Abstract
In light of the recurrent outbreaks of low pathogenic avian influenza (LPAI) and highly pathogenic avian influenza (HPAI), there is a pressing need for the development of vaccines that allow rapid mass vaccination. In this study, we introduced by reverse genetics temperature-sensitive mutations in the PB1 and PB2 genes of an avian influenza virus, A/Guinea Fowl/Hong Kong/WF10/99 (H9N2) (WF10). Further genetic modifications were introduced into the PB1 gene to enhance the attenuated (att) phenotype of the virus in vivo. Using the att WF10 as a backbone, we substituted neuraminidase (NA) for hemagglutinin (HA) for vaccine purposes. In chickens, a vaccination scheme consisting of a single dose of an att H7N2 vaccine virus at 2 weeks of age and subsequent challenge with the wild-type H7N2 LPAI virus resulted in complete protection. We further extended our vaccination strategy against the HPAI H5N1. In this case, we reconstituted an att H5N1 vaccine virus, whose HA and NA genes were derived from an Asian H5N1 virus. A single-dose immunization in ovo with the att H5N1 vaccine virus in 18-day-old chicken embryos resulted in more than 60% protection for 4-week-old chickens and 100% protection for 9- to 12-week-old chickens. Boosting at 2 weeks posthatching provided 100% protection against challenge with the HPAI H5N1 virus for chickens as young as 4 weeks old, with undetectable virus shedding postchallenge. Our results highlight the potential of live att avian influenza vaccines for mass vaccination in poultry.
Although culling of infected poultry remains the most effective strategy to prevent the transmission of the avian influenza virus, when the viruses are widely spread in multiple domestic and wild avian species such as in the case of the Asian H5N1 epidemic, “stamping out” alone is unlikely to be successful. Depopulation of infected flocks in combination with vaccination of at-risk poultry populations is being implemented in several Asian countries, Italy, and Mexico as an alternative strategy to control the spread of the disease (4, 19, 25). Vaccination of high-risk birds or flocks has been shown to be an effective complementary tool to control the spread of avian influenza (8).
There are major limitations in the implementation of vaccination campaigns in Asia due to the endemicity and spread of low pathogenic avian influenza (LPAI) and highly pathogenic avian influenza (HPAI) viruses. Inactivated whole avian influenza virus vaccine and recombinant fowlpox virus vaccine carrying avian influenza virus H5 hemagglutinin (HA) require the administration of the vaccine to each bird individually by parenteral inoculation; an approach that cannot realistically achieve the mass vaccination that would be required to eradicate the disease. Inactivated vaccines elicit strong humoral responses; however, it is commonly accepted that no adequate mucosal or cellular immunity is achieved (48). Previous exposure to the fowlpox virus would cause inconsistent protection for the birds immunized with the fowlpox virus-vectored vaccine (44). Therefore, the major concern is that the current vaccines may only be effective at lessening disease symptoms, not at preventing virus shedding below transmissible levels. Under these circumstances, the vaccine could allow the virus to circulate undetected among birds, further enhancing antigenic drift and spread (19, 21, 38). This is particularly important in the vaccination of domestic ducks, and perhaps other domestic aquatic birds, in which the high efficacy of the vaccine is critical.
Live attenuated (att) vaccines have been shown to protect against diseases in humans and animals while eliminating the risk of infection and/or transmission of the disease. Smallpox and polio in humans and rinderpest in animals are two examples of complete or almost complete eradication of viral diseases by using live att vaccines (9, 24, 37). In poultry, viral diseases are also effectively controlled by using modified live vaccines, such as those for Newcastle disease, Gumboro, infectious laringotracheitis, and Marek's disease (29, 31, 39, 47). In ovo administration of live att vaccines to 18-day-old embryos has been widely applied to commercial broilers in the United States, mainly against Marek's disease. In addition, automated in ovo vaccination delivers a more uniform dose of vaccine to the embryo and elicits earlier immunity than manual vaccination of the posthatching chicks (1, 40).
In the 1960s, Maassab and collaborators developed live att vaccines for type A and B human influenza viruses by serial passage of the wild-type virus at successively lower temperatures in chicken embryo kidney (CEK) cells (22). Recently, a trivalent, live att, cold-adapted (ca), temperature-sensitive (ts) reassortant vaccine (Flumist) has been licensed for use in humans in the United States (27). The ca/ts/att influenza A virus contains HA and neuraminidase (NA) gene segments derived from the currently circulating wild-type strain and the PB2, PB1, PA, NP, M, and NS gene segments from the ca/ts/att master donor virus, A/Ann Arbor/6/60 (H2N2). The viruses replicate efficiently at 25°C (ca) but are restricted at 39°C (ts) and do not replicate in the lungs of infected ferrets (att). The ca/ts/att influenza vaccines are safe, genetically stable, nontransmissible, and likely more immunogenic than inactivated vaccines (18, 28). Administered intranasally, live att vaccines provide long-lasting protection and induce both systemic and secretory immunoglobulin A (IgA) antibodies and cell-mediated immunity, which closely resembles the result of the natural infection (5, 7).
Live att influenza vaccines are also currently used in horses (32, 46). In contrast, live att avian influenza vaccines for poultry have not yet been developed. Sequence analysis revealed 11 amino acid mutations in att A/Ann Arbor/6/60 (H2N2) when compared to the sequence of the wild-type virus (6). Among these mutations, five ts loci only, three in the PB1 gene (K391E, E581G, and A661T), one in the PB2 gene (N265S), and one in the NP gene (D34G), were sufficient to confer to influenza virus A/Puerto Rico/8/34 (H1N1) the ts phenotype in vitro and the att phenotype in ferrets (17). In this report, we show that these same ts mutations conferred the ts phenotype in vitro to an avian influenza virus. Further genetic modifications were introduced into the PB1 gene of the avian virus to enhance the att phenotype in chickens and to discriminate by reverse transcription-PCR (RT-PCR) the vaccinated from the infected birds during acute stages of infection. Our studies showed that a single-dose posthatching or in ovo vaccination promoted efficient levels of protection for vaccinated birds in both the LPAI and HPAI challenge models.
MATERIALS AND METHODS
Viruses and cells.
A/Guinea Fowl/Hong Kong/WF10/99 (H9N2) (WF10) was kindly provided from the repository of St. Jude's Children's Research Hospital by Robert Webster; influenza virus A/Chicken/Delaware/VIVA/04 (H7N2) (CK/04) was obtained from Dennis Senne at the National Veterinary Laboratory Services, USDA; highly pathogenic influenza virus A/Vietnam/1203/04 (H5N1) (A/VN/1203/04) was obtained from the repository at the Centers for Disease Control and Prevention (CDC), Atlanta, Georgia. The viruses were propagated in 10-day-old embryonated specific-pathogen-free chicken eggs at 35°C and stored at −70°C. The viruses were titrated by the Reed and Muench method to determine the 50% egg infectious dose (EID50) (11). The HA titers were determined by HA assay. Madin-Darby canine kidney (MDCK) cells were maintained in modified Eagle's medium (MEM) (Sigma-Aldrich, St. Louis, MO) containing 5% fetal bovine serum (FBS) (Sigma-Aldrich). 293-T human embryonic kidney cells were cultured in OptiMEM I (GIBCO, Grand Island, NY) containing 5% FBS. CEK cells were isolated from 18-day-old chicken embryos and maintained in M199 medium (GIBCO, Grand Island, NY) containing 5% FBS and 2.5% chicken serum.
Cloning and generation of viruses by reverse genetics.
The HA and NA genes of CK/04 (H7N2) were cloned using a set of universal primers as described previously (14, 15). The cloning of the eight genes of the WF10 virus has been described in separate studies (36). The H5Δ (with the deletion of the polybasic amino acid sequence) and N1 genes from A/VN/1203/04 were cloned from the 6PR8:2H5ΔN1 recombinant virus, a kind gift from Ruben Donis, CDC. The cloned genes were sequenced, and the sequences compared to the corresponding viral sequences to determine that the clones did not carry spurious mutations. Sequences were generated by using a Big Dye Terminator v3.1 cycle sequencing kit 1 (Applied Biosystems, Foster City, CA) and a 3100 genetic analyzer (Applied Biosystems), according to the instructions of the manufacturers. The ts mutations in PB1 and PB2 were introduced by site-directed mutagenesis using a commercially available kit (Stratagene, La Jolla, CA). The PB1 gene of the WF10 virus was further modified by PCR, incorporating an HA tag sequence (8 amino acids derived from the influenza virus H3 HA protein sequence [tag]) in frame with the PB1 open reading frame while preserving the essential assembly sequences (30). The HA tag was incorporated in the context of wild-type and ts PB1 sequences as indicated in the text and in Fig. 1. Thus, the C terminus of the PB1 gene at the HA tag junction contains the following sequence: EDMYPYDVPDYASRICSTIEELRRQK-C terminus, in which the underlined amino acids correspond to artificially introduced amino acids, those in italics correspond to the HA tag, and the rest to PB1. For in vitro studies, the HA gene derived from influenza virus A/Mallard/Alberta/24/01 (H7N3) (Mal/01) adapted to MDCK cells, a kind gift from R. Webster, was used because it provides a large-plaque phenotype in MDCK cells in the presence of trypsin (H. Song and D. R. Perez, unpublished).
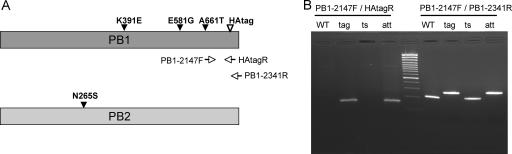
FIG. 1.
Schematic representation of avian influenza virus PB1 and PB2 constructs for the generation of ts and HA-tagged mutant viruses. (A) Site-directed mutagenesis was used to introduce three ts mutations (K391E, E581G, and A661T) into the PB1 gene and one (N265S) into the PB2 gene of the WF10 (H9N2) virus. The PB1 gene was further modified by incorporating an HA tag sequence in frame with the C terminus of the PB1 protein. The HAtagR primer is unique for the HA tag sequences, whereas the PB1-2147F and PB1-2341R primers anneal to sequences in the PB1 gene. (B) Viral RNA was isolated from the recombinant viruses grown in embryonated chicken eggs. The RNA was RT-PCR amplified using two sets of primers as indicated. The RT-PCR products were analyzed on a 2% agarose gel in the presence of ethidium bromide. A 100-bp ladder was used as a molecular weight marker. WT, tag, ts, and att correspond to four different virus strains: 7WF10:1malH7, 7tagWF10:1malH7, 7tsWF10:1malH7, and 7attWF10:1malH7.
Viruses were recovered as described previously (13). Briefly, the day before transfection, confluent 293T and MDCK cells in a 75-cm2 flask were trypsinized, and 10% of each cell line was mixed in 18 ml OptiMEM I; 3 ml of this cell suspension was seeded into one well of a six-well plate. The next day, 1 μg of each plasmid (∼8 μg) was mixed with 18 μl of TransIT LT-1 (Mirus, Madison, WI). After 45 min of incubation at room temperature, the mixture was added to the cells. Six h later, the DNA transfection mixture was replaced by OptiMEM I. Thirty h after transfection, 1 ml of OptiMEM I containing 1 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin was added to the cells. The viruses were propagated in 10-day-old embryonated chicken eggs and titrated by the EID50. The recovery of recombinant viruses was verified by sequencing using specific primers. The wild-type and HA-tagged viruses were differentiated by RT-PCR using the specific primer sets PB1-2147F and HAtagR and PB1-2147F and PB1-2431R, as shown in Fig. 1 (sequences of the primers provided upon request). The genetic stability of the mutant viruses was evaluated by serial passage (10 times) of virus stocks at a 1:10,000 dilution in 10-day-old embryonated eggs.
Plaque assays and immunostaining.
The ca/ts phenotypes of the recombinant viruses were examined by plaque assay in MDCK cells and CEK cells at 32°C, 37°C, 39°C, and 41°C. Confluent cell monolayers in six-well plates were infected with 10-fold dilutions of virus in a total volume of 0.4 ml of phosphate-buffered saline (PBS) for 1 h at 37°C. Cells were washed once with PBS and covered with an overlay of modified Eagle's medium containing 0.9% agar, 0.02% bovine serum albumin, 1% glutamine, and 1 μg/ml TPCK-trypsin. The plates were then incubated at 32°C, 37°C, 39°C, and 41°C under 5% CO2. After 3 days of incubation at 37°C, 39°C, and 41°C or 4 days at 32°C, the overlays were removed and the cells were fixed with 4% paraformaldehyde and permeabilized with 0.2% Triton X-100. The potential endogenous peroxidase activity was destroyed by incubation with 1% H2O2-methanol. After being blocked with 1% bovine serum albumin in PBS, the cells were incubated with mouse anti-WF10 polyclonal antibody prepared in our laboratory, followed by incubation with peroxidase-conjugated goat anti-mouse IgG (Jackson Immuno Research, West Grove, PA). The viral antigen was visualized by incubating the cells in a solution of aminoethylcarbazol (Dakocytomation, Carpinteria, CA). The size and number of plaques were obtained at each temperature and compared to determine the ts phenotype of each virus. The nonpermissive temperature was defined as the lowest temperature that had a titer reduction of 100-fold or greater compared to the titer at 37°C.
Western blot assay.
MDCK cells grown in six-well plates were infected with the recombinant viruses and A/Memphis/98 (H3N2) as control. After infection, the cells were trypsinized and collected by centrifugation. The cells were washed once with ice-cold PBS, resuspended in 50 μl of PBS, and mixed with 100 μl Laemmli sample buffer (Bio-Rad, Hercules, CA). The samples were then boiled for 5 min and centrifuged at 13,000 × g for 3 min at 4°C. For immunoblotting, the cell lysates were fractionated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), and the proteins were transferred onto nitrocellulose membrane (Bio-Rad, Hercules, CA) for immunoblot analysis. The membranes were blocked in 5% nonfat milk in PBS for 1 h at room temperature, and then incubated for 1 h with primary antibodies for NP (mouse anti-WF10 polyclonal antibody), M1 (mouse anti-M1 monoclonal antibody [ATCC, Manassas, VA]), actin (mouse antiactin monoclonal antibody [Chemicon, Temecula, CA]) or the HA tag (rat anti-HA monoclonal antibody [Roche Diagnostics, Indianapolis, IN]). The immunoblots were washed three times with PBS containing 0.05% Tween 20 and subsequently incubated with a 1:10,000 dilution of goat anti-mouse or goat anti-rat IgG conjugated to horseradish peroxidase (Jackson Immuno Research, West Grove, PA). Finally, the membranes were washed three times and visualized by enhanced chemiluminescence (Pierce, Rockford, IL).
Virus replication and transmission study.
Animal studies were approved by the Animal Care and Use Committee of the University of Maryland, College Park. Three 3-week-old White Leghorn chickens (Charles River Laboratories, MA) were inoculated intraocularly, intranasally, orally, and intratracheally with 5 × 106 EID50 of avian influenza virus contained in 1 ml inoculum. Eight drops (0.2 ml) were introduced through the eyes and nares, and 0.8 ml of the virus dilution was equally distributed between oral and tracheal inoculations. The day after infection, three naïve birds were introduced to the same cage with the infected birds, in order to monitor the transmissibility of the virus. Tracheal and cloacal swabs were collected from both the infected and contact birds at days 1, 3, 5, 7, and 9 postinfection. The samples were stored in glass vials diluted in 1 ml freezing medium (50% glycerol-PBS containing antibiotics) and titrated for infectivity in 10-day-old embryonated chicken eggs. Sera were collected 2 weeks after infections and tested for antibodies against HA by an HA inhibition (HI) test. In a separate study, three 3-week-old White Leghorn chickens were infected as described above, except that an additional 0.5 ml of the virus dilution was administrated through the cloaca. At 3 days postinfection, tracheal and cloacal swabs were collected, the birds were sacrificed, lung homogenates were prepared, and the virus was titrated by inoculating 10-day-old embryonated eggs. The birds were observed and scored daily for clinical signs of illness. The experiments were carried out under BSL2 conditions.
Dose-dependent immunization and low pathogenic H7N2 challenge study.
Two-week-old White Leghorn chickens were immunized with 50, 500, 5,000, 5 × 104, 5 × 105, or 1 × 106 EID50 vaccine virus (6attWF10:2ckH7N2) in 0.5 ml of diluent through intraocular, intranasal, oral, and intratracheal inoculation. At 3 and 5 days postvaccination, tracheal swabs from all the vaccinated birds were collected. The presence of both the ts mutation and the HA tag in the recombinant vaccine virus were confirmed by RT-PCR and sequencing as described above. Two weeks after vaccination, the chickens were challenged by intranasal inoculation with 5 × 105 EID50 of influenza virus CK/04, corresponding to 500 50% chicken infectious doses (data not shown). A group of eight chickens immunized only with PBS served as challenge control for virus shedding. To evaluate the level of virus shedding, both tracheal and cloacal swab samples were collected at 3, 5, and 7 days postchallenge. Sera were collected 2 weeks after vaccination and 2 weeks after challenge, respectively. Sera were treated with receptor-destroying enzyme (Denka Seiken Co., Tokyo, Japan) and tested for antibodies against eight HA units of Ck/04 by HI assay following the World Health Organization (WHO) protocol.
Immunization and highly pathogenic H5N1 challenge study.
In ovo vaccination of 18-day-old embryonated specific-pathogen-free chicken eggs was performed as described previously (45). Briefly, the eggs were candled, and a small hole was made through the air cell with a drill. The eggs were injected with 100 μl of high-dose (106 EID50) or low-dose (104 EID50) live att vaccine (6attWF10:2H5ΔN1) or PBS only by using a 21-gauge needle at a depth of 1 in. At 2 weeks posthatching, a boost vaccination was performed, when indicated. Eight chickens from each of the in ovo-vaccinated groups were boosted with either a high dose (106 EID50/0.5 ml) or low dose (104 EID50/0.5 ml). Serum samples were collected from the jugular or wing vein on a weekly basis for the determination of HI antibody titers. At 4 weeks old, the chickens were challenged by intranasal inoculation of 1 × 105 EID50/0.2 ml of A/VN/1203/04 (H5N1) virus. Two groups of eight chickens that were immunized in ovo with 106 EID50 single-dose vaccine were kept until they were 9 or 12 weeks old, at which time the chickens were challenged with 3 × 105 EID50/0.6 ml of A/VN/1203/04 virus. Tracheal and cloacal swab samples were collected on days 2, 4, and 7 postchallenge for virus titration. After challenge, the birds were observed and scored daily for morbidity and mortality for the next 14 days. The survivors were bled and humanely sacrificed at 14 days after challenge. HI antibody titers were determined against eight HA units of the A/VN/1203/04 virus. Challenge studies with the HPAI H5N1 virus were performed in an enhanced biosafety level 3 facility approved by the USDA.
RESULTS
The ts phenotype of the PB1 and PB2 genes in the ca/ts/att A/Ann Arbor/6/60 strain can be transferred to an avian influenza virus.
The ts phenotype of the A/Ann Arbor/6/60 (H2N2) strain, the master donor of the ca human influenza virus, has been mapped to three amino acid mutations in PB1 (K391E, E581G, and A661T), one in PB2 (N265S), and one in NP (D34G) (16). Viruses carrying these mutations can replicate efficiently in vitro at a temperature of about 33°C but are restricted for growth at 38 to 39°C. The attenuation phenotype is observed in vivo in the ferret model in which the mutant viruses establish limited infection in the upper respiratory tract but not in the lower respiratory tract (17). Sequence alignment of the PB1 and PB2 genes revealed that avian influenza viruses do not carry the amino acid mutations found in the ca/ts A/Ann Arbor/6/60 strain and, thus, are not expected to have a ca/ts phenotype (not shown). The WF10 used in our study already contains the D34G mutation found in the NP gene of the ca/ts A/Ann Arbor/6/60 strain. In fact, of the approximately 2,000 avian influenza virus NP sequences available in GenBank, the vast majority code for glycine or serine at position 34, with a single virus strain [A/chicken/Korea/38349-96323/96 (H9N2)] coding for aspartic acid in this position. This observation suggests that the former 2 amino acids may favor the adaptation of influenza viruses to eggs or avian species. In contrast, the NP gene of most human influenza viruses (more than 2,500 sequences are available in GenBank) encode for aspartic acid at position 34, although the occasional emergence of seasonal strains carrying a glycine is not uncommon.
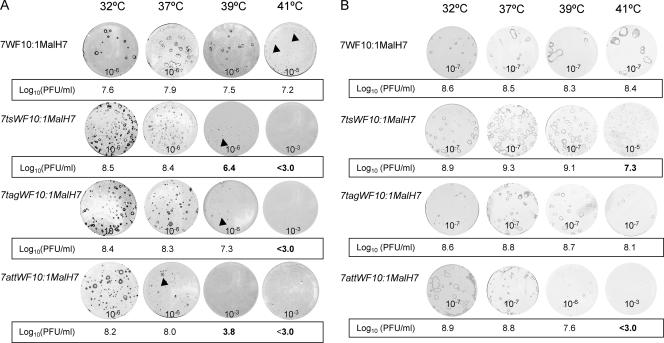
To determine whether the ts mutations found in the ca/ts A/Ann Arbor/6/60 strain would impart the same ts phenotype to an avian influenza virus, the PB1 and PB2 genes of WF10 were mutated accordingly (Fig. 1). Both the ts mutant and wild-type viruses carrying the H7 HA gene from an MDCK cell-adapted Mal/01 (H7N3) virus were recovered. The HA gene from the cell-adapted Mal/01(H7N3) virus provides a large-plaque phenotype in MDCK cells (H. Song and D. R. Perez, unpublished). The mutant virus was designated 7tsWF10:1malH7, whereas its wild-type counterpart was labeled 7WF10:1malH7. We tested the abilities of these viruses to form plaques at different temperatures in MDCK cells (Fig. 2A). Plaque assays were carried out, and 3 days postinfection at 37°C, 39°C, and 41°C or 4 days postinfection at 32°C, the cells were immunostained with mouse anti-WF10 polyclonal antibody. Compared with the titer of the wild-type virus, the 7tsWF10:1malH7 recombinant virus showed a 100-fold reduction in virus titer at 39°C relative to its titer at 37°C. At 41°C, the wild type showed pinpoint plaques, whereas none of the mutants were able to form plaques at this temperature, even at low dilutions (10−3; Fig. 2A).
FIG. 2.
Plaque morphologies of mutant avian influenza viruses at various temperatures. Confluent MDCK cells (A) or CEK cells (B) seeded in six-well plates were infected with recombinant viruses. The numbers 10−7, 10−6, 10−5, 10−4, and 10−3 on the plaque pictures indicate the virus dilution used to infect cells at the indicated temperature. At 3 days postinfection for cells incubated at 37°C, 39°C, or 41°C and 4 days postinfection for those incubated at 32°C, cell monolayers were fixed and the viral antigen was visualized by immunostaining as described in Materials and Methods. The plaques were counted, and virus titers were represented as the log10 PFU/ml, as indicated below the individual plaque picture. A titer of <3.0 log10 PFU/ml) indicates that no virus was detected at 10−3 dilution. The nonpermissive temperature was defined as the lowest temperature that had a titer reduction of 100-fold or greater compared to 37°C. Titers that define the shutoff temperature are shown in bold. Arrows in panel A indicate pinpoint plaques. Note: Adobe Photoshop version 7.0 was used for panel A to enhance the contrast of the plaque immunostaining in MDCK cells.
We wanted also to confirm whether the ts phenotype imparted by the mutations in PB1 and PB2 of the WF10 virus could be maintained in cells of avian origin. Plaque assays were performed using primary CEK cells. As shown in Fig. 2B, the wild-type and ts viruses formed bigger plaques and grew to higher titers in CEK cells than in MDCK cells. This observation is consistent with the results of previous studies that indicate that CEK cells are a better substrate than MDCK cells to propagate avian influenza viruses (43). The pattern of restriction of the ts mutant viruses in CEK cells at different temperatures was similar to the one observed in MDCK cells. It is important to note that there were overall improvements in the abilities of wild-type and mutant viruses to replicate at 39°C and 41°C in CEK cells. Interestingly, although the 7tsWF10:1malH7 virus could not form plaques in MDCK cells at 41°C, it formed small-sized plaques at 41°C in CEK cells. Our results suggest that cellular factors could be contributing to the overall effect on the ts phenotype in these viruses. In our studies, the ts phenotype was more evident in MDCK cells than in CEK cells. Interestingly, the ts viruses were not greatly att in chickens, i.e., titers in the trachea and lungs were statistically indistinguishable from those obtained in infections with wild-type viruses (see Table 1). Thus, additional modifications in the genomes of the avian influenza viruses were needed in order to produce a live att avian influenza virus for birds.
TABLE 1.
Replication of the reassortant viruses in chickensa
| Virus | Virus titer in:
|
||
|---|---|---|---|
| Lungs (log10 EID50/g ± SE) | Trachea (log10 EID50/ml ± SE) | Cloaca (log10 EID50/ml ± SE) | |
| 6WF10:2ckH7N2 | 3.6 ± 0.5 | 3.6 ± 0.8 | 4.0 ± 1.0 |
| 6tsWF10:2ckH7N2 | 3.8 ± 0.6 | 3.2 ± 0.6 | 4.0 ± 1.0 |
| 6tagWF10:2ckH7N2 | 4.0 ± 1.0 | 2.9 ± 0.6 | 2.4 ± 0.5 |
| 6attWF10:2ckH7N2 | BLD | 2.7 ± 0.3 | 1.0b |
Three 3-week old White Leghorn chickens were inoculated intraocularly, intranasally, orally, intratracheally, and cloacally with 5 × 106 EID50 of virus. Three days postinfection, tracheal and cloacal swab samples were collected, and lung homogenates were prepared. The experiment was repeated once. Values are the means ± standard errors for six chickens. The detection limit is 0.7 log10 EID50/ml. BLD, below limit of detection.
Two out of six infected chickens had positive cloacal samples with 1.0 log10 EID50/ml.
An additional genetic modification in the PB1 gene of an avian influenza virus enhances the ts phenotype in vitro and the att phenotype in birds.
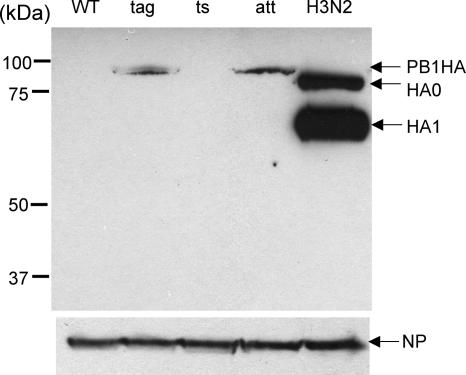
Using reverse genetics, we had previously generated a laboratory strain of influenza virus A/WSN/33 (H1N1) carrying a recombinant PB1 gene in which the C terminus of PB1 was fused to an 8-amino-acid HA epitope tag (PB1tag) (D. R. Perez, unpublished). The growth kinetics of the 7WSN:1PB1tag virus was slower than the kinetics of the wild-type virus, although it reached titers similar to those obtained with the wild-type strain at 37°C and displayed a ts phenotype at 39°C (not shown). We wanted to determine if avian influenza viruses carrying a PB1tag recombinant gene in the context of other ts mutations would be att in birds. We modified the PB1 of the wild-type WF10 virus to carry just the HA epitope tag or the HA tag with the ts loci (Fig. 1A). The new, recovered viruses were labeled 7tagWF10:1malH7 and 7attWF10:1malH7, respectively. The recovery of the recombinant viruses was verified by sequence analysis using viruses grown in eggs. In addition, the recovery of the HA-tagged viruses was demonstrated by RT-PCR. Using the pair of primers PB1-2147 and HA tagR (Fig. 1B), a 150-bp PCR product could be specifically amplified only in the 7tagWF10:1malH7 and 7attWF10:1malH7 viruses, but not in 7tsWF10:1malH7 or 7WF10:1malH7. A second, control PCR product was amplified using the primer pair PB1-2147F and PB1-2341R. The viruses with the HA tag showed a band of slower migration in an agarose gel due to the larger size of the products containing extragenic sequences. The in-frame cloning of the HA tag in PB1 also allowed the detection of the PB1 protein by using a monoclonal antibody against the HA tag (Fig. 3). The expression of the PB1-HA fusion protein of approximately 90 kDa was readily detected from MDCK cell extracts prepared 16 h after infection at a multiplicity of infection (MOI) of 1 with the 7tagWF10:1malH7 and 7tattWF10:1malH7 viruses, but not with either the 7tsWF10:1malH7 or 7WF10:1malH7s virus.
FIG. 3.
Immunoblot analysis of HA epitope expression in virus-infected cells. MDCK cells were infected with different recombinant viruses or A/Memphis/98 (H3N2) (positive control for HA tag expression) at an MOI of 1.0 at 37°C and harvested at 16 h postinfection. After lysis, cellular proteins were separated by 10% SDS-PAGE, blotted onto nitrocellulose, and incubated with monoclonal rat anti-HA (upper panel) or mouse anti-WF10 polyclonal antibody (lower panel). The membrane was subsequently incubated with goat anti-mouse or goat anti-rat IgG conjugated to horseradish peroxidase and developed by enhanced chemiluminescence. A ∼90-kDa band corresponding to the PB1-HA fusion protein is observed in extracts of cells infected with the HA tag-expressing viruses. HA0 and HA1 of the H3 virus are shown. The expression of NP is shown as loading control. The size of protein markers (in kDa) is shown on the left. WT, tag, ts, and att correspond to four different virus strains: 7WF10:1malH7, 7tagWF10:1malH7, 7tsWF10:1malH7, and 7attWF10:1malH7.
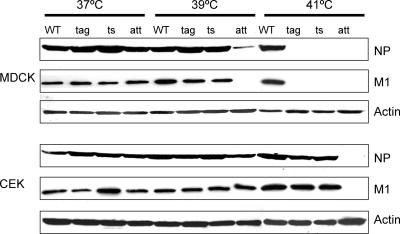
The ca and ts phenotypes of the HA-tagged viruses were examined by plaque assay in MDCK and CEK cells at various temperatures (32°C, 37°C, 39°C, and 41°C) as described above. As shown in Fig. 2, the HA epitope alone was sufficient to confer a ts phenotype to the virus in MDCK at 39°C. Moreover, the HA-tagged virus (7tagWF10:1malH7) failed to form plaques at 41°C, even at a 10−3 dilution. Albeit limited, the ts phenotype was also observed in CEK cells at 41°C; it formed much smaller-sized plaques than the wild-type virus at this temperature. More importantly, the double-mutant virus 7attWF10:1malH7 was completely restricted at 39°C and 41°C in MDCK cells and at 41°C in CEK cells, showing >10,000-fold reductions in virus titers compared to the growth at 32°C. Thus, our strategy resulted in an avian influenza virus with the typical characteristics of a ts strain. These observations were confirmed by analyzing the effect on viral protein synthesis at different temperatures in MDCK and CEK cells. Figure 4 shows the results of Western blot analysis examining the accumulation of one of the early viral proteins, NP, and the late viral protein, M1, at 6 h postinfection in cell extracts previously infected with the indicated influenza viruses at an MOI of 10. In MDCK-infected cells, complete inhibition of protein synthesis for the ts, tag, and att mutant viruses was observed at 41°C. In CEK cells, inhibition of viral protein synthesis at 41°C is only observed with the double-mutant ts HA virus. Interestingly, viral protein synthesis at other temperatures (37°C and 39°C) achieved levels similar to those of the wild-type virus in both cell types, except for the att virus in MDCK cells at 39°C. These results suggest that the ts restriction and the resulting small-plaque phenotype are not due exclusively to alterations of viral protein synthesis at higher temperatures. The ts loci may also be affecting other viral functions, such as nuclear export or assembly. With the ts loci and the incorporation of the HA tag in the PB1 protein, we were able to enhance the ts phenotype of avian influenza virus, making a live att influenza virus.
FIG. 4.
Viral protein accumulation at various temperatures in infected cells. MDCK and CEK cells were infected with recombinant viruses at an MOI of 10 at 37°C, 39°C, and 41°C, and harvested at 6 h postinfection. Cell lysates were prepared and run on a 10% SDS-PAGE. As described in the legend of Fig. 3 and in Materials and Methods, the expression of viral proteins NP and M1 was detected with a mouse anti-WF10 polyclonal antibody and mouse anti-M1 monoclonal antibody, respectively. As loading control, the expression of actin was monitored by using a mouse antiactin monoclonal antibody. WT, tag, ts, and att correspond to four different virus strains: 7WF10:1malH7, 7tagWF10:1malH7, 7tsWF10:1malH7, and 7attWF10:1malH7.
The viruses harboring either the HA tag or ts mutations were not as att in cell cultures at higher temperature as the double-mutant att virus, suggesting that the HA tag and ts mutations worked synergistically to contribute to the ts effect (Table 2). Further analysis revealed that the HA tag virus with the triple (PB1K391E E581G A661Ttag/PB2wt) or double ts mutations (PB1K391E E581Gtag/PB2wt) in PB1 display an attenuation phenotype that resembles that of the double mutant 7attWF10:1malH7, i.e., it failed to form plaques at 41°C in CEK cells at a 10−3 dilution. In contrast, the HA tag virus with the N265S mutation in PB2 (PB1tag/PB2N265S) shows a reduction of only about 1.4 log10 PFU/ml in virus titer at 41°C compared to its growth at 37°C. All other ts/tag combinations have an intermediate ts phenotype compared to that of the 7tsWF10:1malH7 virus.
TABLE 2.
Replication of recombinant viruses at various temperatures in CEK cellsa
| Viruses | Virus titer (log10 PFU/ml)d at:
|
||
|---|---|---|---|
| 37°C | 41°Cb | 37°C/41°C | |
| PB1K391E E581G A661Ttag/PB2N265S (7attWF10:1malH7) | 8.8 | <3.0 | >5.8 |
| PB1K391E E581G A661T/PB2 | 8.6 | 8.2 | 0.4 |
| PB1K391E E581G A661T/PB2N265S (7tsWF10:1malH7) | 9.3 | 7.3 | 2.0 |
| PB1tag/PB2 (7tagWF10:1malH7) | 8.8 | 8.1 | 0.7 |
| PB1tag/PB2N265S | 7.0 | 5.6 | 1.4 |
| PB1K391E E581G A661Ttag/PB2 | 8.7 | <3.0 | >5.7 |
| PB1K391Etag/PB2 | 8.2 | 6.7c | 1.5 |
| PB1E581Gtag/PB2 | 8.6 | 7.5c | 1.1 |
| PB1A661Ttag/PB2 | 8.2 | 7.6c | 0.6 |
| PB1K391E A661Ttag/PB2 | 8.0 | 6.5c | 1.5 |
| PB1K391E E581Gtag/PB2 | 8.6 | <3.0 | >5.6 |
| PB1E581G A661Ttag/PB2 | 8.2 | 6.9c | 1.3 |
Confluent CEK cell monolayers in six-well plates were infected with 10-fold dilutions of viruses. The plaque counts were obtained at each of the temperatures.
A titer of <3.0 log10 PFU/ml indicates that no plaque was detected at a 10−3 dilution. The nonpermissive temperature was defined as the lowest temperature that had a titer reduction of 100-fold or greater compared to the titer at 37°C. Titers that define the shutoff temperature are shown in bold.
Plaque size was reduced and immunostaining weaker than in the same recombinant virus at 37°C.
The virus titer represents the average of two independent experiments.
In order to determine whether our strategy would result in an att virus with potential as a vaccine candidate for birds, we tested the transmission and replication of recombinant viruses carrying the surface proteins of a low pathogenic virus, Ck/04 (H7N2). The Ck/04 (H7N2) is an isolate that was implicated in an outbreak of influenza in poultry in Maryland in 2004. We recovered reassortant viruses that contained the HA and NA genes derived from Ck/04 and different sets of mutant or wild-type genes derived from the WF10 virus. The recombinant virus containing the surface genes of Ck/04 and the internal genes of the wild-type WF10 virus (6WF10:2ckH7N2) replicates and transmits efficiently to naïve contact chickens (Table 3). In contrast, no evidence of transmission was observed with any of the mutant backbones tested, namely the ts, HA, or att virus. No virus shedding and no seroconversion were detected in naïve birds that were placed in contact with chickens infected with any of the mutant viruses (Table 3).
TABLE 3.
Transmission studies of the recombinant viruses in chickensa
| Virus | Chicken group | No. with positive tracheal swab/total no. at day
|
No. that seroconverted/total no.c | ||||
|---|---|---|---|---|---|---|---|
| 1 | 3 | 5 | 7 | 9 | |||
| 6WF10:2ckH7N2 | Inoculatedb | 3/3 | 3/3 | 2/3 | 0/3 | 0/3 | 3/3 |
| Contact | 0/3 | 0/3 | 2/3 | 2/3 | 0/3 | 2/3 | |
| 6tsWF10:2ckH7N2 | Inoculated | 3/3 | 3/3 | 3/3 | 0/3 | 0/3 | 3/3 |
| Contact | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | |
| 6tagWF10:2ckH7N2 | Inoculated | 3/3 | 3/3 | 1/3 | 0/3 | 0/3 | 3/3 |
| Contact | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | |
| 6attWF10:2ckH7N2 | Inoculated | 3/3 | 3/3 | 2/3 | 0/3 | 0/3 | 3/3 |
| Contact | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | |
Three 3-week-old White Leghorn chickens were inoculated intraocularly, intranasally, orally, and intratracheally with 5 × 106 EID50 dose of virus. The next day after infection, three naïve birds were introduced into the same cage as the infected birds. Tracheal and cloacal swab samples were collected from the chickens every 2 days for 9 days after inoculation.
Cloacal swab samples were negative for virus isolation for all inoculated chickens.
Chickens were sacrificed 2 weeks after inoculation and sera were harvested. Seroconversion was confirmed by an HI test.
The att phenotype of the ca/ts/att human influenza virus has been arbitrarily defined as limited virus replication and lack thereof in, respectively, the upper respiratory tract and the lower respiratory tract of the ferret (2, 23). We extended this definition to include birds and to determine whether the combination of the ts and HA tag mutations were sufficient to attenuate the virus, specifically in chickens. Since influenza virus replication can be established both in the respiratory and intestinal tracts in land-based birds, we evaluated cloacal swab samples for the presence of virus after inoculating the virus directly through the cloaca. Three-week-old White Leghorn chickens were infected with 5 × 106 EID50 of virus through the intraocular, intranasal, oral, intratracheal, and cloacal routes. At 3 days postinfection, tracheal and cloacal swab samples were collected; the birds were then sacrificed, lung tissues were harvested, and the viruses were titrated. Our results show that the double-mutant virus 6attWF10:ckH7N2 was att in chickens (Table 1). The double-mutant virus showed approximately 10-fold reductions in virus titers in tracheal swab samples compared to the titers of wild-type virus and failed to replicate in the lower respiratory tract (lung). Only traces of the double-mutant virus were detected in the cloacal swab samples in two out of the six infected chickens. This is probably due to the fact that the temperature in both the intestinal tract and lower respiratory tract of birds is close to 41°C, at which temperature the att virus fails to grow in CEK cells. Our results suggest that it is possible to create an avian influenza virus with an att phenotype in birds, i.e., a virus with only limited replication in the upper respiratory tract, unable to cause disease, unable to transmit and shed in feces, and potentially able protect against field infections if it mounts an adequate immune response.
A single vaccination dose of the 6attWF10:2ckH7N2 virus protects chickens from challenge with an LPAI H7 virus.
In order to evaluate the protective efficacy of the modified live att virus at different doses, 2-week-old chickens were vaccinated intranasally, intraocularly, orally, and intratracheally with 50, 500, 5,000, 5 × 104, 5 × 105, or 106 EID50 of the 6attWF10:2ckH7N2 virus (Table 4). At 2 weeks postvaccination, the chickens were challenged with 100 50% chicken infectious doses of the low pathogenic Ck/04 (H7N2) virus by the intranasal route. Eight unvaccinated chickens were used as positive controls to determine the replication efficiency of the challenge virus. The protective efficacy of the vaccine is shown as the reduction of virus shedding in both trachea and cloaca compared to the level of virus shedding in unvaccinated controls. Both tracheal and cloacal swab samples were collected at days 3, 5, and 7 postchallenge to determine the amount of virus shedding. The chickens vaccinated with equal or more than 5 × 103 EID50 of 6attWF10:2ckH7N2 virus were protected from virus reinfection. Two birds in the group vaccinated with 500 EID50, which seroconverted at 14 days postvaccination, were also fully protected from virus infection. Our results indicate that a relatively small amount of vaccine virus inoculum (≥5 × 103 EID50) was sufficient to provide adequate protection against challenge with an LPAI virus strain. In contrast, the eight unvaccinated control chickens shed a substantial amount of virus after challenge (Table 4).
TABLE 4.
Dose-dependent att H7N2 vaccination study in chickens challenged with LPAI virus Ck/04 (H7N2)a
| Vaccine dose (EID50) | No. with positive HI result/total no. (GMT) at 14 days p.v. | No. shedding virus/total no. (log10 EID50/ml ± SD)b in:
|
No. with positive HI result/total no. (GMT) at 14 d.p.i. | |||||
|---|---|---|---|---|---|---|---|---|
| Trachea at:
|
Cloaca at:
|
|||||||
| 3 d.p.i. | 5 d.p.i. | 7 d.p.i. | 3 d.p.i. | 5 d.p.i. | 7 d.p.i. | |||
| 5 × 101 | 0/3 | 3/3 (4.2 ± 0.8) | 3/3 | 2/3 | 0/3 | 0/3 | 0/3 | 3/3 (47) |
| 5 × 102 | 2/3 (25) | 1/3 (3.2) | 1/3 | 1/3 | 0/3 | 0/3 | 0/3 | 3/3 (80) |
| 5 × 103 | 3/3 (53) | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 3/3 (213) |
| 5 × 104 | 3/3 (66) | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 3/3 (106) |
| 5 × 105 | 3/3 (53) | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 3/3 (186) |
| 1 × 106 | 8/8 (46) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 (65) |
| 0 | 0/8 | 8/8 (4.6 ± 1.1) | 8/8 | 8/8 | 0/8 | 3/8 (3.5 ± 0.6) | 3/8 | 8/8 (64) |
Six groups of 2-week-old chickens were immunized through intraocular, intranasal, oral and intratracheal inoculation with the 6attWF10:2ckH7N2 vaccine strain at doses of 50, 500, 5 × 103, 5 × 104, 5 × 105, and 1 × 106 EID50 in 0.5 ml of diluent. A group of eight chickens vaccinated only with PBS served as challenge control for virus shedding. Two weeks after vaccination, chickens were challenged by intranasal inoculation with 5 × 105 EID50/0.2 ml of Ck/04 (H7N2). Tracheal and cloacal swab samples were collected for virus titration every 2 days for 7 days postchallenge. Sera were collected 2 weeks after vaccination and 2 weeks after challenge. Sera were tested for antibodies to HA by the HI test. GMT, geometric mean reciprocal end-point tier; p.v., postvaccination; d.p.i., days postinfection.
Mean virus titer ± standard deviation. The detection limit is 0.7 log10 EID50/ml.
In ovo vaccination protects chickens from challenge with an HPAI H5N1 virus.
In order to better establish the efficacy of our live att virus, we performed challenge studies using an HPAI H5N1 virus, A/VN/1203/04. In addition, we wanted to establish whether in ovo vaccination of 18-day-old chicken embryos with or without boost vaccination could potentially be a viable alternative to protect chickens against challenge with the HPAI H5N1 virus. We initially generated the 6attWF10:2H5ΔN1 virus, which contains the HA and NA genes of the A/VN/1203/04 virus vaccine strain (6PR8:2H5ΔN1) in which the multiple basic amino acids of the HA cleavage site have been removed (as provided by the CDC). The internal genes of the 6attWF10:2H5ΔN1 virus correspond to the WF10 att backbone (ts and HA tag). Replication and transmission studies using the 6attWF10:2H5ΔN1 virus were carried out on 2-week-old White Leghorn chickens. Once again we found that the virus is highly att: only trace amounts of virus shedding were detected at 3 days postinfection through the trachea, with no virus shedding detected in lung or cloaca; the virus was not able to transmit to the direct contact chickens (data not shown).
Based on our previous studies with the H7 vaccine virus, we chose two doses of the 6attWF10:2H5ΔN1 virus to immunize the chickens: a high dose (106 EID50) or low dose (104 EID50). In ovo administration of the 6attWF10:2H5ΔN1 live att vaccine virus was performed as described in Materials and Methods. Thirty eggs per group were inoculated with either a high or low dose of the vaccine virus or with PBS as mock vaccine control. The hatchability of the high-dose group was 85%, whereas those of the low-dose and PBS groups were 90%. Ten tracheal and cloacal swab samples were taken from each of the two in ovo-vaccinated groups at 3 days postvaccination (1 day posthatching). Only trace amounts of virus shedding were detected from the tracheal swab samples of 3 out of 10 chickens in the low-dose group and 4 out of 10 chickens in the high-dose group (Table 5). No virus shedding was detected from cloacal swab samples in any of the groups. Subsequently, a subset (eight/group) of the in ovo-vaccinated birds received a second, boost vaccination at 2 weeks posthatching. The boost vaccination consisted of either a low dose or a high dose of vaccine virus, which were administered to the low-dose and high-dose in ovo-vaccinated groups, respectively. Analysis of vaccine virus shedding in birds that received the boost dose showed traces of virus in only one out of eight chickens in the low-dose group and none in the high-dose group. In addition, a group of eight 2-week-old naïve chickens received a high dose of the vaccine, with evidence of low virus shedding in only two of the chickens. At 4 weeks of age, blood samples were collected from the chickens in the different vaccination groups to determine the serum HI titers. Subsequently, the chickens were challenged intranasally with 105 EID50 of the A/VN/1203/04 H5N1 HPAI virus, which is equivalent to 200 50% chicken lethal doses. As shown in Table 5, HI titers were observed at 4 weeks of age in 6/10 chickens that were vaccinated in ovo with either the high dose or low dose of virus. The chickens that received a boost dose of the vaccine at the high dose showed HI titers in eight/eight birds, whereas only four/eight birds that received a boost dose at the low dose showed HI titers. In all cases, HI titers were modest, although clearly discernible. Survival after challenge with the HPAI H5N1 virus was observed in all vaccine groups with different efficiencies: 6/10 and 7/10 chickens that received a single in ovo high dose or low dose of vaccine virus, respectively, survived the challenge, whereas 16/16 chickens that received the boost vaccination survived the challenge. Chickens that received a single high dose of the vaccine at 2 weeks posthatching were also protected, although three/eight chickens died after challenge. In comparison, none of the unvaccinated chickens survived after challenge and the median time to death (MDT) was 1.6 days. Birds that received a single in ovo vaccine dose and did not survive the challenge had an MDT of between 2.75 and 3 days, whereas those that were vaccinated at 2 weeks posthatching and did not survive the challenge had an MDT of 6 days. Interestingly, two other groups of chickens (eight/group) that were vaccinated in ovo with a single high dose of the vaccine virus and that were subsequently challenged with the HPAI H5N1 virus at either 9 weeks or 12 weeks of age showed 100% protection against challenge with no signs of disease (three times more challenge virus was used in these groups in order to compensate for differences in body weight compared to the weight of the 4-week-old birds). Only birds that died from the infection showed signs of disease; none of the survivors (vaccinated) showed overt signs of disease. With respect to virus shedding, vaccinated birds showed reductions of between 2 and >4 log10 EID50 in virus titers compared to the titers in unvaccinated birds in samples taken from tracheal swabs. The effect on the reduction of virus shedding was more evident when using samples obtained from the cloaca: only the two 4-week-old groups that received a single dose of the vaccine in ovo showed reductions in virus titers, of approximately 2 log10 EID50/ml, whereas the other vaccinated groups showed no evidence of cloacal virus shedding. It is worth mentioning that no detectable virus shedding was found in both tracheal and cloacal swab samples in the high-dose prime-boost group. Increased HI antibody titers from surviving birds at 14 days postchallenge suggested that all birds in the vaccine groups did actually respond to the challenge virus.
TABLE 5.
Protective efficacy of the live att vaccine against highly pathogenic A/VN/1203/04 (H5N1) challenge in chickensa
| Condition(s) for vaccine groupb | No. positive for virus/total no. (log10 EID50/ml ± SD)d at 3 days p.v.c | Age in wks at time of challenge | No. positive in HI test/total no. (GMT) before challenge | No. positive for virus/total no. (log10 EID50/ml ± SD)d at 2 days p.c. in:
|
No. that died/total no. (MDT in days) | No. positive in HI test/total no. (GMT) at 14 days p.c. | |
|---|---|---|---|---|---|---|---|
| Trachea | Cloaca | ||||||
| Control | NA | 4 | 0/10 | 10/10 (6.0 ± 1.0) | 10/10 (6.0 ± 0.7) | 10/10 (1.6) | NA |
| In ovo, 106, 1x | 4/10 (1.9 ± 0.3) | 4 | 6/10 (15) | 6/10 (3.5 ± 1.4) | 4/10 (4.3 ± 1.7) | 4/10 (2.75) | 6/6 (45) |
| In ovo, 104, 1x | 3/10 (0.7) | 4 | 6/10 (12) | 5/10 (3.0 ± 1.8) | 3/10 (4.0 ± 1.4) | 3/10 (3.0) | 7/7 (108) |
| In ovo, 106, 2x | 0/8e | 4 | 8/8 (10) | 0/8 | 0/8 | 0/8 | 8/8 (47) |
| In ovo, 104, 2x | 1/8 (0.7)e | 4 | 4/8 (15) | 4/8 (2.2 ± 0.4) | 0/8 | 0/8 | 8/8 (128) |
| Posthatching, 106 1x | 2/8 (1.2 ± 0.7) | 4 | 2/8 (10) | 5/8 (1.6 ± 0.8) | 0/8 | 3/8 (6.0) | 5/5 (180) |
| Control | NA | 9 | 0/8 | 8/8 (6.1 ± 0.9) | 8/8 (5.6 ± 0.7) | 8/8 (1.6) | NA |
| In ovo, 106, 1x | ND | 9 | 8/8 (18) | 4/8 (1.8 ± 0.8) | 0/8 | 0/8 | 8/8 (255) |
| Control | NA | 12 | 0/8 | 8/8 (5.5 ± 0.5) | 8/8 (5.2 ± 0.5) | 8/8 (1.6) | NA |
| In ovo, 106, 1x | ND | 12 | 6/8 (10) | 6/8 (1.9 ± 0.7) | 0/8 | 0/8 | 8/8 (840) |
p.v., postvaccination; p.c., postchallenge; NA, not available; ND, not done. GMT, geometric mean reciprocal end-point titer.
Chickens were vaccinated with 106 EID50 or 104 EID50 of virus by in ovo administration or at 2 weeks posthatching. 1x, single vaccination dose; 2x, in ovo vaccination followed by boost vaccination at 2 weeks posthatching.
Data are for tracheal swab samples. Cloacal swab samples were negative for virus.
Mean virus titer ± standard deviation. The detection limit is 0.7 log10 EID50/ml.
Data were gathered after boost vaccination.
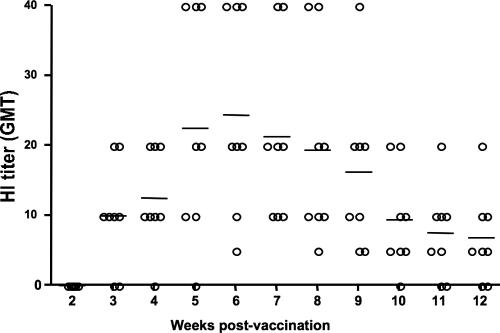
Our studies indicated that chickens that received a single high dose of the vaccine in ovo were more resistant to the HPAI challenge at 9 to 12 weeks than at 4 weeks of age. In order to better understand this effect and to determine whether it was related to the kinetics of antibody production, serum samples were randomly collected from eight of the birds on a weekly basis, and the HI antibody titers, shown in Fig. 5, were determined. Discernible antibody titers were found in six of eight birds at 3 weeks of age and reached peak titers when the birds were 6 weeks old, slowly decreasing thereafter. Our studies also showed that all the chickens that had discernible HI titers survived the challenge with the HPAI H5N1 virus; however, protection was also observed in some birds that did not show measurable seroconversion. Interestingly, since the 12-week-old chickens exhibited lower HI antibody titers than the 4-week-old chickens, the survival of older birds may not necessarily be due solely to increased neutralizing antibody titers but rather to a combined effect of humoral and cellular responses, which were functioning adequately by the time these birds were challenged.
FIG. 5.
Kinetics of HI antibody production in chickens after single-dose (106 EID50) in ovo vaccination with H5N1 live att vaccine. Eighteen-day-old embryos were vaccinated with 106 EID50 6attWF10:2H5ΔN1 virus in ovo. Sera were collected randomly from eight chickens on a weekly basis and tested for neutralizing antibodies against the A/VN/1203/04 (H5N1) virus by the HI test. GMT, geometric mean reciprocal end-point tier. Horizontal lines indicate the mean HI titer.
DISCUSSION
In this study, we tested the potential of the att viruses as a live vaccine for poultry in the LPAI and HPAI challenge models. Our studies revealed that both the H7 and H5 double-mutant att (ts plus HA tag) viruses were highly att in chickens. While the att viruses were able to replicate in the upper respiratory tracts of the birds, no virus or little virus was found in the lungs or cloaca, respectively. No evidence of transmission of the att viruses was observed in the chickens, and no virus shedding and no seroconversion were observed in the contact birds. An obvious advantage of a potential live att avian influenza vaccine is the possibility of a lower amount of virus/antigen being needed in order to provide complete protection compared to the amount of an inactivated-virus vaccine. In addition, since it is a live virus, it is expected to have less variability in terms of protective efficacy from lot to lot compared to the variations observed in the preparation of inactivated vaccines (which are usually compensated with the type and amount of adjuvant used). In the low pathogenic H7N2 challenge study, our approach appears superior compared to an H7 inactivated vaccine, which contains the equivalent of 107.0 EID50 of virus per dose and requires booster vaccination to achieve 100% protection for chickens challenged with the low pathogenic A/Turkey/VA/55/02 (H7N2) virus at dose of 105 EID50 (20). We observed that a single-immunization scheme of the live att vaccine at a dose of 5 × 103 EID50 in chickens provided full protection against infection with 5 × 105 EID50 of the Ck/04 virus. We also performed additional studies in which vaccinated birds were placed in contact with naïve birds challenged with the wild-type Ck/04 virus and a naïve uninfected control group. Under these circumstances, no evidence of transmission of the Ck/04 virus to vaccinated birds was observed by either virus isolation or increased seroconversion, whereas the virus was readily transmitted to the naïve control group (not shown).
The 6attWF10:2H5ΔN1 vaccine virus appears either more att or less immunogenic than the 6attWF10:2H7N2 counterpart, since only two out of eight birds showed HI titers when it was administered at a high dose of 106 EID50 at 2 weeks posthatching; in fact the 6attWF10:2H7N2-vaccinated birds showed measurable HI antibody titers even when the chickens received a dose of vaccine virus of just 5 × 103 EID50. Therefore, in order to maximize the humoral response against the H5 virus, we administered 6attWF10:2H5ΔN1 to 18-day-old chicken embryos in ovo. Our results show that a single dose of the vaccine in ovo induced protective immunity, which provided 100% protection against HPAI H5N1 virus challenge for chickens between 9 and 12 weeks old. The neutralizing antibody titers induced by the vaccine peaked around 6 weeks posthatching, tempting us to speculate that the chickens could be fully protected from 6 weeks old. A boost immunization at 2 weeks posthatching was required to confer 100% protection to challenge at 4 weeks old. In both our H7 and H5 vaccination studies, some of the immunized chickens did not show high levels of seroconversion, although they were fully protected against challenge. Since our approach utilizes a live att virus, it is plausible that local mucosal immunity and/or cell-mediated immunity also contribute to the protection. Coincidentally, it has been shown that a ca avian pneumovirus vaccine achieved full protection in turkeys showing very low levels of seroconversion (33).
The generation of an att avian influenza virus was based on the incorporation of ts mutations found on the PB1 and PB2 genes of the ca/ts/att influenza A/Ann Arbor/6/60 (H2N2) strain and the cloning of an HA tag in frame with the C terminus of the PB1 gene. An important distinction between avian and human influenza viruses relates to their optimal temperature of replication. While human influenza A viruses replicate in the upper respiratory tract at a temperature around 33°C, avian viruses tend to replicate in the intestinal tracts of aquatic birds at a temperature of about 41°C. It is reasonable to speculate that amino acid differences in the internal genes of avian and human influenza viruses are responsible for the optimal temperature of replication. For example, amino acid position 627 in PB2 has been shown to play a role in host range and virulence. Typical avian influenza viruses code for glutamic acid at position 627, whereas human influenza viruses and some of the most lethal forms of H5N1 viruses that have crossed to humans code for a lysine. It has been shown that glutamic acid at position 627 is also a determinant of the cold sensitivity of avian influenza viruses; i.e., it prevents them from growing at temperatures below 33°C (26, 41, 42). The avian influenza virus used in this study possesses glutamic acid at position 627 in PB2. Therefore, incorporation of the ts mutations would not necessarily imply the same level of ts phenotype for an avian influenza virus as for a human influenza virus. Thus, the nonpermissive temperature for the ca/ts/att human virus is around 38°C in MDCK cells (17), whereas for the WF10 virus, it was 39°C.
Host factors may also play a role in determining the ts phenotype, since our studies using cells of mammalian and avian origin showed differences in the abilities of our mutant viruses to form plaques and in protein synthesis. For example, the three different mutant viruses (7tsWF10:1malH7, 7tagWF10:1malH7, and 7attWF10:1malH7) exhibited more-evident ts phenotypes in mammalian cells than in chicken cells. This observation correlates with the observation that viruses containing the WF10 ts backbone are not att in chickens; however, they are substantially att in mice (M. J. Hossain, H. Song, and D. R. Perez, unpublished). Previous studies showed that the heat-shock protein of 70 kDa expressed at 41°C in MDCK cells inhibited the binding of the viral M1 protein to viral ribonucleoproteins and their subsequent nuclear export (12). The different growth characteristics of WF10 in MDCK and CEK cells may reflect distinct interaction patterns between viral proteins and host factors induced in different host cells at higher temperatures.
The incorporation of an HA tag in frame with the C terminus of PB1 provided a genetic marker to differentiate the vaccine strain from the field isolates (using real-time RT-PCR, the HA tag sequence was detected in the swab samples from the vaccinated birds but not in the birds infected by the field isolates; data not shown). The introduction of unrelated sequences into the PB1 gene did not affect the viruses’ viabilities. This is partially due to the fact that the noncoding regions and the last 12 nucleotides of both the 5′ and 3′ coding regions of the PB1 viral RNA, which have recently been shown to be sufficient for efficient incorporation of the PB1 viral RNAs (30), were not altered. It is interesting to note that the introduction of the HA tag has little attenuating effect by itself, but it acts synergistically with the four ts mutations in PB1 and PB2. Our results indicated that all the ts mutations contribute to the ts phenotype of HA-tagged viruses; among these ts mutations, 391E and 581G in PB1 are sufficient to provide the ts phenotype at the same level as in the 7attWF10:1malH7 virus. The influenza virus RNA polymerase is a heterotrimer comprising the PB1, PB2, and PA subunits; PB1 functions as the RNA polymerase catalytic subunit (3). The N-terminal region of PB1 interacts with the C-terminal region of PA, while the C-terminal region of PB1 interacts with the N-terminal region of the PB2 subunit (10, 34, 35). Further studies are needed to determine whether the incorporation of the HA tag at the C terminus of PB1 harboring the ts mutations affects the interaction with PB2, which potentially may be disrupted at higher temperatures. To determine whether the replication of the double-mutant virus in birds would result in the loss of the ts loci, the HA tag modification, or both, RT-PCR and sequencing were performed on viruses recovered from the vaccinated birds. The results from tracheal samples collected at 5 days postvaccination from all the vaccinated birds revealed the expected integrity of the ts loci and/or HA tag mutations, suggesting that the host did not induce genetic alterations in these viruses (not shown). No changes in the in vitro phenotypes of the mutant viruses, which is consistent with the results of the sequence analysis, were observed. Likewise, serial passage in eggs (10 times) of the att virus did not result in mutations at either the ts loci or the HA tag modification, and the virus maintained its expected ts-restricted phenotype in vitro. We also took advantage of the HA tag in the att virus to discriminate the vaccine virus from the wild-type virus by real-time RT-RCR (data not shown) using the specific set of primers shown in Fig. 1. Therefore, these results suggest that the att virus is genetically stable and that no revertant compensatory mutations have emerged.
Taken together, our results suggest that live att avian influenza viruses could have potential as safe live vaccines and be applied for mass vaccination using the in ovo route. The use of in ovo vaccination would also alleviate concerns regarding potential reassortment with other viral strains, since it is commonly accepted that wild-type avian influenza viruses are not usually found in commercial chicken eggs. However, since reassortment is common among influenza A viruses, particularly in avian species, additional studies are required to evaluate the reassortment potential of our live att virus with other influenza A viruses. Strategies that prevent the reassortment of the vaccine virus with other influenza viruses, particularly the reassortment of the HA gene, will facilitate the use of live influenza virus vaccines in poultry. Further studies are also needed to test other delivery routes for mass-vaccination purposes; i.e., aspersion, through drinking water, etc.
The apparent increase and recurrence of avian influenza outbreaks in poultry demands the development of alternative intervention strategies to help prevent or control the spread of the disease. When avian influenza outbreaks expand beyond the borders of one country, eradication and quarantine alone may be unsuccessful in containing the disease. This is particularly true when the neighboring countries do not posses an adequate surveillance structure capable of quickly detecting and containing the virus. The unprecedented geographic expansion of the current H5N1 situation in Asia is perhaps the best example of such an argument. An approach that would allow mass vaccination would greatly contribute to the control of avian influenza outbreaks, particularly if it is effective in many avian species. Our studies suggest that it is possible to develop live att avian influenza viruses that have vaccine potential and would be amenable for mass vaccination.
Acknowledgments
This work was supported in part by grants from NIH-NIAID (R21-AI071014) and USDA (CSREES no. 2005-35605-15388 and CSREES no. 2006-01587).
We thank Xiaoping Zhu, Hongquan Wan, Jaber Hossain, and Alicia Solorzano for helpful discussions and for critically reading the manuscript. We specifically thank Erin Sorrell and Danielle Hickman for comments and for editing the manuscript. We are indebted to Ivan Gomez Osorio for his assistance with the animal studies and Andrea Ferrero for her laboratory managerial skills. We thank Robert Webster, Ruben Donis, and Dennis Senne for providing highly valuable virus strains.
Footnotes
Published ahead of print on 27 June 2007.
REFERENCES
- 1.Ahmad, J., and J. M. Sharma. 1993. Protection against hemorrhagic enteritis and Newcastle-disease in turkeys by embryo vaccination with monovalent and bivalent vaccines. Avian Dis. 37:485-491. [PubMed] [Google Scholar]
- 2.Belshe, R. B., P. M. Mendelman, J. Treanor, J. King, W. C. Gruber, P. Piedra, D. I. Bernstein, F. G. Hayden, K. Kotloff, K. Zangwill, D. Iacuzio, and M. Wolff. 1998. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children. N. Engl. J. Med. 338:1405-1412. [DOI] [PubMed] [Google Scholar]
- 3.Biswas, S. K., and D. P. Nayak. 1994. Mutational analysis of the conserved motifs of influenza A virus polymerase basic protein 1. J. Virol. 68:1819-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Capua, I., and S. Marangon. 2004. Vaccination for avian influenza in Asia. Vaccine 22:4137-4138. [DOI] [PubMed] [Google Scholar]
- 5.Clements, M. L., R. F. Betts, and B. R. Murphy. 1984. Advantage of live attenuated cold-adapted influenza A virus over inactivated vaccine for A/Washington/80 (H3N2) wild-type virus infection. Lancet 1:705-708. [DOI] [PubMed] [Google Scholar]
- 6.Cox, N. J., F. Kitame, A. P. Kendal, H. F. Maassab, and C. Naeve. 1988. Identification of sequence changes in the cold-adapted, live attenuated influenza vaccine strain, A/Ann Arbor/6/60 (H2N2). Virology 167:554-567. [PubMed] [Google Scholar]
- 7.Cox, R. J., K. A. Brokstad, and P. Ogra. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand. J. Immunol. 59:1-15. [DOI] [PubMed] [Google Scholar]
- 8.Ellis, T. M., C. Y. Leung, M. K. Chow, L. A. Bissett, W. Wong, Y. Guan, and J. S. Malik Peiris. 2004. Vaccination of chickens against H5N1 avian influenza in the face of an outbreak interrupts virus transmission. Avian Pathol. 33:405-412. [DOI] [PubMed] [Google Scholar]
- 9.Fenner, F., D. A. Henderson, I. Arita, Z. Jezek, and I. D. Ladnyi. 1988. Smallpox and its eradication. World Health Organization, Geneva, Switzerland. http://whqlibdoc.who.int/smallpox/9241561106.pdf.
- 10.Gonzalez, S., T. Zurcher, and J. Ortin. 1996. Identification of two separate domains in the influenza virus PB1 protein involved in the interaction with the PB2 and PA subunits: a model for the viral RNA polymerase structure. Nucleic Acids Res. 24:4456-4463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hierholzer, J. C., and R. A. Killington. 1996. Virus isolation and quantitation, pp. 25-46. In B.W. Mahy and H. I. Kangro (ed.), Virology methods manual. Academic Press, London, United Kingdom.
- 12.Hirayama, E., H. Atagi, A. Hiraki, and J. Kim. 2004. Heat shock protein 70 is related to thermal inhibition of nuclear export of the influenza virus ribonucleoprotein complex. J. Virol. 78:1263-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann, E., S. Krauss, D. Perez, R. Webby, and R. G. Webster. 2002. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 20:3165-3170. [DOI] [PubMed] [Google Scholar]
- 15.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 16.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18-24. [DOI] [PubMed] [Google Scholar]
- 17.Jin, H., H. Zhou, B. Lu, and G. Kemble. 2004. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J. Virol. 78:995-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.King, J. C., Jr., R. Lagos, D. I. Bernstein, P. A. Piedra, K. Kotloff, M. Bryant, I. Cho, and R. B. Belshe. 1998. Safety and immunogenicity of low and high doses of trivalent live cold-adapted influenza vaccine administered intranasally as drops or spray to healthy children. J. Infect. Dis. 177:1394-1397. [DOI] [PubMed] [Google Scholar]
- 19.Lee, C. W., D. A. Senne, and D. L. Suarez. 2004. Effect of vaccine use in the evolution of Mexican lineage H5N2 avian influenza virus. J. Virol. 78:8372-8381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee, C. W., D. A. Senne, and D. L. Suarez. 2004. Generation of reassortant influenza vaccines by reverse genetics that allows utilization of a DIVA (differentiating infected from vaccinated animals) strategy for the control of avian influenza. Vaccine 22:3175-3181. [DOI] [PubMed] [Google Scholar]
- 21.Lipatov, A. S., E. A. Govorkova, R. J. Webby, H. Ozaki, M. Peiris, Y. Guan, L. Poon, and R. G. Webster. 2004. Influenza: emergence and control. J. Virol. 78:8951-8959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maassab, H. F. 1969. Biologic and immunologic characteristics of cold-adapted influenza virus. J. Immunol. 102:728-732. [PubMed] [Google Scholar]
- 23.Maassab, H. F., A. P. Kendal, G. D. Abrams, and A. S. Monto. 1982. Evaluation of a cold-recombinant influenza virus vaccine in ferrets. J. Infect. Dis. 146:780-790. [DOI] [PubMed] [Google Scholar]
- 24.Macadam, A. J., G. Ferguson, D. M. Stone, J. Meredith, S. Knowlson, G. Auda, J. W. Almond, and P. D. Minor. 2006. Rational design of genetically stable, live-attenuated poliovirus vaccines of all three serotypes: relevance to poliomyelitis eradication. J. Virol. 80:8653-8663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marangon, S., and I. Capua. 2006. Control of avian influenza in Italy: from stamping out to emergency and prophylactic vaccination. Dev. Biol. (Basel) 124:109-115. [PubMed] [Google Scholar]
- 26.Massin, P., S. van der Werf, and N. Naffakh. 2001. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J. Virol. 75:5398-5404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meadows, M. 2003. Nasal flu vaccine approved. FDA Consum. 37:27. [PubMed] [Google Scholar]
- 28.Mendelman, P. M., J. Cordova, and I. Cho. 2001. Safety, efficacy and effectiveness of the influenza virus vaccine, trivalent, types A and B, live, cold-adapted (CAIV-T) in healthy children and healthy adults. Vaccine 19:2221-2226. [DOI] [PubMed] [Google Scholar]
- 29.Muller, H., M. R. Islam, and R. Raue. 2003. Research on infectious bursal disease—the past, the present and the future. Vet. Microbiol. 97:153-165. [DOI] [PubMed] [Google Scholar]
- 30.Muramoto, Y., A. Takada, K. Fujii, T. Noda, K. Iwatsuki-Horimoto, S. Watanabe, T. Horimoto, H. Kida, and Y. Kawaoka. 2006. Hierarchy among viral RNA (vRNA) segments in their role in vRNA incorporation into influenza A virions. J. Virol. 80:2318-2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nair, V. 2004. Successful control of Marek's disease by vaccination. Dev. Biol. (Basel) 119:147-154. [PubMed] [Google Scholar]
- 32.Paillot, R., D. Hannant, J. H. Kydd, and J. M. Daly. 2006. Vaccination against equine influenza: quid novi? Vaccine 24:4047-4061. [DOI] [PubMed] [Google Scholar]
- 33.Patnayak, D. P., B. R. Gulati, A. M. Sheikh, and S. M. Goyal. 2003. Cold adapted avian pneumovirus for use as live, attenuated vaccine in turkeys. Vaccine 21:1371-1374. [DOI] [PubMed] [Google Scholar]
- 34.Perez, D. R., and R. O. Donis. 1995. A 48-amino-acid region of influenza A virus PB1 protein is sufficient for complex formation with PA. J. Virol. 69:6932-6939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perez, D. R., and R. O. Donis. 2001. Functional analysis of PA binding by influenza A virus PB1: effects on polymerase activity and viral infectivity. J. Virol. 75:8127-8136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perez, D. R., R. J. Webby, E. Hoffmann, and R. G. Webster. 2003. Land-based birds as potential disseminators of avian mammalian reassortant influenza A viruses. Avian Dis. 47:1114-1117. [DOI] [PubMed] [Google Scholar]
- 37.Roeder, P. L., J. Lubroth, and W. P. Taylor. 2004. Experience with eradicating rinderpest by vaccination. Dev. Biol. (Basel) 119:73-91. [PubMed] [Google Scholar]
- 38.Savill, N. J., S. G. St. Rose, M. J. Keeling, and M. E. Woolhouse. 2006. Silent spread of H5N1 in vaccinated poultry. Nature 442:757. [DOI] [PubMed] [Google Scholar]
- 39.Senne, D. A., D. J. King, and D. R. Kapczynski. 2004. Control of Newcastle disease by vaccination. Dev. Biol. (Basel) 119:165-170. [PubMed] [Google Scholar]
- 40.Sharma, J. M., and B. R. Burmester. 1982. Resistance to Mareks disease at hatching in chickens vaccinated as embryos with the turkey herpesvirus. Avian Dis. 26:134-149. [PubMed] [Google Scholar]
- 41.Shinya, K., S. Hamm, M. Hatta, H. Ito, T. Ito, and Y. Kawaoka. 2004. PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology 320:258-266. [DOI] [PubMed] [Google Scholar]
- 42.Subbarao, E. K., W. London, and B. R. Murphy. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugimura, T., Y. Murakami, and T. Ogawa. 2000. The susceptibility of culture cells to avian influenza viruses. J. Vet. Med. Sci. 62:659-660. [DOI] [PubMed] [Google Scholar]
- 44.Swayne, D. E., J. R. Beck, and N. Kinney. 2000. Failure of a recombinant fowlpoxvirus vaccine containing an avian influenza hemagglutinin gene to provide consistent protection against influenza in chickens preimmunized with a fowl pox vaccine. Avian Dis. 44:132-137. [PubMed] [Google Scholar]
- 45.Toro, H., D. C. Tang, D. L. Suarez, M. J. Sylte, J. Pfeiffer, and K. R. Van Kampen. 2007. Protective avian influenza in ovo vaccination with non-replicating human adenovirus vector. Vaccine 25:2886-2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Townsend, H. G., S. J. Penner, T. C. Watts, A. Cook, J. Bogdan, D. M. Haines, S. Griffin, T. Chambers, R. E. Holland, P. Whitaker-Dowling, J. S. Youngner, and R. W. Sebring. 2001. Efficacy of a cold-adapted, intranasal, equine influenza vaccine: challenge trials. Equine Vet. J. 33:637-643. [DOI] [PubMed] [Google Scholar]
- 47.Veits, J., D. Luschow, K. Kindermann, O. Werner, J. P. Teifke, T. C. Mettenleiter, and W. Fuchs. 2003. Deletion of the non-essential UL0 gene of infectious laryngotracheitis (ILT) virus leads to attenuation in chickens, and UL0 mutants expressing influenza virus haemagglutinin (H7) protect against ILT and fowl plague. J. Gen. Virol. 84:3343-3352. [DOI] [PubMed] [Google Scholar]
- 48.Wareing, M. D., and G. A. Tannock. 2001. Live attenuated vaccines against influenza; an historical review. Vaccine 19:3320-3330. [DOI] [PubMed] [Google Scholar]