Abstract
Bacillus anthracis is the causative agent of anthrax, and the spore form of the bacterium represents the infectious particle introduced into a host. The spore is surrounded by an exosporium, a loose-fitting membrane composed of proteins and carbohydrates from which hair-like projections extend. These projections are composed mainly of BclA (Bacillus-collagen-like protein of B. anthracis). To date, exact roles of the exosporium structure and BclA protein remain undetermined. We examined differences in spore binding of wild-type Ames and a bclA mutant of B. anthracis to bronchial epithelial cells as well as to the following other epithelial cells: A549, CHO, and Caco-2 cells; the IMR-90 fibroblast line; and human umbilical vein vascular endothelium cells. The binding of wild-type Ames spores to bronchial epithelial cells appeared to be a dose-dependent, receptor-ligand-mediated event. There were similar findings for the bclA mutant, with an additional nonspecific binding component likely leading to significantly more adherence to all nonprofessional phagocytic cell types. In contrast, we detected no difference in adherence and uptake of spores by macrophages for either the wild-type Ames or the bclA mutant strain. These results suggest that one potential role of the BclA fibers may be to inhibit nonspecific interactions between B. anthracis spores with nonprofessional phagocytic cells and thus direct the spores towards uptake by macrophages during initiation of infection in mammals.
Bacillus anthracis, a gram-positive, spore-forming bacillus, is the causative agent of anthrax (11, 25). The spore structure of B. anthracis consists of overlapping layers called the core, cortex, coat, and exosporium (9). The central interior of a spore, known as the core, houses the chromosome. The cortex is a thick layer of peptidoglycan that surrounds the core (27), which is then further enveloped by the spore coat (1). The outermost structure of the B. anthracis spore is a loose-fitting exosporium (12). Approximately 20 exosporium-associated proteins and glycoproteins have been identified from analyses of B. anthracis and Bacillus cereus spores (4, 5, 29, 35-39). The exosporium membrane projects hair-like fibers (12) of which the major component is the BclA glycoprotein (35, 37).
Fibers of the B. anthracis exosporium were once believed to be important for virulence or adherence to host cells (20). However, several studies have demonstrated that the fibers and exosporium are not necessary for full virulence of B. anthracis. Upon identifying the BclA protein, Sylvestre et al. (37) examined the effect of a bclA mutation on the virulence of the attenuated Sterne strain of B. anthracis. In this first study, when spores were administered subcutaneously to mice, no appreciable differences in virulence were observed between the parental Sterne and bclA mutant strains (37). We recently showed that by using a fully virulent strain of B. anthracis, an Ames bclA mutant retains complete virulence in mouse and guinea pig models of anthrax infection (3). Furthermore, Ames mutant spores devoid of an exosporium derived through inactivation of the CotE protein are also as virulent as wild-type spores in guinea pigs and mice (13).
The exact role, if any, for the B. anthracis exosporium in pathogenesis or in the environment remains unknown. However, in a previous study from our laboratories, while following the trafficking of Ames and bclA mutant spores out of the lungs of mice, we noticed that there was a delayed clearance of bclA mutant spores (3). One potential and logical reason for this delay is that spores devoid of the BclA fibers simply bind better to lung epithelium. In this study, we further examined the ability of bclA mutant spores to bind various cell lines. Our results revealed that bclA mutant spores adhered much better to various nonprofessional phagocytic cell types than did wild-type Ames spores. Binding of wild-type Ames spores to bronchial epithelial cells (BEC) apparently involved a novel, dose-dependent, receptor-ligand-mediated event. Although there also seemed to be specific binding of the bclA mutant spores to BEC, there was evidently a nonspecific component mediating spore-cell interactions. In contrast, there was no difference in spore adherence or phagocytosis between wild-type and bclA mutant spores by macrophages.
MATERIALS AND METHODS
Strains and medium.
The fully virulent Ames wild-type strain (23) and Ames-JAB-12, a bclA mutant strain (3), were used for all studies. The bclA mutant strain was obtained by allelic exchange using shuttle vector pEO-3 (24), with the bclA gene replaced with the Ωkan-2 resistance gene (26). After steps to integrate the plasmid into the chromosome (24), kanamycin resistance clones were selected and several were also sensitive to erythromycin (present on pEO-3). Analysis revealed that allelic exchange occurred during this initial step (3). To obtain spores, cultures were sporulated in Difco sporulation medium (34). For purification, the spores were washed with water three times, centrifuged through a Hypaque-76 gradient (Nycomed, Inc., Princeton, NJ), and then washed three times again (4). Immediately before use, the spores were heat activated (65°C for 30 min) and then held on ice.
Cell culture.
The interaction between Ames or bclA mutant spores and eukaryotic cells was examined using several cell lines. Cells, seeded (2.5 × 105 cells/well) into 24-well plates containing glass coverslips, were cultured for 2 to 3 days (37°C; 5% CO2), at which time the cells had formed confluent monolayers. 16HBE14o− (15), a human BEC line, was grown in bronchial epithelial growth (BEG) medium (Cambrex Corporation, East Rutherford, NJ). All other cells used in this study were obtained from the American Type Culture Collection (Manassas, VA). Other epithelial lines included human lung carcinoma (A549), Chinese hamster ovary (CHO), and human colorectal (Caco-2) cells. A549 and Caco-2 cells were maintained in minimum essential medium (Eagle) and Earle's balanced salt solution with nonessential amino acids (EMEM/NEAA) supplemented with 5% fetal bovine serum (FBS). CHO cells were grown in EMEM/NEAA supplemented with 10% FBS and 1% sodium pyruvate. Human lung fibroblasts (IMR-90) were cultured in EMEM/NEAA containing 10% FBS. Murine macrophage-like cell lines (RAW264.7, J774A.1, and MH-S) were cultured as follows: RAW264.7 cells in Dulbecco's modified Eagle's medium (DMEM) supplemented with high glucose, 10% heat-inactivated FBS, and 1% sodium pyruvate; J774A.1 cells in DMEM containing high glucose, 10% heat-inactivated FBS, plus 1.5 g/liter sodium bicarbonate; and MH-S cells in RPMI 1650 medium containing high glucose, 5% heat-inactivated FBS, 1% HEPES, and 1% sodium pyruvate. Human umbilical vein vascular endothelium cells were maintained in MCDB 105 medium supplemented with 10% FBS, 3% endothelial cell growth supplement, 25 mM HEPES, and 10 U heparin/ml of medium.
Spore adherence assays with nonprofessional phagocytic cells.
Spores were added to the cells at indicated multiplicities of infection (MOIs). Cells were infected in the appropriate medium for each cell type, except horse serum was substituted for FBS, as needed, to delay spore germination (41). To promote spore binding, the cell-spore culture plates were centrifuged (260 × g for 10 min, 4°C) and then incubated an additional 60 min at 37°C in 5% CO2. After incubation, the coverslips were removed and rinsed aseptically in a series of three beakers containing phosphate-buffered saline (PBS). For each experiment, three coverslips were examined for every sample and experiments were performed in triplicate unless stated otherwise. Adherence was measured by viable counts or microscopy. Viable counts were determined by first lysing adherent cells in distilled water containing 0.1% Triton X-100 and then plating dilutions of the lysate in duplicate onto LB agar plates. Adherence was also demonstrated by immunofluorescence (IFM) and light microscopy. Samples were fixed in formalin, stained with immunofluorescent dyes (as described below) or spore stain (malachite green), and then counterstained with a Wright-Giemsa stain (Diff-Quik) (44).
BEC intracellular assays.
To determine whether spores of B. anthracis could be taken intracellularly into BEC and, if taken up, whether the number of bclA mutant spores was increased versus the number of Ames wild-type spores, the mammalian cells were incubated with B. anthracis spores as described above. After incubation, the wells were washed 10 times in PBS to remove free spores from the cell-associated ones. Cells were then incubated in medium containing 10% FBS (to promote spore germination), 5 μg/ml of cytochalasin D (to prevent further phagocytosis), and 2.5 μg/ml of gentamicin (to kill residual, noninternalized germinated spores in the medium). Viable counts were determined as described above. Further measurement of the intracellular spore number was obtained by IFM (7, 41). Briefly, coverslips were incubated with a rabbit antibody prepared against either irradiated killed Ames or bclA mutant spores (43). Coverslips were then incubated with secondary antibodies (anti-rabbit immunoglobulin G) conjugated with green (fluorescein isothiocyanate) or red (tetramethyl rhodamine isocyanate) fluorescent tags and added either before or after BEC permeabilization as previously described (7, 41). The stained coverslips were inverted onto glass slides with Vectashield (Vector Laboratories, Burlingame, CA) mountant, which also contained the DAPI (4′,6′-diamidino-2-phenylindole) nuclear stain in order to identify BEC.
Spore treatment.
For irradiation, spores (approximately 1 × 1010 CFU/ml) were exposed to 4 × 106 rads and killing was confirmed by plating aliquots of the treated spores onto sheep blood agar plates. The treated spores were then used as described above to assay for adherence to BEC. Adherence was assessed by microscopic observation of the infected cells stained with malachite green and counterstaining of the BEC. For enzymatic digestion, spores (approximately 1 × 1010 CFU/ml) were treated for 30 min at 37°C in PBS with 10 mg/ml of trypsin or papain (Sigma-Aldrich, St. Louis, MO). The activity of trypsin and papain under these conditions was measured by the EnzChek protease assay kit (Invitrogen, Carlsbad, CA). After treatment, trypsin was inactivated by Complete EDTA-free, protease inhibitor cocktail tablets (Roche Diagnostics Corporation, Indianapolis, IN) according to the manufacturer's instructions and the spores were then washed several times in distilled water. Papain was inactivated by heating at 80°C for 20 min. Spores were examined after protease or papain treatment by phase contrast microscopy to rule out any germination or clumping effects.
Competitive binding assay.
Irradiated spores of either the Ames wild type or bclA mutant were first added to cytochalasin D-treated BEC at an MOI of approximately 0, 20, 100, or 500 spores for one cell, followed by a brief centrifugation as described above. To further enable binding, the cells were then incubated for 30 min at 37°C with 5% CO2. Live Ames or bclA spores were then added at an MOI of approximately 20 to 40 for one cell, and then the spore-plus-cell mixture was centrifuged and incubated for an additional 30 min at 37°C with 5% CO2. The coverslips were then washed, and the BEC were lysed to determine CFU counts of the adherent viable spores. Additional studies for competitively inhibiting spore binding were carried out with both live and irradiated spores added simultaneously to BEC.
Electrophoretic analysis.
Extracts from B. anthracis spores were prepared as previously described (13), except the spores were heated at 70°C instead of 100°C. The extracts were then analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis using 12% Bis-Tris Gel NuPAGE mini-gels (Invitrogen) (22). After electrophoresis, the gels were stained with GelCode Blue (Pierce, Rockford, IL) for total protein or reacted with the GelCode glycoprotein stain (Pierce) to detect glycoproteins or the separated proteins were transferred to polyvinylidene difluoride membranes for immunoblot analysis. To detect the BclA protein along with other spore antigens by immunoblot analysis, whole-spore polyclonal antibody (43) was used as the primary antibody at a dilution of 1:5,000. The blots were then reacted with goat anti-rabbit immunoglobulin G conjugated with horseradish peroxidase as the detecting antibody (Pierce) and 4-chloronaphthol/3,3′-diaminodbenzidine (Pierce) for colorimetric detection of horseradish peroxidase with imidazole/cobalt chloride enhancement.
EM.
Standard methods for both transmission electron microscopy (TEM) and scanning electron microscopy (SEM) were employed. For the EM studies, BEC were infected with either Ames spores (an MOI of 38 for one cell) or bclA mutant spores (an MOI of 44 for one cell) and incubated as described above. The samples were then washed and either fixed or added to fresh medium and then fixed following an additional incubation period. The glass coverslips containing BEC with attached spores were fixed with 1% glutaraldehyde and 4% formaldehyde in Mallonig's buffer for several days at 4°C. Postfixation was performed for 1 h at room temperature in Mallonig's buffer containing 1% osmium tetroxide and then 30 min in 2.5% uranyl acetate. Cells were additionally processed through a series of ethanol rinses. For SEM, the samples were processed through hexamethyldisilizane rinses, mounted onto stubs, sputter coated, and then examined with a SEM Hitachi S-3400. For TEM, the samples were embedded into Spurr's embedding medium overnight at room temperature. Cells were removed by incubation in hydrofluoric acid to dissolve the glass coverslips, and the samples were then sectioned into 90-nm sections. These sections were counterstained with uranyl acetate and Reynold's lead citrate (30). The sections were examined using a Jeol 1230 transmission electron microscope.
Macrophage assays for spore phagocytosis and adherence.
The macrophage-like cell line RAW264.7, cultured on coverslips contained in 24-well plates, was used for in vitro phagocytosis and intracellular spore viability assays as described previously (41, 42). Spores were added at the indicated MOI concentration. To promote spore binding and phagocytosis by the macrophages, cell-spore culture trays were centrifuged (260 × g for 30 min) and then incubated an additional 30 min at 37°C under 5% CO2. After incubation, the wells were washed 10 times in PBS to remove free spores and then incubated in DMEM with horse serum (10%), cytochalasin D (5 μg/ml), and gentamicin (2.5 μg/ml). The wells were washed five more times with PBS, and the coverslips were then removed and washed aseptically in a series of three beakers containing PBS. Phagocytosis and viability were assayed bacteriologically by viable count determinations and light microscopy as well as IFM (7, 41, 42). For macrophage adherence assays, spores were added to macrophages pretreated with cytochalasin D and then tested as described above.
Statistics.
Upon comparing the association between the wild-type and mutant spores to macrophages, statistical significance (P < 0.05) was determined by the two-tailed Student t test using GraphPad Prism software (GraphPad, San Diego, CA).
RESULTS
Interaction of spores with BEC.
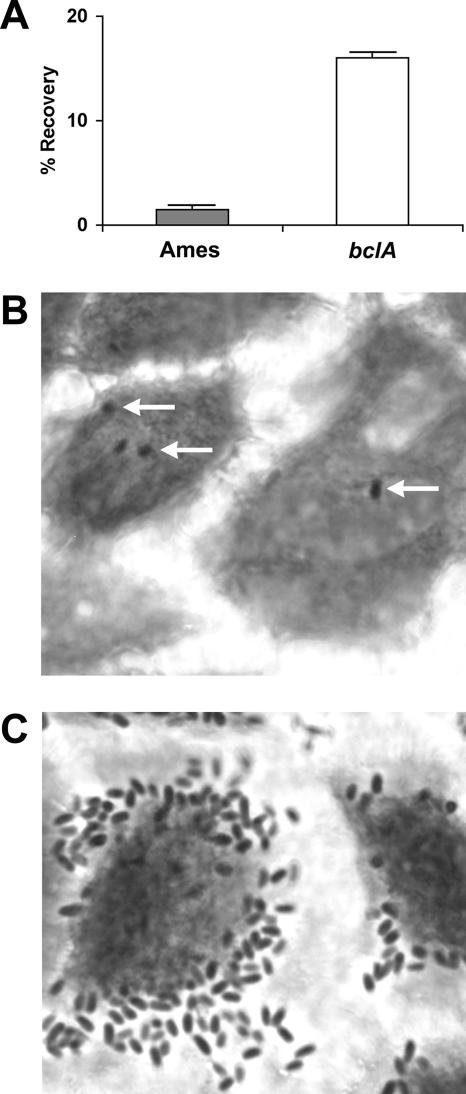
The binding of parental Ames strain and bclA mutant spores to cultured BEC was initially measured by determining the number of recovered CFU after a 1-h incubation of spores with BEC. As shown in Fig. 1A, 16% of the bclA mutant spores were recovered from BEC, in contrast to only 2% recovery of Ames wild-type spores. Control assays were also performed with spores incubated in either conditioned or nonconditioned BEG medium in the absence of BEC. The spores did not form aggregates in either medium (data not shown). In addition, binding assays were performed in the same media, where the spores were added to coverslips without BEC, briefly centrifuged, and incubated for 1 h. Following the standard washing procedures under these conditions, we did not observe (by phase contrast microscopy) any aggregates of either the wild-type Ames or bclA mutant spores binding to the coverslips (data not shown).
FIG. 1.
Association of spores to BEC. (A) BEC were incubated with either Ames wild-type (MOI of 32 to 50 spores for one BEC) or bclA mutant spores (MOI of 21 to 47 spores for one BEC) for 1 h. Following this incubation, the cells were washed and lysed and the bacteria were plated upon LB agar plates. The percent recovery of spores was determined by dividing the number of CFU counts from the lysed cells by the number of spores added. The difference between spore types associated with the BEC was significant (P = 0.0005). Error bars represent the standard errors of the means from three independent experiments. (B and C) Micrographs of spores associated with BEC. Samples were stained with spore stain (malachite green) and counterstained with a Wright-Giemsa stain. (B) Ames spores (indicated by white arrows) with BEC. (C) bclA mutant spores with BEC.
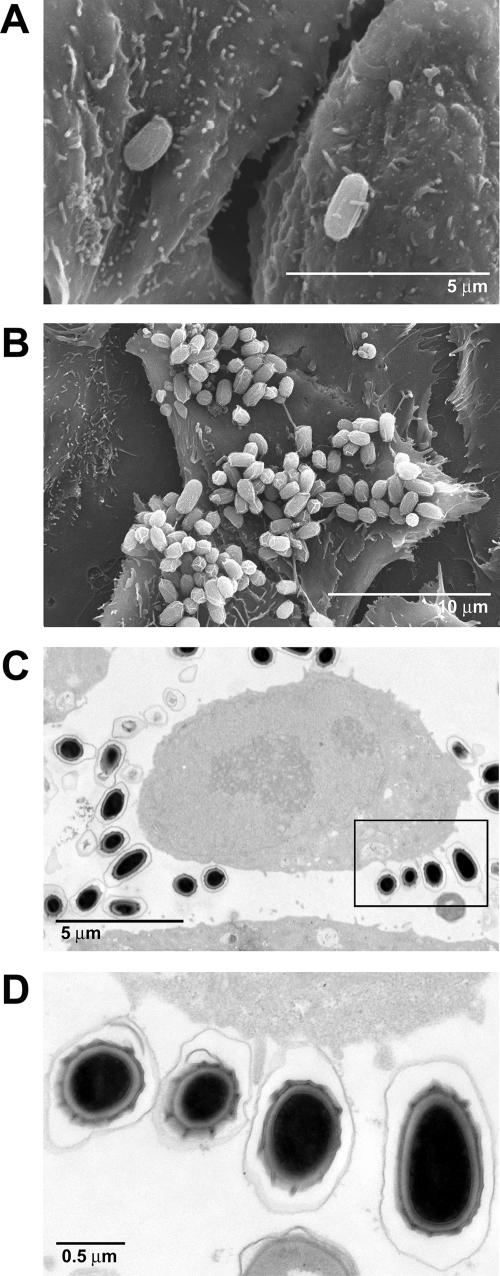
To further verify this significant difference, BEC infected with spores were stained with malachite green and counterstained with Wright-Giemsa (Fig. 1B and C). This increased binding was more closely examined by SEM and TEM analysis (Fig. 2). Very few Ames wild-type spores were found associated with the BEC (Fig. 2A), a striking contrast to the interaction observed with bclA mutant spores when incubated with BEC (Fig. 2B to D). Most of the epithelial cells were surrounded by, and in association with, the mutant spores. As shown in Fig. 2C and D, filopodia were observed projecting from the BEC and making contact with the spores.
FIG. 2.
SEM and TEM micrographs of the interaction between B. anthracis spores and BEC. (A) Adherence of Ames spores to BEC 2 h postinfection. (B) Adherence of bclA mutant spores to BEC 2 h postinfection. (C) bclA mutant spores incubated with BEC. (D) Close-up view from boxed area of panel C.
We tested the effect of BEC age on the level of spore binding by plating approximately 2.5 × 105 cells and growing them to confluence in approximately 5 days versus that of plating at 5 × 105 cells/ml and incubating them overnight before adding spores. For the confluent BEC obtained by either method, we still witnessed increased binding of the bclA mutant versus wild-type spores (data not shown).
Modification of spores and interaction with BEC.
To determine whether the increased adherence we observed with bclA mutant spores was due to some product expressed by the spore while interacting with the BEC, both wild-type and bclA mutant spores were lethally irradiated. When using viable and irradiated spores, there was no difference in binding to BEC as per microscopy (data not shown). These results indicated that the increased adherence of bclA mutant spores to BEC was not due to the expression of germination-linked factors by the spores during this interaction.
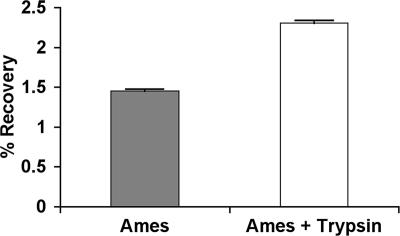
To determine whether altering exposed surface proteins on spores of the wild type or bclA mutant affected binding to BEC, spores were treated with trypsin. After this treatment, the spores were incubated with BEC for adherence assays. Trypsin treatment of the spores did not affect bclA spore binding to BEC (data not shown). However, trypsin treatment of wild-type Ames spores led to a significant increase in binding to BEC, as demonstrated by viable counts (Fig. 3) and microscopy (data not shown). Similar results were also observed when pretreating Ames spores with papain (data not shown). The increased adherence was unrelated to changes in the amount or presence of outer spore proteins. This was determined by TEM or trypsin treatment, followed by glycoprotein staining or Western blot analysis using serum against nongerminated Ames spores (43) (data not shown). Therefore, at this time we are uncertain of what specific effect trypsin or papain had on the spores that led to increased adherence to BEC. Perhaps the enzyme partially cleaved the BclA fibers or some other protein within the exosporium, thus resulting in digestion products undetectable by our analytical methods.
FIG. 3.
Interaction of BEC with Ames spores treated with trypsin. Cytochalasin D-treated BEC were incubated with either untreated Ames spores or trypsin-treated spores for 1 h at an MOI of 23 to 26 spores for one BEC. Following this incubation, the cells were washed and lysed and the bacteria were plated upon LB agar plates. The percent recovery of spores was determined, and the difference in the number of spores (with or without trypsin treatment) associated with the BEC was significant (P = 0.0003). Error bars represent the standard errors of the means from triplicate independent experiments.
Saturation and competitive binding studies.
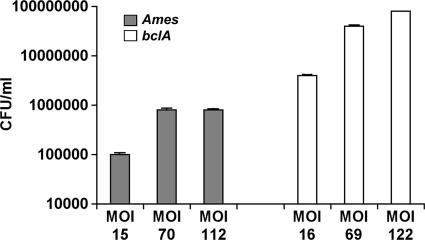
To determine whether spore binding to BEC could be saturated, cytochalasin D-treated BEC were incubated with spores at increasing MOIs. As shown in Fig. 4, the CFU recovered with Ames spores failed to increase at higher MOI levels. These results indicate that cell binding sites for Ames spores are fully occupied on BEC. Additional studies were also performed where the MOI level of Ames spores to BEC was increased from 150 to 300 for one cell. The recovered CFU again did not increase further, and such data suggest a saturable level of Ames spores binding to BEC (data not shown). If the binding sites on BEC are present at low levels, this may be responsible for the relatively low recovery of adherent Ames spores.
FIG. 4.
Saturation of the BEC binding sites for B. anthracis spores. Cytochalasin D-treated BEC were incubated with increasing MOI concentrations of either Ames wild-type or bclA mutant spores, and the numbers of adherent spores were determined by CFU counts. Error bars represent standard errors of the means from the CFU counts. Shown are representative results from an experiment performed in triplicate.
In contrast, the number of CFU recovered with the bclA mutant spores continued to increase with larger MOIs (Fig. 4). Saturation of the BEC surface was never reached in our experiments. These results suggest two possibilities. The first is that there are numerous binding sites for bclA mutant spores on the BEC, and they may not be saturated at the spore levels used for our experiments. The second is that bclA mutant spores may bind nonspecifically to BEC.
To determine whether spore binding to the BEC involved a specific receptor(s)-ligand(s) interaction, cytochalasin D-treated BEC were first exposed to varying MOIs (approximately 0, 20, 100, and 500 spores for one BEC) of either irradiated Ames wild-type or bclA mutant spores for 30 min. Next, live spores of the corresponding strain at a constant MOI were then allowed to adhere for 30 min. The coverslips containing the BEC and spores were washed, and CFU counts representing the live spores were determined. From this assay and as suggested by our previous experiments, the live Ames spores bound to the BEC preincubated with the irradiated Ames spores at levels lower than that observed with the bclA mutant (Table 1). In addition, the binding observed with the Ames spores was more competitively inhibited in a dose-dependent manner as increasing levels of the irradiated Ames spores blocked binding of live spores (Table 1). These results indicated, as also suggested in Fig. 4, that Ames wild-type spores bound to BEC via a specific receptor(s) present on these cells.
TABLE 1.
Competitive binding of irradiated killed and viable Ames or bclA mutant spores to BECa
| Spores added to BEC | MOI of irradiated spores | CFU recoveredb | SE | % Viable spores binding to BECc |
|---|---|---|---|---|
| Ames | 0 | 1.7 × 105 | 8.4 × 103 | |
| Ames | 20 | 1.4 × 105 | 9.1 × 103 | 84.8 |
| Ames | 100 | 9.0 × 104 | 7.3 × 103 | 54.7 |
| Ames | 500 | 2.9 × 104 | 4.1 × 103 | 17.7 |
| bclA | 0 | 5.3 × 106 | 6.4 × 105 | |
| bclA | 20 | 4.4 × 106 | 4.5 × 105 | 83.0 |
| bclA | 100 | 4.2 × 106 | 3.5 × 105 | 78.6 |
| bclA | 500 | 1.6 × 106 | 1.6 × 105 | 28.4 |
Irradiated spores (Ames or bclA mutant) at increasing MOI (0 to 500) were added to cytochalasin D-treated BEC and allowed to adhere.
Following incubation with irradiated spores, viable spores (homologous strain) were then added to the BEC and allowed to interact with the cells. The calculated MOI for Ames spores was 38 for 1 cell and 23 for 1 cell for bclA mutant spores. Adherent viable spores were determined by CFU counts.
The percentage of viable Ames or bclA mutant spores binding to the BEC in the presence of increasing competitor was determined by dividing the CFU recovered with the addition of irradiated spores by the CFU determined with no added spores. A representative experiment is shown from triplicate independent assays.
The competitive binding experiments were repeated by simultaneously adding the irradiated killed and live spores to the BEC. We still observed an inhibition effect with the Ames spores, though it was not as dramatic. For this experiment, an MOI of 30 live spores for one BEC was added with either no competitor or competitor added at an MOI of 20, 100, or 500 irradiated spores for one BEC. We recovered the live spores at a level of 88% with an MOI of 20 irradiated spores compared to the recovery level (100%) with no competitor. When increasing the MOI of irradiated spores to 100 for one BEC, the recovery of live spores decreased to 76%. With the addition of 500 irradiated spores for one BEC, only 61% of the live spores were recovered. These results are from a representative experiment.
When we added live bclA mutant spores to BEC preincubated with varying levels of irradiated bclA spores, there was also competition for adherence observed but it was not as dramatic as that for wild-type Ames spores (Table 1). However, these results do suggest that binding of the bclA mutant spores to BEC also involves a specific component but the dynamics of the spore-host interaction differ from that of wild-type Ames spores. In our assay, there were approximately 30-fold more bclA mutant spores binding to BEC and, thus, the competitor may not have been as effective as it was in the Ames spore-based experiments. In any event, adherence of the bclA mutant spores to BEC may consist of both specific and nonspecific binding mechanisms.
Uptake of spores by BEC.
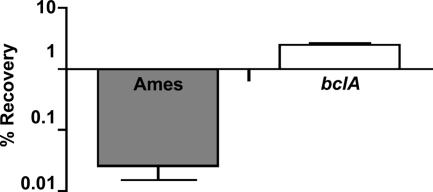
As the association of bclA mutant spores with the BEC was significantly higher than that for Ames spores, we next tested to see whether any of these spores were internalized by the BEC. To demonstrate uptake, we performed gentamicin protection assays with BEC that were incubated with either the Ames or bclA mutant spores for 1 h. After this incubation, the cells were incubated in medium containing FBS and gentamicin for an additional hour. As shown in Fig. 5, we observed low recovery levels (0.025%) of Ames spores that were not killed by the antibiotic and presumably taken up by the BEC. In comparison, the recovery level of the bclA mutant (2.4%) incubated with BEC was significantly higher (approximately 100 times) than that with Ames spores (Fig. 5). One possibility for this difference between strains could be that the bclA spores were slower to germinate than Ames and were therefore less susceptible to antibiotic killing. However, we previously demonstrated that spores of the bclA mutant were no different than Ames in germination ability (3). Control assays were performed with the spores in BEG medium alone for 1 h. For spores of either the Ames wild type or bclA mutant, little germination (<5%) was detected when they were incubated in the BEG medium as determined by heat sensitivity (data not shown). When the Ames and bclA mutant spores were next exposed to BEG medium with 10% FBS for 1 h, germination was measured by heat sensitivity and the levels of germination were more than 95% for both strains. Gentamicin resistance of the two cultures in the control experiment was measured at 4% for the wild type and 0.9% for the bclA mutant. These results indicated that increased recovery of the bclA mutant after incubation with BEC was due to spores located within the BEC and not delayed germination or differences in gentamicin sensitivity.
FIG. 5.
B. anthracis spores within BEC were recovered by gentamicin protection assays. BEC were incubated with either Ames wild-type or bclA mutant spores for 1 h at an MOI of 33 to 39 spores for one BEC. Following this incubation, the medium was replaced with that containing 10% FBS, 5 μg/ml of cytochalasin D, and 2.5 μg/ml of gentamicin. Cells were then lysed, the bacteria were plated, and the percent recovery of the intracellular spores was determined. A difference of spore numbers within the BEC was significant between strains (P = 0.0004). Error bars represent standard errors of the means from three independent experiments.
Intracellular location of the bclA mutant spores was further demonstrated by IFM. The number of spores adherent to, versus located within, BEC was distinguished by double-label fluorescent immunostaining. By using this assay, we determined that 7.0% ± 2.4% of the BEC contained intracellular bclA mutant spores versus only 0.2% ± 0.13% of the BEC that contained Ames wild-type spores (P = 0.04) from three separate samples.
Interaction with other epithelial cells.
To determine whether increased binding of bclA mutant spores was unique to BEC, adherence to other epithelial cells was characterized. We tested spore adherence to the A549 cells, a type II pneumocyte from humans. As seen with BEC, spores of the bclA mutant adhered at a significantly higher rate than did the wild-type Ames spores (Table 2). Likewise, this increased adherence was also observed with CHO and Caco-2 cells. These differences were further confirmed by staining coverslips with malachite green and counterstaining with Wright-Giemsa (data not shown). Thus, for all epithelial cells tested, there was an increased adherence of the mutant versus Ames wild-type spores.
TABLE 2.
Association of spores to nonprofessional phagocytesa
| Cell type | % Recovery for Ames | SE | % Recovery for bclA | SE | P |
|---|---|---|---|---|---|
| A549 | 0.3 | 0.08 | 9.02 | 0.04 | 0.0001 |
| CHO | 2.5 | 0.81 | 31.6 | 9.40 | 0.04 |
| Caco-2 | 0.3 | 0.04 | 18.4 | 3.70 | 0.01 |
| IMR-90 | 0.5 | 0.43 | 21.5 | 0.60 | 0.001 |
| HUVEC | 0.01 | 0.01 | 0.14 | 0.04 | 0.04 |
Cells were incubated with either Ames wild-type or bclA mutant spores for 1 h. The range of calculated MOI levels was 40 to 46 spores for one A549 cell; 40 to 66 spores for one CHO cell; 32 to 38 spores for one CaCo-2 cell; 24 to 46 spores for one IMR-90 cell; and 28 to 30 spores for one HUVEC cell. Following incubation, the cells were washed and lysed and the bacteria were plated on LB agar plates. The percent recovery of spores was determined by dividing the number of CFU counts from lysed cells by the number of spores added. SE values are from triplicate independent experiments.
Interaction with fibroblasts and endothelial cells.
The IMR-90 cell line, a human lung fibroblast, was tested for spore adherence. Again there was significantly increased adherence with bclA mutant spores compared to that with Ames wild-type spores (Table 2). Similar differences were also observed with human umbilical vein vascular endothelium cells. The bclA mutant spores again adhered significantly better than the parental wild-type Ames spores.
Adherence of bclA mutant spores to macrophages.
Phagocytosis by RAW264.7 macrophage-like cells of bclA mutant spores relative to Ames wild-type spores was the same. Spore uptake was measured by CFU and microscopic counts of fluorescent spores or those stained with malachite green (Fig. 6). In order to differentiate between spore adherence in the RAW264.7 cells versus phagocytosis of spores, RAW264.7 cells were treated with cytochalasin D (6). As shown in Table 3, no significant difference was detected with both wild-type and bclA mutant spores adherent to RAW264.7 macrophage-like cells treated with cytochalasin D.
FIG. 6.
Effect of the bclA mutation on uptake of spores by macrophages. RAW264.7 cells were infected with spores at an MOI of 1 to 3 for one cell. (A) Data depict viable counts. The error bars represent standard errors of the means. (B) Microscopic counts of fluorescently labeled samples. (C) Microscopic counts of samples stained with the malachite green spore stain. The phagocytic index is the mean number of spores phagocytosed per macrophage multiplied by 100. Similar results were obtained in at least two additional experiments.
TABLE 3.
Adherence of spores to macrophagesa
| Macrophage cell line | % Recovery for Ames | SE | % Recovery for bclA | SE | P |
|---|---|---|---|---|---|
| RAW264.7 | 16.8 | 7.50 | 6.30 | 3.50 | 0.27 |
| J774A.1 | 8.0 | 0.20 | 11.50 | 2.90 | 0.35 |
| MH-S | 2.0 | 0.35 | 6.60 | 1.00 | 0.05 |
Macrophage-like cells were pretreated with cytochalasin D to prevent phagocytosis, and spores were then incubated with the cells for 1 h at an MOI of five to eight spores for one cell. The percent recovery of spores was determined by dividing the number of CFU counts from the lysed cells by the number of spores added. The difference in spore binding to macrophages was not significant between strains. SE values are representative of three independent experiments.
We then compared the binding to other macrophage-like cell lines, J774A.1 and MH-S, which were treated similarly to RAW264.7 (Table 3). As observed with RAW264.7, J774A.1 and MH-S cells demonstrated no significant difference in spore binding between the wild-type and mutant spores.
DISCUSSION
In a previous study, it was demonstrated that the Ames strain bclA mutant of B. anthracis remained fully virulent when assessed by various models of anthrax infection (3). However, bclA mutant spores appeared to be slightly slower in trafficking from the lungs of mice that had been exposed to aerosolized spores (3). Potentially, the delay in bclA spores could be due to the mutant spores adhering better to the lining of the lung. To test this possibility, we compared the binding of wild-type and bclA mutant spores to BEC by in vitro assays and microscopy (Fig. 1 and 2). The binding of Ames wild-type spores to BEC was measured at a relatively low level. In contrast, bclA mutant spores exhibited a much higher degree of binding to BEC. With increased binding to BEC, we also observed a greater level of intracellular bclA mutant spores (Fig. 5). The role in pathogenesis, if any, of the spores being able to intracellularly enter the BEC remains undetermined. Currently, we are examining the fate of these intracellular bclA mutant spores within BEC. The increased binding of the bclA mutant spores was not unique to BEC since increased adherence was observed for all nonprofessional phagocytic cell types examined (Table 2). It is possible that entry of the B. anthracis spores into nonprofessional phagocytes may represent a bacterial survival tactic that perpetuates disease from within an infected host and a relatively nondestructive reservoir.
While the increased binding of bclA mutant spores to BEC could be due to specific ligand-receptor interactions, the treatment of spores with trypsin or papain did not affect binding, thus decreasing the possibility of a protein adhesin that is sensitive to digestion and exposed on the exosporium devoid of the BclA protein. Binding studies with bclA mutant spores and BEC also revealed that spore adherence was not readily saturated with increasing concentrations of spores (Fig. 4). However, when performing competition studies with lethally irradiated spores of the bclA mutant spores, binding could be partially blocked with a very high dose (Table 1). These results demonstrated that increased binding of the bclA mutant spores to BEC occurred partially through a specific, presumably protease-resistant, ligand-receptor event. However, the saturation experiments suggest that there may also be a nonspecific binding component involved in bclA spore binding to BEC.
In contrast, when Ames spores were treated with trypsin, we noted a significant increase in binding of trypsin-treated spores to the BEC (Fig. 3). However, the specific effect trypsin or papain had on the wild-type spores to cause this increased adherence is unknown to date. In binding assays, the adherence of Ames spores to BEC could be saturated with increasing concentrations (Fig. 4). Furthermore, in competition experiments, the adherence of live Ames spores to BEC was readily dependent upon the dose of competing irradiated spores (Table 1). This inhibition was more pronounced than that observed with the bclA mutant spores. Despite the overall low number of Ames wild-type spores that bound to BEC in contrast to the binding of bclA mutant spores, these results suggest that Ames spores were binding to an unknown receptor(s) in the BEC. Perhaps this receptor(s) is present at a relatively low level on the BEC. It has previously been shown that the interaction of other pathogenic bacteria (32) and bacterial toxins (10) does occur with host cells containing a low density of receptors.
A second possibility would be that the binding interaction between Ames spore ligand and the BEC receptor(s) was weak. In any event, such binding experiments with B. anthracis spores are novel and suggest specific, receptor-mediated interactions that warrant further investigation. The identities of the spore-based ligand(s) and the cell-surface receptor(s) on eukaryotic cells represent obvious targets for focused attention. Such studies can have an impact upon our collective understanding of B. anthracis pathogenesis as well as lead to new methods for treating and/or preventing anthrax.
As per our results, perhaps removal of the BclA fibers further exposes an adhesin that is normally masked or sterically impinged by the fibers. This logic agrees with results following protease treatment of Ames spores, suggesting that loss of proteins from the exosporium does indeed enhance spore binding to BEC. It was recently demonstrated that the exosporium structure may mask spore epitopes from the host immune response (2).
We did not detect significant differences between the wild-type and bclA mutant spores in their adherence to, and phagocytic uptake by, macrophages (Fig. 6 and Table 3). Therefore, the BclA protein was not required for B. anthracis spore adherence to macrophages. These results are surprising as the fibers projecting from the exosporium were previously speculated to function in adherence and/or uptake to the host cells (20). For anthrax infection, the macrophage is considered the primary host cell that transports B. anthracis spores from an entry site into the host's lymphatic system. From this point, spores germinate and lead to a disseminated infection (16, 31). Therefore, it is tempting to speculate that perhaps one role of the BclA fibers in pathogenesis is to inhibit binding to epithelial cells and other nonprofessional phagocytes during the initial stages of infection; therefore, the spores are more readily directed towards macrophages.
If spores bind to cells lining the lung, transport by macrophages could be delayed and the progression of disease might possibly be hampered. It has been shown in several previous studies that the bronchoalveolar spaces are unsuitable for B. anthracis spore germination (3, 8, 17, 18). Furthermore, lung epithelial cells secrete antimicrobial peptides and proteins (19, 21, 40) that could inactivate B. anthracis cells. In a model system using human airway tissue, B. anthracis spores are either killed by epithelial cells or phagocytized by macrophages where germination and subsequent bacillus release occurs (28).
One of our previous studies demonstrated that spores lacking the BclA fibers are still as capable of causing infection as wild-type spores by either an intramuscular or an intranasal challenge in guinea pigs or mice, respectively (3). The animals in both infection models were exposed to spores equivalent to approximately 10 50% lethal doses. In a spore trafficking experiment, the bclA mutant spores still disseminated from the mouse lungs and were presumably transported by alveolar macrophages. However, there appeared to be a slight delay in the trafficking of the bclA mutant spores compared to the trafficking of the parental wild-type strain. During the natural infection of a mammal, the number of spores introduced into the body from the environment would presumably be much lower; therefore, directing spores to macrophages could be critical for successful dissemination of B. anthracis.
The focus of this study was to examine the interaction between spores of B. anthracis, with or without the BclA fibers, and various cell types. However, we did not examine the interaction of vegetative cells of the Ames strain with these mammalian cells. Recently, vegetative cells of the attenuated Sterne strain of B. anthracis have been shown to adhere and are subsequently internalized by HT1080, a connective tissue epithelial cell, and Caco-2 cells (33). As the Sterne strain lacks the pXO2 plasmid containing genes for capsule synthesis (14), the interaction of encapsulated B. anthracis vegetative cells with epithelial cells remains to be examined.
In conclusion, our findings from this study demonstrate that BclA fibers of the B. anthracis spore decreased adherence to nonprofessional phagocytes, but the BclA fibers were not necessary for interacting with macrophages. Binding of B. anthracis spores to BEC appears to be mediated through a specific ligand-receptor interaction that may provide important clues towards more fully understanding anthrax pathogenesis, and how to thwart it.
Acknowledgments
We thank Gabriel Rother and Michelle Saylor for their invaluable technical assistance and Chantal Allamargot at Central Electron Microscopy Facility, University of Iowa, for preparing the electron microscopy samples.
The research described herein was sponsored by the Defense Threat Reduction Agency JSTO-CBD as no. A1_X002_04_RD_B, the Medical Research and Material Command Research Plan as no. 02-4-5C-018 (J.B.), and an In-House Laboratory Innovative Research Award from the Department of the Army under project 92489 (J.B.).
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
Editor: D. L. Burns
Footnotes
Published ahead of print on 2 July 2007.
REFERENCES
- 1.Aronson, A. I., and P. Fitz-James. 1976. Structure and morphogenesis of the bacterial spore coat. Bacteriol. Rev. 40:360-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basu, S., T. J. Kang, W. H. Chen, M. J. Fenton, L. Baillie, S. Hibbs, and A. S. Cross. 2007. Role of Bacillus anthracis spore structures in macrophage cytokine responses. Infect. Immun. 75:2351-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bozue, J., C. K. Cote, K. L. Moody, and S. L. Welkos. 2007. Fully virulent Bacillus anthracis does not require the immunodominant protein BclA for pathogenesis. Infect. Immun. 75:508-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bozue, J. A., N. Parthasarathy, L. R. Phillips, C. K. Cote, P. F. Fellows, I. Mendelson, A. Shafferman, and A. M. Friedlander. 2005. Construction of a rhamnose mutation in Bacillus anthracis affects adherence to macrophages but not virulence in guinea pigs. Microb. Pathog. 38:1-12. [DOI] [PubMed] [Google Scholar]
- 5.Charlton, S., A. J. Moir, L. Baillie, and A. Moir. 1999. Characterization of the exosporium of Bacillus cereus. J. Appl. Microbiol. 87:241-245. [DOI] [PubMed] [Google Scholar]
- 6.Cooper, J. A. 1987. Effects of cytochalasin and phalloidin on actin. J. Cell Biol. 105:1473-1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cote, C. K., C. A. Rossi, A. S. Kang, P. R. Morrow, J. S. Lee, and S. L. Welkos. 2005. The detection of protective antigen (PA) associated with spores of Bacillus anthracis and the effects of anti-PA antibodies on spore germination and macrophage interactions. Microb. Pathog. 38:209-225. [DOI] [PubMed] [Google Scholar]
- 8.Cote, C. K., N. Van Rooijen, and S. L. Welkos. 2006. Roles of macrophages and neutrophils in the early host response to Bacillus anthracis spores in a mouse model of infection. Infect. Immun. 74:469-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Driks, A. 2002. Maximum shields: the assembly and function of the bacterial spore coat. Trends Microbiol. 10:251-254. [DOI] [PubMed] [Google Scholar]
- 10.Fishman, P. H., and E. E. Atikkan. 1980. Mechanism of action of cholera toxin: effect of receptor density and multivalent binding on activation of adenylate cyclase. J. Membr. Biol. 54:51-60. [DOI] [PubMed] [Google Scholar]
- 11.Friedlander, A. M. 2000. Anthrax: clinical features, pathogenesis, and potential biological warfare threat. Curr. Clin. Top. Infect. Dis. 20:335-349. [PubMed] [Google Scholar]
- 12.Gerhardt, P., and E. Ribi. 1964. Ultrastructure of the exosporium enveloping spores of Bacillus cereus. J. Bacteriol. 88:1774-1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giorno, R., J. Bozue, C. Cote, T. Wenzel, K. S. Moody, M. Mallozzi, M. Ryan, R. Wang, R. Zielke, J. R. Maddock, A. Friedlander, S. Welkos, and A. Driks. 2007. Morphogenesis of the Bacillus anthracis spore. J. Bacteriol. 189:691-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green, B. D., L. Battisti, T. M. Koehler, C. B. Thorne, and B. E. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gruenert, D. C., W. E. Finkbeiner, and J. H. Widdicombe. 1995. Culture and transformation of human airway epithelial cells. Am. J. Physiol. 268:L347-L360. [DOI] [PubMed] [Google Scholar]
- 16.Guidi-Rontani, C., M. Levy, H. Ohayon, and M. Mock. 2001. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 42:931-938. [DOI] [PubMed] [Google Scholar]
- 17.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 18.Heine, H. S., J. Bassett, L. Miller, J. M. Hartings, B. E. Ivins, M. L. Pitt, D. Fritz, S. L. Norris, and W. R. Byrne. 2007. Determination of antibiotic efficacy against Bacillus anthracis in a mouse aerosol challenge model. Antimicrob. Agents Chemother. 51:1373-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kida, Y., T. Shimizu, and K. Kuwano. 2006. Sodium butyrate up-regulates cathelicidin gene expression via activator protein-1 and histone acetylation at the promoter region in a human lung epithelial cell line, EBC-1. Mol. Immunol. 43:1972-1981. [DOI] [PubMed] [Google Scholar]
- 20.Koehler, T. M. 2000. Bacillus anthracis, p. 519-528. In V. A. Fischetti, R. P. Novick, J. J. Ferretti, D. A. Portnoy, and J. I. Rood (ed.), Gram-positive pathogens. ASM Press, Washington, DC.
- 21.Lau, Y. E., D. M. Bowdish, C. Cosseau, R. E. Hancock, and D. J. Davidson. 2006. Apoptosis of airway epithelial cells: human serum sensitive induction by the cathelicidin LL-37. Am. J. Respir. Cell Mol. Biol. 34:399-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Little, S., and A. Driks. 2001. Functional analysis of the Bacillus subtilis morphogenetic spore coat protein CotE. Mol. Microbiol. 42:1107-1120. [DOI] [PubMed] [Google Scholar]
- 23.Little, S. F., and G. B. Knudson. 1986. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 52:509-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendelson, I., S. Tobery, A. Scorpio, J. Bozue, A. Shafferman, and A. M. Friedlander. 2004. The NheA component of the non-hemolytic enterotoxin of Bacillus cereus is produced by Bacillus anthracis but is not required for virulence. Microb. Pathog. 37:149-154. [DOI] [PubMed] [Google Scholar]
- 25.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 26.Perez-Casal, J., M. G. Caparon, and J. R. Scott. 1991. Mry, a trans-acting positive regulator of the M protein gene of Streptococcus pyogenes with similarity to the receptor proteins of two-component regulatory systems. J. Bacteriol. 173:2617-2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Popham, D. L. 2002. Specialized peptidoglycan of the bacterial endospore: the inner wall of the lockbox. Cell. Mol. Life. Sci. 59:426-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radyuk, S. N., P. A. Mericko, T. G. Popova, E. Grene, and K. Alibek. 2003. In vitro-generated respiratory mucosa: a new tool to study inhalational anthrax. Biochem. Biophys. Res. Commun. 305:624-632. [DOI] [PubMed] [Google Scholar]
- 29.Redmond, C., L. W. Baillie, S. Hibbs, A. J. Moir, and A. Moir. 2004. Identification of proteins in the exosporium of Bacillus anthracis. Microbiol. 150:355-363. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds, E. 1963. The use of lead citrate at high pH as an electron opaque stain in electron microscopy. J. Cell Biol. 17:208-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 73:485-494. [Google Scholar]
- 32.Rowe, H. A., N. J. Griffiths, D. J. Hill, and M. Virji. 2007. Co-ordinate action of bacterial adhesins and human carcinoembryonic antigen receptors in enhanced cellular invasion by capsulate serum resistant Neisseria meningitidis. Cell. Microbiol. 9:154-168. [DOI] [PubMed] [Google Scholar]
- 33.Russell, B. H., R. Vasan, D. R. Keene, and Y. Xu. 2007. Bacillus anthracis internalization by human fibroblasts and epithelial cells. Cell. Microbiol. 9:1262-1274. [DOI] [PubMed] [Google Scholar]
- 34.Schaeffer, P., J. Millet, and J. P. Aubert. 1965. Catabolic repression of bacterial sporulation. Proc. Natl. Acad. Sci. USA 54:704-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steichen, C., P. Chen, J. F. Kearney, and C. L. Turnbough, Jr. 2003. Identification of the immunodominant protein and other proteins of the Bacillus anthracis exosporium. J. Bacteriol. 185:1903-1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steichen, C. T., J. F. Kearney, and C. L. Turnbough, Jr. 2005. Characterization of the exosporium basal layer protein BxpB of Bacillus anthracis. J. Bacteriol. 187:5868-5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sylvestre, P., E. Couture-Tosi, and M. Mock. 2002. A collagen-like surface glycoprotein is a structural component of the Bacillus anthracis exosporium. Mol. Microbiol. 45:169-178. [DOI] [PubMed] [Google Scholar]
- 38.Sylvestre, P., E. Couture-Tosi, and M. Mock. 2005. Contribution of ExsFA and ExsFB proteins to the localization of BclA on the spore surface and to the stability of the Bacillus anthracis exosporium J. Bacteriol. 187:5122-5128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Todd, S. J., A. J. Moir, M. J. Johnson, and A. Moir. 2003. Genes of Bacillus cereus and Bacillus anthracis encoding proteins of the exosporium. J. Bacteriol. 185:3373-3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vos, J. B., M. A. van Sterkenburg, K. F. Rabe, J. Schalkwijk, P. S. Hiemstra, and N. A. Datson. 2005. Transcriptional response of bronchial epithelial cells to Pseudomonas aeruginosa: identification of early mediators of host defense. Physiol. Genomics 21:324-336. [DOI] [PubMed] [Google Scholar]
- 41.Welkos, S., A. Friedlander, S. Weeks, S. Little, and I. Mendelson. 2002. In-vitro characterisation of the phagocytosis and fate of anthrax spores in macrophages and the effects of anti-PA antibody. J. Med. Microbiol. 51:821-831. [DOI] [PubMed] [Google Scholar]
- 42.Welkos, S., S. Little, A. Friedlander, D. Fritz, and P. Fellows. 2001. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiology 147:1677-1685. [DOI] [PubMed] [Google Scholar]
- 43.Welkos, S. L., C. K. Cote, K. M. Rea, and P. H. Gibbs. 2004. A microtiter fluorometric assay to detect the germination of Bacillus anthracis spores and the germination inhibitory effects of antibodies. J. Microbiol. Methods 56:253-265. [DOI] [PubMed] [Google Scholar]
- 44.Welkos, S. L., R. W. Trotter, D. M. Becker, and G. O. Nelson. 1989. Resistance to the Sterne strain of B. anthracis: phagocytic cell responses of resistant and susceptible mice. Microb. Pathog. 7:15-35. [DOI] [PubMed] [Google Scholar]