Abstract
We report that adaptation to infect the guinea pig did not modify the capacity of foot-and-mouth disease virus (FMDV) to kill suckling mice and to cause an acute and transmissible disease in the pig, an important natural host for this pathogen. Adaptive amino acid replacements (I248→T in 2C, Q44→R in 3A, and L147→P in VP1), selected upon serial passages of a type C FMDV isolated from swine (biological clone C-S8c1) in the guinea pig, were maintained after virus multiplication in swine and suckling mice. However, the adaptive replacement L147→P, next to the integrin-binding RGD motif at the GH loop in VP1, abolished growth of the virus in different established cell lines and modified its antigenicity. In contrast, primary bovine thyroid cell cultures could be productively infected by viruses with replacement L147→P, and this infection was inhibited by antibodies to αvβ6 and by an FMDV-derived RGD-containing peptide, suggesting that integrin αvβ6 may be used as a receptor for these mutants in the animal (porcine, guinea pig, and suckling mice) host. Substitution T248→N in 2C was not detectable in C-S8c1 but was present in a low proportion of the guinea pig-adapted virus. This substitution became rapidly dominant in the viral population after the reintroduction of the guinea pig-adapted virus into pigs. These observations illustrate how the appearance of minority variant viruses in an unnatural host can result in the dominance of these viruses on reinfection of the original host species.
The high potential for adaptation and rapid evolution that derives from the quasispecies dynamics of RNA virus populations (30, 40) can be reflected in the alteration of cell tropism, host range, and virulence (8, 9, 30, 43, 51). Mutant viruses with a modified host range can contribute to the emergence of new animal and human diseases (62). On the other hand, adaptation to a new host has been exploited since the beginning of vaccinology to derive attenuated strains with decreased pathogenicity for the original, natural host (18).
Foot-and-mouth disease virus (FMDV) belongs to the Picornaviridae family and is the etiological agent of the most important animal disease affecting domestic cloven-hoofed animals and a large variety of wild artiodactyls (for reviews, see references 2, 6, 21, 63, 68, and 74). The virus consists of a nonenveloped particle of icosahedral symmetry containing a positive-sense single-stranded RNA genome of about 8.5 kb. A single open reading frame encodes all of the capsid, as well as a total of nine additional mature, nonstructural (NS) proteins, including two proteases (L and 3C) and an RNA-dependent RNA polymerase (3D) (14, 69, 73). As shown for a number of different picornaviruses, the mature NS proteins, as well as some of their protein precursors, are involved in multiple functions needed for virus multiplication and the host cell membrane rearrangements associated with viral RNA replication (3, 25, 35, 46, 55, 60, 65, 82).
FMDV can initiate the infection of cultured cells via different αv integrins (αvβ1,αvβ3, αvβ6, and αvβ8) (15, 31, 41, 44, 45), and viruses that are infectious in vivo have been reported to use integrins αvβ3 and αvβ6 as receptors (45, 58). This latter integrin is expressed constitutively on the epithelial cells targeted by FMDV in cattle and is most likely the major in vivo receptor for this virus (56). Interaction of FMDV with integrins requires an Arg-Gly-Asp (RGD) triplet located at the GH loop of capsid protein VP1 (1). The RGD is also part of a main antigenic site involved in the interaction with neutralizing antibodies (39, 52, 78). The RGD is highly conserved among field FMDV isolates (23), probably reflecting its requirement for the in vivo interaction with integrin receptors (31, 58, 66). However, upon multiple passages in cell culture, FMDV can acquire the capacity to bind heparan sulfate (HS) (42), as a result of a small number of amino acid substitutions that increase the positive charges at the capsid surface (11, 34, 70). Such viruses can use HS as alternative receptors for cell entry and thus can dispense with their RGD motif and remain infectious for cultured cells (70). Alternative nonintegrin, non-HS cell-binding sites in pigs have also been reported for engineered viruses harboring KGE instead of RGD (83), as well as for viruses highly passaged in cell culture that lack the RGD (8, 10).
In addition to the RGD, other residues of the VP1 GH loop are conserved across the FMDV serotypes. Leu (rarely Ile) is conserved as the amino acid located four residues downstream of the RGD (RGD+4), and Leu is most commonly found at the RGD+1 position; however, Arg or Met can occupy this location in some serotypes. Studies using FMDV-derived peptides as competitors of integrin-mediated virus binding and infection have identified the conserved Leu residues at the RGD+1 and RGD+4 sites as key for high-affinity binding to integrins αvβ6 and αvβ8 but not for αvβ3 (20, 54). Crystallographic analysis of chemically reduced virus (50, 67) and of a FMDV peptide in complex with the Fab fragment of two different neutralizing antibodies (39, 78, 79) showed that the VP1 GH loop adopts predominantly one conformation consisting of a short region of β-strand followed by the RGD tripeptide in an open conformation, prior to a 310-helix. In the helix, which differs in hydrogen bonding from an α helix, the RGD+1 and RGD+4 leucines are spatially adjacent on the outer face and favorably positioned for integrin binding (20, 28).
Recent results have suggested that modifications in receptor specificity may occur during FMDV replication in the bovine host. Viruses with SGD instead of RGD were recovered upon propagation of the A24 reference strain in cattle (66). Likewise, amino acid replacements affecting either the RGD motif (R141→G) or adjacent positions (L144→P and L147→P), reported to be important for FMDV binding to some RGD-dependent integrins (20, 54, 64), were present in FMDV type C mutants selected in cattle immunized with VP1 GH loop-containing synthetic peptides (75). These mutants rapidly reverted to a parental RGD context when grown in cultured cells, and this reversion was delayed by the addition of sera from immunized cattle, suggesting a co-evolution of antigenicity and receptor usage in partially protected cattle (76).
Limited information is available on other determinants of FMDV host range and virulence in vivo, but some evidence points to 3A and 3AB as relevant for virus-host interactions (12, 51). In FMDV these NS proteins are unique among picornaviruses since 3A extends its carboxy terminus by at least 60 amino acid residues and three nonidentical copies of 3B are expressed. Each of these copies can be uridylylated in vitro by 3D polymerase (57), the initial, essential step for replication of picornavirus RNA (3, 33). Deletions in 3A have been associated with attenuation in cattle (37) and with the high virulence for swine of a type O FMDV isolated in Taiwan (13). Furthermore, deletions of redundant copies of 3B lead to a decrease in replication efficiency in cell culture (32) and to attenuation in pigs (61).
Natural FMDV isolates can be experimentally adapted to the guinea pig by serial injection in the footpad (4, 17, 24, 47). We previously characterized amino acid substitutions I248→T in 2C, and Q44→R in 3A, which became rapidly imposed during adaptation of a swine type C FMDV (C-S8c1) to the guinea pig. Replacement Q44→R in 3A, either alone or in combination with I248→T in 2C, was sufficient to confer FMDV with the ability to produce lesions in the guinea pig (59). Later in the adaptation process, an additional mutation, L147→P, was selected in the GH loop of capsid protein VP1.
A critical issue, relevant to viral disease emergence and reemergence, is whether adaptation to an unnatural host may entail loss of virulence for the original natural host, an event typical of the process involved in the preparation of classical attenuated vaccines. We show here that adaptation to a new host did not modify the capacity of FMDV to cause an acute and transmissible disease in the pig and to kill suckling mice, a standard animal model used to determine FMDV virulence. The three adaptive mutations I248→T in 2C, Q44→R in 3A, and L147→P in VP1, selected in the guinea pig, were maintained after virus multiplication in swine and mice. However, replacement L147→P in VP1 abolished growth of the virus in established cell lines and modified its antigenicity. In contrast, FMDV with L147→P infected primary cultures of bovine thyroid cells, and this infection was inhibited by antibodies to αvβ6, suggesting that this integrin could serve as a receptor for these mutants in the three animal hosts tested. The dominance of a new amino acid replacement T248→N in 2C (which was already present in a low proportion in the virus adapted to the guinea pig) upon replication of the guinea pig-adapted virus in pigs, illustrates how the appearance of minority variant viruses in an unnatural host can result in the dominance of these viruses on reinfection of the original host species.
MATERIALS AND METHODS
Viruses.
The type C FMDV C-S8c1 is a biological clone derived from a pig field isolate (C-S8) by two passages in BHK-21 cells, a plaque purification and the amplification of the recovered virus to about 109 PFU (72). The origin, and the consensus amino acid sequence at the residues relevant for this study, of the virus populations isolated during adaptation of C-S8c1 virus to guinea pig, of the recombinant FMDV VpC-2C/3A (59), and of viruses recovered upon growth of the guinea pig-adapted virus V2.10b in primary bovine thyroid (pBTY) cells are summarized in Table 1.
TABLE 1.
FMDVs analyzed in this study
| Virus | Origin | Amino acid residuea
|
||
|---|---|---|---|---|
| VP1 (147) | 2C (248) | 3A (44) | ||
| C-S8c1 | Biological clone from C-S8 in BHK-21 cellsb | L | I | Q |
| V2.3 | Third passage in guinea pig | L | T | R |
| V2.7b | Seventh passage in guinea pig | P | T | R |
| V2.10b | Tenth passage in guinea pig | P | T | R |
| V2.11a | Eleventh passage in guinea pigc | P | T | R |
| V2.11b | Eleventh passage in guinea pigc | P | T/Nd | R |
| V2.10BTYa | Biological clone from V2.10 in pBTY cellse | P | T | R |
| V2.10BTYb | Biological clone from V2.10 in pBTY cellse | P | T | R |
| VpC-2C/3A | BHK-21 cells transfected with pC-C/3Af | L | T | R |
Consensus sequence at the amino acid residues (indicated in parentheses) of viral proteins involved in adaptation of C-S8c1 to the guinea pig (59; the present study).
The type C FMDV C-S8 was isolated from an infected pig, and a plaque-purified virus derived from this viral population was amplified to obtain C-S8c1 virus, as detailed in Materials and Methods. The resulting virus was used for guinea pig inoculation and the subsequent serial animal-to-animal inoculations of vesicle homogenates (V.2 viruses).
Pool of lesions from four guinea pigs.
A minor percentage (ca. 10%) of N was observed in the consensus sequence.
V2.10b was used to inoculate pBTY cells, and the virus recovered was subjected to two rounds of plaque purification on these cells. Viruses from two independent plaques were amplified by an additional passage on pBTY cells and were designated V2.10b.BTYa and V2.10b.BTYb.
Recombinant VpC-2C/3A was rescued from cells transfected with plasmid pC-2C/3A (59).
Animals and inoculations.
Male guinea pigs (Dunky Hartley), weighing 250 to 350 g, were inoculated by intradermal injection in the metatarsal pad of the left hind foot with 100 μl of a viral suspension (V2.10b) that was obtained after low-speed centrifugation from about 100 μl of vesicular fluid and tissue homogenized in 400 μl of phosphate-buffered saline (59). Animals were euthanized at day 4 postinfection, and vesicular fluid and epithelia around the vesicles were collected, homogenized, and used for further inoculations. Groups of about 7-day-old Swiss mice were inoculated intraperitoneally with 100 μl of virus V2.10b. Dead animals were scored up to 9 days after inoculation, and survivors were euthanized. Control animals were mock inoculated with phosphate-buffered saline, following the same procedure. Domestic pigs (Large White x Landrace), 3 months of age, weighing 30 to 40 kg and free of antibodies to FMDV were intradermally inoculated with a guinea pig-adapted FMDV (∼104 mouse 50% lethal dose [LD50]) in the heel bulbs of the right forefoot (22). After inoculation, rectal temperatures and clinical signs were monitored daily for 10 days. Animals were treated according to the recommendations of EU directive 86/609 regarding the protection of animals used for experimental and/or scientific purposes.
Cell lines, infectivity assays, and virus titration.
To detect infectious FMDV from animal lesions, the following established cell lines were used: BHK-21 from hamsters; IBRS-2 and MVPK from pigs; LK from sheep; and colon epithelial cells (CCL-242), fetal fibroblasts (CRL-1405), and lung fibroblasts (CCL-158) from guinea pigs. Cells were grown using the culture media indicated by the American Type Culture Collection. Primary bovine thyroid (pBTY) cells were cultivated as described previously (20). Detection of infectivity was considered negative when no signs of cytopathic effect and no PFU were detected after three successive blind passages, using frozen-thawed cell monolayers as inocula. Mock-infected cells were maintained in parallel to control for possible viral contamination. In no case were any signs of viral contamination observed. Plaque assays and virus titration in suckling mice were performed as described previously (7, 29).
Receptor studies.
Competition studies were carried out by using an enzyme-linked immunospot (ELISPOT) assay as described previously (16). Briefly, triplicate cell monolayers in a 96-well plate were treated with either Dulbecco modified Eagle medium, monoclonal antibodies (MAbs), or peptides at room temperature for 0.5 h prior to the addition of virus (multiplicity of infection of ≤1 PFU/cell) for a further 1 h at 37°C. At this time point the cells were washed to remove the virus inocula and competing reagents, and infection continued for 4 h. The cells were then fixed with paraformaldehyde, permeabilized with 0.1% Triton, and incubated with MAb 2C2 (which recognizes the FMDV 3A protein) for 1 h at room temperature, followed by the addition of a biotinylated, goat anti-mouse immunoglobulin G secondary antibody (Southern Biotechnologies) and streptavidin-conjugated alkaline phosphatase (Caltag Laboratories) for 1 h each at room temperature. The alkaline phosphatase substrate (Bio-Rad) was added according to the manufacturer's instructions for 10 min. The cells were then washed with distilled water and allowed to air dry. The infected cells were colored dark-blue and counted by using an ELISPOT Plate reader (Zeiss). Nonspecific labeling was determined by performing the assay on uninfected cells. In experiments with MAbs as competitors, the competing antibody could not be detected by the secondary antibody, i.e., cells were incubated with the competing antibody alone, and the assay was developed as described above.
Extraction and amplification of viral RNA and nucleotide sequencing.
Total RNA from homogenates of vesicular lesions was extracted by using guanidine thiocyanate (26). Briefly, viral RNA directly extracted from lesions was copied into cDNA and PCR amplified into 11 fragments spanning the whole FMDV genome, as described previously (59). PCR-amplified DNAs were purified by using the Wizard PCR Preps DNA purification system (Promega), and their consensus nucleotide sequences were determined either in an automated sequencer (ABI 373) or manually by using the fmol sequencing kit (Promega). The primers used for nucleotide sequencing have been previously described (11, 77). All genomic regions were sequenced at least twice using primers of opposite polarity (11, 77). Genomic positions are numbered from the 5′-end terminal residue, as reported earlier (77). Viral RNA was prepared from cells infected with V2.10b.BTYa and V2.10b.BTYb by using an RNeasy minikit (QIAGEN) and used as a template for an reverse transcription-PCR (RT-PCR) using the One-Step RT-PCR kit (QIAGEN) and the primers C-RGD-for (nt3515-5′-ATCCCACTGCCTACCACAAG-3′) and C-RGD-rev (nt3765-5′-TTGGCTGAATCGGAAGAATC-3′).
Peptides and antibodies.
The RGD peptide with its sequence-derived form the GH loop of VP1 of type O FMDV (VPNLRGDLQVLAQKVAR) and the substituted versions RGEL (VPNLRGELQVLAQKVAR) and RGDLQVP (VPNLRGDLQVPAQKVAR) were synthesized in the peptide synthesis facility at the Institute for Animal Health, Compton, United Kingdom. The MAbs used in the present study were B3A anti-β3, LM609 anti-αvβ3, and 10D5 anti-αvβ6 (all from Chemicon); 37E1 anti-αvβ8 (41) and 6.8G6 anti-αvβ6 (81); and MAb 4C4 to the VP1 GH loop and MAb 6C3 to VP3 (both from C-S8c1) (53). MAb 2C2 (27), which recognizes the FMDV 3A protein (19), was obtained from Emiliana Brocchi (Istituto Zooprofilattico Sperimentale della Lombardia e dell'Emilia Romagna, Brescia, Italy). All of the integrin-specific antibodies used in the present study were shown to be cross-reactive for the appropriate bovine integrin by flow cytometry (data not shown).
Flow cytometry.
Integrin expression in primary BTY cells was analyzed by flow cytometry, as previously described (20).
Western blot assay.
FMDV C-S8c1 particles were concentrated by sedimentation through a sucrose cushion, and viral proteins were quantified by densitometry of the Coomassie blue-stained protein bands separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis in the presence of 8 M urea (53). About 10 pmol (VP1 equivalents) of FMDV C-S8c1 particles or 5 μl of vesicle homogenate were resolved by sodium dodecyl sulfate-urea-polyacrylamide gel electrophoresis and transferred to a nitrocellulose membrane by using the Mini-Protean II and Mini-Trans Blot transfer systems (Bio-Rad). Nonspecific binding of protein to the membrane was blocked by treatment with 2% bovine serum albumin before incubation of the blots with specific MAbs. The membranes were washed, exposed to appropriate secondary antibodies conjugated to horseradish peroxidase, and developed by using an ECL Western blotting detection system (Amersham) according to the manufacturer's instructions.
RESULTS
Guinea pig-adapted FMDV can infect and kill suckling mice.
To analyze the infectivity of the guinea pig-adapted viruses for other animal species, viruses V2.10b (harboring substitutions L147→P in VP1, I248→T in 2C, and Q44→R in 3A, selected during adaptation to the guinea pig) or VpC-2C/3A (carrying replacements I248→T in 2C and Q44→R in 3A) were inoculated in suckling mice. All of the inoculated animals died between days 2 and 7 postinoculation, showing a time course and clinical signs (tremors, ataxia, and paralysis of the hind limbs) similar to those exhibited by mice inoculated with C-S8c1 (Table 2). Homogenates from two of the animals that died after inoculation with V2-10b or VpC-2C/3A caused death when inoculated in new suckling mice. The sequence of the FMDV RNA amplified from these dead animals showed that viruses maintained the adaptive mutations corresponding to the V2-10b or VpC-2C/3A. These results indicate that the replacements selected upon adaptation of C-S8c1 to the guinea pig, including L147→P in VP1, did not alter the capacity of the virus to cause lethal infection of suckling mice.
TABLE 2.
Infectivity in suckling mice of guinea pig-adapted viruses
| FMDV | Inoculuma | Mortalityb (%) |
|---|---|---|
| V2.10b | Vesicle homogenate | 100 (12/12) |
| VpC-2C/3A | 104 PFU | 100 (8/8) |
| C-S8c1 | 104 PFU | 100 (10/10) |
| Control | PBS | 0 (0/3) |
Animals were injected with 100 μl of viral suspension or PBS (control). For V2.10b, a twofold dilution of a vesicle homogenate (59) was used.
The numbers of dead/inoculated mice are indicated in parentheses. The procedures are detailed in Materials and Methods.
Guinea pig-adapted FMDV produces typical clinical signs of disease in pigs and can be transmitted by contact.
To assess the infectivity of the guinea pig-adapted viruses in the pig (the natural host from which C-S8c1 was originally isolated [72]), domestic pigs were inoculated with viruses recovered at a late adaptation passage in guinea pig. To obtain a sufficient amount of virus for these experiments, virus V2.10b was amplified by the independent inoculation of two groups of guinea pigs. Epithelia and vesicular fluid from lesions developed by the animals from each of these groups were collected and were termed V2.11a and V2.11b, respectively. The stability of the adaptive replacements in 2C, 3A, and VP1 was confirmed by determining the consensus nucleotide sequences of viruses V2.11a and V2.11b.
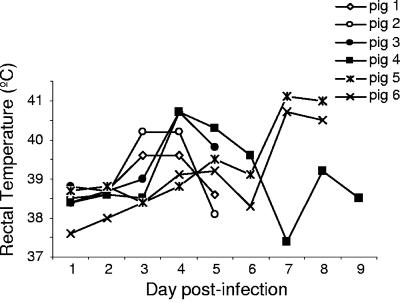
In a first experiment, two domestic pigs (animals 1 and 2) were inoculated with 100 μl of a twofold dilution of viral population V2.11a corresponding to about 104 mouse LD50. Both animals showed typical clinical signs of disease that included development of vesicles and fever (rectal temperature of >39°C) from day 3 postinfection (Table 3 and Fig. 1).
TABLE 3.
Lesions developed by pigs inoculated with guinea pig-adapted virus
| FMDVa | Animal | Lesion location(s) at day postinfectionb:
|
||||
|---|---|---|---|---|---|---|
| 3 | 4 | 5 | 6 | 7 | ||
| V2.11a | 1 | RF, LH, RH, LF, S | RF, LH, RH, LF, S | RF, LH, RH, LF, S† | ||
| 2 | RF, LH, RH, LF, S | RF, LH, RH, LF, S | RF, LH, RH, LF, S† | |||
| V2.11b | 3 | RF | RF, LH, RH, LF, S | RF, LH, RH, LF, S† | ||
| 4 | RF | RF, LH, RH, LF, S | RF, LH, RH, LF, S | RF, LH, RH, LF, S† | ||
| 5c | RF, LH, RH, LF, S | |||||
| 6c | RF, LH, RH, LF, S | |||||
Virus used for pig inoculation in the right fore foot, as described in Materials and Methods.
The location of the lesions observed at different days postinfection are indicated as follows: LH, left hind foot; RH, right hind foot; LF, left forefoot; RF, right forefoot; S, snout. †, Animal slaughtered at the day indicated.
Contact animals. The blank spaces for animals 5 and 6 indicate that no lesions were observed.
FIG. 1.
Rectal temperatures in pigs infected with guinea pig-adapted viruses. Animal numbering as in Table 2.
A second experiment was conducted to confirm the results of pig infections and to evaluate the capacity of the guinea pig-adapted virus to be transmitted by contact. To this aim, two pigs (animals 3 and 4) were inoculated with about 104 mouse LD50 of V2.11b. Two additional pigs (animals 5 and 6) were kept in contact with the inoculated animals within the same box. As in the previous experiment, animals 3 and 4 developed classical clinical signs of disease, including vesicles and fever (Table 3 and Fig. 1). Contact pigs 5 and 6 developed similar clinical signs that appeared from day 7 postinfection, confirming the capacity of V2.11b to infect pigs and to be transmitted by contact.
Replacement T248→N in 2C was selected upon replication of the guinea pig-adapted virus V2.11b in pigs.
Nucleotide sequencing of FMDV RNA regions spanning VP1, 2C, and 3A sequences from vesicles developed by animals 1 and 2 confirmed the stability of the three adaptive mutations present in viral population V2.11a (Table 4). Likewise, all of the sequences from the vesicles of animals inoculated with V.2.11b, including those from contact animals 5 and 6, maintained the adaptive mutations P147 in VP1 and R44 in 3A. However, in animals 3, 4, 5, and 6 position 248 of 2C had undergone substitution T248→N (Table 4). A detailed examination of the 2C nucleotide sequence from V.2.11b population revealed that besides a major nucleotide band corresponding to nucleotide C (ACC triplet) at position 5087 (leading to T248), a minor band of ca. 10% that corresponded to nucleotide A leading to N248 was also observed. This sequence heterogeneity was not found in virus stock V2.11a. Thus, replacement T248→N, which was already detectable in the V.2.11b population, became rapidly dominant in the viral populations recovered from infected pigs.
TABLE 4.
Stability of adaptive mutations in viruses recovered from pigs inoculated with guinea pig-adapted viruses
| FMDV | Animal and lesiona | Amino acid residueb
|
||
|---|---|---|---|---|
| VP1 (147) | 2C (248) | 3A (44) | ||
| V2.11a | 1S | P | T | R |
| 2S | P | T | R | |
| V2.11b | 3RH | P | N | R |
| 3LH | P | N | R | |
| 3S | P | N | R | |
| 4LH | P | N | R | |
| 4S | P | N | R | |
| 4S | P | N | R | |
| 5S | P | N | R | |
| 6LFc | P | N | R | |
Lesions used for viral RNA sequencing are designated by the animal number and lesion location, indicated as follows: LH, left hind foot; RH, right hind foot; LF, left forefoot; RF, right forefoot; S, snout. Two independent lesions developed in the snout by animal 4 were included in this analysis.
The amino acids found at positions 147 of VP1, 248 of 2C, and 44 of 3A are indicated.
The complete genomic RNA sequence of the viral population present in this lesion was determined as described in Materials and Methods.
These results suggest that replacement T248→ N confers a selective advantage for the multiplication and spread of the virus in the pig. No additional nucleotide substitutions were found in the complete genomic RNA sequence determined from a vesicle developed by contact animal 6 (Table 4).
Guinea pig-adapted viruses harboring replacement L147→P in VP1 do not infect several established cell lines.
Viruses adapted to the guinea pig fail to produce a cytopathic effect in a number of established cell lines, including BHK-21 and IBRS-2 cells that are usually used for FMDV amplification (59). Here, we have extended this analysis to include additional FMDV-susceptible cell lines, such as MVPK cells, LK cells, and three guinea pig-derived cell lines. No viral amplification and/or cytopathic effect was observed in any of the seven cell lines tested upon infection with the guinea pig-derived viruses V2.7b and V2.10b, which harbored the three mutations selected during the adaptation process, including substitution L147→P in VP1. In contrast, the cell lines studied were productively infected with C-S8c1, as well as with the guinea pig-adapted virus V2.3, recovered in an early adaptation passage, which included mutations I248→T in 2C and Q44→R in 3A but not L147→P in VP1 (Table 5). The amplification and sequencing of the corresponding RNA regions from the supernatant of cells infected with virus V2.3 confirmed the maintenance of the adaptive mutations in 2C and 3A.
TABLE 5.
Susceptibility of established cell lines to the infection of guinea pig-adapted viruses
| Cell line | FMDVs and cytopathologya
|
||
|---|---|---|---|
| C-S8c1 | V2.3:2C(I248→T);3A(Q44→R) | V2.7b, V2.10b:VP1(L147→P); 2C(I248→T); 3A(Q44→R) | |
| BHK-21 (hamster) | + | +b | - |
| CCL-242 (guinea pig) | ND | + | - |
| CRL-1445 (guinea pig) | ND | + | - |
| CCL 158 (guinea pig) | ND | + | - |
| IBRS-2 (pig) | + | +b | -c |
| MVPK (pig) | + | + | - |
| LK (sheep) | + | + | - |
The FMDVs shown were used for cell inoculation. The adaptive replacements in V2.3, V2.7b, and V2.10b are indicated. +, Cytopathology observed 24 and 48 h postinfection; −, no cytopathology observed after three successive blind passages (see Materials and Methods for details). ND, not done.
In three independent experiments, the presence of the adaptive mutations harbored by the infective viruses was confirmed by direct viral RNA sequencing from culture medium.
A cytopathic effect was observed in one of three inoculations of this cell line. In this case, RNA sequencing from culture medium revealed selection of a direct revertant in position 147 of VP1(P→L).
Likewise, attempts to recover infectious virus from vesicles developed by pigs inoculated with V2.11a and V2.11b resulted in the selection of direct revertants to L147 in VP1 (Table 6). These results suggest that the replacement L147→P in VP1 impairs viral recognition of the integrins functionally expressed in the established cell lines analyzed and pose the interesting question of which receptors are being used to initiate infection in the animal hosts.
TABLE 6.
Viral isolation in cultured cells of viruses from lesions developed by pigs infected with guinea pig-adapted viruses
| FMDV | Lesiona | Viral isolationb
|
|
|---|---|---|---|
| BHK-21 | IBRS-2 | ||
| V2.11a | 1S | - | - |
| 2S | - | - | |
| 2LH | - | - | |
| 3LF | - | +* | |
| 4S | - | - | |
| 4RH | - | - | |
| V2.11b | 5S | - | +* |
| 5RH | +* | +* | |
| 5LH | +* | +* | |
| 6LF | - | - | |
| 6RH | +* | +* | |
| 6S | +* | +* | |
Lesions whose material was used for viral RNA sequencing are indicated by the animal number and lesion location, as in Table 3.
The results correspond to three independent inoculations of cell monolayers with 100 μl of a 1:4 dilution of lesion homogenate. *, A cytopathic effect was observed only in one of the three inoculations. Sequencing analysis showed the presence of a direct reversion (P147→L) in the virus recovered. The “+” and “−” refer to the extent of cytopathology, as described in Table 5.
Viruses harboring replacement L147→P in VP1 can infect primary cultured cells by utilizing integrin αvβ6.
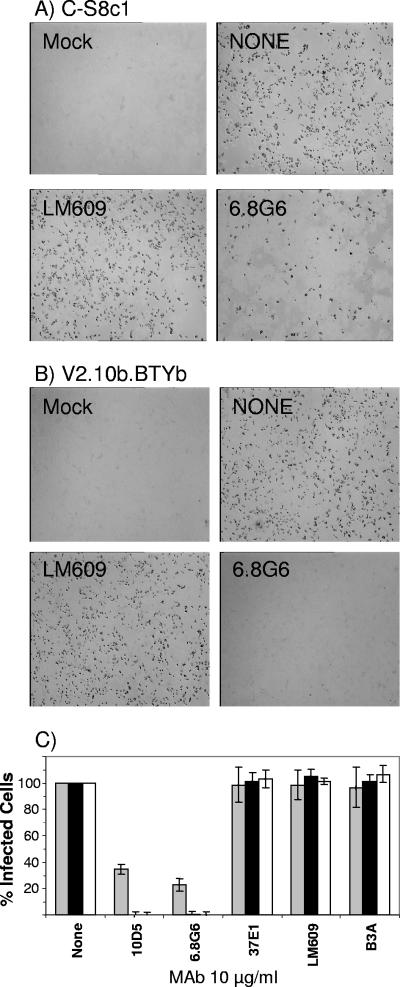
In contrast to established cell lines, primary BTY cells were found to be permissive to guinea pig-derived viruses and cytopathic manifestations were observed at about 18 h postinfection. To further characterize guinea pig-derived FMDV interaction with pBTY cells, two independent virus stocks were generated from guinea pig lesion (V2.10b) material by plaque purification on pBTY cells (see Materials and Methods). These viruses were amplified by one additional passage through pBTY cells and designated V2.10b.BTYa and V2.10b.BTYb. DNA sequencing of RT-PCR products (prepared from infected cell lysates) established that both viruses retained P147 at the RGD+4 site. The failure of these viruses to infect some established cell lines (see above) was confirmed using IBRS-2 and MDBK cells. The receptor(s) used to initiate infection of pBTY cells by V2.10b.BTYa and V2.10b.BTYb was investigated by using function-blocking anti-integrin MAbs. Primary pBTY cells are routinely used at the FMDV World Reference Laboratory at Pirbright, United Kingdom, for virus isolation including from infected tissues collected from swine. Primary pBTY cells consistently express a high level of αvβ6 (20). The expression of αvβ6 on the surfaces of each batch of pBTY cells used in the present study was confirmed by flow cytometry (data not shown) as described previously (20). For these experiments, FMDV C-S8c1 was used as a positive control since this virus has been shown to use αvβ6 as a receptor (45). Primary BTY cells were treated with blocking MAbs to αvβ3, αvβ6, αvβ8, or the β3 subunit prior to and during the incubation with viruses (C-S8c1, V2.10b.BTYa, or V2.10b.BTYb). Infection was quantified by using an ELISPOT assay (Fig. 2), which allows the number of infected cells to be counted (see Materials and Methods and reference 16). Consistent with αvβ6 being the major RGD-binding integrin expressed on pBTY cells, infection by C-S8c1 was inhibited by the αvβ6 MAbs (10D5 and 6.8G6) but not by MAbs to αvβ8, αvβ3, or the β3 subunit (Fig. 2). Similarly, infection by the V2.10b.BTYa and V2.10b.BTYb viruses was inhibited by anti-αvβ6 MAbs but not by MAbs to the other integrins (Fig. 2). Although these studies showed that these viruses use αvβ6 as a receptor, the inhibitory effect of the anti-αvβ6 MAbs appeared to be greater for the V2.10b.BTYa and V2.10b.BTYb viruses than for C-S8c1 (Fig. 2). This observation prompted further experiments to determine the amount of the anti-αvβ6 MAbs required to block infection by C-S8c1 and V2.10b.BTYb. We found that for C-S8c1, ∼80% inhibition was achieved using MAbs 10D5 and 6.8G6 at 10 μg/ml, whereas for V2.10b.BTYb >90% inhibition was achieved at an antibody concentration of only ≤0.3 μg/ml (Fig. 3).
FIG. 2.
Inhibition of FMDV infection by anti-integrin antibodies. Triplicate monolayers of pBTY cells were pretreated with blocking anti-integrin antibodies for 0.5 h at room temperature prior to the addition of virus (multiplicity of infection of ∼1 PFU/cell) for 1 h at 37°C. The antibody remained present during the virus incubation. Excess virus and unbound antibody were removed by washing, and infection continued for a further 4 h. Infected cells (shown as black on the figure) were detected as described in Materials and Methods and counted by using an ELISPOT plate reader. (A and B) Representative well images for C-S8c1 and V2.10b.BTYb, respectively, and data for two antibodies: MAb LM609 anti-αvβ3 and MAb6.8G6 anti-αvβ6. Mock, mock-infected cells; NONE, cells infected in the absence of competing antibody. (C) Number of infected cells as the percentage of the number of infected cells in the absence of antibody (None). Bars: □, C-S8c1; ▪, V2.10b.BTYa; □, V2.10b.BTYb. The mean and standard deviation for triplicate measurements are given. A second experiment (results not shown) gave nearly identical results. MAbs: 10D5 and 6.8G6, anti-αvβ6; 37E1, anti-αvβ8; LM609, anti-αvβ3; B3A, anti-β3.
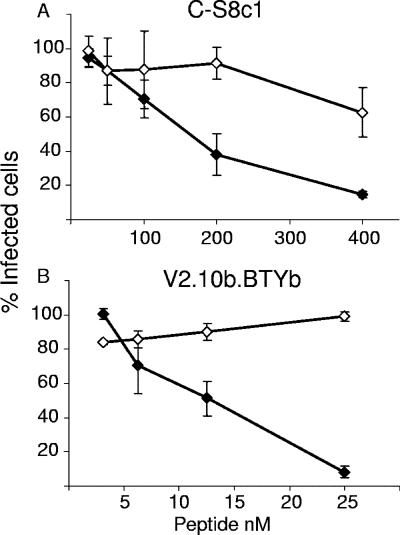
FIG. 3.
Inhibition of FMDV infection by anti-αvβ6 antibodies. Primary BTY cells were treated with anti-αvβ6 antibodies and virus, and the number of infected cells quantified as described in Fig. 2. (A) MAb 10D5; (B) MAb 6.8G6. For each antibody, the number of infected cells is shown as the percentage of the number of infected cells in the absence of competing antibody (None). Bars: □, C-S8c1; □, V2.10b.BTYb. The mean and standard deviation of triplicate measurements are given. A second experiment (results not shown) gave nearly identical results.
The results presented above suggest that the V2.10b.BTYb virus uses αvβ6 as a receptor but appears to do so less efficiently than C-S8c1. To confirm these observations, we also determined the ability of an FMDV-derived RGD-containing peptide to inhibit infection by V2.10b.BTYb and C-S8c1 (Fig. 4). This peptide has been shown to block FMDV binding to RGD-binding integrins (20). Significantly, less peptide was needed to inhibit infection by V2.10b.BTYb (50% inhibitory concentration of ∼12.5 nM) compared to C-S8c1 (50% inhibitory concentration of ∼150 nM). The RGE version of this peptide (at 400 nM) did not inhibit infection by either virus (data not shown). Similarly, a version of the FMDV peptide with a Leu-to-Pro substitution at the RGD+4 site was a poor inhibitor of infection by either virus (Fig. 4). Taken together, these studies show that the V2.10b.BTYb virus containing a Pro at the RGD+4 site is able to use αvβ6 as a receptor for infection but appears to use this integrin less efficiently than C-S8c1, which has a Leu at this site.
FIG. 4.
Inhibition of FMDV infection by RGD peptides. The number of infected cells was quantified as described in Fig. 2, with the exception that peptides were used in place of competing antibody. (A) C-S8c1; (B) V2.10b.BTYb. For each virus, the number of infected cells is shown as the percentage of the number of infected cells in the absence of peptide competition. Symbols: ⧫, wt FMDV peptide (see Materials and Methods); ⋄, peptide containing a Leu-to-Pro substitution at the RGD+4 site. The mean and standard deviation of triplicate measurements are given. A second experiment (results not shown) gave nearly identical results.
Replacement L147→P modifies VP1 antigenicity.
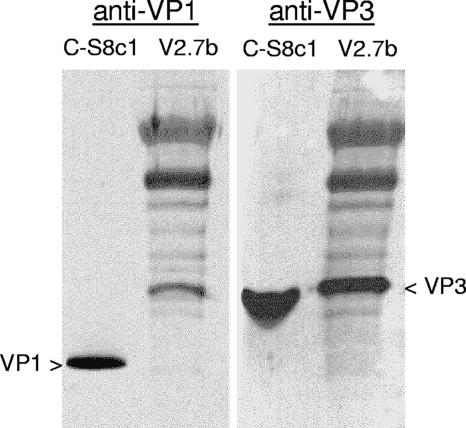
Previous evidence indicated that replacement L147→P drastically affected the recognition of the antigenic site A in VP1 by MAb and swine polyclonal antibodies (54, 64, 80). To test the antigenicity of guinea pig-adapted viruses, a Western blot of the total protein present in the lesion homogenate V2.7b, carrying replacement L147→P in VP1, was immunodetected using MAbs specific for FMDV isolate C-S8c1. As shown in Fig. 5, VP1 from C-S8c1, but not from V2.7b, was detected by MAb 4C4, which recognizes an important neutralizing antigenic site at the GH loop of this protein (52), whereas MAb 6C3 recognized the VP3 from both viruses. Thus, mutation L147→P in VP1 affects both the recognition of integrin receptors and the antigenic properties of the virus.
FIG. 5.
Immunodetection of FMDV C-S8c1 (L147 in VP1) and guinea pig-adapted virus V2.7b (P147 in VP1) by MAb 4C4 to the GH loop in VP1 (anti-VP1). MAb 6C3 to VP3 (anti-VP3) was used as a control.
DISCUSSION
We have shown here that after a total of 11 passages of adaptation of the clonal population FMDV C-S8c1 in the guinea pig, the virus maintained its original capacity to cause vesicular disease in swine and to be transmitted from swine to swine, i.e., it was not attenuated for the original host species.
None of the three amino acid replacements selected during the adaptation to the guinea pig significantly modified the capacity of the virus to produce clinical signs and disease in pigs and death in suckling mice. Replacement in Q44→R in 3A is the only single mutation selected during adaptation that conferred on the virus the capacity to produce vesicular lesions in guinea pigs (59). This mutation, which has also been reported for guinea pig-adapted FMDVs of other serotypes (23), was maintained upon infection of suckling mice and after infection and contact transmission in pigs, suggesting that it does not confer an important selective disadvantage in this natural porcine host. This substitution occurs in a residue close to the 3A hydrophobic domain, and replacements in the analogous region of poliovirus and rhinovirus have also been found to affect cell culture tropism (38, 49), suggesting that changes in this region in picornaviruses may affect replication and/or relevant interactions with host factors. However, the functional implications of replacement Q44→R in 3A remain to be understood. Replacement I248→T in 2C was the first mutation detected during adaptation, although this single mutation does not result in viruses that produce vesicles in the guinea pig (59). Interestingly (and strengthening the notion of a contribution of residue 248 in 2C to the adaptation of the virus to different hosts), the dynamics of mutant selection continued upon replication of the guinea pig-adapted virus in swine by the imposition of a new replacement, T248→N, which was already detectable in a low proportion in V2.11b. Although the initial replacement selected early in the adaptation process, I248→T, was caused by nucleotide transition U→C, replacement T248→N requires a C→A transversion (ACC to AAC), and the direct substitution I248→N requires a U→A transversion (AUC to AAC). In a sampling of multiple sequences of FMDV C-S8c1 passaged in cell culture, transversion C→A was far more frequent than U→A (71). Therefore, N248 may be more favorable than T248 for FMDV C-S8c1 replication both in the guinea pig and pig, but its dominance was delayed by the requirement of two mutational steps due to an unfavorable mutation type. Obviously, other effects on mutational bias could operate in vivo.
Replacement L147→P in capsid protein VP1 was selected later in the adaptation. This replacement impaired recovery of the virus in different cultured cells (59), suggesting an alteration in the recognition of the integrin receptors utilized by the mutants carrying this substitution. Our results confirm that this mutation abolished the capacity of the virus to infect several established cell lines, despite resulting in viruses fully infectious in pig and suckling mice. The RGD-binding integrins expressed by IBRS-2 cells have been determined (20), and competition studies with function-blocking anti-integrin antibodies have identified αvβ8 as the major receptor for FMDV on these cells (20). The failure of the guinea pig-adapted viruses to infect IBRS-2 cells suggests that the Pro substitution at the RGD+4 site is unfavorable for virus binding to αvβ8 and that this integrin is unlikely to be used by the guinea pig-adapted virus for infection in the animal (guinea pig, suckling mice, or porcine) host.
Interestingly, viruses harboring L147→P replacement productively grew in primary cultures of BTY cells. Peptide and antibody competition studies suggest that these viruses use αvβ6 as their receptor on pBTY cells but do so less efficiently than the parental C-S8c1 virus because a lower concentration of peptide/antibody was needed to inhibit infection by the guinea pig-adapted viruses. This conclusion is consistent with previous studies that showed that the RGD+4 Leu is important for ligand binding to αvβ6 (20, 48, 54). In the VP1 GH loop, the RGD+4 Leu forms part of a hydrophobic face of the 310 helix (see Introduction) that is predicted to interact with integrins (20). In the virus particle, Pro at the RGD+4 site could disrupt the helix and thereby reduce the integrin-binding affinity. This explanation most likely accounts for the poor inhibitory effect on infection of the FMDV peptide with Pro at the RGD+4 site (see Fig. 4). Nevertheless, our results suggest that αvβ6 could be the receptor used by the guinea pig-adapted viruses for infection in guinea pigs, swine, and suckling mice.
Thus, adaptation of FMDV C-S8c1 to the guinea pig seems to result from, at least, two selective steps; the first involving selection of mutations in NS proteins 2A and 3C, which could improve the capacity of the virus to replicate and produce lesions, and a second selective step involving a modification to the integrin-binding loop of the virus (the GH loop of VP1). This latter substitution (L147→P) resulted in an apparent reduction in the ability of the guinea pig-adapted virus to use bovine αvβ6 but did not compromise virus multiplication in pigs and suckling mice. Presently, we cannot be certain which integrins are used for infection in the guinea pig, but it is possible that the Leu-to-Pro substitution favors the recognition of alternative guinea pig integrins and thus a wider spread of the virus in this animal host. However, the high degree of amino acid sequence conservation between mammalian integrin chains would suggest this scenario unlikely. What is clear is that the guinea pig-adapted viruses were unable to use αvβ8 or αvβ3 to infect IBRS-2 or MDBK cells, respectively.
The outcome of clinical signs in pigs inoculated with C-S8c1 depends on the virus titer used and usually shows animal-to-animal variation (36). Assuming this, the severity of the infection produced by the guinea pig-adapted viruses was similar to that exhibited by pigs infected with C-S8c1 FMDV. This observation suggests that the guinea pig-adapted viruses maintain the cell tropism and the main pathogenic properties of the parental C-S8c1 virus. These observations, as well as the failure of the guinea pig-adapted viruses to utilize αvβ3 and αvβ8 as receptors (see above), reinforce the argument for αvβ6 as the main in vivo FMDV receptor (20).
The modification in the integrin usage introduced by replacement L147→P in VP1 associates with an antigenic change in the virus, as revealed by the lack of binding to an MAb that recognizes the antigenic site located at the GH loop (Fig. 2). A similar co-evolution of cell tropism and antigenic properties has also been found for type C3 mutants showing this replacement, which were recovered from cattle immunized with synthetic peptides (76). Thus, adaptation of FMDV to different hosts may favor viral antigenic changes.
These results document that for a typical cytopathic virus, important evolutionary events that permit changes in host range may render virus infectivity undetectable in a number of cell lines despite the virus remaining infectious for the original animal host. It must be underlined that had the adaptive mutations in the guinea pig been lethal or highly detrimental for replication in swine, we might have observed a typical case of viral attenuation through passage in an alternative host (5). If that had been the case, the chance occurrence of either multiple reversions or of compensatory mutations would have been the only means of rescuing a virus pathogenic for swine. Thus, the results reported here have direct implications for viral disease emergence in that the chance occurrence of multiple mutations during RNA genome replication, as well as their effect on the fitness on different host species, may determine either a viral emergence or re-emergence or a dead-end infection in a new host.
Acknowledgments
We thank E. Brocchi for the generous supply of MAbs and M. Sánchez for help with the animal experiments at CISA.
Work at CBMSO-CISA was supported by Spanish grants from CICYT (BIO2005-07592-C02-01 and BFU 2005-00863), MEC (Consolider, CSD2006-0007), Fundación Severo Ochoa, and the Ramón y Cajal Program (J.I.N.). T.J., A.B., S.B., and S.C. are supported by DEFRA.
Footnotes
Published ahead of print on 23 May 2007.
REFERENCES
- 1.Acharya, R., E. Fry, D. Stuart, G. Fox, D. Rowlands, and F. Brown. 1989. The three-dimensional structure of foot-and-mouth disease virus at 2.9 Å resolution. Nature 337:709-716. [DOI] [PubMed] [Google Scholar]
- 2.Alexandersen, S., Z. Zhang, A. I. Donaldson, and A. J. Garland. 2003. The pathogenesis and diagnosis of foot-and-mouth disease. J. Comp. Pathol. 129:1-36. [DOI] [PubMed] [Google Scholar]
- 3.Andino, R., N. Boddeker, D. Silvera, and A. V. Gamarnik. 1999. Intracellular determinants of picornavirus replication. Trends Microbiol. 7:76-82. [DOI] [PubMed] [Google Scholar]
- 4.Aramburu, H. G. 1949. A comparison of different methods of inoculating guinea-pigs with the virus of foot-and-mouth disease. J. Comp. Pathol. 59:42-47. [DOI] [PubMed] [Google Scholar]
- 5.Babiuk, L. A. 2002. Vaccination: a management tool in veterinary medicine. Vet. J. 164:188-201. [DOI] [PubMed] [Google Scholar]
- 6.Bachrach, H. L. 1977. Foot-and-mouth disease virus, properties, molecular biology and immunogenicity, vol. I. Virology in agriculture. Allanheld, Osmun, Montclair, NJ.
- 7.Baranowski, E., N. Molina, J. I. Nunez, F. Sobrino, and M. Saiz. 2003. Recovery of infectious foot-and-mouth disease virus from suckling mice after direct inoculation with in vitro-transcribed RNA. J. Virol. 77:11290-11295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baranowski, E., C. M. Ruiz-Jarabo, and E. Domingo. 2001. Evolution of cell recognition by viruses. Science 292:1102-1105. [DOI] [PubMed] [Google Scholar]
- 9.Baranowski, E., C. M. Ruiz-Jarabo, N. Pariente, N. Verdaguer, and E. Domingo. 2003. Evolution of cell recognition by viruses: a source of biological novelty with medical implications. Adv. Virus Res. 62:19-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baranowski, E., C. M. Ruiz-Jarabo, N. Sevilla, D. Andreu, E. Beck, and E. Domingo. 2000. Cell recognition by foot-and-mouth disease virus that lacks the RGD integrin-binding motif: flexibility in aphthovirus receptor usage. J. Virol. 74:1641-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baranowski, E., N. Sevilla, N. Verdaguer, C. M. Ruiz-Jarabo, E. Beck, and E. Domingo. 1998. Multiple virulence determinants of foot-and-mouth disease virus in cell culture. J. Virol. 72:6362-6372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baxt, B., and E. Rieder. 2004. Molecular aspects of foot-and-mouth disease virus virulence and host range: role of host cell receptors and viral factors, p. 145-172. In F. Sobrino and E. Domingo (ed.), Foot-and-mouth disease: current perspectives. Horizon Bioscience, Norfolk, United Kingdom.
- 13.Beard, C. W., and P. W. Mason. 2000. Genetic determinants of altered virulence of Taiwanese foot-and-mouth disease virus. J. Virol. 74:987-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belsham, G. J. 2005. Translation and replication of FMDV RNA. Curr. Top. Microbiol. Immunol. 288:43-70. [DOI] [PubMed] [Google Scholar]
- 15.Berinstein, A., M. Roivainen, T. Hovi, P. W. Mason, and B. Baxt. 1995. Antibodies to the vitronectin receptor (integrin αvβ3) inhibit binding and infection of foot-and-mouth disease virus to cultured cells. J. Virol. 69:2664-2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berryman, S., S. Clark, P. Monaghan, and T. Jackson. 2005. Early events in integrin alphavbeta6-mediated cell entry of foot-and-mouth disease virus. J. Virol. 79:8519-8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bittle, J. L., R. A. Houghten, H. Alexander, T. M. Shinnick, J. G. Sutcliffe, R. A. Lerner, D. J. Rowlands, and F. Brown. 1982. Protection against foot-and-mouth disease by immunization with a chemically synthesized peptide predicted from the viral nucleotide sequence. Nature 298:30-33. [DOI] [PubMed] [Google Scholar]
- 18.Bloom, B. R., and P.-H. Lambert. 2003. The vaccine book. Academic Press/Elsevier Science, San Diego, CA.
- 19.Bruderer, U., H. Swam, B. Haas, N. Visser, E. Brocchi, S. Grazioli, J. J. Esterhuysen, W. Vosloo, M. Forsyth, N. Aggarwal, S. Cox, R. Armstrong, and J. Anderson. 2004. Differentiating infection from vaccination in foot-and-mouth-disease: evaluation of an ELISA based on recombinant 3ABC. Vet. Microbiol. 101:187-197. [DOI] [PubMed] [Google Scholar]
- 20.Burman, A., S. Clark, N. G. Abrescia, E. E. Fry, D. I. Stuart, and T. Jackson. 2006. Specificity of the VP1 GH loop of foot-and-mouth disease virus for αv integrins. J. Virol. 80:9798-9810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burrows, R., J. A. Mann, A. J. Garland, A. Greig, and D. Goodridge. 1981. The pathogenesis of natural and simulated natural foot-and-mouth disease infection in cattle. J. Comp. Pathol. 91:599-609. [DOI] [PubMed] [Google Scholar]
- 22.Carrillo, C., J. Plana, R. Mascarella, J. Bergada, and F. Sobrino. 1990. Genetic and phenotypic variability during replication of foot-and-mouth disease virus in swine. Virology 179:890-892. [DOI] [PubMed] [Google Scholar]
- 23.Carrillo, C., E. R. Tulman, G. Delhon, Z. Lu, A. Carreno, A. Vagnozzi, G. F. Kutish, and D. L. Rock. 2005. Comparative genomics of foot-and-mouth disease virus. J. Virol. 79:6487-6504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cowan, K. M., and R. Trautman. 1965. Antibodies produced by guinea pigs infected with foot-and-mouth disease virus. J. Immunol. 94:858-867. [PubMed] [Google Scholar]
- 25.Choe, S. S., D. A. Dodd, and K. Kirkegaard. 2005. Inhibition of cellular protein secretion by picornaviral 3A proteins. Virology 337:18-29. [DOI] [PubMed] [Google Scholar]
- 26.Chomczynski, P., and N. Sacchi. 1987. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 162:156-159. [DOI] [PubMed] [Google Scholar]
- 27.De Diego, M., E. Brocchi, D. Mackay, and F. De Simone. 1997. The nonstructural polyprotein 3ABC of foot-and-mouth disease virus as a diagnostic antigen in ELISA to differentiate infected from vaccinated cattle. Arch. Virol. 142:2021-2033. [DOI] [PubMed] [Google Scholar]
- 28.DiCara, D., C. Rapisarda, J. L. Sutcliffe, S. M. Violette, P. H. Weinreb, I. R. Hart, M. J. Howard, and J. F. Marshall. 2007. Structure-function analysis of Arg-Gly-Asp helix motifs in αvβ6 integrin ligands. J. Biol. Chem. 282:9657-9665. [DOI] [PubMed] [Google Scholar]
- 29.Domingo, E., M. Davila, and J. Ortin. 1980. Nucleotide sequence heterogeneity of the RNA from a natural population of foot-and-mouth-disease virus. Gene 11:333-346. [DOI] [PubMed] [Google Scholar]
- 30.Domingo, E., V. Martin, C. Perales, A. Grande-Perez, J. Garcia-Arriaza, and A. Arias. 2006. Viruses as quasispecies: biological implications. Curr. Top. Microbiol. Immunol. 299:51-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duque, H., and B. Baxt. 2003. Foot-and-mouth disease virus receptors: comparison of bovine αv integrin utilization by type A and O viruses. J. Virol. 77:2500-2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Falk, M. M., F. Sobrino, and E. Beck. 1992. VPg gene amplification correlates with infective particle formation in foot-and-mouth disease virus. J. Virol. 66:2251-2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferrer-Orta, C., A. Arias, R. Agudo, R. Perez-Luque, C. Escarmis, E. Domingo, and N. Verdaguer. 2006. The structure of a protein primer-polymerase complex in the initiation of genome replication. EMBO J. 25:880-888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fry, E. E., S. M. Lea, T. Jackson, J. W. Newman, F. M. Ellard, W. E. Blakemore, R. Abu-Ghazaleh, A. Samuel, A. M. King, and D. I. Stuart. 1999. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 18:543-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garcia-Briones, M., M. F. Rosas, M. Gonzalez-Magaldi, M. A. Martin-Acebes, F. Sobrino, and R. Armas-Portela. 2006. Differential distribution of nonstructural proteins of foot-and-mouth disease virus in BHK-21 cells. Virology 349:409-421. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Briones, M. M., E. Blanco, C. Chiva, D. Andreu, V. Ley, and F. Sobrino. 2004. Immunogenicity and T-cell recognition in swine of foot-and-mouth disease virus polymerase 3D. Virology 322:264-275. [DOI] [PubMed] [Google Scholar]
- 37.Giraudo, A. T., E. Beck, K. Strebel, P. A. de Mello, J. L. La Torre, E. A. Scodeller, and I. E. Bergmann. 1990. Identification of a nucleotide deletion in parts of polypeptide 3A in two independent attenuated aphthovirus strains. Virology 177:780-783. [DOI] [PubMed] [Google Scholar]
- 38.Harris, J. R., and V. R. Racaniello. 2005. Amino acid changes in proteins 2B and 3A mediate rhinovirus type 39 growth in mouse cells. J. Virol. 79:5363-5373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hewat, E. A., N. Verdaguer, I. Fita, W. Blakemore, S. Brookes, A. King, J. Newman, E. Domingo, M. G. Mateu, and D. I. Stuart. 1997. Structure of the complex of an Fab fragment of a neutralizing antibody with foot-and-mouth disease virus: positioning of a highly mobile antigenic loop. EMBO J. 16:1492-1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holland, J., K. Spindler, F. Horodyski, E. Grabau, S. Nichol, and S. VandePol. 1982. Rapid evolution of RNA genomes. Science 215:1577-1585. [DOI] [PubMed] [Google Scholar]
- 41.Jackson, T., S. Clark, S. Berryman, A. Burman, S. Cambier, D. Mu, S. Nishimura, and A. M. King. 2004. Integrin alphavbeta8 functions as a receptor for foot-and-mouth disease virus: role of the beta-chain cytodomain in integrin-mediated infection. J. Virol. 78:4533-4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jackson, T., F. M. Ellard, R. A. Ghazaleh, S. M. Brookes, W. E. Blakemore, A. H. Corteyn, D. I. Stuart, J. W. Newman, and A. M. King. 1996. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J. Virol. 70:5282-5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jackson, T., A. M. King, D. I. Stuart, and E. Fry. 2003. Structure and receptor binding. Virus Res. 91:33-46. [DOI] [PubMed] [Google Scholar]
- 44.Jackson, T., A. P. Mould, D. Sheppard, and A. M. King. 2002. Integrin alphavbeta1 is a receptor for foot-and-mouth disease virus. J. Virol. 76:935-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jackson, T., D. Sheppard, M. Denyer, W. Blakemore, and A. M. King. 2000. The epithelial integrin alphavbeta6 is a receptor for foot-and-mouth disease virus. J. Virol. 74:4949-4956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Knox, C., K. Moffat, S. Ali, M. Ryan, and T. Wileman. 2005. Foot-and-mouth disease virus replication sites form next to the nucleus and close to the Golgi apparatus, but exclude marker proteins associated with host membrane compartments. J. Gen. Virol. 86:687-696. [DOI] [PubMed] [Google Scholar]
- 47.Knudsen, R. C., C. M. Groocock, and A. A. Andersen. 1979. Immunity to foot-and-mouth disease virus in guinea pigs: clinical and immune responses. Infect. Immun. 24:787-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kraft, S., B. Diefenbach, R. Mehta, A. Jonczyk, G. A. Luckenbach, and S. L. Goodman. 1999. Definition of an unexpected ligand recognition motif for αvβ6 integrin. J. Biol. Chem. 274:1979-1985. [DOI] [PubMed] [Google Scholar]
- 49.Lama, J., M. A. Sanz, and L. Carrasco. 1998. Genetic analysis of poliovirus protein 3A: characterization of a non-cytopathic mutant virus defective in killing Vero cells. J. Gen. Virol. 79(Pt. 8):1911-1921. [DOI] [PubMed] [Google Scholar]
- 50.Logan, D., R. Abu-Ghazaleh, W. Blakemore, S. Curry, T. Jackson, A. King, S. Lea, R. Lewis, J. Newman, N. Parry, et al. 1993. Structure of a major immunogenic site on foot-and-mouth disease virus. Nature 362:566-568. [DOI] [PubMed] [Google Scholar]
- 51.Mason, P. W., M. J. Grubman, and B. Baxt. 2003. Molecular basis of pathogenesis of FMDV. Virus Res. 91:9-32. [DOI] [PubMed] [Google Scholar]
- 52.Mateu, M. G. 1995. Antibody recognition of picornaviruses and escape from neutralization: a structural view. Virus Res. 38:1-24. [DOI] [PubMed] [Google Scholar]
- 53.Mateu, M. G., J. L. Da Silva, E. Rocha, D. L. De Brum, A. Alonso, L. Enjuanes, E. Domingo, and H. Barahona. 1988. Extensive antigenic heterogeneity of foot-and-mouth disease virus of serotype C. Virology 167:113-124. [DOI] [PubMed] [Google Scholar]
- 54.Mateu, M. G., M. L. Valero, D. Andreu, and E. Domingo. 1996. Systematic replacement of amino acid residues within an Arg-Gly-Asp-containing loop of foot-and-mouth disease virus and effect on cell recognition. J. Biol. Chem. 271:12814-12819. [DOI] [PubMed] [Google Scholar]
- 55.Moffat, K., G. Howell, C. Knox, G. J. Belsham, P. Monaghan, M. D. Ryan, and T. Wileman. 2005. Effects of foot-and-mouth disease virus nonstructural proteins on the structure and function of the early secretory pathway: 2BC but not 3A blocks endoplasmic reticulum-to-Golgi transport. J. Virol. 79:4382-4395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Monaghan, P., S. Gold, J. Simpson, Z. Zhang, P. H. Weinreb, S. M. Violette, S. Alexandersen, and T. Jackson. 2005. The αvβ6 integrin receptor for foot-and-mouth disease virus is expressed constitutively on the epithelial cells targeted in cattle. J. Gen. Virol. 86:2769-2780. [DOI] [PubMed] [Google Scholar]
- 57.Nayak, A., I. G. Goodfellow, and G. J. Belsham. 2005. Factors required for the Uridylylation of the foot-and-mouth disease virus 3B1, 3B2, and 3B3 peptides by the RNA-dependent RNA polymerase (3Dpol) in vitro. J. Virol. 79:7698-7706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Neff, S., D. Sa-Carvalho, E. Rieder, P. W. Mason, S. D. Blystone, E. J. Brown, and B. Baxt. 1998. Foot-and-mouth disease virus virulent for cattle utilizes the integrin αvβ3 as its receptor. J. Virol. 72:3587-3594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nunez, J. I., E. Baranowski, N. Molina, C. M. Ruiz-Jarabo, C. Sanchez, E. Domingo, and F. Sobrino. 2001. A single amino acid substitution in nonstructural protein 3A can mediate adaptation of foot-and-mouth disease virus to the guinea pig. J. Virol. 75:3977-3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O'Donnell, V. K., J. M. Pacheco, T. M. Henry, and P. W. Mason. 2001. Subcellular distribution of the foot-and-mouth disease virus 3A protein in cells infected with viruses encoding wild-type and bovine-attenuated forms of 3A. Virology 287:151-162. [DOI] [PubMed] [Google Scholar]
- 61.Pacheco, J. M., T. M. Henry, V. K. O'Donnell, J. B. Gregory, and P. W. Mason. 2003. Role of nonstructural proteins 3A and 3B in host range and pathogenicity of foot-and-mouth disease virus. J. Virol. 77:13017-13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Parrish, C. R., and Y. Kawaoka. 2005. The origins of new pandemic viruses: the acquisition of new host ranges by canine parvovirus and influenza A viruses. Annu. Rev. Microbiol. 59:553-586. [DOI] [PubMed] [Google Scholar]
- 63.Pereira, H. G. 1981. Foot-and-mouth disease. Academic Press, Inc., London, England.
- 64.Pfaff, E. 1997. Recognition sites of RGD-dependent integrins. R. G. Landes Co., Austin, TX.
- 65.Porter, A. G. 1993. Picornavirus nonstructural proteins: emerging roles in virus replication and inhibition of host cell functions. J. Virol. 67:6917-6921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rieder, E., T. Henry, H. Duque, and B. Baxt. 2005. Analysis of a foot-and-mouth disease virus type A24 isolate containing an SGD receptor recognition site in vitro and its pathogenesis in cattle. J. Virol. 79:12989-12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rowlands, D., D. Logan, R. Abu-Ghazaleh, W. Blakemore, S. Curry, T. Jackson, A. King, S. Lea, R. Lewis, J. Newman, et al. 1994. The structure of an immunodominant loop on foot and mouth disease virus, serotype O1, determined under reducing conditions. Arch. Virol. (Suppl. 9):51-58. [DOI] [PubMed] [Google Scholar]
- 68.Rowlands, D. J. 2003. Foot-and-mouth disease: special issue. Virus Res. 91:1-161.
- 69.Ryan, M. D., M. L. L. Donelly, M. Flint, V. M. Cowton, G. Luke, L. E. Hughes, C. Knox, and P. de Felipe. 2004. Foot-and-mouth disease proteinases, p. 53-76. In F. Sobrino and E. Domingo (ed.), Foot-and-mouth disease: current perspectives. Horizon Bioscience, Norfolk, United Kingdom.
- 70.Sa-Carvalho, D., E. Rieder, B. Baxt, R. Rodarte, A. Tanuri, and P. W. Mason. 1997. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J. Virol. 71:5115-5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sierra, M., A. Airaksinen, C. Gonzalez-Lopez, R. Agudo, A. Arias, and E. Domingo. 2007. Foot-and-mouth disease virus mutant with decreased sensitivity to ribavirin: implications for error catastrophe. J. Virol. 81:2012-2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sobrino, F., M. Davila, J. Ortin, and E. Domingo. 1983. Multiple genetic variants arise in the course of replication of foot-and-mouth disease virus in cell culture. Virology 128:310-318. [DOI] [PubMed] [Google Scholar]
- 73.Sobrino, F., M. Saiz, M. A. Jimenez-Clavero, J. I. Nunez, M. F. Rosas, E. Baranowski, and V. Ley. 2001. Foot-and-mouth disease virus: a long known virus, but a current threat. Vet. Res. 32:1-30. [DOI] [PubMed] [Google Scholar]
- 74.Sobrino, F., and E. Domingo (ed.). 2004. Foot-and-mouth disease: current perspectives. Horizon Bioscience, Norfolk, United Kingdom.
- 75.Taboga, O., C. Tami, E. Carrillo, J. I. Nunez, A. Rodriguez, J. C. Saiz, E. Blanco, M. L. Valero, X. Roig, J. A. Camarero, D. Andreu, M. G. Mateu, E. Giralt, E. Domingo, F. Sobrino, and E. L. Palma. 1997. A large-scale evaluation of peptide vaccines against foot-and-mouth disease: lack of solid protection in cattle and isolation of escape mutants. J. Virol. 71:2606-2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tami, C., O. Taboga, A. Berinstein, J. I. Nunez, E. L. Palma, E. Domingo, F. Sobrino, and E. Carrillo. 2003. Evidence of the coevolution of antigenicity and host cell tropism of foot-and-mouth disease virus in vivo. J. Virol. 77:1219-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toja, M., C. Escarmis, and E. Domingo. 1999. Genomic nucleotide sequence of a foot-and-mouth disease virus clone and its persistent derivatives: implications for the evolution of viral quasispecies during a persistent infection. Virus Res. 64:161-171. [DOI] [PubMed] [Google Scholar]
- 78.Verdaguer, N., M. G. Mateu, D. Andreu, E. Giralt, E. Domingo, and I. Fita. 1995. Structure of the major antigenic loop of foot-and-mouth disease virus complexed with a neutralizing antibody: direct involvement of the Arg-Gly-Asp motif in the interaction. EMBO J. 14:1690-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Verdaguer, N., G. Schoehn, W. F. Ochoa, I. Fita, S. Brookes, A. King, E. Domingo, M. G. Mateu, D. Stuart, and E. A. Hewat. 1999. Flexibility of the major antigenic loop of foot-and-mouth disease virus bound to a Fab fragment of a neutralizing antibody: structure and neutralization. Virology 255:260-268. [DOI] [PubMed] [Google Scholar]
- 80.Verdaguer, N., N. Sevilla, M. L. Valero, D. Stuart, E. Brocchi, D. Andreu, E. Giralt, E. Domingo, M. G. Mateu, and I. Fita. 1998. A similar pattern of interaction for different antibodies with a major antigenic site of foot-and-mouth disease virus: implications for intratypic antigenic variation. J. Virol. 72:739-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Weinreb, P. H., K. J. Simon, P. Rayhorn, W. J. Yang, D. R. Leone, B. M. Dolinski, B. R. Pearse, Y. Yokota, H. Kawakatsu, A. Atakilit, D. Sheppard, and S. M. Violette. 2004. Function-blocking integrin αvβ6 monoclonal antibodies: distinct ligand-mimetic and nonligand-mimetic classes. J. Biol. Chem. 279:17875-17887. [DOI] [PubMed] [Google Scholar]
- 82.Whitton, J. L., C. T. Cornell, and R. Feuer. 2005. Host and virus determinants of picornavirus pathogenesis and tropism. Nat. Rev. Microbiol. 3:765-776. [DOI] [PubMed] [Google Scholar]
- 83.Zhao, Q., J. M. Pacheco, and P. W. Mason. 2003. Evaluation of genetically engineered derivatives of a Chinese strain of foot-and-mouth disease virus reveals a novel cell-binding site which functions in cell culture and in animals. J. Virol. 77:3269-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]