Abstract
The potential use of variola virus, the etiological agent of smallpox, as a bioterror agent has heightened the interest in the reinitiation of smallpox vaccination. However, the currently licensed Dryvax vaccine, despite its documented efficacy in eradicating smallpox, is not optimal for the vaccination of contemporary populations with large numbers of individuals with immunodeficiencies because of severe adverse effects that can occur in such individuals. Therefore, the development of safer smallpox vaccines that can match the immunogenicity and efficacy of Dryvax for the vaccination of contemporary populations remains a priority. Using the Wyeth strain of vaccinia virus derived from the Dryvax vaccine, we generated a recombinant Wyeth interleukin-15 (IL-15) with integrated IL-15, a cytokine with potent immunostimulatory functions. The integration of IL-15 into the Wyeth strain resulted in a >1,000-fold reduction in lethality of vaccinated athymic nude mice and induced severalfold-higher cellular and humoral immune responses in wild-type mice that persisted longer than those induced by the parental Wyeth strain. The superior efficacy of Wyeth IL-15 was further demonstrated by the ability of vaccinated mice to fully survive a lethal intranasal challenge of virulent vaccinia virus even 10 months after vaccination, whereas all mice vaccinated with parental Wyeth strain succumbed. By integrating IL-15 into modified vaccinia virus Ankara (MVA), a virus currently under consideration as a substitute for the Dryvax vaccine, we developed a second vaccine candidate (MVA IL-15) with greater immunogenicity and efficacy than Dryvax. Thus, Wyeth IL-15 and MVA IL-15 viruses hold promise as more-efficacious and safe alternatives to the Dryvax vaccine.
One of the greatest medical triumphs of the 20th century was the eradication of smallpox, a pestilence that had plagued mankind for thousands of years as attested by the presence of suggestive pock lesions in the mummified body of Rameses V, who died in 1160 BC (26). This monumental achievement within a span of 20 years that began as a WHO initiative in 1958 to control smallpox and then intensified in 1966 as a campaign to achieve eradication in 10 years was made possible by the relentless efforts of dedicated international teams of public health workers and epidemiologists and the availability of a highly efficacious live vaccine (18). During the smallpox eradication campaign, vaccine preparations were manufactured as infected calf lymph, a process that is now unacceptable in an era of bovine spongiform encephalopathy, from the American (Wyeth), British (Lister/Elstree), and Russian (EM63) strains of vaccinia virus with similar reactogenicities. Complications noted at the time included postvaccinal encephalitis, progressive vaccinia virus infection, especially in recipients with immunologic deficiencies, eczema vaccinatum in vaccinees or their contacts with skin eczema, and generalized vaccinia virus infection. These vaccine-associated complications were more pronounced in individuals with underlying immunodeficiencies who often contracted vaccinia by contact with a vaccinee (29, 30). Toward the later stages of the eradication campaign, a derivative of vaccinia virus, modified vaccinia virus Ankara (MVA), which had undergone over 570 passages in chicken embryo fibroblasts, resulting in the loss of over 15% of its genomic content, including many of its host-range-associated genes, was used as a prevaccine to reduce vaccine-associated complications in more than 100,000 people for whom the Dryvax vaccine was contraindicated due to preexisting immunodeficiencies or skin conditions (2, 31).
Despite the certification of the Global Commission that smallpox had been eradicated in 1979 and the discontinuation of routine smallpox vaccination by all countries, military personnel in both the United States and Russia have continued smallpox vaccinations because of the many well-recognized attributes of variola virus that can be efficiently exploited in biological warfare (41). In more-recent times, the tragic terrorist and anthrax attacks in 2001 have heightened the concerns of smallpox virus being used as a bioterror agent against civilian populations (17). Because of the discontinuation of vaccinations almost 3 decades ago, it is estimated that more than half of the global population is immunologically naïve to variola virus (8, 35). Though it is likely that people who had been previously vaccinated in the 1970s would still have some level of protection against serious disease or death (10, 11, 14, 15, 21), there have been documented cases of repeat natural infections of smallpox after a lag time of 10 or more years (18, 40). Also, revaccination every 3 years was the norm during the smallpox vaccination campaigns because of the waning of vaccine-induced immunity. Although the probability of intentional release of variola virus remains unquantifiable, the effects of such a release could be catastrophic in a nonimmune population. Spurred by the specter of the alarming possibility that smallpox could potentially be reintroduced through bioterrorism with devastating consequences, the need and the eventual possibility of a large-scale vaccination campaign in the United States are actively debated and widely contemplated. Despite its proven track record of effectively combating smallpox, the currently available licensed vaccine (Dryvax, New York City Board of Health strain; Wyeth Laboratories) can still cause serious complications in vaccinated individuals as mentioned earlier, and more recently, the occurrence of myocarditis or myopericarditis in some of the vaccinees has further eroded its suitability for present-day use (6, 20). Thus, a safer vaccine that can match the efficacy of the Dryvax vaccine is urgently needed for populations with greater numbers of individuals with immunodeficiencies or atopic skin diseases or for organ transplant recipients who can possibly acquire contact vaccinia virus from a vaccinated individual. In developing vaccine candidates with greater safety profiles suitable for contemporary populations, many different approaches are under consideration and include the deletion of putative virulence genes from the genome of the current vaccine strain (23), DNA (25, 38) or subunit vaccines that incorporate putative protective antigens of vaccinia virus (19, 22), and the use of strains, such as MVA, that have been passaged in alternative hosts, resulting in attenuation and poor replicative capacity (9, 16). There is considerable enthusiasm for moving forward with MVA for licensure at the present time (12, 32, 33, 43). MVA has been used as a prevaccine in vaccine campaigns in the 1970s in Germany in more than 100,000 immunocompromised individuals or individuals with skin conditions, thus supporting the view that it can be administered to immunodeficient people without detrimental effects (31, 42). However, what remains unproven and unknown is whether MVA can mount an immune response that can prevent the disease in an actual smallpox outbreak. Also, we have no way of knowing whether MVA would have any efficacy as a postexposure vaccine, whereas in the case of the Dryvax vaccine this has been well documented (18), although the mechanism of protection was shown to be the same for both vaccinia viruses in mice (4). In direct comparisons of immune responses generated by MVA and Dryvax in nonhuman primates, it was revealed that the immune responses generated by MVA were less robust both quantitatively and qualitatively (12, 43), thus making a compelling argument that the immunogenicity of MVA needs to be improved if it is to be used as a primary vaccine, although in its present form it may still be suitable as a prevaccine to Dryvax. Yet, another crucial unknown with respect to MVA is its potential to cause cardiotoxicity. Postvaccine (Dryvax) myopericarditis became increasingly apparent during both the civilian and military smallpox vaccination programs of 2003 as well as in the phase III trials of cell culture-derived ACAM2000 vaccine, leading to premature termination of the trial (6, 20). The problem of whether postvaccination cardiotoxicity (though not directly due to replicating virus in the cardiac tissues) is something unique to Dryvax vaccine or whether it may also be shared by less-virulent viruses, such as MVA, is a worrisome concern that can be addressed only by a large-scale MVA trial.
Collectively, these issues underscore the importance of developing and testing other alternative vaccine candidates if current efforts in advancing MVA toward licensure fail to live up to expectations. Therefore, with this goal in mind, we have focused on developing an efficacious but less reactogenic vaccine with a greater safety profile that can also be administered to immunodeficient individuals. Exploiting our previous observations that the integration of interleukin-15 (IL-15), an immune-enhancing cytokine with profound effects on CD8 memory T cells, NK cells, and cytokine-chemokine networks, into the vaccinia virus genome results in a several-thousand-fold reduction in lethality to athymic nude mice (39) yet induces longer-lived CD8 memory T cells (36) as well as higher-avidity T cells (37), we generated two vaccine candidates, namely, Wyeth-IL-15 and MVA-IL-15, and demonstrated their superior efficacy over the currently licensed Dryvax smallpox vaccine in a mouse model.
MATERIALS AND METHODS
Viruses.
Vaccinia virus Western Reserve (WR) was purchased from the American Type Culture Collection (Manassas, VA). The Wyeth New York Board of Health strain of vaccinia virus (termed “Wyeth”) was obtained from Wyeth Ayerst Laboratories (Marietta, PA). Modified vaccinia virus Ankara was kindly provided by Bernard Moss at the National Institute of Allergy and Infectious Diseases. To create recombinant vaccinia viruses carrying the human IL-15 gene, pTFHA transfer vector (1) with a 1.8-kb DNA fragment encompassing the hemagglutinin gene of the WR strain of vaccinia virus and the Escherichia coli gpt gene was used. The Wyeth strain with integrated human IL-15 (Wyeth-IL-15) and MVA with integrated human IL-15 (MVA-IL-15) were generated as described previously (39). The Wyeth strain of vaccinia virus and its recombinant derivatives were grown and titers were determined in CV-1 monkey kidney cells from the ATCC, whereas the MVA strain and its recombinant derivatives were grown in BHK-21 cells from the ATCC.
Mice and immunizations.
Female BALB/c mice (6 to 10 weeks old) were purchased from the Frederick Cancer Research Facility (Frederick, MD). Animal procedures were carried out under institutionally approved protocols. Mice were immunized subcutaneously at the tail base with 2 × 106 PFU of the viruses.
Antibodies, cytokine staining, and flow cytometry.
Fluorescent or biotin-labeled anti-mouse CD4 (GK1.5) and CD8α (53-6.7 clone) were obtained from Pharmingen. For intracellular cytokine staining, spleen CD8+ T cells from the immunized mice were stimulated with Wyeth strain-infected irradiated splenocytes. Cells were stained by following the manufacturer's protocol (Pharmingen). All antibodies were purchased from Pharmingen, and the background staining was controlled by using isotype control antibodies. Cells stained with the appropriate antibodies were analyzed on a FACSCalibur (Becton Dickinson).
Plaque reduction neutralization assay.
Sera collected from immunized or unvaccinated control mice were heat inactivated for 30 min at 56°C. Serial twofold dilutions of serum samples were mixed with an equal volume containing 150 PFU of WR vaccinia virus for 60 min at 37°C in 24-well plates, followed by the addition of 1 × 106 CV-1 cells per well. After a period of 1 h of incubation, cells were overlaid with 10% Dulbecco modified Eagle medium containing 0.75% carboxymethylcellulose. The plates were incubated at 37°C for 48 h and then stained with a solution containing 10% formaldehyde, 5% acetic acid, 60% ethanol, and 1% crystal violet. Each well was evaluated for the number of plaques, and the reciprocal serum dilution yielding a 90% reduction in the plaque count was determined and expressed as the neutralization titer. Each sample was assayed in triplicate.
Cytotoxicity assay.
Cytotoxic T-lymphocyte (CTL) activity was measured using a 5-h assay with 51Cr-labeled target cells. Spleen CD8+ T cells from the immunized mice were restimulated with Wyeth-infected and irradiated splenocytes for 1 week in a medium that contained RPMI 1640 with 10% fetal bovine serum, 4 mM glutamine, 50 μM 2-mercaptoethanol, and 10% T-STIM (rat T-STIM from BD Discovery Labware, Inc., Bedford, MA) in vitro. To infect splenocytes with the Wyeth strain of vaccinia virus, cells were incubated with 5 multiplicities of infection (MOI) of the virus for 2 h at 37°C and then washed twice with serum-free RPMI 1640 medium. P815 target cells were infected with 5 MOI of Wyeth and then pulsed with 51Cr for 2 h at 37°C. The percentage of specific 51Cr release was calculated as follows: 100 × (experimental release − spontaneous release)/(maximum release − spontaneous release). Spontaneous release was determined from target cells incubated without effector cells, and maximum release was determined in the presence of 5% Triton X-100.
Protection study.
Animals immunized with the respective viruses were challenged intranasally with 106 PFU of WR vaccinia virus 1 or 10 months after immunization. The titers of virus required for intranasal challenge experiments were determined previously (45, 46). The body weight of individual mice was measured daily. Mice with a weight loss of >25% were required to be euthanized, generally necessitating termination of the experiments. Age-matched unimmunized mice served as controls in the protection studies.
Statistical analysis.
Analysis of variance was used to determine the effects of different immunization protocols on the magnitude of cellular responses and weight change resulting from virus challenge. The Fisher least-significant-difference test and pairwise t test (two samples, two-tailed Student's t test) were used to compare pairs of immunization protocols, and significance levels were set at a P value of 0.05.
RESULTS AND DISCUSSION
Generation of IL-15-integrated Wyeth and MVA strains of vaccinia virus.
For the Wyeth strain of vaccinia virus from the Dryvax vaccine, our objective was to reduce its virulence without the removal of any genetic elements other than recombination-associated inactivation of the hemagglutinin gene from a virus that is considered a gold standard for efficacy and immunogenicity for an infectious disease vaccine, thereby enhancing its safety profile. We have previously shown that the integration of IL-15 into the neurovirulent WR strain of vaccinia virus results in a drastic reduction of its virulence when inoculated into T-cell-deficient athymic nude mice that correlated with a rapid induction of gamma interferon and inflammatory chemokines, allowing these mice to tolerate and survive an inoculum several-thousand-fold larger than that of the parental virus. The cytokine IL-15 is a 14-kDa, 114-amino-acid polypeptide with a four-α-helix bundle structure made primarily by monocytes and dendritic cells with potent effects on both innate and adaptive immune systems (reviewed in reference 44). IL-15 stimulates the proliferation of activated CD4− CD8−, CD4+ CD8+, CD4+, and CD8+ T cells and promotes the maintenance of CD8+ CD44hi memory T cells as well as the generation, proliferation, and activation of NK cells. IL-15, unlike its close relative IL-2, which plays a central role in the activation-induced cell death of T cells, actually inhibits this process while exerting no inductive effects on the generation or maintenance of regulatory T cells that can attenuate antigen-induced immune responses. In addition, IL-15 also facilitates the induction of CTLs, particularly with high avidity, that persist longer (37) as well as the immunoglobulin synthesis of B cells, thus collectively contributing to more-robust and -durable immune responses.
The integration of the human IL-15 gene into the hemagglutinin locus of the Wyeth strain resulted in a strain (Wyeth-IL-15) that displayed growth kinetics and plaque morphology similar to those of the parental Wyeth strain of vaccinia virus and secreted abundant IL-15 into the infected culture supernatant. Furthermore, the Wyeth-IL-15 strain displayed attenuation of lethality to athymic nude mice (data not shown) similar to that reported previously for the WR strain of vaccinia virus (39). On the other hand, the rationale to integrate IL-15 into MVA, which is avirulent even in immunodeficient mice or immunodeficient primates, was to enhance its relatively modest immunogenicity, especially in primates. The growth and replication of MVA-IL-15 in BHK-21 cells and primary chicken embryo fibroblasts were identical to those of parental MVA (data not shown).
Characterization of vaccine-induced cellular immune responses.
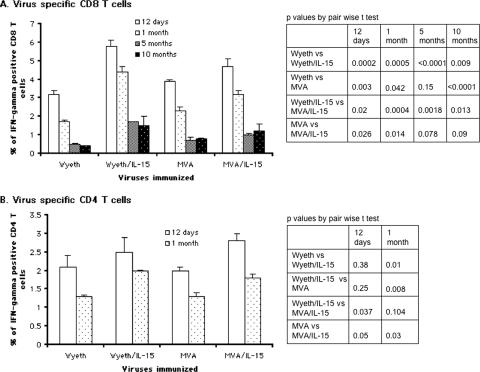
To compare the immunogenicities of IL-15-integrated vaccinia viruses, BALB/c mice were immunized with each of the vaccine candidates. An identical dose of each vaccine (2 × 106 PFU) was administered subcutaneously at the base of the tail and boosted once 4 weeks after the primary vaccination so that direct comparisons could be made among the four vaccine agents tested. The integration of IL-15 into the Wyeth strain not only attenuated its virulence but also further enhanced the immunogenicity of this virus. When vaccinia virus-specific CD8+ T-cell responses were assessed in vaccinated mice over a period of 10 months by intracellular gamma interferon (IFN-γ) cytokine staining, as shown in Fig. 1A, Wyeth-IL-15 conferred a significantly more robust response than the parental Wyeth strain (P = 0.009 at 10 months) that persisted over a period of 1 year when experiments were terminated. It was indeed remarkable to note that at 10 months postvaccination with the Wyeth-IL-15 strain, vaccinia virus-specific CD8+ T cells still accounted for more than 1.5% of total CD8+ T lymphocytes. Interestingly, the nonreplicative MVA strain, when inoculated at equivalent doses of 2 × 106 PFU, induced vaccinia virus-specific CD8+ T-cell responses in vaccinated mice on a par with those induced by the replicating Wyeth strain, with a consistent tendency to be slightly higher, which was statistically significant (P = 0.0001) at the last time point of evaluation at 10 months. More importantly, regardless of the virus strain, the integration of IL-15 resulted in enhanced, long-lived CD8+ T-cell responses consistent with what we and others have reported previously for mice (28, 36), although the degree of enhancement was more pronounced in the replicating Wyeth strain than in the nonreplicative MVA strain. When we examined the vaccinia virus-specific CD4+ T-cell responses in vaccinated mice, as shown in Fig. 1B, it was apparent that both Wyeth and MVA strains were capable of inducing similar yet robust responses in vaccinated animals. Moreover, there was a discernible yet significant improvement of this CD4+ T-cell response when IL-15 was integrated into the Wyeth and MVA strains (P = 0.01 and P = 0.03 at 1 month postvaccination for the two strains, respectively), which was somewhat unexpected because unlike in humans, the effects of IL-15 on the CD4+ T-cell subset in mice have been considered to be marginal. However, in contrast to long-lived CD8+ T-cell responses, the induced CD4+ T-cell responses were undetectable by 5 months postvaccination for all four strains regardless of whether IL-15 was used as an adjuvant.
FIG. 1.
IL-15-integrated vaccine viruses display augmented CD8+ and CD4+ T-cell responses. Animals were immunized subcutaneously with 2 × 106 PFU of the respective virus. At the indicated time points, three to four immunized animals were sacrificed and their splenocytes harvested and pooled. Stimulator cells were prepared from syngeneic splenocytes infected with the Wyeth strain of vaccinia virus at an MOI of 5 for 6 h, followed by γ-irradiation. Responder cells were stained for intracellular IFN-γ according to the vendor's protocol (Pharmingen). Panel A depicts vaccinia virus-specific CD8+ T cells, and panel B depicts vaccinia virus-specific CD4+ T cells. Data are the means ± standard errors for two separate experiments that showed similar results.
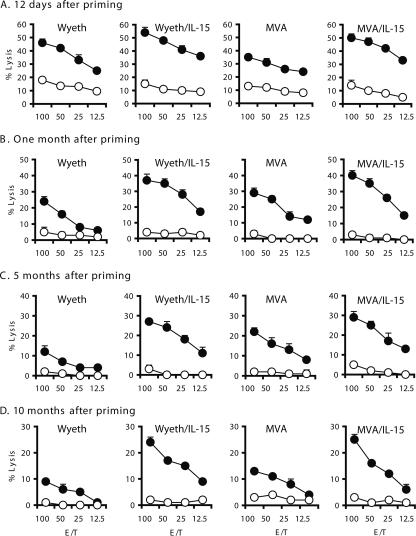
To further corroborate and validate the more dominant anti-vaccinia virus CD8 T-cell responses induced by the vaccine candidates as determined by intracellular IFN-γ staining, we performed CTL assays in parallel to determine the capacity of CD8+ T cells to lyse vaccinia virus-infected target cells. As shown in Fig. 2, the splenocytes from vaccinated animals after a 7-day in vitro restimulation in the presence of irradiated Wyeth strain-infected syngeneic splenocytes were capable of effectively lysing Wyeth strain-infected P815 mastocytoma cells. Both the greater magnitude and the longer persistence of CD8+ T-cell lytic responses for the two viral vaccine candidates expressing IL-15 were concordant with the responses obtained by intracellular IFN-γ staining.
FIG. 2.
IL-15-integrated vaccines induce CD8+ CTLs with enhanced lytic activity and prolonged memory. Animals were immunized subcutaneously with 2 × 106 PFU of the indicated vaccine candidate. Twelve days (A), 1 month (B), 5 months (C), and 10 months (D) after immunization, three to four mice were sacrificed from each group, their splenocytes were harvested and pooled, and CD8+ T cells were isolated. CD8+ T cells were then stimulated in vitro for 1 week with syngeneic splenocytes infected with the Wyeth strain of vaccinia virus at an MOI of 5 and subjected to γ-irradiation. P815 cells infected with the Wyeth strain (filled circles) served as target cells, while uninfected P815 cells (open circles) served as controls in a 5-hour 51Cr release assay. The x axis represents the effector-to-target cell ratio. Two separate experiments showed similar results, and the data presented are the means ± standard errors for a triplicate treatment in one experiment.
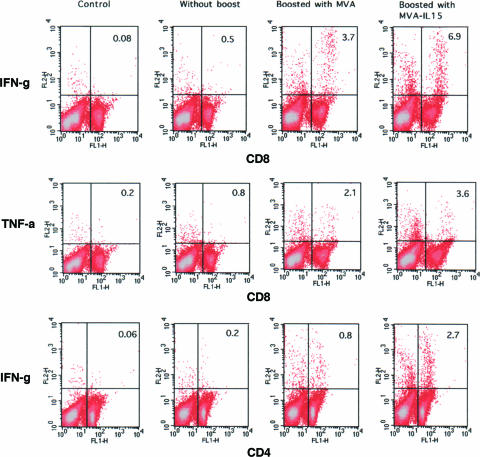
The successful use of MVA as a prevaccine prior to vaccination with a standard dose of smallpox vaccine in immunocompromised individuals during the last stages of the smallpox campaign in Germany has been documented (31, 42) and more recently has been replicated in murine as well as primate studies in which prior vaccination with MVA showed no interference with the immune responses induced by the Wyeth strain of vaccinia virus (4, 12, 33, 34, 46). However, if replication-deficient MVA vaccine is to be chosen and recommended as the most appropriate smallpox vaccine for contemporary populations, then it is critical to validate that nonreplicating MVA can induce a substantial immune response even in people who were vaccinated with the standard Dryvax vaccine almost 3 decades earlier and who still retain some level of immunity against vaccinia virus. This category of people could account for as much as 50% of the current population. Therefore, to model this scenario, first we immunized mice with a potent replication-competent vaccinia virus and allowed the anti-vaccinia virus immune response to wane over a period of 14 months, at which point we then revaccinated these animals with either nonreplicating MVA or MVA-IL-15 and monitored the induction of CD8+ and CD4+ T-cell responses by intracellular cytokine staining. As shown in Fig. 3, MVA was capable of inducing a substantial anamnestic CD8+ T-cell immune response as determined by intracellular IFN-γ as well as tumor necrosis factor alpha (TNF-α) staining, thus illustrating the polyfunctional nature of this induced anti-vaccinia virus CD8+ T-cell response. More importantly, when MVA-IL-15 was used in the revaccination instead of MVA, the induced anti-vaccinia virus polyfunctional CD8+ T-cell responses were even more dramatic (3.7% versus 6.9% for IFN-γ and 2.1% versus 3.6% for TNF-α). Consistent with the data shown in Fig. 1B, the levels of vaccinia virus-specific CD4+ T cells in vaccinated animals after 14 months were minimal. However, revaccination with MVA was able to significantly enhance the waning CD4+ T-cell responses in these animals and yet again MVA-IL-15 was superior to MVA (4-fold versus over 10-fold induction in CD4+ T-cell responses), further reinforcing the notion that IL-15 could positively affect CD4+ T-cell responses in mice. Therefore, the data shown in Fig. 1, 2, and 3 collectively indicate that the integration of IL-15 into either the Wyeth or MVA strain of vaccinia virus results in a virus that is far superior in inducing vaccinia virus-specific cellular immune responses both qualitatively, as reflected by the longer duration of the induced responses, and quantitatively.
FIG. 3.
A host previously vaccinated with a replicating vaccinia virus can be effectively boosted with replication-deficient MVA to induce cellular immune responses. Animals were first vaccinated with 2 × 106 PFU of WR vaccinia virus and 14 months later boosted with an identical dose of MVA or MVA-IL-15 virus subcutaneously. Nine days after the boost, splenocytes were harvested and pooled from three animals in each group. Pooled splenocytes were then stimulated with Wyeth strain-infected (5 MOI), irradiated syngeneic spleen cells. After in vitro stimulation, the responder cells were stained for surface CD4+ and CD8+ expression, followed by intracellular cytokine staining for IFN-γ (IFN-g) and TNF-α (TNF-a). Spleen cells from unvaccinated animals (control group) and animals that did not receive a booster vaccination were also included in the comparative analysis. The data shown are representative of two independent experiments.
Characterization of vaccine-induced antibody responses.
It was known that smallpox vaccination induced strong antibody responses in the recipients and contributed to the protection against smallpox. In fact, vaccinia virus immune globulin prepared from individuals hyperimmunized with the Dryvax vaccine was used in postexposure prophylaxis of smallpox and remains the approved standard of care for complications associated with smallpox vaccination (7, 27). Postvaccination protection studies of mice have revealed an important role for antibodies in the clearance of WR vaccinia virus after an intranasal challenge, although whether antibodies per se are responsible for this clearance remains controversial (4, 46). However, in a recent report, Edghill-Smith et al. (13) showed that in rhesus macaques, the ablation of B cells but not CD4+ or CD8+ T cells resulted in the death of monkeys vaccinated with Dryvax after an intravenous monkeypox virus challenge. Therefore, it is imperative that any potential second/third-generation smallpox vaccine be as effective as Dryvax vaccine in its ability to elicit anti-vaccinia virus antibodies in vaccine recipients.
IL-15 has been implicated in B-cell proliferation, differentiation as well as antibody synthesis, and secretion (3, 24). In addition, there is suggestive evidence to implicate a role for IL-15 in serological memory (5) and we have previously demonstrated that a recombinant vaccine with integrated IL-15 expressing the gp160 of human immunodeficiency virus generated a more robust and durable antibody response to human immunodeficiency virus gp160 than recombinant vaccinia virus that expressed gp160 alone (36).
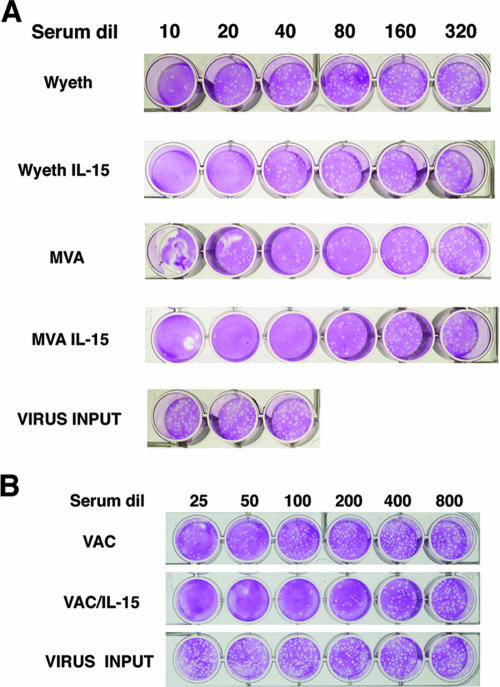
It is likely that mass vaccination against smallpox would most likely be undertaken as a consequence of intentional release of this deadly pathogen in a bioterror incident where potential recipients would have a high probability of imminent exposure or, still worse, of being postexposure victims. Therefore, it is imperative to have a validated vaccine that can induce neutralizing antibodies with sufficiently high titers with minimal lag time. In addressing this issue, we examined the kinetics of induction of vaccinia virus-neutralizing antibodies in the vaccinated mice with the four different vaccine agents. Remarkably, all four viruses induced detectable neutralizing serum antibodies by day 6 postvaccination (data not shown). However, as shown in Fig. 4A, by day 12 postvaccination, the neutralizing antibody titers were demonstrably higher in animals that received the vaccine agents with integrated IL-15 (antibody titer of 10 in Wyeth-vaccinated group versus 20 in Wyeth-IL-15-vaccinated group and a titer of 40 in MVA-vaccinated group versus 80 in MVA-IL-15-vaccinated group), indicating a clear beneficial role for IL-15 in the maturation of antibody responses. It is also noteworthy that the neutralizing antibody titer consistently appeared even higher for MVA-IL-15 than for Wyeth-IL-15 vaccination (20 versus 40). Interestingly, the presence of IL-15 in the microenvironment of initial B-cell events imparts a lasting impact on the antibody response generated since even after 14 months, neutralizing antibody levels were maintained at a higher level in mice that received vaccinia virus with integrated IL-15 than in mice that received the parental vaccinia virus, as shown in Fig. 4B (compare a titer of 25 without IL-15 to a titer of 100 with integrated IL-15).
FIG. 4.
Rapid induction of vaccinia virus-neutralizing antibodies in vaccinated animals augmented by coexpression of IL-15. (A) Animals were vaccinated with 2 × 106 PFU of the indicated vaccine agent subcutaneously, and 12 days later, blood was collected by retro-orbital bleeding and sera were separated. Within groups, sera were pooled (from five animals) and serially diluted sera were mixed with 150 PFU of WR vaccinia virus for plaque reduction neutralization. (B) Animals were vaccinated with Wyeth or Wyeth-IL-15 (2 × 106 PFU), and 14 months later, blood was collected and sera were separated. Serial dilutions (dil) of pooled sera from each group (five animals per group) were tested for the presence of vaccinia virus-neutralizing antibodies by a plaque reduction assay. The data shown are representative of three independent experiments. VAC, vaccinia virus.
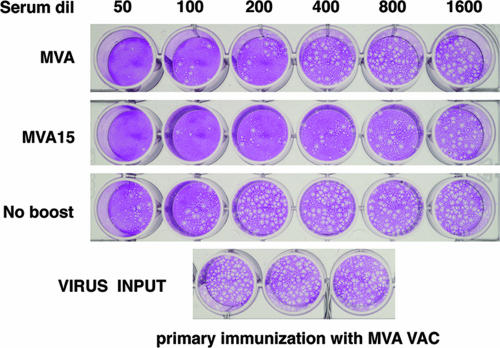
Having confirmed that vaccinia virus with integrated IL-15 induces neutralizing antibodies with higher titers that persist over an extended period of time, we were interested in assessing whether we could replicate the beneficial effects of IL-15 on persistent antibody responses in a host with preexisting vaccinia virus-neutralizing antibodies akin to someone who had previously been vaccinated. First, animals were vaccinated with MVA, and 10 weeks after primary immunization, mice were divided into three groups. One group was sham vaccinated with phosphate-buffered saline (no-boost group) and another group was boosted with MVA, whereas the last group was boosted with MVA-IL-15. Animals were then maintained for 6 months, and at that point, their serum vaccinia virus-neutralizing antibody levels were measured by a 90% plaque reduction neutralization test. As shown in Fig. 5, both MVA and MVA-IL-15 were capable of eliciting boosted antibody responses in animals with prior neutralizing antibodies against vaccinia virus. The pooled sera from animals that were not boosted had a titer of 50. However, reimmunization with a virus that coexpresses IL-15 (MVA-IL-15) results in a neutralizing antibody titer that is approximately fourfold higher than that for MVA (titer of 100 in MVA-vaccinated group versus 400 in MVA-IL-15-vaccinated group). Thus, the data from Fig. 3 and 5, taken together, would argue that even individuals who were vaccinated 3 decades ago with some remaining residual immunity against vaccinia virus are likely to respond more robustly to a smallpox vaccine with integrated IL-15.
FIG. 5.
IL-15-integrated vaccinia virus induces higher neutralizing antibody levels even in animals with preexisting vaccinia virus-neutralizing antibodies. Animals were first vaccinated with MVA (2 × 106 PFU) and boosted 10 weeks later with MVA or MVA-IL-15 (MVA15). Six months after the boosting serum, vaccinia virus-neutralizing antibody levels were determined in revaccinated animals by a plaque reduction assay, using serial dilutions (dil) of pooled sera from each group of five animals. The data shown are representative of three independent experiments. VAC, vaccinia virus.
Vaccine-induced protective efficacy after intranasal WR strain challenge.
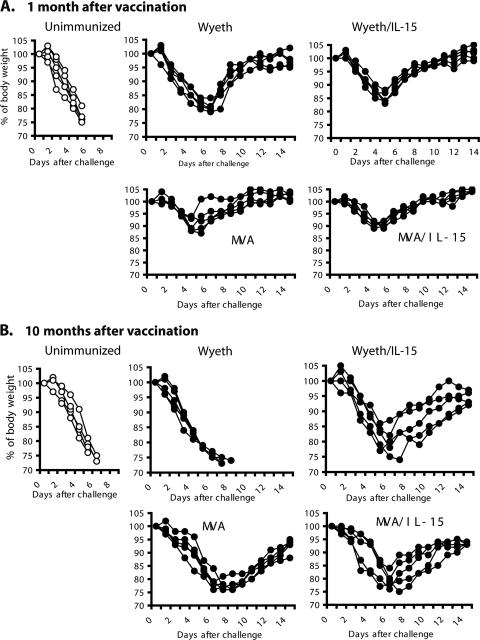
Having established that the integration of IL-15 into either Wyeth or MVA results in a derivative virus with superior immunogenicity, we wished to ascertain how this superior immunogenicity would affect protective efficacy. Mice challenged intranasally with the WR strain of vaccinia virus developed fulminant pneumonia with subsequent systemic dissemination resulting in multiorgan involvement. It is considered that the pathophysiology associated with this small animal model generally resembles some aspects of smallpox in humans, and hence, it is a reasonable model to assess the efficacy of therapeutics and vaccine candidates for smallpox (45). Therefore, we evaluated our vaccine agents with integrated IL-15 for their efficacy against intranasal challenge of vaccinated BALB/c mice with the WR strain of vaccinia virus in parallel with their parental Wyeth and MVA strains of vaccinia virus. In the first set of experiments, animals were given a single equivalent dose of vaccine (2 × 106 PFU) and then challenged with 106 PFU of WR vaccinia virus at 30 days postvaccination. As shown in Fig. 6A, all control unvaccinated animals lost more than 30% of their body weight by the 6th day postchallenge, requiring euthanization. In addition, all four groups of vaccinated animals showed some weight loss during this period following challenge but subsequently recovered fully. The degree of weight loss was as follows: control unvaccinated animals > Wyeth-vaccinated animals > Wyeth-IL-15-vaccinated animals > MVA-vaccinated animals > MVA-IL-15-vaccinated animals. The greatest weight loss among the vaccinated animals was observed in the group of animals vaccinated with the Wyeth strain (approximately 20%), and they also displayed the longest recovery time in reestablishing their body weight to prechallenge levels. Animals vaccinated with IL-15-integrated viruses generally lost less weight than their counterparts vaccinated without IL-15 and also reestablished their body weights to prechallenge levels faster. Although this pattern was consistent in two separate experiments, these differences were not statistically significant among the four groups. The protective efficacy patterns seen here for Wyeth- and MVA-vaccinated animals are in agreement with those of other published studies in that both the MVA and Wyeth strains of vaccinia virus show comparable efficacies in this mouse model (4, 9, 33, 34, 46). The slightly greater loss of body weight in Wyeth-vaccinated animals, as we saw in our studies, than in MVA-vaccinated animals has been noted by others as well (46). More importantly, in the short-term efficacy studies, because both Wyeth and MVA induced protection, the impact of the coexpression of IL-15 on the protective efficacy could have been masked, despite enhanced immunological responses in the mice vaccinated with IL-15-integrated viruses.
FIG. 6.
Animals vaccinated with IL-15-integrated vaccinia viruses better tolerate a lethal intranasal vaccinia virus challenge. Four groups of mice, five animals per group, were vaccinated with equivalent doses (2 × 106) of the respective vaccine agents. (A) Vaccinated animals were challenged 30 days after vaccination. (B) Vaccinated animals were also challenged 10 months after vaccination. For intranasal challenge of vaccinated animals, 1 × 106 PFU of the WR strain of vaccinia virus was used. The body weights of individual animals were measured daily after intranasal challenge. Age-matched unimmunized mice were included in the challenge experiments to serve as controls. Two separate experiments showed similar weight loss patterns.
Therefore, to assess any differences in the long-term durability of vaccine-induced protective efficacy among the vaccine agents, a second set of experiments was undertaken. After a single equivalent dose of the respective vaccine agent, animals were maintained for a period of 10 months before challenge with WR vaccinia virus intranasally. As shown in Fig. 6B, the disease course and the loss of body weight in the unvaccinated control animals were essentially the same as before in the short-term efficacy study following challenge with WR virus, even though here the animals were considerably aged at the time of challenge. However, what was surprising was that all five animals in the group that was vaccinated with the Wyeth strain became ill and had to be euthanized because their body weight loss exceeded 30% of the normal body weight within 10 days of challenge, whereas all the animals in the other three groups survived the WR vaccinia virus challenge despite some degree of initial weight loss. It should be noted that in animals that were vaccinated with the Wyeth strain, despite vaccine failure, there were demonstrable albeit very low levels of anti-vaccinia virus CD8+ T-cell and antibody responses. Therefore, it appears that in this mouse model, vaccine breakthrough is linked to a critical threshold of immunity against vaccinia virus, since this group had the lowest levels of CD8+ T-cell and vaccinia virus-neutralizing antibody responses (Fig. 1 and 4). More importantly, although the objective of integrating IL-15 into the Wyeth vaccine strain was to attenuate the virulence of this vaccinia virus, the expression of IL-15 also confers enhanced immunogenicity and protective efficacy to a vaccine that is already considered a gold standard for effective vaccines against infectious diseases. With respect to MVA, in the intranasal WR challenge model, as has been shown by a number of studies, MVA is on a par with Wyeth in short-term protective efficacy (4, 9, 33, 34, 46), and from the data presented in Fig. 6B, it appears to outperform Wyeth in long-term protective efficacy.
Although much has been learned about immunogenicity, protective efficacy, and the contribution of cellular and antibody responses for recovery from vaccinia virus from the intranasal WR vaccinia challenge model in mice, one needs to be cautious in extrapolating these findings in the context of primates or humans. In contrast to observations made in WR challenge experiments with mice, a limited number of studies conducted with nonhuman primates suggest that MVA is poor in immunogenicity in comparison to the licensed Dryvax Wyeth strain and have shown that at least two doses of MVA are needed to attain the level of immunogenicity conferred by a single dose of the Wyeth strain of vaccinia virus (12, 43). Correlates of protection against smallpox remain to be elucidated, and the efficacy evaluation of newer vaccine candidates remains extraordinarily complex for a fatal infectious disease that does not naturally exist at the present time. The prevailing consensus is to test such vaccine candidates in several relevant animal models for comparative efficacies and immunogenicities along with the licensed Dryvax vaccine for the licensure of such candidates. Further testing of the IL-15-integrated Wyeth and MVA strains we have generated along with the parental Wyeth and MVA strains of vaccinia virus in cynomolgus monkeys for immunogenicity and assessment of their efficacy against a monkeypox virus challenge will provide further insights into their suitability and will facilitate the fulfillment of licensing requirements for IL-15-integrated vaccinia virus as a newer-generation smallpox vaccine. In summary, by integrating IL-15 cytokine into Wyeth and MVA strains, we have developed two smallpox vaccine candidates with greater immunogenicity and efficacy yet with more-attenuated virulence than the currently licensed Dryvax vaccine suitable for contemporary populations.
Acknowledgments
We thank Bernard Moss, NIAID, for provision of reagents, advice, and support.
This work was in part supported by the Intramural Research Program of the National Cancer Institute, Center for Cancer Research, NIH, and by a 3-year competitive research funding award to L.P.P. from the Trans-NIH/FDA Intramural Biodefense Program.
Footnotes
Published ahead of print on 6 June 2007.
REFERENCES
- 1.Alexander, W. A., B. Moss, and T. R. Fuerst. 1992. Regulated expression of foreign genes in vaccinia virus under the control of bacteriophage T7 RNA polymerase and the Escherichia coli lac repressor. J. Virol. 66:2934-2942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antoine, G., F. Scheiflinger, F. Dorner, and F. G. Falkner. 1998. The complete genomic sequence of the modified vaccinia Ankara strain: comparison with other orthopoxviruses. Virology 24:365-396. [DOI] [PubMed] [Google Scholar]
- 3.Armitage, R. J., B. M. Macduff, J. Eisenman, R. Paxton, and K. H. Grabstein. 1995. IL-15 has stimulatory activity for the induction of B cell proliferation and differentiation. J. Immunol. 154:483-490. [PubMed] [Google Scholar]
- 4.Belyakov. I. M., P. L. Earl, A. Dzutsev, V. A. Kuznetsov, M. Lemon, L. S. Wyatt, J. T. Snyder, J. D. Ahlers, G. Franchini, B. Moss, and J. A. Berzofsky. 2003. Shared modes of protection against poxvirus infection by attenuated and conventional smallpox vaccine viruses. Proc. Natl. Acad. Sci. USA 100:9458-9463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernasconi, N. L., E. Traggiai, and A. Lanzavecchia. 2002. Maintenance of serological memory by polyclonal activation of human memory B cells. Science 298:2199-2202. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2003. Cardiac adverse events following smallpox vaccination—United States, 2003. Morb. Mortal. Wkly. Rep. 52:248-250. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. 2001. Vaccinia (smallpox) vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2001. Morb. Mortal. Wkly. Rep. 50(RR-10):1-25. [PubMed] [Google Scholar]
- 8.Cohen, J. 2001. Smallpox vaccinations: how much protection remains? Science 294:985. [DOI] [PubMed] [Google Scholar]
- 9.Coulibaly, S., P. Bruhl, J. Mayrhofer, K. Schmid, M. Gerencer, and F. G. Falkner. 2005. The nonreplicating smallpox candidate vaccines defective vaccinia Lister (dVV-L) and modified vaccinia Ankara (MVA) elicit robust long-term protection. Virology 341:91-101. [DOI] [PubMed] [Google Scholar]
- 10.Crotty, S., P. Felgner, H. Davies, J. Glidewell, L. Villarreal, and R. Ahmed. 2003. Long-term B cell memory in humans after smallpox vaccination. J. Immunol. 171:4969-4973. [DOI] [PubMed] [Google Scholar]
- 11.Demkowicz, W. E., Jr., R. A. Littaua, J. Wang, and F. A. Ennis. 1996. Human cytotoxic T-cell memory: long-lived responses to vaccinia virus. J. Virol. 70:2627-2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Earl, P. L., J. L. Americo, L. S. Wyatt, L. A. Eller, J. C. Whitbeck, G. H. Cohen, R. J. Eisenberg, C. J. Hartmann, D. L. Jackson, D. A. Kulesh, M. J. Martinez, D. M. Miller, E. M. Mucker, J. D. Shamblin, S. H. Zwiers, J. W. Huggins, P. B. Jahrling, and B. Moss. 2004. Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature 428:182-185. [DOI] [PubMed] [Google Scholar]
- 13.Edghill-Smith, Y., H. Golding, J. Manischewitz, L. R. King, D. Scott, M. Bray, A. Nalca, J. W. Hooper, C. A. Whitehouse, J. E. Schmitz, K. A. Reimann, and G. Franchini. 2005. Smallpox vaccine-induced antibodies are necessary and sufficient for protection against monkeypox virus. Nat. Med. 11:740-747. [DOI] [PubMed] [Google Scholar]
- 14.Eichner, M. 2003. Analysis of historical data suggests long-lasting protective effects of smallpox vaccination. Am. J. Epidemiol. 158:717-723. [DOI] [PubMed] [Google Scholar]
- 15.el-Ad, B., Y. Roth, A. Winder, Z. Tochner, T. Lublin-Tennenbaum, E. Katz, and T. Schwartz. 1990. The persistence of neutralizing antibodies after revaccination against smallpox. J. Infect. Dis. 161:446-448. [DOI] [PubMed] [Google Scholar]
- 16.Empig, C., J. R. Kenner, M. Perret-Gentil, B. E. Youree, E. Bell, A. Chen, M. Gurwith, K. Higgins, M. Lock, A. D. Rice, J. Schriewer, F. Sinangil, E. White, R. M. Buller, T. S. Dermody, S. N. Isaacs, and R. W. Moyer. 2006. Highly attenuated smallpox vaccine protects rabbits and mice against pathogenic orthopoxvirus challenge. Vaccine 24:3686-3694. [DOI] [PubMed] [Google Scholar]
- 17.Fauci, A. S. 2002. Smallpox vaccination policy—the need for dialogue. N. Engl. J. Med. 346:1319. [DOI] [PubMed] [Google Scholar]
- 18.Fenner. F., D. A. Henderson, I. Arita, et al. 1988. Smallpox and its eradication. World Health Organization, Geneva, Switzerland.
- 19.Fogg, C., S. Lustig, J. C. Whitbeck, R. J. Eisenberg, G. H. Cohen, and B. Moss. 2004. Protective immunity to vaccinia virus induced by vaccination with multiple recombinant outer membrane proteins of intracellular and extracellular virions. J. Virol. 78:10230-10237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halsell, J. S., J. R. Riddle, J. E. Atwood, the Department of Defense Smallpox Vaccination Clinical Evaluation Team, et al. 2003. Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA 289:3283-3289. [DOI] [PubMed] [Google Scholar]
- 21.Hammarlund, E., M. W. Lewis, S. G. Hansen, L. I. Strelow, J. A. Nelson, G. J. Sexton, J. M. Hanifin, and M. K. Slifka. 2003. Duration of antiviral immunity after smallpox vaccination. Nat. Med. 9:1131-1137. [DOI] [PubMed] [Google Scholar]
- 22.Heraud, J. M., Y. Edghill-Smith, V. Ayala, I. Kalisz, J. Parrino, V. S. Kalyanaraman, J. Manischewitz, L. R. King, A. Hryniewicz, C. J. Trindade, M. Hassett, W. P. Tsai, D. Venzon, A. Nalca, M. Vaccari, P. Silvera, M. Bray, B. S. Graham, H. Golding, J. W. Hooper, and G. Franchini. 2006. Subunit recombinant vaccine protects against monkeypox. J. Immunol. 177:2552-2564. [DOI] [PubMed] [Google Scholar]
- 23.Herrero-Martinez, E., K. L. Roberts, M. Hollinshead, and G. L. Smith. 2005. Vaccinia virus intracellular enveloped virions move to the cell periphery on microtubules in the absence of the A36R protein. J. Gen. Virol. 86:2961-2968. [DOI] [PubMed] [Google Scholar]
- 24.Hiroi, T., M. Yanagita, N. Ohta, G. Sakaue, and H. Kiyono. 2000. IL-15 and IL-15 receptor selectively regulate differentiation of common mucosal immune system-independent B-1 cells for IgA responses. J. Immunol. 165:4329-4337. [DOI] [PubMed] [Google Scholar]
- 25.Hooper, J. W., E. Thompson, C. Wilhelmsen, M. Zimmerman, M. A. Ichou, S. E. Steffen, C. S. Schmaljohn, A. L. Schmaljohn, and P. B. Jahrling. 2004. Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. J. Virol. 78:4433-4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hopkins, D. R. 1983. Princes and peasants: smallpox history. University of Chicago Press, Chicago, IL.
- 27.Kempe, C. H., C. Bowles, and T. Meiklejohn. 1961. The use of vaccinia hyperimmune gamma-globulin in the prophylaxis of smallpox. Bull. W. H. O. 25:41-48. [PMC free article] [PubMed] [Google Scholar]
- 28.Kutzler, M. A., T. M. Robinson, M. A. Chattergoon, D. K. Choo, A. Y. Choo, P. Y. Choe, M. P. Ramanathan, R. Parkinson, S. Kudchodkar, Y. Tamura, M. Sidhu, V. Roopchand, J. J. Kim, G. N. Pavlakis, B. K. Felber, T. A. Waldmann, J. D. Boyer, and D. B. Weiner. 2005. Coimmunization with an optimized IL-15 plasmid results in enhanced function and longevity of CD8 T cells that are partially independent of CD4 T cell help. J. Immunol. 175:112-123. [DOI] [PubMed] [Google Scholar]
- 29.Lane, J. M., F. L. Ruben, J. M. Neff, and J. D. Millar. 1970. Complications of smallpox vaccination, 1968: results of ten statewide surveys. J. Infect. Dis. 122:303-309. [DOI] [PubMed] [Google Scholar]
- 30.Lane, J. M., F. L. Ruben, J. M. Neff, and J. D. Millar. 1969. Complications of a smallpox vaccination, 1968. N. Engl. J. Med. 281:1201-1208. [DOI] [PubMed] [Google Scholar]
- 31.Mayr, A., V. Hochstein-Mintzel, and H. Stickl. 1975. Passage history, properties, and applicability of the attenuated vaccinia virus strain MVA. Infection 3:6-14. [Google Scholar]
- 32.McCurdy, L. H., B. D. Larkin, J. E. Martin, and B. S. Graham. 2004. Modified vaccinia Ankara: potential as an alternative smallpox vaccine. Clin. Infect. Dis. 38:1749-1753. [DOI] [PubMed] [Google Scholar]
- 33.McCurdy, L. H., J. A. Rutigliano, T. R. Johnson, M. Chen, and B. S. Graham. 2004. Modified vaccinia virus Ankara immunization protects against lethal challenge with recombinant vaccinia virus expressing murine interleukin-4. J. Virol. 78:12471-12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meseda, C. A., A. D. Garcia, A. Kumar, A. E. Mayer, J. Manischewitz, L. R. King, H. Golding, M. Merchlinsky, and J. P. Weir. 2005. Enhanced immunogenicity and protective effect conferred by vaccination with combinations of modified vaccinia virus Ankara and licensed smallpox vaccine Dryvax in a mouse model. Virology 339:164-175. [DOI] [PubMed] [Google Scholar]
- 35.Mortimer, P. P. 2003. The new cell culture smallpox vaccine should not be offered to the general population. Rev. Med. Virol. 13:17-20. [DOI] [PubMed] [Google Scholar]
- 36.Oh, S., J. A. Berzofsky, D. S. Burke, T. A. Waldmann, and L. P. Perera. 2003. Coadministration of HIV vaccine vectors with vaccinia viruses expressing IL-15 but not IL-2 induces long-lasting cellular immunity. Proc. Natl. Acad. Sci. USA 100:3392-3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oh, S., L. P. Perera, D. S. Burke, T. A. Waldmann, and J. A. Berzofsky. 2004. IL-15/IL-15Ralpha-mediated avidity maturation of memory CD8+ T cells. Proc. Natl. Acad. Sci. USA 101:15154-15159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Otero, M., S. A. Calarota, A. Dai, A. S. De Groot, J. D. Boyer, and D. B. Weiner. 2006. Efficacy of novel plasmid DNA encoding vaccinia antigens in improving current smallpox vaccination strategy. Vaccine 24:4461-4470. [DOI] [PubMed] [Google Scholar]
- 39.Perera, L. P., C. K. Goldman, and T. A. Waldmann. 2001. Comparative assessment of virulence of recombinant vaccinia viruses expressing IL-2 and IL-15 in immunodeficient mice. Proc. Natl. Acad. Sci. USA 98:5146-5151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rao, A. R. 1972. Smallpox. Kothari Book Depot, Bombay, India.
- 41.Redfield, R. R., D. C. Wright, W. D. James, T. S. Jones, C. Brown, and D. S. Burke. 1987. Disseminated vaccinia in a military recruit with human immunodeficiency virus (HIV) disease. N. Engl. J. Med. 316:673-676. [DOI] [PubMed] [Google Scholar]
- 42.Stickl, H., V. Hochstein-Mintzel, A. Mayr, H. C. Huber, H. Schäfer, and A. Holzner. 1974. MVA vaccination against smallpox: clinical tests with an attenuated live vaccinia virus strain (MVA). Dtsch. Med. Wochenschr. 99:2386-2392. (In German.) [DOI] [PubMed] [Google Scholar]
- 43.Stittelaar, K. J., G. van Amerongen, I. Kondova, T. Kuiken, R. F. van Lavieren, F. H. Pistoor, H. G. Niesters, G. van Doornum, B. A. van der Zeijst, L. Mateo, P. J. Chaplin, and A. D. Osterhaus. 2005. Modified vaccinia virus Ankara protects macaques against respiratory challenge with monkeypox virus. J. Virol. 79:7845-7851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waldmann, T. A. 2006. The biology of interleukin-2 and interleukin-15: implications for cancer therapy and vaccine design. Nat. Rev. Immunol. 6:595-601. [DOI] [PubMed] [Google Scholar]
- 45.Williamson, J. D., R. W. Reith, L. J. Jeffrey, J. R. Arrand, and M. Mackett. 1990. Biological characterization of recombinant vaccinia viruses in mice infected by the respiratory route. J. Gen. Virol. 71:2761-2767. [DOI] [PubMed] [Google Scholar]
- 46.Wyatt, L. S., P. L. Earl, L. A. Eller, and B. Moss. 2004. Highly attenuated smallpox vaccine protects mice with and without immune deficiencies against pathogenic vaccinia virus challenge. Proc. Natl. Acad. Sci. USA 101:4590-4595. [DOI] [PMC free article] [PubMed] [Google Scholar]