Abstract
There is an urgent need for an efficacious vaccine against tuberculosis (TB). Cellular immune responses are key to an effective protective response against TB. Recombinant adenovirus (rAd) vectors are especially suited to the induction of strong T-cell immunity and thus represent promising vaccine vehicles for the prevention of TB. We have previously reported on rAd vector serotype 35, the serotype of choice due to low preexisting immunity worldwide, which expresses a unique fusion protein of Mycobacterium tuberculosis antigens Ag85A, Ag85B, and TB10.4 (Ad35-TBS). Here, we demonstrate that Ad35-TBS confers protection against M. tuberculosis when administered to mice through either an intranasal or an intramuscular route. Histological evaluation of lung tissue corroborated the protection and, in addition, demonstrated differences between two mouse strains, with diffuse inflammation in BALB/c mice and distinct granuloma formation in C57BL/6 mice. Epitope mapping analysis in these mouse strains showed that the major T-cell epitopes are conserved in the artificial fusion protein, while three novel CD8 peptides were discovered. Using a defined set of T-cell epitopes, we reveal differences between the two mouse strains in the type of protective immune response, demonstrating that different antigen-specific gamma interferon (IFN-γ)-producing T cells can provide protection against M. tuberculosis challenge. While in BALB/c (H-2d) mice, a dominant CD8 T-cell response was detected, in C57BL/6 (H-2b) mice, more balanced CD4/CD8 T-cell responses were observed, with a more pronounced CD4 response in the lungs. These results unify conflicting reports on the relative importance of CD4 versus CD8 T-cell responses in protection and emphasize the key role of IFN-γ.
Tuberculosis (TB), an airborne disease caused by Mycobacterium tuberculosis, is responsible for 2 million deaths each year, with more than 90% of cases occurring in developing countries. It has been estimated that one-third of the world population is infected with M. tuberculosis, and about 5 to 10% of the infected individuals will develop TB during their lifetime. The increasing global impact of TB has been linked to growing poverty, increased emigration, deterioration of public health care, the spread of human immunodeficiency virus, and the development of multidrug-resistant strains of M. tuberculosis. Bacille Calmette-Guérin (BCG), a live and attenuated strain of Mycobacterium bovis, is the only available vaccine against TB to date and has been used for the vaccination of newborns for decades. The vaccine is effective in preventing serious complications of childhood TB, but its efficacy wanes over a period of 10 to 15 years, rendering adolescents increasingly susceptible to pulmonary TB. Significant efforts are being made to generate a more effective TB vaccine (3, 24, 50), and vaccination regimens aimed to improve BCG-induced protection are currently the most favorable approach (4, 14, 19, 21, 29, 36). The most promising antigens for vaccine generation include proteins of the Ag85 mycolyl transferase complex and members of the ESAT family (37, 38). These secreted antigens proved to be immunogenic in humans and are able to induce protective immunity in animal models, as was demonstrated with recombinant BCG (21), a DNA vaccine (23), purified proteins (11, 22), and recombinant viral vectors (29, 36, 48, 51).
The exact correlates of protection against TB are not yet fully understood. However, experimental evidence that has accumulated over recent years supports the idea that gamma interferon (IFN-γ)-producing cells play a key role in protection against challenge with M. tuberculosis (32, 42). Replication-deficient (E1-deleted) adenovectors are particularly suited for the induction of insert-specific cellular immunity and, as such, are being considered as promising vaccine vectors for the prevention of infectious diseases (1, 5, 34, 35, 39, 46). In addition, an efficient manufacturing technology has been developed for adenovector-based vaccines (15), enabling the production of millions of vaccine dosages required for vaccination against infectious diseases such as TB, malaria, and AIDS. Natural infection with wild-type adenoviruses (Ads) does pose a problem for vaccines based on highly prevalent serotypes such as Ad type 5 (Ad5) due to the induction of neutralizing antibodies that are able to blunt the efficacy of the vaccine (27, 40). Ad35 has the advantage of a low prevalence of preexisting immunity worldwide, which, if present at all, is accompanied by low neutralizing antibody titers (25, 43, 45). Additionally, the immunogenicity and the protective potential of Ad35 is not hampered by preexisting immunity against the most commonly encountered Ad5 serotype (2, 33). Recent studies have demonstrated that a single vaccination with an Ad35 vector induces only a low level of neutralizing antibodies against Ad35 in nonhuman primates (30), which opens up possibilities for homologous Ad35 prime-boost immunization regimens in the human population.
With the aim of generating a vaccine against TB, we have produced Ad35-TBS, a recombinant Ad35 vector expressing the M. tuberculosis antigens Ag85A, Ag85B, and TB10.4 (a member of ESAT family) arranged in the vector as a single fusion protein (17). This fusion protein encoded by recombinant Ad35 (rAd35) is efficiently expressed and induces T-cell responses against individual antigens either as a stand-alone vaccine (17) or following a BCG prime (36). It is expected that the presence of multiple antigens in a single vaccine will provide a large array of epitopes, which is essential for the broad coverage of heterogeneous HLA haplotypes present in human populations.
In this study, we have characterized Ad35-TBS vector-induced immune responses regarding the type and specificity of IFN-γ-producing T cells in mice of two different haplotypes (H-2d and H-2b). The protective potential of the vaccine, administered either intranasally (i.n.) or intramuscularly (i.m.), was determined in a mouse M. tuberculosis challenge model.
MATERIALS AND METHODS
Recombinant Ad35-TBS.
The generation of a recombinant Ad35 vector expressing TB antigens Ag85A, Ag85B, and TB10.4 as a single fusion protein (Ad35-TBS) has been described previously (17). Briefly, PER.C6 cells were cotransfected with an adaptor pAdApt35Bsu plasmid containing the TBS insert in the former E1 region and plasmids containing the remaining viral genome, all predigested with appropriate enzymes to liberate the Ad sequences from the plasmid backbone. Viruses were plaque purified and propagated on adherent T-cell cultures. Purified stocks were obtained using standard CsCl gradient centrifugation and, upon dialysis, were formulated in phosphate-buffered saline-5% sucrose.
Mice.
Six- to eight-week-old female BALB/c (H-2d) and C57BL/6 (H-2b) mice were purchased from Harlan (Zeist, The Netherlands) and Charles River (Maastricht, The Netherlands) and kept at the institutional animal facility under specific-pathogen-free conditions during the experiment. Mycobacterium challenge experiments were performed at the Animal Facility of the Amsterdam Medical Center. Institutional committees for animal care and use reviewed and approved the mouse experiments.
Immunization and T-cell assays.
In a dose-finding study, mice were injected intramuscularly (i.m.) with 107 to 1010 viral particles (VP) of Ad35-TBS or 1010 VP of Ad35-E (adenovector without transgene). Two weeks after the immunization, the antigen-specific T-cell response was determined using intracellular cytokine staining (ICS) specific for IFN-γ. T-cell epitope mapping experiments were performed 2 weeks after i.m. injection with 109 VP of Ad35-TBS (n = 5) or Ad35-E (n = 3). The protective immune response was evaluated in mice vaccinated i.m. or i.n. with 109 VP of Ad35-TBS 6 weeks after the vaccination.
For i.m. immunization, mice received the required vector dose in a total volume of 100 μl (50 μl/hind leg); for i.n. immunization, the total volume was 20 μl (10 μl per nostril). Mycobacterium bovis BCG Danish SSI-1331 (BCG preclinical research standard; CBER/FDA) was diluted in diluent for the BCG preclinical research standard (CBER/FDA) and administered subcutaneously (s.c.) in the neck at a dose of 6 × 105 CFU in a total volume of 200 μl.
For pentamer staining, performed as described previously (27), mice were bled using a tail cut with intervals of 5 to 7 days until 4 weeks postimmunization.
Two weeks (dose finding and epitope mapping) or 6 weeks (protective immune response) after the immunization, animals were sacrificed, and organs (spleens and lungs) were collected to serve as a source of cells for immunological assays. Splenocytes were isolated as described previously (17). In order to isolate lung mononuclear cells, lungs were perfused in situ with 4 ml warm phosphate-buffered saline through the right ventricle of the heart. The lung tissue was cut into small pieces, subjected to collagenase type 1 (150 U/ml) digestion for 1 h at 37°C, and minced through a 70-μm Falcon cell strainer using a 5-ml syringe plunger. Upon lysis of red blood cells in ACK lysing buffer (Invitrogen, Carlsbad, CA), lung cells were washed in R10 medium and passed through a 30-μm preseparation filter (Miltenyi Biotec, Auburn, CA).
The immune responses were determined using ICS or an enzyme-linked immunospot (ELISPOT) assay as described previously (17, 27). For epitope mapping, splenocytes were pooled per group, while for the immunogenicity evaluation, mice were assessed individually.
Peptides used for in vitro stimulation were purchased from ADI (San Antonio, TX), SynPep Corp. (Dublin, CA), and Pepscan Systems (Lelystad, The Netherlands). The Ag85-specific H-2d pentamer was purchased from ProImmune Ltd. (Oxford, United Kingdom).
Experimental infection and readout.
A vial of M. tuberculosis strain Erdman (M. tuberculosis preclinical research standard; CBER/FDA) was thawed and diluted in sterile 0.9% NaCl. The lung infection was induced as described previously (26, 49). Briefly, mice were anesthetized by inhalation with isoflurane (Abott Laboratories Ltd., Kent, United Kingdom) and inoculated i.n. with M. tuberculosis in 50 μl saline at a dose generating ±150 CFU per lung 1 day after the inoculation (optimal challenge dose as determined in pilot experiments) (data not shown). Six weeks after the inoculation, mice were sacrificed, and lung, spleen, and part of the liver were removed aseptically, weighed, and homogenized in 5 volumes of sterile 0.9% NaCl. Tenfold dilutions were plated onto Middlebrook 7H11 agar plates to determine bacterial loads. Plates were incubated for 3 weeks at 37°C, and the colonies were counted. The CFU are expressed per organ (lung and spleen) or per gram tissue (liver).
For the protection experiments, mice were immunized with 109 VP of Ad35-TBS i.n. or i.m. The positive control group received 6 × 105 CFU BCG s.c., while the negative control group was left untreated (naïve). Mice that received 109 VP of Ad35-E i.n. or i.m were used as additional negative control groups. Results obtained with these mice were comparable to results obtained with naïve mice (data not shown). Six weeks after the immunization, groups of mice (eight mice per group) were sacrificed in order to determine the immune status of the animals, and other groups (17 mice per group) were challenged by an i.n. administration of virulent M. tuberculosis. The next day, two mice of each challenged group were sacrificed, and bacterial counts in the lungs were determined in order to confirm the challenge dose (data not shown). Six weeks after the challenge, the remaining mice (15 per group) were sacrificed, and lungs, spleens, and livers were collected for the quantification of bacterial load (CFU) and histopathological examination (lungs only).
Histological evaluation.
Lungs were harvested for histological evaluation 6 weeks after M. tuberculosis infection, fixed in 10% buffered formalin, and embedded in paraffin. Sections of 4 μm were stained with hematoxylin and eosin and analyzed by a pathologist who was blinded for the treatment allocation. To score lung inflammation and damage, the entire lung section was analyzed with respect to the following parameters: interstitial inflammation, endothelialitis, bronchitis, granuloma formation, edema, and pleuritis. Each parameter was graded on a scale from 0 to 4, with 0 being absent, 1 being mild, 2 being moderate, 3 being severe, and 4 being very severe. The cumulative inflammation score was expressed as the sum of the scores for each parameter, with the maximum being 24. Confluent (diffuse) inflammatory infiltrate was quantified separately and expressed as a percentage of the lung surface.
Statistical analysis.
Statistical analysis was performed using the Student t test on log10-transformed CFU counts and nontransformed histological scores. The difference was considered significant when the P value was <0.05.
RESULTS
Vector dose finding.
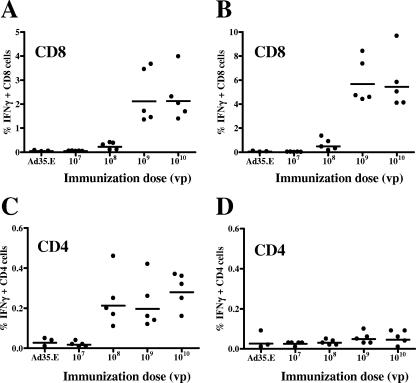
In order to determine the optimal vector dose for the follow-up epitope mapping and challenge experiments, we immunized mice with increasing doses of Ad35-TBS (107 to 1010 VP) and analyzed the immune response using ICS 2 weeks after immunization. The results obtained for C57BL/6 mice are shown in Fig. 1. The figure demonstrates a strong vector dose-dependent CD8 T-cell response to Ag85 (Fig. 1A) and TB10.4 (Fig. 1B), while a significant CD4 T-cell response was detected for Ag85 (Fig. 1C) but not for TB10.4 (Fig. 1D). The peptide pool for Ag85B was not included in this analysis since in previous experiments we found similar responses obtained upon stimulation with Ag85A or Ag85B total pools (17). As can be seen in Fig. 1, CD4 responses were detected at an immunization dose of 108 VP, while 109 VP was the optimal dose for inducing the CD8 responses. Although antigen-specific CD4 cells were detected at a lower vaccination dose than antigen-specific CD8 cells, the ICS method seemed to be more robust for the detection of CD8 than for the detection of CD4 responses, with a relatively lower percentage of IFN-γ-positive CD4 cells seen in the flow cytometric experiments.
FIG. 1.
Immunogenicity of Ad35-TBS. Groups of C57BL/6 mice were immunized i.m. with 107 to 1010 VP of Ad35-TBS (five mice per group) or 1010 VP of Ad35-E (control) (three mice per group). Two weeks after immunization, the antigen-specific T-cell response was determined using ICS upon an in vitro stimulation of splenocytes with the peptide pools covering the whole sequence of Ag85A or TB10.4. The percentages of antigen-specific IFN-γ-positive CD8 and CD4 cells are shown for Ag85A (A and C) and TB10.4 (B and D). Bars represent geometric means.
A similar dose-response dependence was found for BALB/c mice (data not shown). However, for this mouse strain, we could not detect significant CD4 responses using the 15-mer peptide pools for the in vitro stimulation of splenocytes.
Based on these results, we have selected the vector dose of 109 VP for the subsequent epitope mapping and challenge experiments.
T-cell epitope mapping.
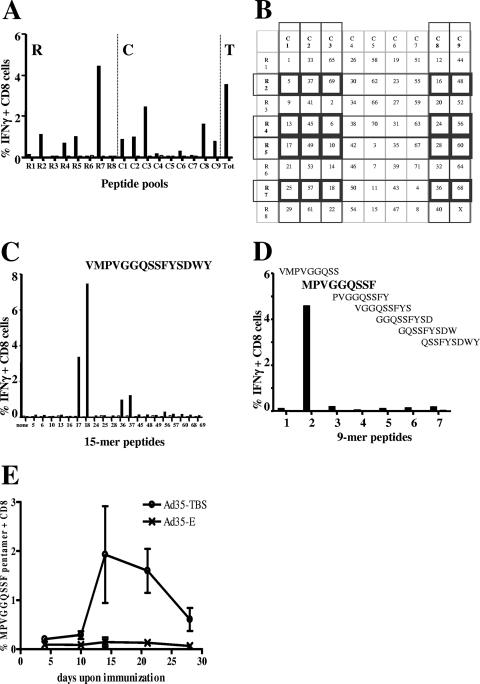
The Ad35-TBS vaccine encodes a fusion protein comprised of three different M. tuberculosis antigens (17). In order to confirm that the major known T-cell epitopes are retained in this artificial fusion molecule and to generate tools to characterize the immune response in more detail in follow-up studies, we have performed extensive epitope mapping using an optimized flow cytometric method (20, 44). The method is based on the intracellular IFN-γ staining in combination with surface staining for CD4 and CD8 markers. This method enables the identification of an immunodominant peptide(s) among a pool of overlapping peptides (15-mer peptides with 10 or 11 amino acids overlapping sequences) covering the whole protein sequence using a peptide matrix. The peptide matrix mapping approach is illustrated in Fig. 2, with an example of identification of the Ag85 CD8 epitope MPVGGQSSF in the BALB/c mouse strain. For peptide matrix mapping, individual peptides (numbers starting from 1 on) are arranged in wells of a multiwell plate in an ordered fashion (no peptides with overlapping sequences were in the same row or in the same column) and subsequently pooled in small row (R) and column (C) peptide pools. Thus, each individual peptide is present in two independent pools: one R and one C pool. Upon immunization, splenocytes are stimulated with row and column pools, and the pools inducing T-cell response are subsequently identified. The identification of the R and C peptide pools that contain a reactive peptide(s) (Fig. 2A) enables the identification of wells containing individual potentially reactive 15-mer peptides (intersection of the positive R pool and the positive C pool in the peptide array matrix) (Fig. 2B). In the second immunization experiment, the reactive 15-mer peptide is identified among potentially reactive peptides (Fig. 2C). Based on the sequence of the reactive 15-mer peptide, the overlapping 9-mer peptides (9-mer peptides with 8 amino acids overlapping sequences, covering the whole sequence of the 15-mer peptide) are generated and tested in the third immunization experiment to map the epitope (Fig. 2D). The identified 9-mer epitope can be used to generate antigen- and haplotype-specific tetramers or pentamers, which enables live monitoring of the immune response in individual mice (Fig. 2E).
FIG. 2.
Identification of an Ag85-specific T-cell epitope as an example of the epitope mapping procedure. Groups of BALB/c mice were immunized with 109 VP of Ad35-TBS (five mice per group) or Ad35-E (three mice per group) (control). Two weeks after immunization, the T-cell immune response was determined using ICS upon an in vitro stimulation of splenocytes with the small 15-mer peptide pools (A). Possibly reactive peptides were identified as the intersection of positive R and C pools (B) and used for in vitro stimulation in the follow-up experiment (C). From the identified positive peptide, overlapping 9-mer peptides were generated, covering the whole sequence, and used for in vitro stimulation in the follow-up experiment (D). The identification of the positive 9-mer peptide enables the generation of a specific pentamer, which makes it possible to monitor the development of an immune response in the blood in time (E). Black bars represent results obtained with the pooled splenocytes of Ad35-TBS-immunized mice, while white bars indicate the background levels measured with splenocytes from Ad35-E (control)-immunized mice. Bars in E represent standard errors of the means. T, total pool.
We applied this method to identify T-cell epitopes in mice of two different haplotypes: BALB/c (H-2d) and C57BL/6 (H-2b). A number of immunodominant T-cell epitopes in TB proteins encoded by Ad35-TBS were identified for both mouse strains (summarized in Table 1). The majority of epitopes that we identified had been reported previously in studies employing a single protein or DNA immunization (9, 13, 28, 41, 52). Our findings thus confirm that Ad35-TBS induces responses to epitopes present in native proteins. Besides confirming the established epitopes, we have identified novel CD8-specific peptides in C57BL/6 mice for antigens Ag85 (two overlapping 15-mer peptides covering amino acids 1 to 19) (p1-19) and TB10.4 (epitope p4-12 and peptide p73-87). In contrast to C57BL/6 mice, we could not detect any CD4 epitope in BALB/c mice using 15-mer peptides. We could, however, confirm CD4 reactivity upon stimulation with the Ag85A 20-mer peptide LTSELPGWLQANRHVKPTGS (amino acids 101 to 120), previously reported as being positive (48), with about 0.2% IFN-γ-positive CD4 cells detected in spleens of Ad35-TBS-immunized mice.
TABLE 1.
Specific T-cell peptides identified using an epitope mapping approach
| Strain | Antigen | Epitope type | % Positive cells (avg ± SD) | Amino acid position | Amino acid sequence (reference[s]) |
|---|---|---|---|---|---|
| BALB/c (H-2d) | Ag85A/B | CD8 | 3.96 ± 1.46 | 70-78 | MPVGGQSSF (9, 13, 28) |
| Ag85A | CD8 | 0.92 ± 0.47 | 144-152 | VYAGAMSGL (9) | |
| Ag85B | CD8 | 0.90 ± 0.70 | 141-159 | IYAGSLSAL (13) | |
| Ag85B | CD8 | 1.78 ± 0.73 | 151-165 | ALLDPSQGMGPSLIG (9, 13) | |
| TB10.4 | CD8 | 2.42 ± 0.41 | 20-28 | GYAGTLQSL (28) | |
| C57BL/6 (H-2b) | Ag85A/B | CD8 | 2.69 ± 1.39 | 1-19 | FSRPGLPVEYLQVPSPSMGa |
| Ag85A | CD4 | 0.15 | 241-255 | QDAYNAGGGHNGVFD (13, 41, 52) | |
| Ag85A | CD4 | 0.18 ± 0.07 | 261-279 | THSWEYWGAQLNAMKPDLQ (13, 41, 52)a | |
| Ag85B | CD4 | 0.16 | 241-255 | QDAYNAAGGHNAVFN (13, 41, 52) | |
| Ag85B | CD4 | 0.16 ± 0.04 | 261-280 | THSWEYWGAQLNAMKGDLQS (13, 41, 52)a | |
| TB10.4 | CD8 | 4.98 ± 0.84 | 4-12 | IMYNYPAML | |
| TB10.4 | CD8 | 4.13 ± 1.84 | 73-87 | SSTHEANTMAMMARD |
Sequence covered by two positive overlapping 15-mer peptides. Smaller epitopes are not identified.
Selected identified epitopes and the 20-mer peptide were used as a tool for the characterization of the immune response in the challenge experiments.
Protective ability of Ad35-TBS.
In order to determine the protective efficacy of Ad35-TBS, mice were immunized either i.n. or i.m. and challenged with a virulent M. tuberculosis strain. In the epitope mapping experiments, we observed differences in the types of responses mounted by mice of different haplotypes. To correlate the immune responses with protection, we included both mouse strains in the challenge experiments.
The results of the CFU counts in different organs are presented in Table 2. In naïve mice, M. tuberculosis counts were around 106 CFU in the lungs of both mouse strains, while the counts in spleen and liver were 10- to 100-fold lower. The BCG vaccination, given as a control vaccination, decreased the CFU counts by 0.7 to 1.2 log10 units in different organs. These findings are in agreement with previously published results. In BALB/c mice, immunization with Ad35-TBS using the i.n. route (P < 0.05) but not the i.m. route (P > 0.05) provided significant protection against M. tuberculosis, which is in agreement with the results obtained previously by others using Ad5-Ag85A (48). In C57BL/5 mice, however, both routes of immunization conferred statistically significant protection (P < 0.05). In both mouse strains, both routes of immunization were highly efficient in providing protection against dissemination of M. tuberculosis from lung to spleen and liver.
TABLE 2.
CFU counts in different organs
| Group | Mean log CFU (95% CI)a
|
||
|---|---|---|---|
| Lung | Spleen | Liver/g | |
| BALB/c | |||
| Naive (control) | 6.05 (5.82-6.28) | 5.37 (5.22-5.52) | 3.78 (3.51-4.06) |
| Ad35-TBS i.n. | 5.62 (5.34-5.90)* | 4.73 (4.49-4.98)*** | 2.62 (2.35-2.88)**** |
| Ad35-TBS i.m. | 5.85 (5.70-5.99) | 3.98 (3.82-4.14)**** | 3.13 (2.97-3.30)*** |
| BCG s.c. | 5.37 (5.10-5.64)** | 4.59 (4.37-4.80)**** | 2.72 (2.49-2.96)**** |
| C57BL/6 | |||
| Naive (control) | 6.21 (6.07-6.34) | 4.88 (4.77-4.99) | 4.05 (3.86-4.24) |
| Ad35-TBS i.n. | 5.82 (5.58-6.06)* | 4.45 (4.29-4.60)**** | 3.45 (3.17-3.73)** |
| Ad35-TBS i.m. | 5.99 (5.85-6.14)* | 4.34 (3.95-4.74)* | 3.63 (3.44-3.81)** |
| BCG s.c. | 5.37 (5.22-5.53)**** | 4.24 (4.02-4.46)**** | 2.81 (2.56-3.06)**** |
CI, confidence interval. ****, P < 0.0001; ***, P < 0.0005; **, P < 0.005; *, P < 0.05.
Histological evaluation.
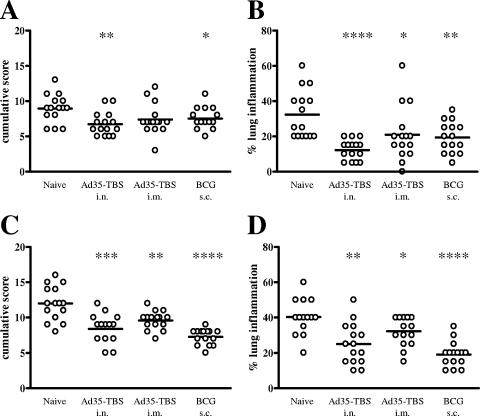
The protection, as determined by CFU, was corroborated by a microscopic examination of lung tissue from the challenged mice. In Fig. 3, the histopathologic scores and the degrees of lung inflammation are shown for all groups. Vaccination with Ad35-TBS significantly decreased the cumulative histopathological score of all animals, except for the i.m. immunized BALB/c mice, which corresponds to the CFU counts. In all vaccinated groups, the degree of inflammation was significantly decreased compared to naïve (nonvaccinated) animals.
FIG. 3.
Histological evaluation. The cumulative inflammation score (A and C) and the percentage of lung inflammation (B and D) were determined for BALB/c (A and B) and C57BL/6 (C and D) mice 6 weeks after challenge. Bars represent means. ****, P < 0.0001; ***, P < 0.0005; **, P < 0.005; *, P < 0.05.
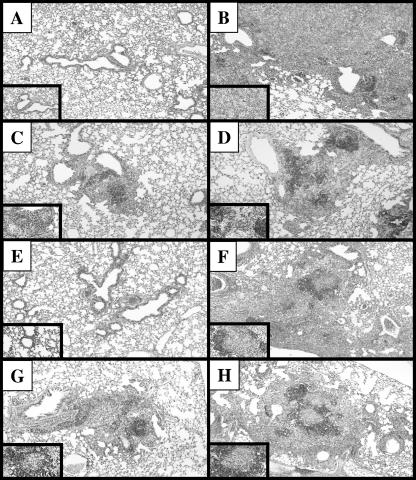
In Fig. 4, representative microscopic images of lungs are shown for a healthy mouse (Fig. 4A and E), naïve mice (Fig. 4B and F), i.n. (Fig. 4C and G) and i.m. (Fig. 4D and H) immunized mice, and challenged BALB/c (Fig. 4A to D) and C57BL/6 mice (Fig. 4E to H). It is clear that the two mouse strains exhibit different histopathologies upon M. tuberculosis challenge. BALB/c mice show diffuse inflammation throughout the lung tissue, with numerous macrophages and mononuclear cells (Fig. 4B), whereas in C57BL/6 mice distinct granuloma formation can be observed (Fig. 4F), with a rim of mononuclear cells surrounding macrophage-rich islands. Vaccination with Ad35-TBS, either i.n. or i.m., led to an improved lung histology in both strains compared to nonvaccinated animals. Again, C57BL/6 mice exhibited more pronounced granulomas than BALB/c mice.
FIG. 4.
Histopathology of the lungs. The representative microscopic images of lungs from an untreated mouse (control) (A and E), a nonvaccinated challenged mouse (naïve) (B and F), an Ad35-TBS i.n. vaccinated challenged mouse (C and G), and an Ad35-TBS i.m. vaccinated challenged mouse (D and H) are shown for BALB/c (A to D) and C57BL/6 (E to H) mouse lines. Inserts show a part of the lung at a higher magnification (×20).
The histological evaluation thus confirmed that the Ad35-based TB vaccine candidate Ad35-TBS affords protection against M. tuberculosis infection.
Immune status of animals at the time of challenge.
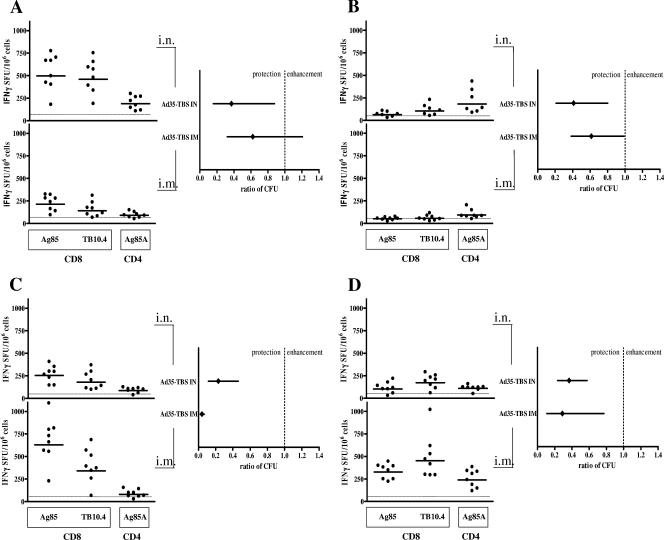
In order to determine the immune status of animals at the time of challenge (6 weeks after the immunization), we have analyzed the immune responses induced with Ad35-TBS both in lung and spleen. As a readout, we performed an ELISPOT assay upon in vitro stimulation with Ag85- or TB10.4-specific CD4 and CD8 peptides identified in the epitope mapping experiments (Table 1). For BALB/c mice, we selected the following peptides for the stimulation: the dominant CD8 epitope amino acids 70 to 78 for Ag85 and the CD8 epitope amino acids 20 to 28 for TB10.4. Since no positive CD4 15-mer peptide was identified for Ag85A, we used the CD4 20-mer epitope, previously reported to be positive (48) and confirmed to be positive in our experiments. For the C57BL/6 mice, we selected the following peptides: two overlapping 15-mer peptides covering amino acids 1 to 19 (CD8-specific peptides) and a mix of four peptides (amino acids 241 to 255 and 261 to 280) (CD4-specific peptides) for Ag85 and the CD8 epitope amino acids 4 to 12 for TB10.4. It should be noted that by excluding subdominant Ag85 CD8 epitopes for BALB/c mice and the alternative CD8 TB10.4 epitope for C57BL/6 mice, the total TB-specific CD8 responses might have been underestimated in both strains. The immune response induced in the lung upon an immunization with Ad35-TBS is presented in Fig. 5A (for BALB/c mice) and B (for C57BL/6 mice), with the upper left graph showing the response upon i.n. immunization and the lower left graph showing the response upon i.m. immunization. The response measured upon the in vitro stimulation of splenocytes is depicted in Fig. 5C (for BALB/c mice) and D (for C57BL/6 mice). To facilitate visual comparisons between immunogenicity and protection, we expressed protection as the ratio of CFU counts from the immunized versus naïve mice with 95% confidence intervals (Fig. 5C, right).
FIG. 5.
Immune status of animals at the time of challenge. Six weeks after the immunization with 109 VP of Ad35-TBS, the antigen-specific CD8 and CD4 T-cell responses were determined using ELISPOT upon an in vitro stimulation of lung cells (A and B) and splenocytes (C and D) of BALB/c (A and C) and C57BL/6 (B and D) mice. The results obtained upon i.n. immunization are shown in upper left panels, and those obtained upon i.m. immunization are shown in lower left panels. The corresponding protection, expressed as the ratio of CFU of vaccinated to CFU of naïve mice, is shown in the right panels. Bars in the left panels represent geometric means, and bars in the right panels show 95% confidence intervals of the mean values (diamonds). Dashed lines indicate the background levels in the ELISPOT assay. SFU, spot-forming units.
As can be seen in Fig. 5A, a strong CD8 response and a significantly lower CD4 response were induced in lungs of BALB/c mice upon i.n. immunization, and significant protection was achieved. In contrast, i.m. immunization induced a modest CD8 response and no measurable CD4 immune response in lungs, and the protection level did not reach significance. In lungs of C57BL/6 mice (Fig. 5B), however, the i.n. immunization induced primarily a CD4 response to Ag85 and a low CD8 response to TB10.4, whereas the i.m. immunization generated a low but detectable CD4 response to Ag85. Interestingly, this CD4 response in lungs of C57BL/6 mice, although relatively low, was able to mount statistically significant protection against M. tuberculosis challenge. Simple visual comparison of the protective response induced upon i.n. immunization of BALB/c and C57BL/6 mice suggests that different types of immune responses are capable of providing protection in different mouse strains, although the CD4 response seems to be more efficient. With regard to the immune response in spleen, which was protective against the dissemination of M. tuberculosis, either of the immunization routes induced a strong T-cell response, with somewhat more efficient response and protection induced upon i.m. immunization for both strains. Again, the protection in BALB/c mice was mediated through dominant CD8 responses with a barely detectable CD4 response (Fig. 5C), whereas in C57BL/6 mice, more balanced CD4 and CD8 responses were detected (Fig. 5D).
We have compiled the results from both mouse strains, from both immunization routes, and from both organs (lung and spleen) in a regression analysis where the rate of protection was studied as a function of the total number of detected IFN-γ-producing cells. A modest correlation was observed between these two parameters, although statistical significance was not achieved (P = 0.058), probably due to a high number of variables and a small sample size. From this regression analysis, 292 IFN-γ-producing cells/106 cells appeared to be associated with a 50% reduction in the mycobacterium load.
DISCUSSION
In this study, we demonstrate that a rAd35-vectored TB vaccine candidate, expressing three M. tuberculosis antigens as a single fusion protein, is able to induce a strong T-cell response and subsequently provide protection against an M. tuberculosis challenge in a small-rodent animal model. Both CD4 and CD8 IFN-γ-producing T cells were associated with this antimycobacterial immunity.
Although the correlate of protection in TB is not resolved yet, it is clear that IFN-γ- and related cytokine-mediated cellular immune responses play a major role in the protection (32, 42). These findings provide a rationale for the development of vaccination strategies that are based on the induction of cellular immunity. In particular, recombinant adenoviral vectors have the intrinsic ability to induce a strong cellular immune response by generating a population of T cells that are able to produce high levels of IFN-γ and to execute cytotoxic activity. Adenovectors are highly immunogenic and protective in preclinical animal models (2, 33), and recently, their immunogenicity in humans was demonstrated in clinical trials (J. Shiver, presented at the Keystone Symposium on HIV Vaccine Development: Progress and Prospects, Whistler, British Columbia, Canada, 2004). Besides being effective as a stand-alone vaccine, adenovectors are suitable as priming (2, 6) or boosting (2, 7, 36) vaccines, providing an opportunity for tailor-made immunization regimens designed to generate the required immune response. Among the different human Ad serotypes, Ad35 has an advantage of low seroprevalence in all age groups worldwide (25, 43, 45).
To generate a TB vaccine candidate (named Ad35-TBS), we incorporated antigens Ag85A, Ag85B, and TB10.4, which have exhibited highly promising vaccine properties in animal models and have been proven immunogenic in humans, into a rAd35 vector (17). The multiple antigens combined in a single vaccine increase the number of epitopes available, enabling a broad coverage of heterogeneous HLA haplotypes in humans. As demonstrated previously, the fusion protein is efficiently expressed upon adenovector-mediated cell infection and induces immune responses in mice (17). In the current study, we further explored the immunogenicity and determined the protective potential of the vector in two mouse strains of different haplotypes. We demonstrated that Ad35-TBS induces an antimycobacterial protective effect when applied either i.n. or i.m. Wang et al. (48) previously established that i.n. but not i.m. vaccination of BALB/c mice with Ad5-Ag85A provides potent protection against M. tuberculosis. Using the same mouse strain (BALB/c), we confirmed this finding. Moreover, in mice of a different haplotype (C57BL/6), both routes of immunization were shown to be protective against M. tuberculosis infection. The i.m. immunization route, albeit somewhat less efficient in reducing the mycobacterial burden in the lungs than the i.n. route, was superior at lowering M. tuberculosis systemic dissemination to the spleen.
Using the epitope mapping approach, we demonstrated that the fusion protein encoded by Ad35-TBS vector induces T-cell responses directed toward the same major epitopes as those identified previously using individual antigens (9, 13, 28, 41, 52). In addition, we identified three novel epitopes, which were not detected upon immunization of mice with single proteins and/or DNA encoding for individual antigens. It is known that in a protein, neighboring sequences influence the processing of T-cell epitopes and their presentation to antigen-presenting cells (8, 16). It is thus possible that the sequence context in the TB fusion protein facilitates efficient processing of otherwise silent epitopes, thus expanding the range of reactive epitopes. Using an epitope mapping approach with 15-mer peptides, we did not detect the CD4 epitopes in BALB/c mice that have been reported previously (9, 13, 18). This might be due to the apparent lower robustness of the ICS in detecting CD4-specific T cells in mice. Another possibility it that the 15-mer peptides that we used in study, in contrast to the 18- to 20-mer peptides used previously by others (9, 13, 48), are less suited for the detection of the response to previously reported CD4 peptides. Indeed, using the 20-mer peptide, reported previously as being the dominant CD4 epitope for Ag85A in BALB/c mice (9, 13, 48), we could detect the antigen-specific CD4 cells induced with Ad35-TBS in this mouse strain.
An interesting finding of our study concerns the type of cellular immune response associated with protection. In BALB/c mice, a predominant CD8 response was induced, while in C57BL/6 mice, the CD4 and CD8 responses were more balanced, with a more pronounced CD4 response in the lungs. This dissimilarity between the two mouse strains in the type of cellular response might somehow reflect the observed differences in lung histopathology upon M. tuberculosis challenge, with diffuse inflammation observed in BALB/c mice compared to granuloma formation in C57BL/6 mice. Mouse strains of different backgrounds may thus utilize different immunological mechanisms to fight M. tuberculosis infection. When all results for both mouse strains were compiled in a regression analysis, the rate of protection achieved with the vaccine correlated to the total IFN-γ response (although just not reaching statistical significance), thus supporting the role of IFN-γ in protection (32, 42). It should be noted that due to the relatively low sample size, we did not discriminate between CD4 and CD8 IFN-γ responses in this analysis, despite the fact that CD4 cells seemed to be more efficient than CD8 cells in providing protection in lungs. It is tempting to speculate that this might be due to a higher IFN-γ production capacity of CD4 cells than CD8 cells, as has recently been reported for T cells in a BCG infection model (31). However, this hypothesis remains to be confirmed. Our findings regarding the phenotype of antigen-specific T cells unify somewhat contradicting reports claiming the importance of either CD4 (12, 18) or CD8 (10, 47) cells in protection against TB. The finding that protection is achieved in animals of different immunological backgrounds with different types of T cells as the key mediators is promising when considering the vaccination of HLA haplotype-heterogeneous human populations.
Taken together, our results demonstrate that adenovector-based vaccines are able to induce a T-cell immune response that reduced the mycobacterium burden in the lungs of challenged animals and reduced the dissemination of M. tuberculosis. We also show that the i.n. route of immunization provides stronger protection against M. tuberculosis infection than the i.m. route, which is in agreement with a previous report (48). Recent unpublished results by Skeiky et al. indicate that in prime-boost vaccination regimens with rAd35, an i.m. route can be as efficient as an i.n. immunization (Y. A. W. Skeiky et al., unpublished data). Caution should be taken when extrapolating routing results obtained in rodent models directly to the human population. Rodents are suitable and inevitable for the first selection of vaccine candidates to demonstrate the intrinsic immunogenicity and possible protective potential. Unfortunately, we have no animal model that predicts the efficacy of selected vaccine candidates in humans. Only a retrospective comparison of the efficacy of vaccine candidates in humans with results obtained in animal models can provide us with immunological correlates of protection and criteria with which we can better select suitable vaccine candidates in the future.
In conclusion, we have demonstrated that recombinant Ad35 expressing multiple TB antigens induces a cellular immune response that is able to confer protection in a mouse model of tuberculosis. IFN-γ-producing CD4 and CD8 T cells were both associated with this protective property.
Acknowledgments
We thank Michael Brennan for kindly providing BCG and M. tuberculosis preclinical research standards. Sandrine Florquin is acknowledged for her expert histological evaluation of the lung tissues. We thank Dan Barouch for critical reading of the manuscript.
Editor: R. P. Morrison
Footnotes
Published ahead of print on 25 May 2007.
REFERENCES
- 1.Barouch, D. H., and G. J. Nabel. 2005. Adenovirus vector-based vaccines for human immunodeficiency virus type 1. Hum. Gene Ther. 16:149-156. [DOI] [PubMed] [Google Scholar]
- 2.Barouch, D. H., M. G. Pau, J. H. Custers, W. Koudstaal, S. Kostense, M. J. Havenga, D. M. Truitt, S. M. Sumida, M. G. Kishko, J. C. Arthur, B. Korioth-Schmitz, M. H. Newberg, D. A. Gorgone, M. A. Lifton, D. L. Panicali, G. J. Nabel, N. L. Letvin, and J. Goudsmit. 2004. Immunogenicity of recombinant adenovirus serotype 35 vaccine in the presence of pre-existing anti-Ad5 immunity. J. Immunol. 172:6290-6297. [DOI] [PubMed] [Google Scholar]
- 3.Baumann, S., A. N. Eddine, and S. H. Kaufmann. 2006. Progress in tuberculosis vaccine development. Curr. Opin. Immunol. 18:438-448. [DOI] [PubMed] [Google Scholar]
- 4.Brooks, J. V., A. A. Frank, M. A. Keen, J. T. Bellisle, and I. M. Orme. 2001. Boosting vaccine for tuberculosis. Infect. Immun. 69:2714-2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capone, S., A. Meola, B. B. Ercole, A. Vitelli, M. Pezzanera, L. Ruggeri, M. E. Davies, R. Tafi, C. Santini, A. Luzzago, T. M. Fu, A. Bett, S. Colloca, R. Cortese, A. Nicosia, and A. Folgori. 2006. A novel adenovirus type 6 (Ad6)-based hepatitis C virus vector that overcomes preexisting anti-Ad5 immunity and induces potent and broad cellular immune responses in rhesus macaques. J. Virol. 80:1688-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casimiro, D. R., A. J. Bett, T. M. Fu, M. E. Davies, A. Tang, K. A. Wilson, M. Chen, R. Long, T. McKelvey, M. Chastain, S. Gurunathan, J. Tartaglia, E. A. Emini, and J. Shiver. 2004. Heterologous human immunodeficiency virus type 1 priming-boosting immunization strategies involving replication-defective adenovirus and poxvirus vaccine vectors. J. Virol. 78:11434-11438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casimiro, D. R., L. Chen, T. M. Fu, R. K. Evans, M. J. Caulfield, M. E. Davies, A. Tang, M. Chen, L. Huang, V. Harris, D. C. Freed, K. A. Wilson, S. Dubey, D. M. Zhu, D. Nawrocki, H. Mach, R. Troutman, L. Isopi, D. Williams, W. Hurni, Z. Xu, J. G. Smith, S. Wang, X. Liu, L. Guan, R. Long, W. Trigona, G. J. Heidecker, H. C. Perry, N. Persaud, T. J. Toner, Q. Su, X. Liang, R. Youil, M. Chastain, A. J. Bett, D. B. Volkin, E. A. Emini, and J. W. Shiver. 2003. Comparative immunogenicity in rhesus monkeys of DNA plasmid, recombinant vaccinia virus, and replication-defective adenovirus vectors expressing a human immunodeficiency virus type 1 gag gene. J. Virol. 77:6305-6313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Del Val, M., H. J. Schlicht, T. Ruppert, M. J. Reddehase, and U. H. Koszinowski. 1991. Efficient processing of an antigenic sequence for presentation by MHC class I molecules depends on its neighboring residues in the protein. Cell 66:1145-1153. [DOI] [PubMed] [Google Scholar]
- 9.Denis, O., A. Tanghe, K. Palfliet, F. Jurion, T. P. van den Berg, A. Vanonckelen, J. Ooms, E. Saman, J. B. Ulmer, J. Content, and K. Huygen. 1998. Vaccination with plasmid DNA encoding mycobacterial antigen 85A stimulates a CD4+ and CD8+ T-cell epitopic repertoire broader than that stimulated by Mycobacterium tuberculosis H37Rv infection. Infect. Immun. 66:1527-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Derrick, S. C., C. Repique, P. Snoy, A. L. Yang, and S. Morris. 2004. Immunization with a DNA vaccine cocktail protects mice lacking CD4 cells against an aerogenic infection with Mycobacterium tuberculosis. Infect. Immun. 72:1685-1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dietrich, J., C. Aagaard, R. Leah, A. W. Olsen, A. Stryhn, T. M. Doherty, and P. Andersen. 2005. Exchanging ESAT6 with TB10.4 in an Ag85B fusion molecule-based tuberculosis subunit vaccine: efficient protection and ESAT6-based sensitive monitoring of vaccine efficacy. J. Immunol. 174:6332-6339. [DOI] [PubMed] [Google Scholar]
- 12.D'Souza, S., O. Denis, T. Scorza, F. Nzabintwali, H. Verschueren, and K. Huygen. 2000. CD4+ T-cells contain Mycobacterium tuberculosis infection in the absence of CD8+ T-cells in mice vaccinated with DNA encoding Ag85A. Eur. J. Immunol. 30:2455-2459. [DOI] [PubMed] [Google Scholar]
- 13.D'Souza, S., V. Rosseels, M. Romano, A. Tanghe, O. Denis, F. Jurion, N. Castiglione, A. Vanonckelen, K. Palfliet, and K. Huygen. 2003. Mapping of murine Th1 helper T-cell epitopes of mycolyl transferases Ag85A, Ag85B, and Ag85C from Mycobacterium tuberculosis. Infect. Immun. 71:483-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eddine, A. N., and S. H. Kaufmann. 2005. Improved protection by recombinant BCG. Microbes Infect. 7:939-946. [DOI] [PubMed] [Google Scholar]
- 15.Fallaux, F. J., A. Bout, I. van der Velde, D. J. van den Wollenberg, K. M. Hehir, J. Keegan, C. Auger, S. J. Cramer, H. van Ormondt, A. J. van der Eb, D. Valerio, and R. C. Hoeben. 1998. New helper cells and matched early region 1-deleted adenovirus vectors prevent generation of replication-competent adenoviruses. Hum. Gene Ther. 9:1909-1917. [DOI] [PubMed] [Google Scholar]
- 16.Hadeler, K. P., C. Kuttler, and A. K. Nussbaum. 2004. Cleaving proteins for the immune system. Math. Biosci. 188:63-79. [DOI] [PubMed] [Google Scholar]
- 17.Havenga, M., R. Vogels, D. Zuijdgeest, K. Radosevic, S. Mueller, M. Sieuwerts, F. Weichold, I. Damen, J. Kaspers, A. Lemckert, M. van Meerendonk, R. van der Vlugt, L. Holterman, D. Hone, Y. Skeiky, R. Mintardjo, G. Gillissen, D. Barouch, J. Sadoff, and J. Goudsmit. 2006. Novel replication-incompetent adenoviral B-group vectors: high vector stability and yield in PER.C6 cells. J. Gen. Virol. 87:2135-2143. [DOI] [PubMed] [Google Scholar]
- 18.Hervas-Stubbs, S., L. Majlessi, M. Simsova, J. Morova, M. J. Rojas, C. Nouze, P. Brodin, P. Sebo, and C. Leclerc. 2006. High frequency of CD4+ T cells specific for the TB10.4 protein correlates with protection against Mycobacterium tuberculosis infection. Infect. Immun. 74:3396-3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hess, J., D. Miko, A. Catic, V. Lehmensiek, D. G. Russell, and S. H. Kaufmann. 1998. Mycobacterium bovis bacille Calmette-Guerin strains secreting listeriolysin of Listeria monocytogenes. Proc. Natl. Acad. Sci. USA 95:5299-5304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmeister, B., F. Kiecker, L. Tesfa, H. D. Volk, L. J. Picker, and F. Kern. 2003. Mapping T-cell epitopes by flow cytometry. Methods 29:270-281. [DOI] [PubMed] [Google Scholar]
- 21.Horwitz, M. A., G. Harth, B. J. Dillon, and S. Maslesa-Galic. 2000. Recombinant bacillus Calmette-Guerin (BCG) vaccines expressing the Mycobacterium tuberculosis 30-kDa major secretory protein induce greater protective immunity against tuberculosis than conventional BCG vaccines in a highly susceptible animal model. Proc. Natl. Acad. Sci. USA 97:13853-13858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horwitz, M. A., B. W. Lee, B. J. Dillon, and G. Harth. 1995. Protective immunity against tuberculosis induced by vaccination with major extracellular proteins of Mycobacterium tuberculosis. Proc. Natl. Acad. Sci. USA 92:1530-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huygen, K., J. Content, O. Denis, D. L. Montgomery, A. M. Yawman, R. R. Deck, C. M. DeWitt, I. M. Orme, S. Baldwin, C. D'Souza, A. Drowart, E. Lozes, P. Vandenbussche, J. P. Van Vooren, M. A. Liu, and J. B. Ulmer. 1996. Immunogenicity and protective efficacy of a tuberculosis DNA vaccine. Nat. Med. 2:893-898. [DOI] [PubMed] [Google Scholar]
- 24.Kaufmann, S. H., and A. J. McMichael. 2005. Annulling a dangerous liaison: vaccination strategies against AIDS and tuberculosis. Nat. Med. 11:S33-S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kostense, S., W. Koudstaal, M. Sprangers, G. J. Weverling, G. Penders, N. Helmus, R. Vogels, M. Bakker, B. Berkhout, M. Havenga, and J. Goudsmit. 2004. Adenovirus types 5 and 35 seroprevalence in AIDS risk groups supports type 35 as a vaccine vector. AIDS 18:1213-1216. [DOI] [PubMed] [Google Scholar]
- 26.Leemans, J. C., S. Florquin, M. Heikens, S. T. Pals, R. van der Neut, and T. van der Poll. 2003. CD44 is a macrophage binding site for Mycobacterium tuberculosis that mediates macrophage recruitment and protective immunity against tuberculosis. J. Clin. Investig. 111:681-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lemckert, A. A., S. M. Sumida, L. Holterman, R. Vogels, D. M. Truitt, D. M. Lynch, A. Nanda, B. A. Ewald, D. A. Gorgone, M. A. Lifton, J. Goudsmit, M. J. Havenga, and D. H. Barouch. 2005. Immunogenicity of heterologous prime-boost regimens involving recombinant adenovirus serotype 11 (Ad11) and Ad35 vaccine vectors in the presence of anti-Ad5 immunity. J. Virol. 79:9694-9701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Majlessi, L., M.-J. Rojas, P. Brodin, and C. Leclerc. 2003. CD8+-T-cell responses of mycobacterium-infected mice to a newly identified major histocompatibility complex class I-restricted epitope shared by proteins of the ESAT-6 family. Infect. Immun. 71:7173-7177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McShane, H., A. A. Pathan, C. R. Sander, S. M. Keating, S. C. Gilbert, K. Huygen, H. A. Fletcher, and A. V. Hill. 2004. Recombinant modified vaccinia virus Ankara expressing antigen 85A boosts BCG-primed and naturally acquired antimycobacterial immunity in humans. Nat. Med. 10:1240-1244. [DOI] [PubMed] [Google Scholar]
- 30.Nanda, A., D. M. Lynch, J. Goudsmit, A. A. Lemckert, B. A. Ewald, S. M. Sumida, D. M. Truitt, P. Abbink, M. G. Kishko, D. A. Gorgone, M. A. Lifton, L. Shen, A. Carville, K. G. Mansfield, M. J. Havenga, and D. H. Barouch. 2005. Immunogenicity of recombinant fiber-chimeric adenovirus serotype 35 vector-based vaccines in mice and rhesus monkeys. J. Virol. 79:14161-14168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ngai, P., S. McCormick, C. Small, X. Zhang, A. Zganiacz, N. Aoki, and Z. Xing. 2007. Gamma interferon responses of CD4 and CD8 T-cell subsets are quantitatively different and independent of each other during pulmonary Mycobacterium bovis BCG infection. Infect. Immun. 75:2244-2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.North, R. J., and Y. J. Jung. 2004. Immunity to tuberculosis. Annu. Rev. Immunol. 22:599-623. [DOI] [PubMed] [Google Scholar]
- 33.Ophorst, O. J., K. Radosevic, M. J. Havenga, M. G. Pau, L. Holterman, B. Berkhout, J. Goudsmit, and M. Tsuji. 2006. Immunogenicity and protection of a recombinant human adenovirus serotype 35-based malaria vaccine against Plasmodium yoelii in mice. Infect. Immun. 74:313-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santra, S., M. S. Seaman, L. Xu, D. H. Barouch, C. I. Lord, M. A. Lifton, D. A. Gorgone, K. R. Beaudry, K. Svehla, B. Welcher, B. K. Chakrabarti, Y. Huang, Z. Y. Yang, J. R. Mascola, G. J. Nabel, and N. L. Letvin. 2005. Replication-defective adenovirus serotype 5 vectors elicit durable cellular and humoral immune responses in nonhuman primates. J. Virol. 79:6516-6522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shiver, J. W., and E. A. Emini. 2004. Recent advances in the development of HIV-1 vaccines using replication-incompetent adenovirus vectors. Annu. Rev. Med. 55:355-372. [DOI] [PubMed] [Google Scholar]
- 36.Skeiky, Y. A., and J. C. Sadoff. 2006. Advances in tuberculosis vaccine strategies. Nat. Rev. Microbiol. 4:469-476. [DOI] [PubMed] [Google Scholar]
- 37.Skjot, R. L., I. Brock, S. M. Arend, M. E. Munk, M. Theisen, T. H. Ottenhoff, and P. Andersen. 2002. Epitope mapping of the immunodominant antigen TB10.4 and the two homologous proteins TB10.3 and TB12.9, which constitute a subfamily of the esat-6 gene family. Infect. Immun. 70:5446-5453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skjot, R. L., T. Oettinger, I. Rosenkrands, P. Ravn, I. Brock, S. Jacobsen, and P. Andersen. 2000. Comparative evaluation of low-molecular-mass proteins from Mycobacterium tuberculosis identifies members of the ESAT-6 family as immunodominant T-cell antigens. Infect. Immun. 68:214-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, L. Xu, Z. Y. Yang, M. Roederer, R. A. Koup, P. B. Jahrling, and G. J. Nabel. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424:681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sumida, S. M., D. M. Truitt, A. A. Lemckert, R. Vogels, J. H. Custers, M. M. Addo, S. Lockman, T. Peter, F. W. Peyerl, M. G. Kishko, S. S. Jackson, D. A. Gorgone, M. A. Lifton, M. Essex, B. D. Walker, J. Goudsmit, M. J. Havenga, and D. H. Barouch. 2005. Neutralizing antibodies to adenovirus serotype 5 vaccine vectors are directed primarily against the adenovirus hexon protein. J. Immunol. 174:7179-7185. [DOI] [PubMed] [Google Scholar]
- 41.Tanghe, A., S. D'Souza, V. Rosseels, O. Denis, T. H. Ottenhoff, W. Dalemans, C. Wheeler, and K. Huygen. 2001. Improved immunogenicity and protective efficacy of a tuberculosis DNA vaccine encoding Ag85 by protein boosting. Infect. Immun. 69:3041-3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tascon, R. E., E. Stavropoulos, K. V. Lukacs, and M. J. Colston. 1998. Protection against Mycobacterium tuberculosis infection by CD8+ T cells requires the production of gamma interferon. Infect. Immun. 66:830-834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thorner, A. R., R. Vogels, J. Kaspers, G. J. Weverling, L. Holterman, A. A. C. Lemckert, A. Dilraj, L. M. McNally, P. M. Jeena, S. Jepsen, P. Abbink, A. Nanda, P. E. Swanson, A. T. Bates, K. L. O'Brien, M. J. E. Havenga, J. Goudsmit, and D. Barouch. 2006. Age dependence of adenovirus-specific neutralizing antibodies in sub-Saharan Africa. J. Clin. Microbiol. 44:3781-3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tobery, T. W., S. Wang, X. M. Wang, M. P. Neeper, K. U. Jansen, W. L. McClements, and M. J. Caulfield. 2001. A simple and efficient method for the monitoring of antigen-specific T-cell responses using peptide pool arrays in a modified ELISpot assay. J Immunol. Methods 254:59-66. [DOI] [PubMed] [Google Scholar]
- 45.Vogels, R., D. Zuijdgeest, R. van Rijnsoever, E. Hartkoorn, I. Damen, M. P. de Bethune, S. Kostense, G. Penders, N. Helmus, W. Koudstaal, M. Cecchini, A. Wetterwald, M. Sprangers, A. Lemckert, O. Ophorst, B. Koel, M. van Meerendonk, P. Quax, L. Panitti, J. Grimbergen, A. Bout, J. Goudsmit, and M. Havenga. 2003. Replication-deficient human adenovirus type 35 vectors for gene transfer and vaccination: efficient human cell infection and bypass of preexisting adenovirus immunity. J. Virol. 77:8263-8271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang, D., A. L. Schmaljohn, N. U. Raja, C. M. Trubey, L. Y. Juompan, M. Luo, S. B. Deitz, H. Yu, J. Woraratanadharm, D. H. Holman, K. M. Moore, B. M. Swain, W. D. Pratt, and J. Y. Dong. 2006. De novo syntheses of Marburg virus antigens from adenovirus vectors induce potent humoral and cellular immune responses. Vaccine 24:2975-2986. [DOI] [PubMed] [Google Scholar]
- 47.Wang, J., M. Santosuosso, P. Ngai, A. Zganiacz, and Z. Xing. 2004. Activation of CD8 T-cells by mycobacterial vaccination protects against pulmonary tuberculosis in the absence of CD4 T-cells. J. Immunol. 173:4590-4597. [DOI] [PubMed] [Google Scholar]
- 48.Wang, J., L. Thorson, R. W. Stokes, M. Santosuosso, K. Huygen, A. Zganiacz, M. Hitt, and Z. Xing. 2004. Single mucosal, but not parenteral, immunization with recombinant adenoviral-based vaccine provides potent protection from pulmonary tuberculosis. J. Immunol. 173:6357-6365. [DOI] [PubMed] [Google Scholar]
- 49.Wieland, C. W., S. Florquin, E. D. Chan, J. C. Leemans, S. Weijer, A. Verbon, G. Fantuzzi, and T. van der Poll. 2005. Pulmonary Mycobacterium tuberculosis infection in leptin-deficient ob/ob mice. Int. Immunol. 17:1399-1408. [DOI] [PubMed] [Google Scholar]
- 50.Williams, A., G. J. Hatch, S. O. Clark, K. E. Gooch, K. A. Hatch, G. A. Hall, K. Huygen, T. H. Ottenhoff, K. L. Franken, P. Andersen, T. M. Doherty, S. H. Kaufmann, L. Grode, P. Seiler, C. Martin, B. Gicquel, S. T. Cole, P. Brodin, A. S. Pym, W. Dalemans, J. Cohen, Y. Lobet, N. Goonetilleke, H. McShane, A. Hill, T. Parish, D. Smith, N. G. Stoker, D. B. Lowrie, G. Kallenius, S. Svenson, A. Pawlowski, K. Blake, and P. D. Marsh. 2005. Evaluation of vaccines in the EU TB Vaccine Cluster using a guinea pig aerosol infection model of tuberculosis. Tuberculosis (Edinburgh) 85:29-38. [DOI] [PubMed] [Google Scholar]
- 51.Xing, Z., M. Santosuosso, S. McCormick, T. C. Yang, J. Millar, M. Hitt, Y. Wan, J. Bramson, and H. M. Vordermeier. 2005. Recent advances in the development of adenovirus- and poxvirus-vectored tuberculosis vaccines. Curr. Gene Ther. 5:485-492. [DOI] [PubMed] [Google Scholar]
- 52.Yanagisawa, S., M. Koike, A. Kariyone, S. Nagai, and K. Takatsu. 1997. Mapping of V beta 11+ helper T-cell epitopes on mycobacterial antigen in mouse primed with Mycobacterium tuberculosis. Int. Immunol. 9:227-237. [DOI] [PubMed] [Google Scholar]