1 |
DNR indicates do not resuscitate.
Difficulty with Pain Medications: n = 82. A transformed variable (Pain Medication Stress), incorporating all 146 observations, was used in regressions.
Single-Item Measures
Two patients reporting an Islamic or Muslim religious affiliation were excluded from the study. The religious affiliation variable consists of Catholic, Protestant, and other Christian denominations. Formal supports were social or health services provided to patients in order to maintain independence at home (e.g., visiting nurse, meals on wheels). Patients were receiving formal supports at admission or began receiving them upon referral by the palliative care nurse or social worker. Informal supports consisted of family members and friends who were available to provide care or assistance as needed.
Patients were asked to rate their attitudes on 2 items, Pain Attitude and Symptom Attitude, during comprehensive assessments every 3 months. Each item was measured using the same scale with 3 response categories (1, hopeful; 2, neutral; 3, pessimistic/fearful). Both items were added to create an index for Pain and Symptom Attitude, which is a regression outcome shared across all 146 participants. The Pain and Symptom Attitude index ranged from neutral to hopeful in almost all patients. When 4 patients with pessimistic/fearful attitudes were excluded, none of the findings changed in any of the analyses.
Although other variables (depression, patient unaware of prognosis, DNR, living will) could be stigmatizing or arouse fear, patient responses were coded into 3 categories (no, unknown, or yes) by the social worker or nurse, who were careful not to introduce bias by soliciting an unambiguous response. The availability of the unknown category to reflect missing or ambiguous responses should account for sources of unreliability that would otherwise bias the no responses.16 The nurse or social worker asked the patient, “Did you feel depressed during the past week?” Language was avoided that would characterize the patient as being depressed. Patient Unaware of Prognosis reflects the patient’s belief about their prognosis. Note that the palliative care team may be uncertain about the prognosis, and some patients may not be informed even when a prognosis is clear (e.g., in patients with cognitive impairment). Minorities such as African Americans may be highly distrustful towards components of care, such as DNR (do not resuscitate) status or the availability of a living will, which may fuel fears of second-rate, nonaggressive care.7,8 The potential for arousing mistrust could have prompted the nurse and social worker to skip certain items, leading them to categorize patients disproportionately within the unknown category.
Although the collected variables constitute single-item measures, they are likely to be reliable and valid because of the use of sensitive response options as well as because of various practices by the palliative care nurse and social worker. These practices involve frequent attention, diligent recording, and triangulation of information sources (e.g., referring provider, patient, caregiver, family members), in addition to resolving any inconsistencies across sources.
Data Analysis
Data were analyzed using SPSS® version 12. We estimated Spearman rank correlations to examine bivariate relations across variables prior to conducting multivariate analyses. The Aday and Andersen Behavioral Model of Health Utilization guided the order of entry of predictors into the multivariate regressions based on predisposing, enabling, and need factors. Binomial logistic regression and ordinal logistic regression (using the PLUM procedure) were used to test the effects of religious affiliation, insurance status, and their interactions in predicting stress in managing pain medication as well as pain and symptom attitude.
RESULTS
Descriptive Findings
Univariate analyses
African Americans comprise 69.2% of the sample and Latinos the remainder (30.8%; Table 1). Approaching two thirds (61.6%) reported a religious affiliation. Three insurance categories (Uninsured, Medicaid Only, and Medicaid and Medicare) each comprise 21.9% of the sample, while Medicare Only comprises 24.7%. More than half the patients (56.8%) were taking pain medications.
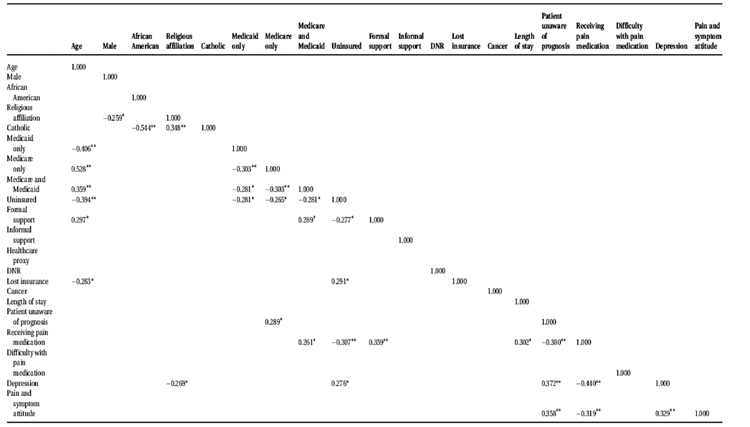
Correlation analyses
In Table 2, most Spearman Rank correlations remain statistically significant after Bonferroni correction of P values, which attests to the reliability of these items. The magnitude and directions of all relationships are consistent with clinical knowledge, suggesting that the items have concurrent and discriminant validity.
TABLE 2.
Correlations
DNR indicates do not resuscitate.
Spearman rank correlation was used because variables had 2 or 3 ordinal response categories.
Difficulty with Pain Medication is based on the 82 participants coded affirmatively on the prior variable Receiving Pain Medication.
P <.0016 (Bonferroni correction at .05 level, 2-tailed).
P <.0003 (Bonferroni correction at .01 level, 2-tailed).
The disclosure of a religious affiliation is associated with less depression and more positive pain and symptom attitudes. Religious affiliation is also related to higher formal social support and a greater likelihood of taking pain medications.
Patients with Medicare coverage only are more likely to be unaware of their prognosis. Patients with Medicare and Medicaid are more likely to be on pain medication and receive formal support. Uninsured status is related to less formal support, confirmed DNR status, less likelihood of taking pain medications, and risk for depression. Formal support is more likely when patients are on pain medication, which is associated with longer length of stay and patient awareness of prognosis. When patients are unaware of their prognosis or not on pain medication, more negative pain and symptom attitudes are more likely, and all 3 variables are associated with risk for depression.
Multivariate Findings
Binomial logistic regression (Pain medication stress)
In the main-effect model of Table 3, Uninsured status significantly predicts lower pain medication stress, while Medicare Only tentatively predicts (P < .10) lower pain medication stress. Odds ratios reveal that insured patients are almost 9 times more likely than uninsured patients to report moderate or high pain medication stress, while those with Medicare Only are 4 times more likely than other patients to report no or low pain medication stress. These findings could reflect the fact that patients who are uninsured or covered only by Medicare are less likely to be on pain medication, as shown in Table 2 (respectively, r = −0.307, P <.01; r = −0.175, P <.05).
TABLE 3.
Binary Logistic Regressions Predicting Low Pain Medication Stress*
| Variable | b | SE | Significance | Odds ratio (95% CI) |
|---|---|---|---|---|
| Male | .206 | .472 | .662 | 1.229 (.487, 3.100) |
| African American | .773 | .568 | .174 | 2.167 (.711, 6.599) |
| Age | −.020 | .021 | .342 | .980(.940, 1.022) |
| Religious affiliation | −.383 | .505 | .449 | .682 (.253, 1.835) |
| Catholic | .148 | .741 | .841 | 1.160 (.272, 4.951) |
| Medicaid only | .399 | .754 | .597 | 1.490 (.340, 6.533) |
| Medicare only | 1.392 | .796 | .080 | 4.022 (.846, 19.133) |
| Uninsured | 2.176 | .813 | .007 | 8.815 (1.791, 43.381) |
| Medicaid and Medicare | −.372 | .793 | .639 | .689 (.146, 3.264) |
| DNR | −.462 | .899 | .607 | .630 (.108, 3.671) |
| Cancer | .102 | .477 | .831 | 1.107 (.435, 2.819) |
| Patient unaware of prognosis | ||||
| Unknown: | 2.617 | .875 | .003 | 13.696 (2.463, 76.155) |
| Yes: | .303 | .698 | .665 | 1.354 (.344, 5.320) |
| Length of stay (>3 months) | −1.593 | .527 | .002 | .203 (.072, .571)† |
| 1. Model χ2 (df) | 63.154 | (14) | <.0001 | |
| 2. Nagelkerke’sR-Square | .471 |
Initially, Pain Medication Stress with four ordinal categories (i.e., no pain medication, pain medication-no difficulty, pain medication-some difficulty, pain medication-a lot of difficulty) was predicted; however, the assumption of parallel slopes was violated (i.e., the predictors cannot be assumed to have the same impact across all ordinal thresholds). Therefore, Pain Medication Stress was re-specified by collapsing the first two and then the last two categories, and di-chotomous logistic regression was used. The prediction of low pain medication stress is reported because it yields positive b parameters that result in odds ratios >1.
The odds ratio and 95% CI become 4.919 (1.752, 13.814) when the dependent dummy variable was recoded to predict high Pain Medication Stress. When Length of Stay (>3 months) was dropped, the remaining parameters did not change appreciably.
Simultaneously, Patient Unaware of Prognosis and Length-of-Stay (>3 months) both predict lower pain medication stress. Patients considered to be unaware of their prognosis are 13 times more likely than others to report no or low pain medication stress, while patients with a length-of-stay greater than 3 months are about 5 times more likely than others to report moderate or high pain medication stress.
None of the interaction terms involving religious affiliation and each health insurance category were statistically significant predictors of pain medication stress (not shown). Statistical power was assessed to detect the separate interaction effects represented by each of the 4 interactions and their first-order derivative component terms. Power was acceptable (between 0.60 and 0.70) to test the statistically insignificant interaction effects involving Religious affiliation with Medicare Only, but was low (less than 0.30) to test the remaining 3 interactions.
Ordinal logistic regression (Pain and symptom attitude)
In the first model of Table 4 (i.e., Main Effects), both Religious Affiliation and Pain Medication Stress predict more hopeful pain and symptom attitudes, while Patient Unaware of Prognosis predicts less hopeful pain and symptom attitudes.
TABLE 4.
Multivariate Ordinal Regressions Predicting Pain and Symptom Attitude
| Main effects
|
Religious affiliation x Medicaid
|
Religious affiliation x Uninsured
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | Significance | (95% CI) | b | SE | Significance | (95% CI) | b | SE | Significance | (95% CI) | |
| Sex | −.319 | .388 | .411 | (−1.07, 0.44) | −.260 | .401 | .516 | (−1.04, 0.52) | −.287 | .396 | .469 | (−1.06, 0.49) |
| African American | −.415 | .451 | .356 | (−1.29, 0.46) | −.421 | .464 | .365 | (−1.33, 0.49) | −.578 | .472 | .221 | (−1.50, 0.34) |
| Age | .027 | .018 | .124 | (−0.01, 0.06) | .027 | .018 | .131 | (−0.01, 0.06) | .032 | .018 | .076 | (−0.00, 0.06) |
| Religious affiliation | −.995 | .416 | .017 | (−1.81, −0.18) | −1.700 | .476 | <.001 | (−2.63, −0.76) | −.535 | .455 | .239 | (−1.42, 0.35) |
| Catholic | .277 | .594 | .641 | (−0.88, 1.44) | .304 | .593 | .609 | (−.085, 1.46) | .331 | .603 | .583 | (−.085, 1.51) |
| Medicaid only | .276 | .636 | .664 | (−0.97, 1.52) | −1.404 | .891 | .115 | (−3.15, 0.34) | .228 | .634 | .719 | (−1.01, 1.47) |
| Medicare only | −.223 | .676 | .742 | (−1.54, 1.10) | −.096 | .695 | .890 | (−1.45, 1.26) | −.320 | .680 | .638 | (−1.65, 1.01) |
| Uninsured | .539 | .622 | .386 | (−0.68, 1.75) | .516 | .644 | .423 | (−0.74, 1.77) | 1.636 | .813 | .044 | (0.04, 3.23) |
| Medicaid and Medicare | .515 | .657 | .432 | (−0.77, 1.80) | .836 | .675 | .215 | (−0.48, 2.15) | .315 | .662 | .635 | (−0.98, 1.61) |
| DNR | −.432 | .668 | .518 | (−1.74, 0.87) | −.442 | .701 | .528 | (−1.82, 0.93) | −.502 | .684 | .463 | (−1.84, 0.83) |
| Cancer | −.541 | .361 | .135 | (−1.24, 0.16) | −0.771 | .380 | .042 | (−1.51, −0.02) | −.486 | .370 | .189 | (−1.21, 0.23) |
| Patient unaware of prognosis | .660 | .275 | .017 | (−.012, 1.20) | .616 | .280 | .028 | (−1.51, 0.02) | .604 | .281 | .032 | (0.05, 1.15) |
| Pain medication stress | −.551 | .202 | .007 | (−0.94, −0.15) | −.612 | .212 | .004 | (−1.02, −0.19) | −.580 | .205 | .005 | (−0.98, −0.17) |
| Religious affiliation x Medicaid | 2.910 | .954 | .002 | (1.04, 4.77) | ||||||||
| Religious affiliation × Uninsured | −2.29 | .930 | .014 | −4.11, −0.47 | ||||||||
| 1. Model χ2 (df) | 35.34 | (13) | <.001 | 45.974 | (14) | <.001 | 41.668 | (14) | <.001 | |||
| 2. Goodness of Fit (Model to Data) | ||||||||||||
| Pearson (df) | 288.0 | (273) | .255 | 285.58 | (272) | .274 | 289.61 | (272) | .221 | |||
| Deviance (df) | 257.4 | (273) | .742 | 246.86 | (272) | .861 | 251.17 | (272) | .813 | |||
| Nagelkerke’s R-square | .249 | .312 | .287 | |||||||||
DNR indicates do not resuscitate.
When added as a predictor in all 3 regressions, Length of Stay (>3 months) was not statistically significant; the remaining parameters did not change appreciably.
In the second model (i.e., Religious affiliation × Medicaid), Medicaid Only does not predict pain and symptom attitudes. However, the interaction between Religious Affiliation and Medicaid is associated with less hopeful pain and symptom attitudes.
In the third model (i.e., Religious affiliation × Uninsured), Uninsured is positive and statistically significant, reflecting that uninsured patients overall have less hopeful pain and symptom attitudes. However, Uninsured patients with a Religious Affiliation, as revealed by the interaction, have more hopeful pain and symptom attitudes.
Statistical power was moderate to high to test the 4 statistically significant interaction effects involving religious affiliation with each of the insurance categories. Power ranged from 0.90 to 0.95 to test the interaction effect involving Religious affiliation and Uninsured, and from 0.80 to 0.85 to test the interaction effect involving Religious affiliation and Medicaid Only; power was acceptable (between 0.60 and 0.70) to test the statistically insignificant interaction effects involving Religious affiliation with Medicare Only and with Medicaid and Medicare.
DISCUSSION
There were no differences in pain medication stress within insurance categories based on whether patients were known to have a religious affiliation. One explanation may be that patients may be seeking alternative assistance from clergy late during their illness. Thus, clergy may be making late referrals to the palliative care program, when pain and symptoms are likely to be full blown and more difficult to control than had they been managed consistently all along.
Late referrals involving clergy may be a consequence of physicians and other health providers either making late referrals or failing to consider palliative care at all. In the Japanese study cited earlier,11 late referrals to specialized palliative care services occurred because 1) physicians did not want to refer “too early,” and 2) physicians, patients, and family members avoided discussion about palliative care to manage increasingly debilitating pain and symptoms. It is also possible that clergy may be missing opportunities to refer patients earlier; in-service education with clergy might be effective.
The limitation of low statistical power to detect 3 of the 4 interactions predicting pain medication stress suggests that such an interpretation should be made cautiously. Nevertheless, this limitation may not be a major practical concern given that there is an acceptable level of power to detect one of the effects (i.e., Religious affiliation × Medicare Only). If any of the remaining interaction effects are real, the insufficient power to detect them would still correspond to their being much lower in effect size than the interaction effect between Religious affiliation and Medicare Only (which proved insignificant). Therefore, if any genuine interactions effects were missed, they are likely to be much less useful as clinical distinctions.
Although religious affiliation is not associated with differences in pain medication stress across insurance categories, Medicaid patients with a religious affiliation do report less hopeful pain and symptom attitudes, which could be associated with a lack of social support, more advanced stage of illness, or symptom burden. Patients with few resources may especially seek help from religious institutions, and palliative care referrals by clergy of uninsured individuals are likely to qualify for Medicaid coverage when there is a need for medications to control pain and other symptoms. Indeed, 2 bivariate analyses suggest that patients covered only by Medicaid are somewhat more likely to be taking pain medications than are other patients (χ2 Fisher exact test, P = .069; Spearman rank correlation = 0.16, P = .053).
Conversely, uninsured patients with a religious affiliation disclose more hopeful pain and symptom attitudes. A greater sense of hope could stem from their experience of being successfully referred by clergy to the palliative care service, especially when being uninsured had created past difficulties in gaining access to health care. This explanation appears plausible, especially since pain medication stress by uninsured patients was not predicted to be lower among those with a religious affiliation (Table 4).
The more hopeful attitudes among uninsured patients with a religious affiliation are less likely to be due to anticipation of future Medicaid coverage for pain and other medications, based on their participation in the process of completing a Medicaid application. The anticipation of future Medicaid coverage is an unlikely explanation because more hopeful attitudes would also be expected for uninsured patients without a religious affiliation. (Instead, while statistically significant, the regression coefficient in Table 4 for Uninsured has the opposite sign to that for Religious affiliation × Uninsured, reflecting less hopeful attitudes in uninsured patients without a religious affiliation).
Uninsured patients were more likely to become eligible for Medicaid once a need for palliative care was demonstrated. Some patients may be uninsured because of drug and alcohol problems, homelessness, and other issues that suggest the potential for difficulties in cooperating with the social worker during the Medicaid application process. Uninsured patients may be less able to take advantage of formal support, and more likely to drop out of the palliative care program, although the majority of uninsured clients were more recently admitted (i.e., too early for completion and approval of Medicaid applications). In the Latino community, perhaps a tradition of trusting and seeking support from American clergy and religious institutions might not be as well developed as in the African American community, especially among undocumented immigrants, who may fear the process of applying for Medicaid.
Although religiosity or specific religious beliefs may foster coping, the simple affiliation of patients with religious institutions and clergy may also foster coping. This process involves receptivity and outreach by religious institutions, not only within their faith communities, but beyond them, into local neighborhoods and service communities (e.g., soup kitchens, homeless services). Outreach efforts may also be working in reverse, in which individuals who are disenfranchised and economically disadvantaged (or others on their behalf) may seek out religious affiliations as medical conditions and symptoms become more serious.
Limitations
There may be self-selection among uninsured patients in seeking out, or being sought out by, religious institutions. Uninsured patients experiencing a need for pain medication could more easily qualify for Medicaid coverage, which would be pursued by the social worker in order to reduce patient financial burden and to increase institutional reimbursement. However, it is unclear whether uninsured patients were sought out as readily for referral to the palliative care service when symptoms were experienced that were less likely to be managed with medications. Perhaps such patients might not qualify as readily for Medicaid. Similar concerns pertain to patients experiencing homelessness or addiction problems, who may find it difficult to follow through with medication regimens or with insurance application requirements. Conversely, the data had already been collected as a required part of receiving clinical care; the current study is afforded with a more representative sample than a prospective study would provide.
The broad term “religious affiliation” comprises a wide diversity of patients, including those who 1) have strong religious beliefs and practices, 2) attend religious services and social functions, and 3) became part of the religious referral network because of serious unmet health care needs. Unfortunately, data on clergy referrals could not be obtained.
There may be different interpretations in the meanings of Pain Attitude and Symptom Attitude, the 2 variables that comprise the Pain and Symptom Attitude index. Both of these variables are measured using a 3-category, ordinal scale, in which pessimistic/fearful and hopeful are labels for the extreme categories. Some patients may interpret feeling hopeful in terms of their capacity to endure or cope with pain and symptoms, while others may emphasize expectations of relief from pain and symptoms. Prayer and faith in God may result in hopefulness and comfort, but others may refuse pain medication because they believe that their suffering helps atone for past sins, or out of a belief that their suffering is God’s will, which they should patiently accept. The Medicaid variable represents a heterogeneous group of patients. The data were collected after the patients were in the palliative care program; some patients, however, might have had Medicaid coverage for quite some time before admission, whereas others became eligible for Medicaid after admission.
The absence of a pain variable as a predictor of pain medication stress and of pain and symptom attitude is an important limitation—pain affects difficulty with pain medication and may directly influence pain attitude. As an indicator of continuing need for palliative care, the length of stay predictor may account for some multivariate effects attributable to pain and other symptoms. R-square values may also be attenuated by the preponderance of dummy variables and crude ordinal variables as predictors.
Implications
An intriguing possibility may help explain our findings. Certain aspects of religious affiliations might generate effects similar to a recently reported guided imagery intervention, which successfully changed the meaning of pain so that it was no longer perceived as “never-ending.”17 Religious imagery also might shift pain and symptom attitudes to be more positive and hopeful among uninsured patients who recently gained access to palliative care. The more hopeful pain and symptom attitudes in uninsured patients with a religious affiliation, however, may mask actual problems. That is, more hopeful attitudes could actually make it more difficult for caregivers, clergy, and health providers to become aware of the full scope of pain, symptom, and medication difficulties. It is unclear whether uninsured patients with more hopeful pain and symptom attitudes tend to develop less hopeful attitudes once they gain Medicaid coverage, and/or whether less hopeful attitudes stem from other patients who were already covered by Medicaid upon admission to the palliative care program.
Since religious affiliation did not predict reduced pain medication stress within any of the health insurance subgroups, the study did not reveal indirect evidence that would suggest that social or instrumental support from clergy or religious institutions helped reduce difficulties with pain medications, beyond facilitating access and admission to the palliative care program. Normally, this explanation would have derived additional support from the fact that additional interactions based on Religious Affiliation and the variable, Patient Unaware of Prognosis, were statistically insignificant (findings not shown). However, since prognoses can be positive, negative, or uncertain, the variable Patient Unaware of Prognosis appears to be too broadly construed (i.e., a better, targeted variable would have been Patient Unaware of a Negative Prognosis). Therefore, our inability to reveal indirect evidence should not be taken to mean that religious, social, or instrumental support by clergy or religious institutions was nonexistent or ineffective.
Still, despite its broad construction, this variable may be reflecting certain trends within the main effects regressions. After controlling for the remaining predictors, Patient Unaware of Prognosis predicts lower pain medication stress (Table 3) but less hopeful pain and symptom attitudes (Table 4). Conversely, Pain Medication Stress predicts more positive pain and symptom attitudes (Table 4).
These divergent findings may reflect the role of caregivers who assume greater responsibility for managing pain medication as illness becomes more debilitating and patients experience cognitive decline, which could be associated with their being unaware of their prognosis. (The salience of cognitive decline in older patients is suggested by the correlation between Medicare Only and Patient Unaware of Prognosis in Table 2). Patients with cognitive decline may experience low levels of pain medication stress even as they feel less hopeful about pain and symptom control and their illness prognosis. With fatigue and cognitive decline, they may become less capable of communicating their pain and symptom needs to caregivers. In contrast, patients at earlier illness stages may experience more effective pain and symptom control even as they encounter difficulties in managing their pain medication.
In summary, inner city African American and Latino patients affiliated with a religion reveal more hopeful pain and symptom attitudes when they are uninsured and less hopeful attitudes when they are covered only by Medicaid. Palliative care programs should carefully consider how best to integrate religious support networks as pipelines for program referrals and potential partners for supportive care and psychosocial interventions.
Acknowledgments
We thank Liz Alvarado, MSW, and Eno Onda, RN, for their efforts in data collection, and Debra Burns for creating the SPSS data file and conducting preliminary analyses.
Footnotes
Presented at Exploring Models to Eliminate Cancer Disparities Among African American and Latino Populations: Research and Community Solutions, Atlanta, Georgia, April 21–22, 2005.
Supported by Grant funding from a Social Work Leadership Development Award (Project on Death in America (Open Society Institute)); The National Institute of Mental Health and The Hartford Geriatric Social Work Faculty Scholars Program.
References
- 1.Link BG, Phelan JC. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(Extra Issue):80–94. [PubMed] [Google Scholar]
- 2.Williams BR. Dying young, dying poor: A sociological examination of existential suffering among low socioeconomic status patients. J Palliat Med. 2004;7:27–37. doi: 10.1089/109662104322737223. [DOI] [PubMed] [Google Scholar]
- 3.Gibson R. Palliative care for the poor and disenfranchised: A review from the Robert Wood Johnson Foundation. J R Soc Med. 2001;94:486–489. doi: 10.1177/014107680109400921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonham VL. Race, ethnicity, and pain treatment: Striving to understand the causes and solutions to the disparities in pain management. J Law Med Ethics. 2001;29:52–68. doi: 10.1111/j.1748-720x.2001.tb00039.x. [DOI] [PubMed] [Google Scholar]
- 5.Sambamoorthi U, Walkup J, McSpiritt E, Warner L, Castle N, Crystal S. Racial differences in end of life care for patients with AIDS. AIDS Public Policy J. 2000;15:136–148. [PubMed] [Google Scholar]
- 6.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. JAMA. 2000;284:2518–2521. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 7.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end of life care among inner city African Americans and Latinos. J Palliat Med. 2004;7:247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 8.Krakauer E, Crenner C, Fox K. Barriers to optimum end of life care for minority patients. J Am Geriatr Soc. 2002;50:182–190. doi: 10.1046/j.1532-5415.2002.50027.x. [DOI] [PubMed] [Google Scholar]
- 9.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 10.Field A, Maher P, Webb D. Cross cultural research in palliative care. Soc Work Health Care. 2002;35:523–543. doi: 10.1300/j010v35n01_10. [DOI] [PubMed] [Google Scholar]
- 11.Morita T, Akechi T, Ikenaga M, et al. Late referrals to specialized palliative care service in Japan. J Clin Oncol. 2005;23:2637–2644. doi: 10.1200/JCO.2005.12.107. [DOI] [PubMed] [Google Scholar]
- 12.Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48:1779–1789. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 13.Neighbors HW, Musick MA, Williams DR. The African American minister as a source of help for serious personal crisis: Bridge or barrier to mental health care? Health Educ Behav. 1998;26:759–777. doi: 10.1177/109019819802500606. [DOI] [PubMed] [Google Scholar]
- 14.Zuvekas SH, Taliaferro GS. Pathways to access: Health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Aff. 2003;22:2139–2153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 15.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 16.Francoeur RB. A flexible item to screen for depression in inner-city minorities during palliative care symptom assessment. Am J Geriatr Psychiatry. 2006;14:227–235. doi: 10.1097/01.JGP.0000194648.49784.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewandowski W, Good M, Draucker CB. Changes in the meaning of pain with the use of guided imagery. Pain Manag Nurs. 2005;6:58–67. doi: 10.1016/j.pmn.2005.01.002. [DOI] [PubMed] [Google Scholar]