Abstract
Background
propanil pesticide poisoning can produce methaemoglobinaemia, tissue hypoxia, and depression of CNS and respiratory system. It has been recorded only rarely worldwide and most current poison texts consider propanil to be of low toxicity. However, propanil self-poisoning is a significant clinical problem in parts of Sri Lanka and a not uncommon cause of death.
Aim of study
to report the clinical features and management of severe propanil poisoning.
Patients and Methods
we report a retrospective case series of patients who were treated in the intensive care unit (ICU) of and/or died in Anuradhapura General Hospital between 1998 and early 2002.
Results
sixteen patients were identified. Common manifestations of toxicity included confusion, reduced conscious level, cyanosis, and respiratory depression. Marked haemolysis was noted in several patients. Nine deaths occurred due to respiratory depression and cardiorespiratory arrest. Management was difficult given the lack of IV methylene blue, inability to measure methaemoglobin levels, and paucity of ICU beds.
Conclusions
this series indicates that propanil poisoning can be a severe form of self-poisoning, particularly in resource-poor settings. We have now initiated the establishment of a prospective series of propanil poisoned patients to further describe its clinical features, responsiveness to therapy, and case fatality rate.
Introduction
Pesticide poisoning is an important problem in parts of the developing world.1-4 While occupational and accidental poisonings are common,1,5 the majority of deaths follow deliberate self-poisoning.3,6-8 Organophosphorus (OP) pesticides are the most widely used and cause most deaths.3 However, other pesticides are significant problems in particular regions3 – for example, paraquat in the Caribbean and Pacific,9,10 the organochlorine endosulfan in South Asia,6,11,12 and propanil in Sri Lanka. This local epidemiology should determine requirements for treatment facilities, antidotes, and staff training in the management of acute poisoning.
Propanil [N-(3,4-dichlorophenyl) propanamide, see figure] is a contact herbicide used widely for rice cultivation. Propanil and its major metabolite, 3,4-dichloroanilide salt, induce the conversion of Fe2+ in haemoglobin to Fe3+, forming methaemoglobin (metHb) and lowering the blood’s oxygen carrying capacity. It is considered to be of low to moderate toxicity,13-16 with a quoted rat LD50 for the technical grade product of ∼1400 mg/kg14 or >2500 mg/kg.15,16 The literature suggests that it is a rare cause of poisoning – just eleven cases have been reported worldwide, from Sri Lanka (6 cases; of whom 2 died),17,18 Cuba (3 cases, no deaths)19 and Japan (2 cases; of whom 1 died).20,21 It is not covered in many toxicology handbooks16,22-24 or major toxicology textbooks.25
1.
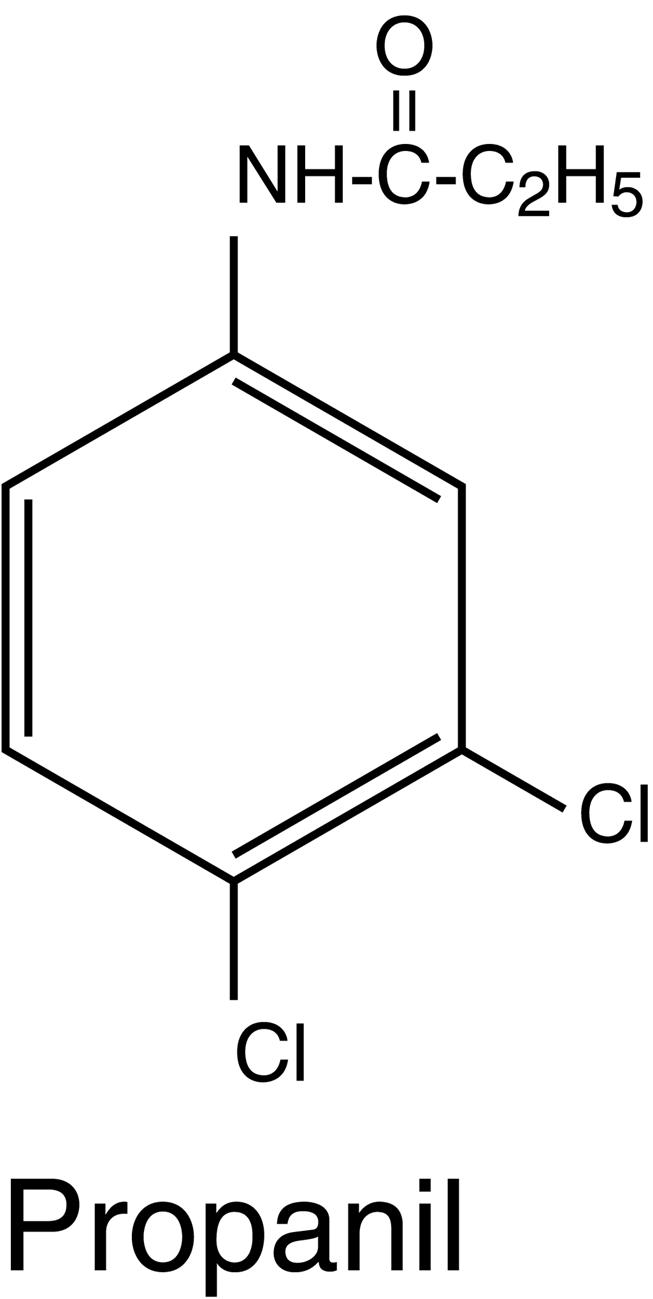
Chemical structure of propanil [N-(3,4-dichlorophenyl) propanamide].
Since 1995, we have worked in Anuradhapura, north central Sri Lanka, carrying out clinical trials on poisoning and envenomation. During this time, we have seen many patients admitted with propanil self-poisoning and noted it to be a significant clinical problem, at times requiring patient admission to the intensive care unit (ICU) and causing deaths. This study reports a retrospective case series of severe cases of propanil poisoning admitted to Anuradhapura General Hospital since January 1998. This series belies the mild-to-moderate toxicity label that is typically ascribed to propanil.
Patients and Methods
Anuradhapura General Hospital is a secondary referral centre for 950,000 people, mostly rural farmers, living in the Anuradhapura district of Sri Lanka’s North Central Province and the primary health centre for the 25-50,000 people living in and around the town of Anuradhapura. It also receives patient transfers from secondary hospitals to the north and east (in particular from Mannar, Vavuniya, and Polonnaruwa districts). The hospital has 1070 beds; there are 194 general medical beds with over 150% bed occupancy staffed by two consultant physicians, four medical SHOs (residents) and 6-8 interns. There is no emergency department, adult patients being transferred directly to the medical wards which receive around 1800 poisoning cases each year, more than 95% of which are intentional and 60% with pesticides (ref. 3 and unpublished results).
Propanil poisoning is classified by the Sri Lankan Health Services as an ‘other pesticide poisoning’ (ie non-OP or carbamate) (ICD 10, T60.1-T60.9). As such, it is not possible to distinguish propanil cases from other causes of non OP/carbamate pesticide poisoning within hospital and national records. We therefore obtained the hospital notes for all ‘other pesticide poisoning’ deaths recorded at Anuradhapura General Hospital for the period January 1998 to March 2002.
These records were hand searched for propanil cases, the relevant notes reviewed, and information extracted. Before the introduction of a clerking proforma in early 2002, medical clerking was normally brief due to the large patient load, supplying few details, in particular of volume ingested or brand of propanil. All 16 patients were transfers from peripheral hospitals; bottles brought by patients were left at these hospitals and not available to the clerking doctor in Anuradhapura. A case was identified by the history from patient or relative, or diagnosis of propanil poisoning in the transfer letter, and clinical features consistent with the diagnosis.
The ICU admissions register from January 1998 to March 2002 was searched for cases of propanil poisoning. In some cases, the admitting diagnosis was entered as ‘poisoning’, with no further description, so it is likely that this method of finding cases understates the true number of admissions to ICU with propanil poisoning. It was often not clear from the notes how many days a patient was intubated during their stay on ICU. We therefore chose to determine the number of days on ICU since this could be double checked from notes and ICU register, and would cover cardiovascular complications of propanil poisoning (anaemia and hypotension) where intubation was not required.
Results
Between January 1998 and March 2002, propanil pesticide poisoning resulted in at least sixteen severe poisoning admissions to Anuradhapura General Hospital (table). Nine patients were admitted to the medical ICU; nine patients died, seven within 24hrs of admission and before admission to ICU. Marked variability in investigations and treatment was noted due to the lack of resources, including frequent unavailability of basic blood tests and IV preparations of methylene blue.
Table 1.
Patients admitted to Anuradhapura General Hospital between Jan 1998 and March 2002 who were either admitted to ICU or who died.
| Patient | Date | Age/Gender | Hrs post-ingestion to AGH | Clinical features | Investigations | Treatment | Days in ICU | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 03/98 | 65 /M | 5 | Deeply unconscious with dilated pupils. Bilateral creps, cyanosed. Arrested, intubated. CPR unsuccessful. | / |
PU: atropine, furosemide, IVI AGH: GL, MB po, antibiotics, intubated, O2 |
0 | Died 21hrs post-admission |
| 2 | 11/98 | ? / M | not known | Semiconscious. Small pupils. Alcohol ++. Respiratory distress and had cardiac arrest. | / |
PU: GL, furosemide, atropine, IVI AGH: MB iv, AA po, blood transfusion |
0 | Died 17hrs post-admission. |
| 3 | 11/98 | 32 / M | 3 | Unconscious, not initially cyanosed. While in ICU had respiratory arrest following end of IPPV. Also developed pneumonia. | Hb 13.2 |
PU: GL, IVI AGH: intubated, MB iv, AA po, blood transfusion 1 unit. ICU: 3 days IPPV, then again after resp. arrest, antibiotics |
4 | Discharged alive day 10. |
| 4 | 12/98 | 60 / M | 1.5 | Initially CVS stable. Then had cardiorespiratory arrest. | / |
PU: GL AGH: GL, IVI, O2, MB po, AA po. |
0 | Died 17hrs post-admission. |
| 5 | 01/99 | 35 / M | 2.75 | Cyanosed, respiratory depression (RR 7/min) requiring ventilation. Died from cardiac arrest in ICU. | / |
PU: FE AGH: GL, MB po, AA po, antibiotics ICU: intubation, ventilation |
3 | Died day 4. |
| 6 | 01/99 | 32 / M | 5 | Responsive only to pain in PU. Widespread lung creps. Cyanosed. Did not require ventilation | Hb 5.6 Bil 2.1 (D 0.9, I 1.2) |
PU: GL, furosemide AGH: GL, AC, MP po, antibiotics ICU: intubation and oxygen |
2 | Discharged alive day 6. |
| 7 | 02/99 | 72 / M | 2.75 | Drowsy, lung creps. Developed respiratory distress requiring intubation and ventilation. 22hrs later arrested. | / |
PU: GL AGH: GL, MB po, O2 |
0 | Died 23hrs post-admission. |
| 8 | 06/99 | 16 / F | 4 | Initially treated as OP, then became cyanosed. Responding only to pain. 16/40 pregnant — died in utero. Post-delivery, developed oedema and melaena. | Hb 6.4 Bil 3.3 (D 0.9, I 2.4) |
PU: GL attempted AGH: MB po, AA po ICU: 4 days IPPV, 3 days O2via T-tube, extubated day 8, blood transfusion, FFP. |
10 | Discharged alive day 20. |
| 9 | 10/99 | 19 / F | 14.5 | Initially presented to Polonnaruwa Base Hospital: central cyanosis, confused, Sats 80%. No ICU beds so transferred to AGH. Intubation not required. | Hb 11.2 SGPT 10 |
PU: GL AGH: MB po, AA po ICU: oxygen by face mask |
2 | Discharged alive day 5. |
| 10 | 11/99 | 45 / M | 3.75 | Unconscious, cyanosed, pinpoint pupils. CVS stable initially, then arrested. | / |
PU: GL AGH: GL, MB po, MB iv, O2 |
0 | Died 6.5hrs post-admission. |
| 11 | 12/99 | 25 / M | 1.75 | Unconscious, cyanosed, vomiting, lung creps. CVS stable initially. Later arrested. | / |
PU: GL AGH: GL, MB po, O2 |
0 | Died 3.5hrs post-admission. |
| 12 | 10/00 | 36 / M | 5.5 | Drowsy, central cyanosis (76% sats), dark urine, hypotensive | Hb 7.3, Retic 8% SGOT 112 SGPT 112 |
PU: GL, fluids AGH: GL, AC, MB po, AA po ICU: dopamine, intubated, 20hrs IPPV, blood transfusion |
7 | Discharged alive day 27. |
| 13 | 11/01 | 45 / M | 5.5 | Developed respiratory weakness. Initially treated as OP, then became cyanosed. | / |
PU: FE, atropine, IV fluids AGH: GL, AC, atropine ICU: O2 via nasal cannulae |
3 | Discharged alive day 3. |
| 14 | 05/01 | 52 / F | 2.25 | Cyanosed. Admitted to ICU on admission. Discharged back to ward after 3 days. Arrested 6 days later - ? cause | Hb 11.3 SGOT 66, SGPT 53 |
PU: FE, IVI AGH: AC, antibiotics, AA po, O2 ICU: O2 via nasal cannulae. |
Died day 9. | |
| 15 | 12/01 | 50 / M | 4 | Drowsy, vomiting, no cyanosis on admission. Developed respiratory failure for which transferred to ICU | / |
PU: refused GL and NG tube. Given atropine, furosemide, hydrocortisone, IVI AGH: GL, AC, IVI, MB po ICU: intubated, ventilated |
1 | Died day 3. |
| 16 | 03/02 | 15 / F | 1.45 | Admitted conscious to PU. Had small pupils so received atropine. Reduced GCS on admission to AGH, hypotensive and cyanosed | Hb 5.8 Bil 3.9 (D 1.5, I 2.4) SGPT 224 SGOT 73 |
PU: GL, atropine AGH: MB po, AA po, antibiotics. ICU: intubated, O2 via T-tube. Given blood transfusion |
9 | Discharged alive day 14. |
Abbreviations: AA, ascorbic acid; AC, activated charcoal, AGH, Anuradhapura General Hospital; SGPT, alanine transaminase; SGOT, aspartate transaminase; Bil, bilirubin (D - direct, I - indirect); CPR, cardiopulmonary resuscitation; FE, forced emesis; FFP, fresh frozen plasma; GCS, Glasgow coma score; GL, gastric lavage; Hb, haemoglobin; ICU, intensive care unit; IPPV, intermittent positive pressure ventilation; IVI, intravenous fluid infusion; MB, methylene blue; po, by mouth; OP, organophosphorus pesticide; PU, peripheral health unit/rural hospital; Retic, reticulocyte count.
Typical clinical features in these patients included confusion, reduced conscious level, cyanosis, and development of respiratory depression. Twelve patients required respiratory support: nine were intubated because of poor respiratory effort and six required mechanical ventilation. One died soon after intubation and before ventilation could be arranged; four patients had a cardiorespiratory arrest and died before instigation of intubation or ventilation. The 16 week old fetus of a pregnant woman died in utero; the mother survived the poisoning.
A full blood count was not recorded for many patients. However, two patients were noted to have had Hb levels between 5 and 6g/dl and required blood transfusion. Bilirubin concentrations were increased in the three patients it was measured in and a reticulocyte count of 8% was noted in one patient, both consistent with haemolysis. Alanine and/or aspartate transaminases were more than twice the upper limits of normal in two of the four patients in whom they were analysed. Blood gas analysis for measurement of methaemoglobin levels was not available in the hospital.
The majority received either forced emesis or gastric lavage on two occasions – on initial presentation to a peripheral hospital and again on admission to Anuradhapura, some three to six hours post-ingestion. Ipecacuanha was not available so forced emesis was performed by asking the patients to put their fingers down their throat after drinking water or sodium bicarbonate. Activated charcoal was given to four patients on presentation to the secondary hospital.
Specific management of these patients was constrained by a shortage of IV methylene blue preparations from late 1998 – only one patient receiving it IV. Instead, patients routinely received oral preparations of methylene blue (300mg daily) and ascorbic acid (1-2g bd) as the only available reducing agents.30 Five patients received a blood transfusion for anaemia but none received an exchange transfusion to lower metHb levels
Discussion
The world literature on acute propanil pesticide poisoning consists of eleven cases, suggesting that propanil is not a frequent cause of poisoning. It is also often described as being a mild form of poisoning, causing little serious toxicity.16,31 It is therefore perhaps hardly surprising that propanil poisoning is not mentioned in many toxicology books.
However, propanil poisoning is a significant clinical problem in parts of Sri Lanka and the sixteen severe cases presented in this paper belie the belief that it is a mild poison. Nine patients were admitted to ICU and nine patients died, seven before they could get to the ICU. The method of case finding means this is a series of severe poisonings only. Discussion with doctors in Anuradhapura and current rates of presentation indicate that around 40 patients are admitted in total each year, suggesting that as many as 150 patients may have been admitted during the same period with a case fatality rate of around 5%.
Propanil and its major metabolite, 3,4-dichloroanilide salt, induce the conversion of Fe2+ in haemoglobin to Fe3+, forming metHb. MetHb cannot bind O2 and therefore the O2 carrying capacity of the blood is decreased. MetHb levels less than 20% are usually asymptomatic although patients appear centrally cyanosed.26 Levels greater than 20% produce headache, lethargy and dizziness; further increases result in decreased consciousness, convulsions, shock and, above 70%, death.26 Metabolites of propanil may also cause a severe haemolytic anaemia with formation of Heinz bodies, exacerbating the MetHb-induced decrease in the blood’s O2 carrying capacity.27,28
Diagnosis may be made through history, measurement of metHb levels, or clinically through the typical combination of altered mental status, cyanosis, and dyspnoea.26 Treatment is with reducing agents, in particular IV or oral preparations of methylene blue,29 or by exchange transfusion. MetHb levels are useful for evaluating treatment efficacy.
The management of these patients was not ideal – intravenous methylene blue, a relatively cheap antidote which is the treatment of choice for methaemoglobinaemia of any cause, was available for only one patient (who died – see table). All others received oral preparations of methylene blue or ascorbic acid. Although apparently successful in de Silva’s case series,18 this treatment regimen is problematic for significant intoxications given the variability and unpredictability in bioavailability of the oral preparations.
It is estimated that an oral dose of 3-5mg/kg methylene blue PO is equivalent to 1-2mg/kg IV.29 Oral preparations have been used for mild, inherited causes of metHb with good effect, but the IV administration is generally recommended for acute symptomatic exposures. Duration of administration of methylene blue is dependent on the half-life of the ingested agent, and repeat dosing may be necessary.29 No human propanil toxicokinetic data has been published.26 Some researchers have suggested that methylene blue should be used with caution in aniline-induced metHb since it may exacerbate Heinz body formation and haemolytic anaemia. Repeat doses may thus increase haemolysis without further reducing metHb levels.32
Ascorbic acid may not be useful for acute metHb because of its slow onset of action. In addition, there appears to be a dose-limited absorption of ascorbic acid, with minimal plasma changes observed in doses in excess of 90-150mg daily. No advantage has been shown from daily intakes exceeding 200mg, with surplus amounts being eliminated unchanged through the kidney.29
MetHb levels could not be analysed and this may in part explain why exchange transfusion was not given to these patients. Treatment was often started on an empirical basis for OP poisoning (the most common pesticide poisoning locally) in small peripheral hospitals when it was not yet clear which pesticide had been ingested. Investigations were often difficult to perform, some assays requiring transport to laboratories in Colombo, with a 2 week turn around time.
It is not clear whether the deaths could have been prevented with IV methylene blue, better investigational facilities, and earlier admission to ICU. The ICU has four beds and is always full – mostly with poisoning and common krait (Bungarus caeruleus) snake bite patients who together occupy 60% of ICU beds.6 It is often very difficult to get a patient admitted and the patients must be managed on the open ward, where one to two doctors and three nurses look after more than 70 patients.
Eight patients received gastric decontamination on more than one occasion – on admission to both the peripheral unit and Anuradhapura. One patient refused gastric lavage at the peripheral hospital but received it in Anuradhapura four hours post-ingestion. Gastric lavage at the secondary hospital would have been performed more than two hours post-ingestion in all patients who received it, and in the majority (6/10) after more than four hours.
The practice of a second gastric lavage seems unlikely to benefit patients. Since commercial preparations of propanil are sold in Sri Lanka as a 30% emulsion or 50% aqueous solution, gastric lavage or forced emesis will increase the risk of aspiration of the solvent. The routine practice of gastric lavage in patients presenting more than four hours post-ingestion runs counter to recent recommendations of the US and European Clinical Toxicology Associations.33 However, as noted by doctors in Sri Lanka and India, all the studies used to formulate these guidelines were on poisoning with medicines and their relevance to pesticide poisoning is not clear.30,34
There are also difficulties in using activated charcoal since the lack of IV preparations requires the use of oral drugs. Activated charcoal might affect absorption of methylene blue or ascorbic acid and therefore possibly should not be given to patients with propanil poisoning until IV drugs become available. Although there are no studies of activated charcoal binding to propanil or its clinical effectiveness in propanil poisoning, the molecular weight of propanil (218.1) suggests that it should bind. It is currently not given on first presentation to a peripheral unit because of cost: 1600 Sri Lankan rupees (∼16USD) is considered too expensive for these peripheral units.
There have been no prospective case series of acute propanil poisoning describing case fatality rate or clinical features. Clinical features are based on small retrospective series and include gastrointestinal irritation (possibly a solvent effect), cyanosis, stupor and central respiratory depression,26,31 all features seen in our patients. However, the few details recorded in the case notes make it difficult to get a better picture. We have therefore now set up a prospective study to record clinical features, responsiveness to treatment, and case fatality rate of propanil self-poisoning.
Acknowledgements
we thank Sandya Basanayake, Udaye Rajakaruna, Ariyaworthi, Mahinda, and Chandrika of the Anuradhapura records office for their help in obtaining patient records, and Dr Asoka Munasinghe, Medical Superintendent, Anuradhapura Hospital, for permission to review them. ME is a Wellcome Trust Career Development Fellow in Tropical Clinical Pharmacology and a Foulkes Fellow. Funded by grant GR063560MA from the Wellcome Trust’s Tropical Interest Group to ME.
References
- 1.Dinham B. The pesticide hazard. A global health and environmental audit. London: Zed Books; 1993. [Google Scholar]
- 2.Van der Hoek W, Konradsen F, Athukorala K, Wanigadewa T. Pesticide poisoning: a major health problem in Sri Lanka. Soc Sci Med. 1998;46:495–504. doi: 10.1016/s0277-9536(97)00193-7. [DOI] [PubMed] [Google Scholar]
- 3.Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. Q J Med. 2000;93:715–31. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]
- 4.Karalliedde L, Eddleston M, Murray V. Organophosphates and health. London: Imperial College Press; 2001. The global picture of organophosphate insecticide poisoning; pp. 431–71. [Google Scholar]
- 5.Wesseling C, McConnell R, Partanen T, Hogstedt C. Agricultural pesticide use in developing countries: health effects and research needs. Int J Health Services. 1997;27:273–308. doi: 10.2190/E259-N3AH-TA1Y-H591. [DOI] [PubMed] [Google Scholar]
- 6.Eddleston M, Sheriff R, Hawton K. Deliberate self-harm in Sri Lanka: an overlooked tragedy in the developing world. BMJ. 1998;317:133–5. doi: 10.1136/bmj.317.7151.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Public health impact of pesticides used in agriculture. Geneva: WHO; 1990. [Google Scholar]
- 8.Besbelli N, International Programme on Chemical Safety Report of the second meeting of the advisory group of the epidemiology of pesticide poisoning project; 17-18 December 2001; Geneva, Switzerland: WHO Headquarters; 2002. [Google Scholar]
- 9.Bowles JR. Preventative strategies on suicide. Leiden: E.J.Brill; 1995. Suicide in Western Samoa. An example of a suicide prevention program in a developing country; pp. 173–206. [Google Scholar]
- 10.Daisley H, Simmons V. Forensic analysis of acute fatal poisonings in the southern districts of Trinidad. Vet Hum Toxicol. 1999;41:23–5. [PubMed] [Google Scholar]
- 11.Singh N, Singh C, Kumar H, Brar GK. Endosulfan poisoning: a study of 22 cases. J Assoc Physicians India. 1992;40:87–8. [PubMed] [Google Scholar]
- 12.Chugh SN, Dhawan R, Agrawal N, Mahajan S. Endosulfan poisoning in northern India: a report of 18 cases. Int J Clin Pharmacol Ther. 1998;36:474–7. [PubMed] [Google Scholar]
- 13.Pesticides. A safety manual. 2 edn. London: Shell International Chemical Company Ltd; 1983. [Google Scholar]
- 14.World Health Organization WHO recommended classification of pesticides by hazard and guidelines to classification 2000-2001. 2001. WHO/PCS/01.4. Geneva; WHO; [Google Scholar]
- 15.Farm chemicals handbook ′99. Willoughby, OH: Meister Publishing Company; 1999. [Google Scholar]
- 16.Reigart JR, Roberts JR. Recognition and management of pesticide poisonings. 5 edn. Washington DC: Office of Pesticide Programs, Environmental Protection Agency; 1999. Other herbicides; pp. 118–24. [Google Scholar]
- 17.Wijekoon PNB, Sivaramakrisna N, Nimalasuriya A. Acute haemolysis and renal failure in chlorinated hydrocarbon poisoning. Ceylon Med J. 1974;19:37–8. [PubMed] [Google Scholar]
- 18.De Silva WAS, Bodinayake CK. Propanil poisoning. Ceylon Med J. 1997;42:81–4. [PubMed] [Google Scholar]
- 19.Martinez Cabrera J, Velazquez Ogando R. Intoxicacion por sustancias metahemoglobinizantes. Estudio retrospectivo de 39 pacientes. Rev Cubana Med. 1998;37:77–82. [Google Scholar]
- 20.Yamazaki M, Terada M, Kuroki H, Honda K, Matoba R, Mitsukuni Y. Pesticide poisoning initially suspected as a natural death. J Forensic Sci. 2001;46:165–70. [PubMed] [Google Scholar]
- 21.Hori Y, Nakajima M, Fujisawa M, Shimada K, Hirota T, Yoshioka T. [Simultaneous determination of propanil, carbaryl and 3,4-dichloroaniline in human serum by HPLC with UV detector following solid phase extraction] Yakugaku Zasshi. 2002;122:247–51. doi: 10.1248/yakushi.122.247. [DOI] [PubMed] [Google Scholar]
- 22.Olson K. Poisoning and drug overdose. 3 edn. Stamford, CT: Appleton & Lange; 1999. [Google Scholar]
- 23.Henry J, Wiseman H. Management of poisoning. A handbook for health care workers. Geneva: WHO/UNEP/ILO; 1997. [Google Scholar]
- 24.Aggarwal P, Wali JP. Diagnosis and management of common poisoning. Delhi: Oxford University Press; 1997. [Google Scholar]
- 25.Kreiger RI. Handbook of pesticide toxicology. San Diego: Academic Press; 2001. [Google Scholar]
- 26.Fernando R, Widyaratna D. IPCS (PIM 440) Propanil. 1990. www.intox.org.
- 27.McMillan DC, Bradshaw T, Hinson J, Jollow D. Role of metabolites in propanil-induced hemolytic anemia. Toxicol Appl Pharmacol. 1991;110:70–8. doi: 10.1016/0041-008x(91)90290-u. [DOI] [PubMed] [Google Scholar]
- 28.McMillan DC, Bradshaw T, McMillian J, Hinson J, Jollow D. Contribution of 3,4-dichlorophenylhydroxylamine in propanil-induced hemolytic anemia. Adv Exp Med Biol. 1991;283:343–5. doi: 10.1007/978-1-4684-5877-0_44. [DOI] [PubMed] [Google Scholar]
- 29.Martindale: The Complete Drug Reference. 32 edn. London: Pharmaceutical Press; 1999. Methylene Blue. [Google Scholar]
- 30.Fernando R. Management of acute poisoning. 2 edn. Colombo, Sri Lanka: National Poisons Information Centre; 1998. [Google Scholar]
- 31.EXTOXNET. Pesticide information profile. Propanil. Extoxnet 1996
- 32.Harvey JW, Keitt AS. Studies of the efficacy and potential hazards of methylene blue therapy in aniline-induced methaemoglobinaemia. Br J Haematol. 1983;54:29–41. doi: 10.1111/j.1365-2141.1983.tb02064.x. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Clinical Toxicology. European Association of Poisons Centres and Clinical Toxicologists Position statement: gastric lavage. J Toxicol Clin Toxicol. 1997;35:711–9. doi: 10.3109/15563659709162568. [DOI] [PubMed] [Google Scholar]
- 34.Bhattarai MD. Gastric lavage is perhaps more important in developing countries [letter] BMJ. 2000;320:711. [PMC free article] [PubMed] [Google Scholar]


