Abstract
The success of Staphylococcus aureus as a pathogen can largely be attributed to the plethora of genetic regulators encoded within its genome that temporally regulate its arsenal of virulence determinants throughout its virulence lifestyle. Arguably the most important of these is the two-component, quorum-sensing system agr. Over the last decade, the controversial presence of a second quorum-sensing system (the TRAP system) has been proposed, and it has been mooted to function as the master regulator of virulence in S. aureus by modulating agr. Mutants defective in TRAP are reported to be devoid of agr expression, lacking in hemolytic activity, essentially deficient in the secretion of virulence determinants, and avirulent in infection models. A number of research groups have questioned the validity of the TRAP findings in recent years; however, a thorough and independent analysis of its role in S. aureus physiology and pathogenesis has not been forthcoming. Therefore, we have undertaken such an analysis of the TRAP locus of S. aureus. We found that a traP mutant was equally hemolytic as the wild-type strain. Furthermore, transcriptional profiling found no alterations in the traP mutant in expression levels of agr or in expression levels of multiple agr-regulated genes (hla, sspA, and spa). Analysis of secreted and surface proteins of the traP mutant revealed no deviation in comparison to the parent. Finally, analysis conducted using a murine model of S. aureus septic arthritis revealed that, in contrast to an agr mutant, the traP mutant was just as virulent as the wild-type strain.
Staphylococcus aureus is a major human pathogen that is considered to be one of the most common causes of human disease (42). The success of S. aureus as an infectious agent is largely due to its ability to cause a wide range of infections in a plethora of ecological niches within the host. These can range from the relatively benign, such as soft tissue infections, boils, and abscesses, to the systemic and life threatening, such as endocarditis, septic arthritis, osteomyelitis, pneumonia, and septicemia. The array of pathologies caused by S. aureus is facilitated by the arsenal of virulence determinants encoded within its genome, all of which are tightly regulated both temporally and spatially throughout its pathogenic life cycle (42, 51). This is achieved through an army of regulatory mechanisms that encompass DNA-binding proteins, two-component regulators, sigma factors, and quorum-sensing mechanisms (1, 3, 12, 15-18, 22, 26, 30, 32, 34, 51, 71).
Arguably the most important of all of these regulatory loci is the agr system, a quorum-sensing two-component regulator that has been shown by numerous investigators to be central to the infectious capacity of S. aureus (1, 34, 47, 49, 55). Agr is a temporal regulatory element that is maximally expressed from the postexponential phase onwards, where it represses surface and attachment proteins and upregulates the synthesis of toxins and exoenzymes. Upon entry into stationary phase, agr expression in vitro is seen to decline, with such an eclipse of activity also observed during in vivo analyses (69). The agr locus is comprised of two distinct transcripts driven by the divergent promoters P2 and P3. P2 results in the transcription of the agrBDCA cluster; with agrBD encoding the quorum-sensing arm of the agr locus, while agrCA encodes the two-component regulatory activity (39, 46, 48). AgrB functions as a membrane-associated protease that serves to cleave and export a modified octapeptide form of AgrD (autoinducing peptide [AIP]), which acts as the quorum-sensing ligand (35, 36, 45, 48, 72, 73). In the extracellular milieu AIP, at a sufficient density threshold, binds its receptor, AgrC, inducing its phosphorylation (40). The newly phosphorylated AgrC then in turn induces the phosphorylation of its target molecule, AgrA, which has the effect of upregulating the P3 promoter of the agr operon, which encodes RNAIII, the regulatory effector of the system (46, 55).
Over the last decade, the controversial presence of a second quorum-sensing system in S. aureus has been proposed, and it has been mooted to function as the master regulator of virulence in this organism by modulating the activity of agr (5-8, 31, 37, 38). This system, referred to as staphylococcal quorum-sensing system 1 (SQS1) (the agr system has been termed SQS2) (37), is proposed to operate upstream of Agr, controlling the activity of RNAIII via its own autoregulatory mechanism. SQS1 operates by the constitutive release of ribosomal protein L2 (RNAIII-activating protein [RAP]), into the supernatants of S. aureus cultures (38). Once the extracellular concentration of RAP has achieved a sufficient density, it activates its target protein, TRAP (for target of RAP), and induces the phosphorylation of three conserved TRAP histidine residues (8, 31). From here TRAP is proposed to interact with the agr system, bringing about its upregulation. In addition to the presence of TRAP and RAP, there is also an antagonistic repressing peptide referred to as RNAIII-inhibitory peptide (RIP) (4-6). RIP is produced by a coagulase-negative Staphylococcus species that is believed to be either S. xylosus, S. warnerii, or possibly even S. hominis (10, 50). RIP serves to compete with RAP in mediating the activity of TRAP; thus, if RIP binds to TRAP instead of RAP, then TRAP is dephosphorylated, shutting down SQS1 and consequently the agr system (8, 31).
The controversial nature of SQS1 is the result of over a decade of individual investigation by the researchers R. P. Novick and N. Balaban. Below is presented a review of this published work on quorum sensing in S. aureus by these groups in order to provide a better understanding of the subject and to place in context the findings of the present study.
The existence of RAP was first noted by Balaban and Novick (9), who showed it to be a 38-kDa protein produced by post-exponential-phase cultures of S. aureus. They also noted the presence of RIP, which was shown to be produced by an exoprotein-deficient strain of S. aureus known as RN833. Shortly after this record appeared in the literature, a further study by Ji et al. (36) revealed that the agr-stimulating activity observed by Balaban and Novick (9) was not actually the result of the 38-kDa RAP protein but was via the action of a modified octapeptide form of AgrD, termed AIP. It was suggested that the 38-kDa RAP anomalously copurifies with AIP, thus explaining the results of the earlier publication. Furthermore, Ji et al. (36) demonstrated that AIP could not function as a linear peptide, and they speculated that it may require cyclic anhydride linkage mediated through a conserved cysteine residue to gain activity. A later study by Ji et al. (35) demonstrated that AIPs from nonself cultures can function to inhibit, rather than activate, RNAIII synthesis. It was proposed that this formed the basis of a novel system of cross-species interference, where staphylococcal strains from different biotypes could inhibit the virulence potential of competitors in an infectious environment. In this study, Ji et al. (35) also validated their earlier assumption (36), showing that linear forms of AIPs are nonfunctional but that synthetic cyclic derivatives are functional.
In contrast to the work of the Novick group, a 1998 publication by Balaban and coworkers (8) indicated not only that the original 38-kDa RAP is found in both agr-functional and -nonfunctional strains but that it does indeed possess RNAIII-stimulating activity. Thus, it was proposed that RAP is an additional, agr-independent, activator of RNAIII synthesis. It was further suggested, although without supporting evidence, that antibodies against RAP can inhibit RNAIII synthesis in S. aureus cultures. Additionally, mice pretreated with RAP from either agr+ or agr mutant strains were protected from challenge by S. aureus. RIP was also purified and sequenced by Balaban et al. (8), revealing it to be a heptapeptide (YSPXTNF). A synthetic form of RIP (YSPWTNF) was generated, and both RIP forms were shown to inhibit RNAIII production, and to function effectively in the therapeutic treatment of S. aureus infections.
Almost immediately following this publication, two further studies regarding RNAIII activating components were presented. The first, by Otto et al. (53), detailed the purification and characterization of AIP from S. epidermidis. They found that in S. epidermidis, AIP is a cyclic octapeptide that depends on the conserved cysteine residue for cyclization. Otto et al. (53) generated a number of modified forms of AIP that varied in size, amino acid content, and structure (both linear and cyclic). No activity was attributable to any of the peptides other than the cyclic octapeptide based on the native AIP of S. epidermidis. Following this publication, Mayville et al. (43) described the design and synthesis of a number of different octapeptides from various S. aureus biotypes. Their studies corroborated the findings of Otto et al. (53), revealing AIP to depend entirely on cysteine-based cyclization for both stimulating and inhibitory activities.
In 2000, Novick and coworkers (50) detailed their own analysis of RAP and its interactions with the agr system. They could find no agr-stimulating activity in agr-deficient strains. Furthermore the only agr-activating components in agr-positive strains stemmed from the presence of AIP. Purification analysis revealed that the removal of AIP from agr-stimulating fractions of S. aureus supernatants required three rounds of dialysis. Thus, it was proposed that AIP contamination is the explanation for the RAP data of Balaban and coworkers (8, 9). Novick et al. (50) also generated synthetic RIP following the protocols of Balaban et al. (8); however, they were unable to associate any RNAIII inhibition or protection during S. aureus infection for the linear RIP. Finally, they conducted an analysis of RN833, the original source of RIP, and found that rather than being a mutant derivative of S. aureus, it was in fact likely to be S. warnerii (85% certainty). Analysis of the RN833 agr locus revealed an agrD sequence that would encode an AIP closely resembling RIP (YSPCTNFF), and thus they concluded that RIP is, and always has been, a nonself, inhibitory AIP.
In their response to the work of Novick et al. (50), Balaban and coworkers (10) countered that their RAP and RIP purification and production methods are considerably different to those employed by Novick et al. (50) and that this might explain the observed discrepancies. Furthermore, their own analysis of RN833 revealed it to be S. xylosus (99% certainty) and indicated a non-agr-located DNA sequence from RN833 that would encode RIP as described in their previous works. Unfortunately, no data or explanations as to how this sequence was derived were presented. It was also suggested that the multiple rounds of dialysis employed by Novick and coworkers to purify AIP would result in the degradation of RAP, explaining why they were unable to purify it from S. aureus cultures. Additionally, N-terminal sequence data for RAP were presented, showing it to closely resemble that of the ribosomal protein L2. Further to this, the discovery of TRAP was presented, detailing it to be specifically phosphorylated by RAP and dephosphorylated by RIP. A continued analysis of TRAP was contained in a 2001 publication by Balaban et al. (7) detailing and confirming the described interplay of RIP and RAP with TRAP. Mutations within the TRAP locus resulted in strains of S. aureus being almost entirely devoid of RNAIII production. It was also shown that once RAP induces agr induction, TRAP is dephosphorylated by the agr system. This leads to a model whereby RAP and, thus, TRAP are required to initiate agr activity.
In 2003 Korem et al. (38) conducted investigations with RAP, confirming it to be the S. aureus ortholog of ribosomal protein L2. Analysis of a variety of strains, including S. aureus, S. xylosus, S. epidermidis, and Escherichia coli strains, revealed that L2 is secreted only by strains of S. aureus and that secretion occurs constitutively and not as the result of cell lysis. Following this paper closely was the 2004 publication by Gov et al. (31), who showed that TRAP contains three conserved histidine residues, all of which are phosphorylated and required for function. Replacement of any one of these residues with alanine led to a failure of the TRAP protein to become phosphorylated at any of the remaining histidine residues, and thus strains bearing alterations in any of these three histidine residues behave like TRAP-negative mutants. Phenotypic analysis of a traP-inactivated mutant revealed it to be nonhemolytic, devoid of RNAIII production, and entirely avirulent in a murine model of S. aureus-induced cellulitis.
The most recent study on the RAP/TRAP system was a transcriptional profiling study (37). In this investigation, microarray analysis revealed that the expression levels of many virulence-involved genes were altered in a traP mutant. A comparison of these genes with data from similar studies using agr mutants of S. aureus revealed almost total overlap in their regulons. As the RAP/TRAP SQS1 system of S. aureus is proposed to modulate the activity of agr, this result was consistent with the proposed model for SQS1 activity.
In this study, we introduced a disrupted allele of the traP open reading frame into both the S. aureus 8325-4 and Newman strains. Transcription profiling of agr and agr-regulated genes and protein secretion, hemolytic activity, and virulence studies revealed absolutely no role for traP in the regulation of agr or the virulence of S. aureus.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth conditions.
The S. aureus strains used are listed in Table 1. All strains created in this study were confirmed by PCR and Southern blot analyses for correct construction (data not shown). S. aureus was grown in 100 ml brain heart infusion broth (Oxoid) (1:2.5 flask/volume ratio) at 37°C with shaking at 250 rpm (60), unless indicated otherwise. When required, antibiotics were added at the following concentrations: tetracycline, 5 mg liter−1; erythromycin, 5 mg liter−1; lincomycin, 25 mg liter−1; and kanamycin, 50 mg liter−1.
TABLE 1.
S. aureus strains
| Strain | Genotype or description | Reference or source |
|---|---|---|
| 8325-4 | Wild-type strain cured of prophages | Lab stock |
| Newman | Wild-type strain, human clinical isolate | 25 |
| PC6911 | 8325-4 agr::tet | 14, 51 |
| LES77 | Newman agr::tet | This study |
| VKS101 | COL traP::kan | 31, 61 |
| LES78 | 8325-4 traP::kan | This study |
| LES79 | Newman traP::kan | This study |
| SH101F7 | 8325-4 pAZ106::hld (RNAIII) agr+ | 32 |
| LES80 | 8325-4 traP::kan pAZ106::hld (RNAIII) agr+ | This study |
| LES81 | Newman pAZ106::hld (RNAIII) agr+ | This study |
| LES82 | Newman traP::kan pAZ106::hld (RNAIII) agr+ | This study |
| PC322 | 8325-4 pAZ106::hla hla+ | 14 |
| LES83 | 8325-4 traP::kan pAZ106::hla hla+ | This study |
| LES84 | Newman pAZ106::hla hla+ | This study |
| LES85 | Newman traP::kan pAZ106::hla hla+ | This study |
| LES07 | 8325-4 pAZ106::sspA sspA+ | 32 |
| LES86 | 8325-4 traP::kan pAZ106::sspA sspA+ | This study |
| LES87 | Newman pAZ106::sspA sspA+ | This study |
| LES88 | Newman traP::kan pAZ106::sspA sspA+ | This study |
| PC203 | 8325-4 pAZ106::spa spa+ | 14 |
| LES89 | 8325-4 traP::kan pAZ106::spa spa+ | This study |
| LES90 | Newman pAZ106::spa spa+ | This study |
| LES91 | Newman traP::kan pAZ106::spa spa+ | This study |
Generation of bacterial strains used in this study.
All the strains employed in this study either represent existing published isogenic mutant or reporter gene fusion strains (for specific references, see Table 1) or have been created from these previously documented strains via standard S. aureus phage transduction techniques using phage 80α. Thus, to generate strains LES78 (8325-4 traP::kan) and LES79 (Newman traP::kan), strain VKS101 (COL traP::kan) (31, 61) was used as a donor strain in separate transductions with the wild-type strains, 8325-4 and Newman, respectively. Kanamycin-resistant transductants were obtained and screened by PCR and Southern blot analysis to confirm the presence of the traP::kan allele. To generate the reporter gene fusion strains used in this study, strains LES78 and LES79 were then used as recipients in separate transductions, and strain SH101F7 (hld) (32), PC322 (hla) (14), LES85 (sspA) (32), or PC203 (spa) (14) was used as the donor strain. To generate the Newman reporter gene fusion strains, these same four strains were used as donor strains and Newman was used as the recipient. Transductants were screened for the presence of the correct chromosomally located reporter construct and for the presence of the appropriate traP allele. Strain LES77 (Newman agr::tet) was created using PC6911 (14, 51) as the donor strain and Newman as the recipient. After each strain was genotypically verified, the phenotypic properties were determined.
β-Galactosidase assays.
Levels of β-galactosidase activity were measured as described previously (59). Fluorescence was measured using a Bio-Tek Synergy HT plate reader with a 0.1-s count time and calibrated with standard concentrations of 4-methyl umbelliferone. One unit of β-galactosidase activity was defined as the amount of enzyme that catalyzed the production of 1 pmol 4-methyl umbelliferone min−1 optical density at 600 nm (OD600) unit−1. Assays were performed on duplicate samples and the values averaged. The results presented here were representative of three independent experiments that showed less than 10% variability.
Protein analysis.
Extracellular and surface protein sample preparation and analysis were conducted using 12% (wt/vol) sodium dodecyl sulfate-polyacrylamide gel electrophoresis as described previously (15, 44). The equivalent protein amounts per gel are given in the legend to Fig. 3.
FIG. 3.
Secreted and surface-associated protein profiles of the traP mutant. (A) Secreted protein profiles of 8325-4 (lane 1), 8325-4 traP::kan (lane 2), and 8325-4 agr::tet (lane 3). Protein samples are equivalent to 1.0 OD600 unit of original culture. (B) Secreted protein profiles of Newman (lane 1), Newman traP::kan (lane 2), and Newman agr::tet (lane 3). Protein samples are equivalent to 2.0 OD600 units of original culture. (C) Surface-associated protein profiles of 8325-4 (lane 1), 8325-4 traP::kan (lane 2), and 8325-4 agr::tet (lane 3). Protein samples are equivalent to 150 OD600 units of original culture. (D) Surface-associated protein profiles of Newman (lane 1), Newman traP::kan (lane 2), and Newman agr::tet (lane 3). Protein samples are equivalent to 75 OD600 units of original culture. The arrow denotes the 55-kDa band corresponding to surface protein A, which was subjected to densitometric analysis.
Experimental model of S. aureus sepsis and arthritis.
Female NRMI mice, 6 to 8 weeks old, were purchased from B & K Universal AB (Sollentuna, Sweden) and kept in the animal facility of the Department of Rheumatology and Inflammation Research, Göteborg University. S. aureus strain Newman and its isogenic traP::kan mutant were cultured on horse blood agar plates at 37°C for 24 h, harvested, washed in phosphate-buffered saline (PBS), and resuspended in PBS supplemented with 10% dimethyl sulfoxide and 5% bovine serum albumin. Aliquots of bacterial suspensions with a known CFU/ml, as determined by viable counts, were stored at −20°C. Before inoculation, the bacterial cultures were thawed, washed once with PBS, and diluted in PBS to the desired concentration. Mice were inoculated intravenously with 4 × 106 bacteria of either strain Newman or Newman traP::kan. Viable counts of the inocula were determined in each experiment to confirm the accuracy of each dose. Mice were monitored individually for 10 days, by an observer blinded to the identity of the experimental groups, for general appearance, weight change, mortality, and development of arthritis. Clinical arthritis, defined by visible erythema and/or swelling of at least one joint, was scored from 0 to 3 for each limb (1, mild swelling and/or erythema; 2, moderate swelling and erythema; 3, marked swelling and erythema). An arthritic index was generated by adding the scores for each limb of a given animal. The statistical evaluation of weight change and severity of clinical arthritis between groups was performed using a Mann-Whitney U test. A chi-square test was used for comparison of frequency of clinical arthritis between groups. A P value of <0.05 (after Bonferroni correction for multiple comparisons) is deemed to indicate a statistically significant difference.
RESULTS
Inactivation of traP has no impact on the hemolytic nature of S. aureus.
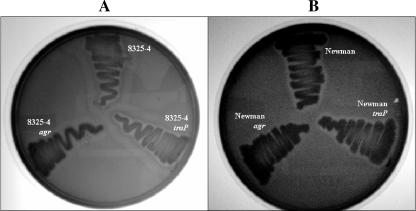
As detailed above, Balaban et al. have repeatedly demonstrated that mutations in traP abolish the synthesis of RNAIII in S. aureus (8, 31, 38). One of the major hallmarks of an agr-deficient strain is a total lack of α-hemolysin activity. Indeed it has been noted on repeated occasions (11, 31) that an 8325-4 traP mutant is nonhemolytic when tested using sheep blood agar. Therefore, we analyzed the traP mutant in both the 8325-4 and Newman backgrounds for secreted hemolytic activity using sheep blood agar plates (Fig. 1). As a negative control, an existing agr-null strain was also included for comparison. Regardless of the background, inactivation of traP had no discernible affect on the secreted hemolytic activity of S. aureus. Indeed, this observation is even more striking in comparison to the agr mutant, which displayed a total lack of detectable hemolysis about its periphery.
FIG. 1.
Secreted hemolytic activity of the traP mutant. S. aureus strains were streaked onto TSA sheep blood agar (Remel) and incubated for either 24 h (8325-4 lineage strains) (A) or 48 h (Newman lineage strains) (B). Tight zones of clearing around the immediate periphery of strains indicate secreted α-hemolysin, while the more diffuse zones around the strains correspond to secreted β-hemolysin.
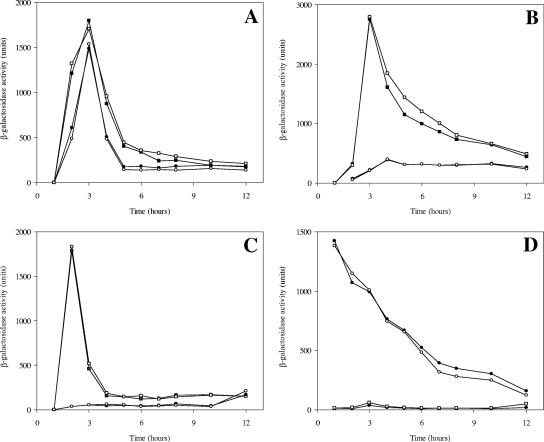
Transcriptional quantification reveals TRAP to play no role in the modulation of agr transcription or activity.
Further to our analysis of secreted hemolysis, we proceeded to specifically quantify the effect of traP deletion on the transcription of classically agr-regulated genes. Those selected were hld, which is encoded by RNAIII and as such serves as a direct measure of agr transcription; the sspA serine protease gene, which has been shown repeatedly to be positively regulated by the agr system (13, 32, 33, 41, 58); the gene for surface protein A (spa), an equally well-documented component known to be classically repressed by agr (14, 54, 65); and the α-hemolysin gene itself (hla) so as to corroborate our activity findings. The expression of each of these genes has been shown to be controlled by TRAP, in an agr-mediated manner, as detailed by a recent transcriptional profiling study (37). These investigations were again conducted in both the 8325-4 and Newman backgrounds so as to give a representative analysis of the role of TRAP.
In every instance tested there was absolutely no alteration in expression of each of these genes when comparing the traP::kan mutant to the parental strain in both S. aureus backgrounds (Fig. 2). In each example the timing, level, and temporal pattern of expression for hld, hla, sspA, and spa appeared in the wild-type exactly as they do in the traP mutant. This would indicate that the loss of TRAP in both Newman and 8325-4 backgrounds has no impact whatsoever on the transcriptional regulation of agr or on the expression of those genes in the agr regulon.
FIG. 2.
Transcription profiling analysis. The transcriptional activities of hld (RNAIII) (A), α-hemolysin (hla) (B), V8 serine protease (sspA) (C), and surface protein A (spa) (D) were measured throughout growth in the 8325-4 (▪), 8325-4 traP::kan (□), Newman (•), and Newman traP::kan (○) backgrounds. All strains were grown at 37°C with shaking, and samples taken at the times indicated were assayed for β-galactosidase activity. The results are representative of at least three separate experiments.
Disruption of traP has no bearing on secreted or surface protein profiles of S. aureus.
Agr has been speculated to regulate over 100 genes in the S. aureus genome (24, 74). Furthermore, the work of Korem et al. (37) demonstrates that TRAP itself regulates more than 75 genes, an effect which is largely speculated to be a direct result of its modulation of agr. Thus, we undertook analysis of the secreted and surface-associated proteins of S. aureus in both the Newman and 8325-4 backgrounds in order to determine if any alteration in protein profiles between the parent and TRAP mutant strain could be observed. As with the hemolysis experiments, an agr mutant strain was also included in order to function as a representative control. No detectable variation in secreted protein profiles in either the 8325-4 or Newman background was observed between the parental strain and the traP::kan isogenic mutants (Fig. 3A and B). The same cannot be said when comparing the agr mutant to either the parental strain or the traP::kan mutant, which shows pleiotropic alterations in the proteins secreted by both S. aureus strains. The same series of observations were also made for the surface-associated protein profiles in each background (Fig. 3C and D), where no variation between the traP::kan mutant and parent could be seen in either the 8325-4 or Newman background. Again, as with the secreted proteins, the agr mutant strain displays widely different surface-associated protein profiles. Indeed, densitometric analysis (conducted using the Fujifilm Multi Gauge software) of the 55-kDa protein band corresponding to surface protein A in the Newman lineage strains reveals no deviation in protein levels between the traP::kan mutant and its parental strain. An approximately twofold increase in the intensity of this band is observed between Newman and the Newman agr::tet mutant.
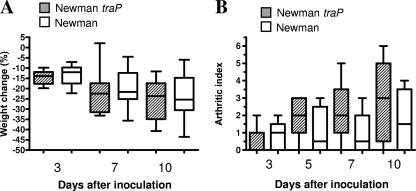
Analysis using a murine model of septic arthritis infection reveals TRAP to be entirely dispensable for the virulence of S. aureus.
Arguably the most striking characteristic attributed to mutations in traP is the lack of virulence in animal models of infection (31). Therefore, we decided to test the mutation using our well-established model of murine septic arthritis (63) in an attempt to definitively attribute a role for TRAP in S. aureus pathogenesis. The choosing of this model is particularly pertinent as the TRAP antagonist RIP has been shown to protect mice from S. aureus infection in this very same model (4). Furthermore, agr has previously been shown to be vital for full virulence in this model of infection (1); thus, should TRAP wield influence on S. aureus physiology via agr modulation, then the loss of TRAP in this model should render the mutant entirely avirulent.
Accordingly mice were inoculated with 4 × 106 organisms of either Newman or the isogenic Newman trap::kan mutant in a blinded fashion and monitored for acute signs of septic arthritis via mortality, weight loss, and an established arthritic index. At 10 days postinoculation, one mouse from the Newman group had died, while two from the mutant group had died. Furthermore, evaluation of the weight loss in both groups during the course of the infection revealed no statistically significant alterations in weight fluctuation between Newman- and Newman traP::kan-infected mice (Fig. 4A). Finally, analysis for overt signs of arthritic disease in each mouse revealed that six out of nine mice inoculated with strain Newman had clear signs of arthritic infection, while seven out of eight mice inoculated with Newman traP::kan displayed overt signs of the disease (Fig. 4B). Blinded scoring of the severity of infection revealed absolutely no discernible difference between infection groups. Thus, it is apparent that TRAP is entirely dispensable for the progression of septic arthritis using our murine model of infection, an observation that is somewhat incongruous with the findings of Gov et al. (31).
FIG. 4.
The presence of a functional traP locus is not required for the virulence of S. aureus in a murine model of septic arthritis. Female NRMI mice were inoculated with either S. aureus Newman or Newman traP::kan. Animals were continuously monitored over the course of the 10-day infection for weight loss (A) and for overt signs of arthritis in a double-blind fashion using an established arthritic index (B). Error bars indicate standard deviations. No statistically significance difference could be discerned between the two infection groups.
DISCUSSION
Here we have described a specific and independent analysis of the TRAP-based system of Staphylococcus aureus that has recently been referred to as SQS1 (31). Balaban and coworkers have published a number of papers detailing SQS1 as the master regulator of pathogenesis in S. aureus, which resides at the top of the regulation cascade by controlling agr (5, 6, 7, 8, 31, 37, 38). Other groups within the S. aureus research community have questioned the validity of the findings of Balaban and coworkers (45, 50, 52, 53), and thus we concluded that an independent study to support or refute these findings was of paramount importance to our understanding of this field. What we have found is that in not a single instance can we provide any data to support the claims of Balaban et al. that SQS1 serves to regulate agr, and thus virulence determinant synthesis and pathogenesis, in S. aureus.
It has previously been shown that mutants lacking the effector molecule of SQS1, TRAP, are entirely nonhemolytic when tested using blood agar media (11, 31). Our investigations found that, quite conversely, the TRAP-negative mutant appears to be equally as hemolytic as the parental strain in both S. aureus 8325-4 and Newman. Furthermore, our transcriptional analysis studies revealed the temporal regulation of α-hemolysin remains unchanged in the TRAP mutant in both of our wild-type strains. Indeed, not only is hla transcription unaffected by the traP mutation, but we can find no alteration in agr transcription either. Further to this, the transcription of two other agr-regulated components, one positively regulated (sspA) and one negatively regulated (spa), also remained unaltered in the TRAP-negative mutant. It is worth noting that in the recent genome-wide transcriptional profiling study by Korem et al. (37), each of the four loci we investigated were found to be subject to regulation by TRAP. Finally, our most crucial finding is the observation that a Newman TRAP-deficient mutant is equally as virulent as its parental strain.
In their 2004 publication, Balaban and coworkers detailed that an 8325-4 traP mutant was completely attenuated in virulence in a murine model of cellulitis (31). We acknowledge that our infection model and wild-type background strain are different from those used by Balaban et al.; however, it should be noted that the absolute requirement for agr in our infection model has previously been demonstrated (1). Thus, should SQS1 function as described by Balaban and coworkers, by modulating agr activity, then one would reasonably expect a TRAP mutant to be equally attenuated in the septic arthritis model of infection. Indeed, both RIP and RAP, antagonistic components of SQS1 that modulate TRAP activity, have both been described extensively as playing a central role in the capacity of S. aureus to initiate disease. RAP has been successfully used to vaccinate and protect mice prior to infection with S. aureus (5, 70), while RIP has been used successfully to therapeutically arrest infections caused by numerous strains of both S. aureus and S. epidermidis (2, 5, 7, 9, 11, 19, 20, 21, 23, 27, 28, 29, 31, 57, 66). Indeed, the efficacy of RIP in preventing infection in our own septic arthritic model of infection has already been demonstrated (4). Additionally, in that same study it was observed that the protective role of RIP is neither model nor strain specific. Thus, by extension, unless RIP possesses another role outside of its modulation of TRAP activity, then it follows that the entire SQS1 system, TRAP included, is vital for all S. aureus infections. However, given our own infection model analyses, one is left to question the validity of the findings regarding SQS1 in S. aureus pathogenesis.
An obvious explanation for the disparity between our results and those of the Balaban group is not immediately forthcoming. However, there are a number of discrepancies within the literature that may shed some light on the matter. First, one overriding concern presents itself from the study of Balaban et al. (7) in which the TRAP mutant used, termed OU20, was created and analyzed in the RN4220 background. Recent analysis by Traber and Novick (64) has demonstrated that RN4220 has a defect in its agr locus which results in it being nonhemolytic and suffering from a delay in agr activation by at least 2 to 3 h. Thus, any analysis of RNAIII, or indeed agr function, conducted in RN4220 would prove to be, at best, less than ideal. Furthermore, it would appear that the wild-type strain used for comparison with OU20 was RN6390b, yet analysis of RN4220 with RN6390 is clearly not a valid comparison in light of the work of Traber and Novick.
We acknowledge that in their paper Balaban et al. (7) include a footnote stating that the same traP mutation was also made and analyzed in 8325-4 and was found to be similar to that in RN4220. However, no data are presented to verify this statement, and in light of the data of Traber and Novick (64), it is clear 8325-4 and RN4220 are widely different strains. A subsequent publication on TRAP by Gov et al. (31) introduces a newly generated TRAP mutant (and the one utilized in the present study), which was made via alternate techniques (61) and analyzed in the 8325-4 background. We cannot readily find a direct explanation for the difference in observations between this paper and that of Gov et al. (31); however, one explanation does present itself. The agr locus of S. aureus is a huge physiological burden on the organism, particularly in the in vitro environment, where it proves to be largely superfluous. Thus, it has been observed by many groups that when incorrectly handled, random and spontaneous mutations occur in agr, rendering it nonfunctional (13, 34, 45, 55, 62, 67, 68). While we cannot categorically state that this is the overriding explanation for the observations of Balaban and coworkers, the spontaneous mutation of agr in their TRAP mutant strain would indeed explain their data. Indeed, the legitimacy of this explanation can easily be tested via additional transductional outcross analyses and, in a broader context, speaks to the need for implementing care when handling mutations with such profound effects on cellular physiology. Additionally, this scenario readily explains the findings of the recent traP microarray study (37), where the TRAP regulon was found to almost entirely overlap with the previously reported agr regulon (24).
The apparent efficacy of RIP and RAP as therapeutic treatments of staphylococcal diseases is well documented (2, 5, 7, 9, 11, 19-21, 23, 27, 28, 29, 31, 57, 66, 70); however, given that we have demonstrated no role for TRAP in the pathogenesis of S. aureus, it must be concluded that any effectivity that these agents may have is not the result of their TRAP-mediated, agr-modulating activity. The existence of RAP is indeed contentious, with other groups unable to demonstrate its presence in the supernatants of S. aureus cultures (50). In the publication by Gov et al. (31), the presence of TRAP-like signal-transducing proteins in other gram-positive pathogens is noted, with reference being made to those from Listeria spp. and Bacillus spp. being phosphorylated. Furthermore, in a 2003 publication by Balaban et al. (6), the presence in S. epidermidis of a phosphorylated TRAP that is modulated by RIP is detailed. These observations are curious given that in the 2003 publication by Korem et al. (38) it is noted that L2, or RAP, is seemingly secreted only by strains of S. aureus. We acknowledge that while there is no current evidence regarding that fate of L2 in the Listeria or Bacillus strains referred to by Gov et al. (31), the 2003 paper by Korem et al. (38) clearly shows that S. epidermidis does not secrete L2 into the culture medium. Thus, the phosphorylation of TRAP in S. epidermidis seemingly occurs either in a RAP-independent manner or in a manner at odds with that noted for S. aureus. These apparent discrepancies would seemingly cast doubt on the validity of the RIP/RAP/TRAP system as an overarching signal transduction mechanism as proposed by Balaban and coworkers.
The presence and function of RIP are somewhat unusual and still something of a mystery. Indeed, the actual designation RIP is now somewhat confusing, as multiple and varying chemical manifestations of this peptide have been investigated by Balaban and coworkers, yet all are simply referred to as RIP (2, 5, 7, 9, 11, 19-21, 23, 27-29, 31, 57, 66). RIP was originally identified as being secreted by an exoprotein-deficient, nitrosoguanidine-mutated derivative of S. aureus Foggi, termed RN833 (9). Later analysis has shown the strain to either be S. warnerii, S. xylosus, or maybe even S. hominis (10, 50). Regardless of its true origin, it is apparent that RIP is produced by a staphylococcus other than S. aureus. Thus, the suggestion by Novick and coworkers that RIP is actually an AIP that serves via the classic model to inhibit agr in nonself staphylococci (49) is both reasonable and plausible. Indeed, the sequence of RIP is remarkably similar to that of AgrD from S. warnerii, as observed by Novick and coworkers (50). However, Balaban et al. insist that RIP is encoded within the S. xylosus genome at a location other than the agr operon and that the peptide functions in a linear form (7, 8). It has been shown by independent groups that AIPs do not function as linear peptides and that they require a dehydration event to form the cyclic thiolactone based around the conserved cysteine residue (2, 36, 43, 53). Given that the RIP derivatives produced by Balaban et al. are linear peptides lacking the conserved cysteine, the specific nature by which RIP functions is unclear; however, given our findings, it seems obvious that it is not functioning via the inhibition of agr under the proposed model of Balaban and coworkers. It is quite possible that the observation of Otto (52) that the concentrations at which RIP has been used (∼10 to 50 mg/liter) are in a range at which most peptides with a degree of amphipathy can inhibit adhesion in a detergent-like manner may explain this conundrum.
In summary, we have conducted an independent analysis of the RIP/RAP/TRAP system as defined by Balaban and coworkers and can find absolutely no evidence for its role in the regulation of agr or of other virulence determinants in S. aureus. It is unclear exactly what the true role of TRAP is in S. aureus physiology, but it is clear that it has no role in regulation or pathogenesis.
Acknowledgments
We kindly thank Mark Smeltzer and Laura Tsang for sharing strains and unpublished data with us.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 4 June 2007.
REFERENCES
- 1.Abdelnour, A., S. Arvidson, T. Bremell, C. Ryden, and A. Tarkowski. 1993. The accessory gene regulator (agr) controls Staphylococcus aureus virulence in a murine arthritis model. Infect. Immun. 61:3879-3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anguita-Alonso, P., A. Giacometti, O. Cirioni, R. Ghiselli, F. Orlando, V. Saba, G. Scalise, M. Sevo, R. Patel, and N. Balaban. 2007. RNAIII-inhibiting peptide-loaded polymethylmethacrylate prevents in vivo Staphylococcus aureus biofilm formation. Antimicrob. Agents Chemother. 51:2594-2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arvidson, S., and K. Tegmark. 2001. Regulation of virulence determinants in Staphylococcus aureus. Int. J. Med. Microbiol. 291:159-170. [DOI] [PubMed] [Google Scholar]
- 4.Balaban, N., O. Cirioni, A. Giacometti, R. Ghiselli, J. B. Braunstein, C. Silvestri, F. Mocchegiani, V. Saba, and G. Scalise. 2007. Treatment of Staphylococcus aureus biofilm infection by the quorum-sensing inhibitor RIP. Antimicrob. Agents Chemother. 51:2226-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balaban, N., L. V. Collins, J. S. Cullor, E. B. Hume, E. Medina-Acosta, O. Vieira da Motta, R. O'Callaghan, P. V. Rossitto, M. E. Shirtliff, L. Serafim da Silveira, A. Tarkowski, and J. V. Torres. 2000. Prevention of diseases caused by Staphylococcus aureus using the peptide RIP. Peptides 21:1301-1311. [DOI] [PubMed] [Google Scholar]
- 6.Balaban, N., A. Giacometti, O. Cirioni, Y. Gov, R. Ghiselli, F. Mocchegiani, C. Viticchi, M. S. Del Prete, V. Saba, G. Scalise, and G. Dell'Acqua. 2003. Use of the quorum-sensing inhibitor RNAIII-inhibiting peptide to prevent biofilm formation in vivo by drug-resistant Staphylococcus epidermidis. J. Infect. Dis. 187:625-630. [DOI] [PubMed] [Google Scholar]
- 7.Balaban, N., T. Goldkorn, Y. Gov, M. Hirshberg, N. Koyfman, H. R. Matthews, R. T. Nhan, B. Singh, and O. Uziel. 2001. Regulation of Staphylococcus aureus pathogenesis via target of RNAIII-activating protein (TRAP). J. Biol. Chem. 276:2658-2667. [DOI] [PubMed] [Google Scholar]
- 8.Balaban, N., T. Goldkorn, R. T. Nhan, L. B. Dang, S. Scott, R. M. Ridgley, A. Rasooly, S. C. Wright, J. W. Larrick, R. Rasooly, and J. R. Carlson. 1998. Autoinducer of virulence as a target for vaccine and therapy against Staphylococcus aureus. Science 280:438-440. [DOI] [PubMed] [Google Scholar]
- 9.Balaban, N., and R. P. Novick. 1995. Autocrine regulation of toxin synthesis by Staphylococcus aureus. Proc. Natl. Acad. Sci. USA 92:1619-1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balaban, N., B. Singh, T. Goldkorn, A. Rasooly, J. V. Torres, and O. Uziel. 2000. Activation and inhibition of the staphylococcal AGR system. Science 287:391a. [Google Scholar]
- 11.Balaban, N., P. Stoodley, C. A. Fux, S. Wilson, J. W. Costerton, and G. Dell'Acqua. 2005. Prevention of staphylococcal biofilm-associated infections by the quorum sensing inhibitor RIP. Clin. Orthoped. Rel. Res. 437:48-54. [DOI] [PubMed] [Google Scholar]
- 12.Bischoff, M., P. Dunman, J. Kormanec, D. Macapagal, E. Murphy, W. Mounts, B. Berger-Bachi, and S. Projan. 2004. Microarray-based analysis of the Staphylococcus aureus σB regulon. J. Bacteriol. 186:4085-4099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bjorklind, A., and S. Arvidson. 1980. Mutants of Staphylococcus aureus affected in the regulation of exoprotein synthesis. FEMS Microbiol. Lett. 7:203-206. [Google Scholar]
- 14.Chan, P. F., and S. J. Foster. 1998. The role of environmental factors in the regulation of virulence-determinant expression in Staphylococcus aureus 8325-4. Microbiology 144:2469-2479. [DOI] [PubMed] [Google Scholar]
- 15.Chan, P. F., and S. J. Foster. 1998. Role of SarA in virulence determinant production and environmental signal transduction in Staphylococcus aureus. J. Bacteriol. 180:6232-6241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung, A. L., J. M. Koomey, C. A. Butler, S. J. Projan, and V. A. Fischetti. 1992. Regulation of exoprotein expression in Staphylococcus aureus by a locus (sar) distinct from agr. Proc. Natl. Acad. Sci. USA 89:6462-6466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung, A. L., and P. Ying. 1994. Regulation of alpha- and beta-hemolysins by the sar locus of Staphylococcus aureus. J. Bacteriol. 176:580-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheung, A. L., and G. Zhang. 2002. Global regulation of virulence determinants in Staphylococcus aureus by the SarA protein family. Front. Biosci. 7:1825-1842. [DOI] [PubMed] [Google Scholar]
- 19.Cirioni, O., A. Giacometti, R. Ghiselli, G. Dell'Acqua, Y. Gov, W. Kamysz, J. Lukasiak, F. Mocchegiani, F. Orlando, G. D'Amato, N. Balaban, V. Saba, and G. Scalise. 2003. Prophylactic efficacy of topical temporin A and RNAIII-inhibiting peptide in a subcutaneous rat pouch model of graft infection attributable to staphylococci with intermediate resistance to glycopeptides. Circulation 108:767-771. [DOI] [PubMed] [Google Scholar]
- 20.Cirioni, O., A. Giacometti, R. Ghiselli, G. Dell'Acqua, F. Orlando, F. Mocchegiani, C. Silvestri, A. Licci, V. Saba, G. Scalise, and N. Balaban. 2006. RNAIII-inhibiting peptide significantly reduces bacterial load and enhances the effect of antibiotics in the treatment of central venous catheter-associated Staphylococcus aureus infections. J. Infect. Dis. 193:180-186. [DOI] [PubMed] [Google Scholar]
- 21.Dell'Acqua, G., A. Giacometti, O. Cirioni, R. Ghiselli, V. Saba, G. Scalise, Y. Gov, and N. Balaban. 2004. Suppression of drug-resistant staphylococcal infections by the quorum-sensing inhibitor RNAIII-inhibiting peptide. J. Infect. Dis. 190:318-320. [DOI] [PubMed] [Google Scholar]
- 22.Deora, R., T. Tseng, and T. K. Misra. 1997. Alternative transcription factor σB of Staphylococcus aureus: characterization and role in transcription of the global regulatory locus sar. J. Bacteriol. 179:6355-6359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Domenico, P., E. Gurzenda, A. Giacometti, O. Cirioni, R. Ghiselli, F. Orlando, M. Korem, V. Saba, G. Scalise, and N. Balaban. 2004. BisEDT and RIP act in synergy to prevent graft infections by resistant staphylococci. Peptides 25:2047-2053. [DOI] [PubMed] [Google Scholar]
- 24.Dunman, P. M., E. Murphy, S. Haney, D. Palacios, G. Tucker-Kellogg, S. Wu, E. L. Brown, R. J. Zagursky, D. Shlaes, and S. J. Projan. 2001. Transcription profiling-based identification of Staphylococcus aureus genes regulated by the agr and/or sarA loci. J. Bacteriol. 183:7341-7353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duthie, E. S., and L. L. Lorenz. 1952. Staphylococcal coagulase; mode of action and antigenicity. J. Gen. Microbiol. 6:95-107. [DOI] [PubMed] [Google Scholar]
- 26.Fournier, B., A. Klier, and G. Rapoport. 2001. The two-component system ArlS-ArlR is a regulator of virulence gene expression in Staphylococcus aureus. Mol. Microbiol. 41:247-261. [DOI] [PubMed] [Google Scholar]
- 27.Ghiselli, R., A. Giacometti, O. Cirioni, G. Dell'Acqua, C. Bergnach, F. Orlando, F. Mocchegiani, C. Silvestri, B. Skerlavaj, A. Licci, N. Balaban, M. Zanetti, G. Scalise, and V. Saba. 2006. RNAIII-inhibiting peptide in combination with the cathelicidin BMAP-28 reduces lethality in mouse models of staphylococcal sepsis. Shock 26:296-301. [DOI] [PubMed] [Google Scholar]
- 28.Giacometti, A., O. Cirioni, R. Ghiselli, G. Dell'Acqua, F. Orlando, G. D'Amato, F. Mocchegiani, C. Silvestri, M. S. Del Prete, M. Rocchi, N. Balaban, V. Saba, and G. Scalise. 2005. RNAIII-inhibiting peptide improves efficacy of clinically used antibiotics in a murine model of staphylococcal sepsis. Peptides 26:169-175. [DOI] [PubMed] [Google Scholar]
- 29.Giacometti, A., O. Cirioni, Y. Gov, R. Ghiselli, M. S. Del Prete, F. Mocchegiani, V. Saba, F. Orlando, G. Scalise, N. Balaban, and G. Dell'Acqua. 2003. RNA III-inhibiting peptide inhibits in vivo biofilm formation by drug-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 47:1979-1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giraudo, A. T., C. G. Raspanti, A. Calzolari, and R. Nagel. 1994. Characterization of a Tn551-mutant of Staphylococcus aureus defective in the production of several exoproteins. Can. J. Microbiol. 40:677-681. [DOI] [PubMed] [Google Scholar]
- 31.Gov, Y., I. Borovok, M. Korem, V. K. Singh, R. K. Jayaswal, B. J. Wilkinson, S. M. Rich, and N. Balaban. 2004. Quorum sensing in staphylococci is regulated via phosphorylation of three conserved histidine residues. J. Biol. Chem. 279:14665-14672. [DOI] [PubMed] [Google Scholar]
- 32.Horsburgh, M. J., J. L. Aish, I. J. White, L. Shaw, J. K. Lithgow, and S. J. Foster. 2002. σB modulates virulence determinant expression and stress resistance: characterization of a functional rsbU strain derived from Staphylococcus aureus 8325-4. J. Bacteriol. 184:5457-5467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janzon, L., and S. Arvidson. 1990. The role of the delta-lysin gene (hld) in the regulation of virulence genes by the accessory gene regulator (agr) in Staphylococcus aureus. EMBO J. 9:1391-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Janzon, L., S. Lofdahl, and S. Arvidson. 1989. Identification and nucleotide sequence of the delta-lysin gene, hld, adjacent to the accessory gene regulator (agr) of Staphylococcus aureus. Mol. Gen. Genet. 219:480-485. [DOI] [PubMed] [Google Scholar]
- 35.Ji, G., R. Beavis, and R. P. Novick. 1997. Bacterial interference caused by autoinducing peptide variants. Science 276:2027-2030. [DOI] [PubMed] [Google Scholar]
- 36.Ji, G., R. C. Beavis, and R. P. Novick. 1995. Cell density control of staphylococcal virulence mediated by an octapeptide pheromone. Proc. Natl. Acad. Sci. USA 92:12055-12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Korem, M., Y. Gov, M. D. Kiran, and N. Balaban. 2005. Transcriptional profiling of target of RNAIII-activating protein, a master regulator of staphylococcal virulence. Infect. Immun. 73:6220-6228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Korem, M., A. S. Sheoran, Y. Gov, S. Tzipori, I. Borovok, and N. Balaban. 2003. Characterization of RAP, a quorum sensing activator of Staphylococcus aureus. FEMS Microbiol. Lett. 223:167-175. [DOI] [PubMed] [Google Scholar]
- 39.Kornblum, J., B. N. Kreiswirth, S. J. Projan, H. F. Ross, and R. P. Novick. 1990. Agr: a polycistronic locus regulating exoprotein synthesis in Staphylococcus aureus, p. 373-402. In R. P. Novick (ed.), Molecular biology of the staphylococci. VCH Publishers, New York, NY.
- 40.Lina, G., S. Jarraud, G. Ji, T. Greenland, A. Pedraza, J. Etienne, R. P. Novick, and F. Vandenesch. 1998. Transmembrane topology and histidine protein kinase activity of AgrC, the agr signal receptor in Staphylococcus aureus. Molec. Microbiol. 28:655-662. [DOI] [PubMed] [Google Scholar]
- 41.Lindsay, J. A., and S. J. Foster. 1999. Interactive regulatory pathways control virulence determinant production and stability in response to environmental conditions in Staphylococcus aureus. Mol. Gen. Genet. 262:323-331. [DOI] [PubMed] [Google Scholar]
- 42.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 43.Mayville, P., G. Ji, R. Beavis, H. Yang, M. Goger, R. P. Novick, and T. W. Muir. 1999. Structure-activity analysis of synthetic autoinducing thiolactone peptides from Staphylococcus aureus responsible for virulence. Proc. Natl. Acad. Sci. USA 96:1218-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McAleese, F. M., E. J. Walsh, M. Sieprawska, J. Potempa, and T. J. Foster. 2001. Loss of clumping factor B fibrinogen binding activity by Staphylococcus aureus involves cessation of transcription, shedding and cleavage by metalloprotease. J. Biol. Chem. 276:29969-29978. [DOI] [PubMed] [Google Scholar]
- 45.McNamara, P. J., and J. J. Iandolo. 1998. Genetic instability of the global regulator agr explains the phenotype of the xpr mutation in Staphylococcus aureus KSI9051. J. Bacteriol. 180:2609-2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morfeldt, E., I. Panova-Sapundjieva, B. Gustafsson, and S. Arvidson. 1996. Detection of the response regulator AgrA in the cytosolic fraction of Staphylococcus aureus by monoclonal antibodies. FEMS Microbiol. Lett. 143:195-201. [DOI] [PubMed] [Google Scholar]
- 47.Novick, R. P. 2003. Autoinduction and signal transduction in the regulation of staphylococcal virulence. Mol. Microbiol. 48:1429-1449. [DOI] [PubMed] [Google Scholar]
- 48.Novick, R. P. 2000. Pathogenicity factors and their regulation, p. 392-407. In V. A. Fischetti, R. P. Novick, J. J. Ferretti, D. A. Portnoy, and J. I. Rood (ed.), Gram-positive pathogens. ASM Press, Washington, DC.
- 49.Novick, R. P., S. J. Projan, J. Kornblum, H. F. Ross, G. Ji, B. Kreiswirth, F. Vandenesch, and S. Moghazeh. 1995. The agr P2 operon: an autocatalytic sensory transduction system in Staphylococcus aureus. Mol. Gen. Genet. 248:446-458. [DOI] [PubMed] [Google Scholar]
- 50.Novick, R. P., H. F. Ross, A. M. S. Figueiredo, G. Abramochkin, and T. Wuir. 2000. Activation and inhibition of the staphylococcal AGR system. Science 287:391a. [Google Scholar]
- 51.Novick, R. P., H. F. Ross, S. J. Projan, J. Kornblum, B. Kreiswirth, and S. Moghazeh. 1993. Synthesis of staphylococcal virulence factors is controlled by a regulatory RNA molecule. EMBO J. 12:3967-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Otto, M. 2004. Quorum-sensing control in staphylococci—a target for antimicrobial drug therapy? FEMS Microbiol. Lett. 241:135-141. [DOI] [PubMed] [Google Scholar]
- 53.Otto, M., R. Sussmuth, G. Jung, and F. Gotz. 1998. Structure of the pheromone peptide of the Staphylococcus epidermidis agr system. FEBS Lett. 424:89-94. [DOI] [PubMed] [Google Scholar]
- 54.Patel, A. H., J. Kornblum, B. Kreiswirth, R. Novick, and T. J. Foster. 1992. Regulation of the protein A-encoding gene in Staphylococcus aureus. Gene 114:25-34. [DOI] [PubMed] [Google Scholar]
- 55.Peng, H. L., R. P. Novick, B. Kreiswirth, J. Kornblum, and P. Schlievert. 1988. Cloning, characterization, and sequencing of an accessory gene regulator (agr) in Staphylococcus aureus. J. Bacteriol. 170:4365-4372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qiu, R., W. Pei, L. Zhang, J. Lin, and G. Ji. 2005. Identification of the putative staphylococcal AgrB catalytic residues involving the proteolytic cleavage of AgrD to generate autoinducing peptide. J. Biol. Chem. 280:16695-16704. [DOI] [PubMed] [Google Scholar]
- 57.Ribeiro, P. D., O. D. Ribeiro, A. M. Marcolan, and E. Medina-Acosta. 2003. Treatment efficacy of the lead RNAIII-inhibiting peptide YSPWTNF-NH2 in acquired Staphylococcus aureus sepsis: a histopathological assessment. Peptides 24:1829-1836. [DOI] [PubMed] [Google Scholar]
- 58.Shaw, L., E. Golonka, J. Potempa, and S. J. Foster. 2004. The role and regulation of the extracellular proteases of Staphylococcus aureus. Microbiology 150:217-228. [DOI] [PubMed] [Google Scholar]
- 59.Shaw, L. N., J. Aish, J. E. Davenport, M. C. Brown, J. K. Lithgow, K. Simmonite, H. Crossley, J. Travis, J. Potempa, and S. J. Foster. 2006. Investigations into σB-modulated regulatory pathways governing extracellular virulence determinant production in Staphylococcus aureus. J. Bacteriol. 188:6070-6080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shaw, L. N., E. Golonka, G. Szmyd, S. J. Foster, J. Travis, and J. Potempa. 2005. Cytoplasmic control of premature activation of a secreted protease zymogen: deletion of staphostatin B (SspC) in Staphylococcus aureus 8325-4 yields a profound pleiotropic phenotype. J. Bacteriol. 187:1751-1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Singh, V. K., R. K. Jayaswal, and B. J. Wilkinson. 2001. Cell wall-active antibiotic induced proteins of Staphylococcus aureus identified using a proteomic approach. FEMS Microbiol. Lett. 199:79-84. [DOI] [PubMed] [Google Scholar]
- 62.Somerville, G. A., S. B. Beres, J. R. Fitzgerald, F. R. DeLeo, R. L. Cole, J. S. Hoff, and J. M. Musser. 2002. In vitro serial passage of Staphylococcus aureus: changes in physiology, virulence factor production, and agr nucleotide sequence. J. Bacteriol. 184:1430-1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tarkowski, A., M. Bokarewa, L. V. Collins, I. Gjertsson, O. H. Hultgren, T. Jin, I. M. Jonsson, E. Josefsson, E. Sakiniene, and M. Verdrengh. 2002. Current status of pathogenetic mechanisms in staphylococcal arthritis. FEMS Microbiol. Lett. 217:125-132. [DOI] [PubMed] [Google Scholar]
- 64.Traber, K., and R. Novick. 2006. A slipped-mispairing mutation in AgrA of laboratory strains and clinical isolates results in delayed activation of agr and failure to translate δ- and α-hemolysins. Mol. Microbiol. 59:1519-1530. [DOI] [PubMed] [Google Scholar]
- 65.Vandenesch, F., J. Kornblum, and R. P. Novick. 1991. A temporal signal, independent of agr, is required for hla but not spa transcription in Staphylococcus aureus. J. Bacteriol. 173:6313-6320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vieira-da-Motta, O., P. D. Ribeiro, W. Dias da Silva, and E. Medina-Acosta. 2001. RNAIII inhibiting peptide (RIP) inhibits agr-regulated toxin production. Peptides 22:1621-1627. [DOI] [PubMed] [Google Scholar]
- 67.Vuong, C., S. Kocianova, Y. Yao, A. B. Carmody, and M. Otto. 2004. Increased colonization of indwelling medical devices by quorum-sensing mutants of Staphylococcus epidermidis in vivo. J. Infect. Dis. 190:1498-1505. [DOI] [PubMed] [Google Scholar]
- 68.Vuong, C., H. L. Saenz, F. Gotz, and M. Otto. 2000. Impact of the agr quorum-sensing system on adherence to polystyrene in Staphylococcus aureus. J. Infect. Dis. 182:1688-1693. [DOI] [PubMed] [Google Scholar]
- 69.Wright, J. S., III, R. Jin, and R. P. Novick. 2005. Transient interference with staphylococcal quorum sensing blocks abscess formation. Proc. Natl. Acad. Sci. USA 102:1691-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yang, G., H. Cheng, C. Liu, Y. Xue, Y. Gao, N. Liu, B. Gao, D. Wang, S. Li, B. Shen, and N. Shao. 2003. Inhibition of Staphylococcus aureus pathogenesis in vitro and in vivo by RAP-binding peptides. Peptides 24:1823-1828. [DOI] [PubMed] [Google Scholar]
- 71.Yarwood, J. M., J. K. McCormick, and P. M. Schlievert. 2001. Identification of a novel two-component regulatory system that acts in global regulation of virulence factors of Staphylococcus aureus. J. Bacteriol. 183:1113-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang, L., L. Gray, R. P. Novick, and G. Ji. 2002. Transmembrane topology of AgrB, the protein involved in the post-translational modification of AgrD in Staphylococcus aureus. J. Biol. Chem. 277:34736-34742. [DOI] [PubMed] [Google Scholar]
- 73.Zhang, L., J. Lin, and G. Ji. 2004. Membrane anchoring of the AgrD N-terminal amphipathic region is required for its processing to produce a quorum-sensing pheromone in Staphylococcus aureus. J. Biol. Chem. 279:19448-19456. [DOI] [PubMed] [Google Scholar]
- 74.Ziebandt, A. K., D. Becher, K. Ohlsen, J. Hacker, M. Hecker, and S. Engelmann. 2004. The influence of agr and σB in growth phase dependent regulation of virulence factors in Staphylococcus aureus. Proteomics 4:3034-3047. [DOI] [PubMed] [Google Scholar]