Abstract
OBJECTIVE
To determine whether use of clinical decision rules or rapid streptococcal antigen detection tests (alone or in combination) can lower the number of unnecessary prescriptions for antibiotics for adults with acute sore throats.
DESIGN
Four-arm randomized controlled trial.
SETTING
Family practice offices in eastern Newfoundland.
PARTICIPANTS
Forty urban and suburban family practitioners.
INTERVENTIONS
Participants were randomly assigned to one of 4 arms (usual practice, decision rules only, rapid antigen test only, decision rules and antigen test combined), and each recruited successive adult patients presenting with acute sore throat as their main symptom. Following usual care or use of decision rules or rapid antigen tests or both (where applicable), physicians were to record what they prescribed for each patient.
MAIN OUTCOME MEASURES
Prescribing rates and types of antibiotics prescribed.
RESULTS
The prescribing rate using decision rules (55%) did not differ significantly from the rate using usual clinical practice (58%). Physicians using rapid antigentests, both alone and with decision rules, had significantly lower prescribing rates (27% and 38%, respectively, both P < .001).
CONCLUSION
Evidence-based clinical decision rules alone do not change family doctors’ prescribing behaviour. Use of rapid antigen tests might allow physicians to persuade patients that negative results (and hence, viral infection) mean antibiotic therapy is not required.
RÉSUMÉ
OBJECTIF
Déterminer si l’utilisation de règles de décisions cliniques ou de tests rapides de dépistage des antigènes de streptocoques (seuls ou combinés) peut réduire le nombre d’ordonnances d’antibiotiques inutiles pour des adultes souffrant de mal de gorge aigu.
CONCEPTION
Étude contrôlée randomisée à 4 volets.
CONTEXTE
Cabinets de pratique familiale dans l’Est de Terre-Neuve.
PARTICIPANTS
Quarante praticiens de la médecine familiale en milieu urbain et en banlieue.
INTERVENTIONS
On a assigné au hasard les participants à l’un des 4 volets (pratique habituelle, règles de décision seulement, test rapide de dépistage des antigènes seulement, règles de décisions et test des antigènes combinés). Chacun a recruté les patients adultes seprésentant successivement avec un mal de gorge aigu comme principal symptôme. À la suite des soins habituels, de l’utilisation des règles de décisions, des tests de dépistage rapide des antigènes ou des deux (selon le cas), les médecins devaient consigner ce qu’ils avaient prescrit à chacun de ces patients.
PRINCIPALES MESURES DES RÉSULTATS
Taux de prescription et types d’antibiotique prescrits.
RÉSULTATS
Le taux de prescription après avoir utilisé les règles de décisions (55%) ne différait pas considérablement de celui des médecins suivant leur pratique clinique habituelle (58%). Les médecins qui utilisaient les tests de dépistage rapide des antigènes, seuls ou combinés aux règles de décisions, enregistraient des taux beaucoup plus bas de prescription (27% et 38% respectivement, dans les deux cas P < ,001).
CONCLUSION
Les règles de décisions cliniques fondées sur des données scientifiques, utilisées seules, ne changent pas le comportement des médecins de famille en matière de prescription. L’utilisation des tests de dépistage rapide des antigènes pourrait permettre aux médecins de persuader leurs patients que des résultats négatifs (donc une infection virale) signifient que l’antibiothérapie n’est pas nécessaire.
Acute respiratory tract infections are the reason for about a quarter of all visits to family doctors in North America, and a quarter of these visits are for acute sore throat.1 The large number of sore throats means that they account for 3% to 6% of all office visits.2,3
In adults, 85% to 90% of sore throats are caused by viral infections.4 Treating patients who have sore throats with antibiotics does not relieve symptoms very much, if at all. A study of patients with tonsillitis in 17 countries found that the mean duration of fever was 2 to 3 days, regardless of whether or not patients took penicillin.5 Patients who test positive for group A β-hemolytic streptococcus (GABHS) who are treated with penicillin have relief of symptoms about 16 hours earlier than those who test negative for GABHS.6 Treated or not, 85% of patients are completely free of symptoms at 1 week.7
Mentioning a sore throat to a doctor almost guarantees a prescription for antibiotics. In Australia, 89% of patients with sore throats got antibiotic prescriptions8; in the United States, the rate was 73%.9 A study of 73 Newfoundland family doctors found that 84% of them prescribed antibiotics to adults with sore throats.10 In Holland, which has a tradition of low prescribing rates for antibiotics, the rate was still 52%.11
Attempts have been made to derive simple sore throat decision rules (STDR) so that doctors can more appropriately prescribe antibiotics for patients likely to have GABHS. In general, 4 clinical features have been found useful in deciding which adults are most likely to have GABHS infection: fever, tonsillar exudates, anterior cervical lymphadenopathy, and the absence of cough (Table 112). A Canadian study found that using clinical rules would have reduced prescriptions for antibiotics among adults with sore throats by 88%13 if doctors had followed these rules. Another study showed that, while using the rules improved physicians’ estimates of the presence or absence of GABHS, it did not alter how they used antibiotics.14 We wanted to know whether using STDR would change doctors’ antibiotic prescribing practices appropriately.
Table 1. Sore throat decision rules used in our study.
Score of =1—no need for antibiotics, 3 or 4—antibiotics are required, 2—antibiotics might or might not be beneficial.
| PATIENT HAS | YES | NO |
|---|---|---|
| Cough | −1 | +1 |
| Fever >38º | +1 | 0 |
| Swollen submandibular glands | +1 | 0 |
| Exudate on throat or tonsils | +1 | 0 |
Adapted from Centor et al.12
Rapid antigen detection tests (RADT) provide results much more quickly than the criterion standard of GABHS detection, agar plate culture, does. Rapid antigen detection tests have a specificity in the 95% range, so false-positive results are rare.15 The sensitivity of RADT increases with the number of positive clinical features a patient has.16 The primary advantage of RADT over throat-swab cultures is that results can be available in only 5 to 10 minutes, and the test costs as little as $5. Treatment, if needed, can be started before patients leave the doctor’s office.
A literature review using the terms “rapid antigen test,” “streptococcal sore throat,” and “primary care” found that RADTs have been used in various parts of the world: Denmark,17 New Mexico,18 the Netherlands,17 Israel,19 the Canary Islands,20 and Switzerland.21 In general, these studies concluded that the RADT was a valid test for diagnosing streptococcal sore throat in adults and that it had high specificity and positive predictive values. The value of RADT for children was less clear.
Using either STDR or RADT should allow family doctors to make rapid and more informed decisions than when they use usual clinical judgment. The objectives of this trial were to compare rates of diagnosis of likely GABHS infection, represented by prescriptions for antibiotics, using usual clinical judgment, STDR, RADT, and both STDR and RADT, and to assess whether STDR and RADT are better used alone or in combination.
METHODS
This randomized controlled trial was conducted in family doctors’ offices in eastern Newfoundland during February, March, and April 2005. The study was approved by Memorial University of Newfoundland’s Human Investigations Committee.
Physicians known not to be in family practice (either from the investigators’ personal knowledge or from the records of the Newfoundland and Labrador Medical Association) were removed from the list of non-specialist physicians in the study area. Successive random blocks of 40 family physicians were approached to take part in the study (using the Dillman technique) until 40 physicians were recruited.
The trial had 4 arms: a control group continuing usual clinical practice, a group using STDR, a group using RADT, and a group using both STDR and RADT. Physicians in the control arm were asked to follow their usual clinical practices and record their prescribed management. All others were required to administer the appropriate intervention first and then record their management.
We based our STDR upon those developed and tested for adults by Centor and colleagues at the University of Virginia,12 but modified them to reflect evidence from other studies of adult patients (Table 112).22,23 Once doctors assessed patients using STDR criteria, they made recommendations based on total scores. A score of =1 suggested there was no need for antibiotics, while a score of 3 or 4 suggested that antibiotics were required. A score of 2 indicated that antibiotics might or might not be beneficial. When using the combined STDR and RADT intervention, doctors were asked to use the RADT only when the score on the STDR was 2. We only suggested what physicians should do with each category of score; we did not command or expect obedience from family doctors.
The RADT used in the trial was the Clearview® Exact Strep A dipstick from Wampole Laboratories. This test is reported by the manufacturers to have a sensitivity of about 90% and a specificity of about 95%.
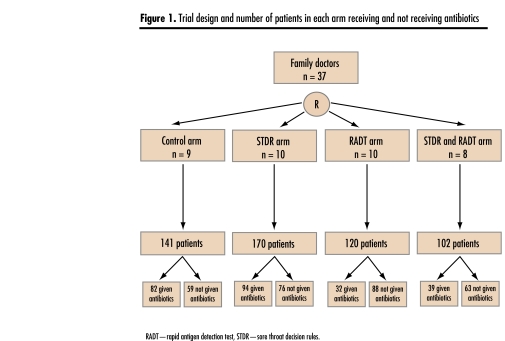
The 40 physicians who agreed to take part in the study were randomly allocated to 1 of 4 trial arms, and each was asked to recruit 20 successive adult patients (aged 19 years or older) who presented with acute sore throat as their primary symptom. We did not ask doctors to record clinical or demographic characteristics of the patients; we wanted the doctors to do as little extra work as possible. We oversampled to compensate for physicians who might not enter the total number of subjects requested. Figure 1 shows the trial design. To detect a 25% reduction in the rate of antibiotic prescribing, 98 patients were required in each trial arm (2-tailedα.05, β .20). χ2 comparisons using the Statistical Package for the Social Sciences for Windows, release 11.0.1, were used to test for differences in prescribing rates between the control group and the intervention groups. Analysis of covariance was used to compare differences in demographics among the groups of physicians.
Figure 1.
Trial design and number of patients in each arm receiving and not receiving antibiotics
RESULTS
Of the 204 general practitioners in eastern Newfoundland, 157 were in active family practice. Three successive samples of 40 physicians were asked to be in the study until a total of 40 physicians was recruited. Of the 120 physicians in these random samples, 40 agreed to take part and 80 declined. The first, second, and third efforts recruited 11, 17, and 12 doctors, respectively. Table 2 shows some characteristics of the physicians by study group. There were no significant differences between doctors in the 4 groups, nor were the study group doctors different from the 80 physicians who declined to take part in the study (analysis of covariance, F = 2.12, P > .05). In all, 37 of the 40 recruited physicians actually entered patients in the trial.
Table 2.
Characteristics of physicians recruited to each study arm and of non-participating physicians: None of the differences between groups was significant (analysis of covariance: F = 2.12; df = 4,19).
| CHARACTERISTIC | NON-PARTICIPATING PHYSICIANS N = 80 | USUAL-CARE ARM N = 10 | STDR ARM N = 10 | RADT ARM N = 10 | COMBINED STDR AND RADT ARM N = 10 |
|---|---|---|---|---|---|
| Mean no. of years since Graduation | 15.2 | 13.9 | 19.0 | 17.4 | 19.3 |
| Sex (% female) | 62 | 70 | 60 | 60 | 50 |
| Canadian graduate (%) | 84 | 100 | 90 | 100 | 90 |
| Member of the College of Family Physicians of Canada (%) | 59 | 70 | 70 | 50 | 60 |
RADT—rapid antigen detection test, STDR—sore throat decision rules.
The number of patients entered was 533, with a mean of 14.5 patients for each doctor (range, 4 to 20). The physicians wrote a total of 247 prescriptions for antibiotics (46.7% of patients received antibiotics).
Table 3 shows the number of patients recruited in each arm of the trial and the rates of antibiotic prescribing. Doctors in the usual-practice and STDR-only arms wrote prescriptions for approximately the same proportion of patients (58% and 55%, respectively). Doctors in the RADT-only and the combined STDR and RADT arms prescribed antibiotics to fewer patients (27% and 38%, respectively). Doctors in the RADT and combined STDR and RADT arms prescribed antibiotics to significantly fewer patients than doctors in the usual-practice group did (Table 3). Doctors in the groups who used RADT alone or in combination with STDR recruited fewer patients (120 and 102, respectively) than doctors in the usual-practice and STDR-only groups did (141 and 170, respectively).
Table 3.
Percentage of antibiotic prescriptions by study arm
| STUDY ARM | NO. OF PHYSICIANS | NO. OF PATIENTS | NO. OF ANTIBIOTIC PRESCRIPTIONS | % OF VISITS WHERE ANTIBIOTICS WERE PRESCRIBED | χ2 | P VALUE |
|---|---|---|---|---|---|---|
| Usual practice | 9 | 141 | 82 | 58.2 | ||
| STDR only | 10 | 170 | 94 | 55.3 | 0.590 | NS |
| RADT only | 10 | 120 | 32 | 26.7 | 49.048 | <.001 |
| STDR and RADT | 8 | 102 | 39 | 38.2 | 16.705 | <.001 |
| TOTAL | 37 | 533 | 247 | 46.7 |
RADT—rapid antigen detection test, STDR—sore throat decision rules.
Amoxicillin was the most commonly prescribed antibiotic; 115 of 247 (47%) prescriptions were for amoxicillin. Penicillin was second, with 50 prescriptions (20%). A variety of other antibiotics constituted less than 10% of prescriptions each.
DISCUSSION
Inherent in the design of this trial was a potential clustering of patients by physician. Clustering has the effect of widening confidence intervals. The 95% confidence levels of the proportions of antibiotic prescriptions in the higher-prescribing groups (usual care and STDR) did not overlap with those of the lower-prescribing groups (RADT and combined STDR and RADT). Accordingly, we think that differences we observed were so great that our results are robust.
In this trial, we found that use of the RADT, either as the only diagnostic aid or in combination with the STDR, was associated with a significantly lower rate of antibiotic prescribing. Use of the STDR alone did not appear to affect physicians’ prescribing rates. The lower antibiotic prescribing rates, of 27% in the RADT-only arm and 38% in the combined STDR and RADT arm, are similar to those found in a previous primary care study in Switzerland where use of the RADT reduced antibiotic prescribing from 60% to 37%.21
The apparent inability of the STDR to change doctors’ behaviour had been found in 2 previous studies.14,24 A recent survey of 1000 American pediatricians found that 42% would start antimicrobials before they knew diagnostic test results, and 27% of them would continue treatment even if test results were negative.25 We do not know why doctors are so resistant to changing their practice, even when they know the STDR and the test results.26 Our study suggests that doctors are more confident with the results of a diagnostic test than they are with decision rules. Negative RADT results seem to give physicians more confidence about explaining to patients why antibiotics are not needed for their throat infections.
Questions and concerns
Several intriguing questions remain about the use of RADT in doctors’ offices. Even after using RADT, the antibiotic prescribing rate was still 27%, higher than the known community infection rate with GABHS.4 Perhaps the GABHS infection rate in these patients was higher than usual, or perhaps some of the positive RADT results were from patients who were GABHS carriers. It is also possible that physicians in the RADT arms recruited patients with symptoms and signs more suggestive of GABHS. The relative inconvenience of performing the test might have discouraged them from enrolling those less likely to have GABHS and might help explain the lower overall enrolment in the RADT and combined STDR and RADT arms.
Of some concern was the finding that, when an antibiotic was used, it was likely to be amoxicillin (47%). Group A β-hemolytic streptococci are uniformly susceptible to penicillin V. Clearly patients who received amoxicillin were not allergic to penicillin, and we do not know why amoxicillin was prescribed so often. We are conducting a qualitative study of doctors who took part in this trial to gain more insight into their prescribing practices.
Conclusion
Our study found that use of the RADT in primary care offices (either alone or in conjunction with the STDR) was associated with a significant reduction in prescriptions for antibiotics among adults whose primary complaint was an acute sore throat.
Acknowledgment
Kathy Murphy was the research nurse on this study. Theresa Kerrivan coordinated the paperwork for the study and handled correspondence. Jennifer Braun helped with preliminary data analysis.
POINTS DE REPÈRE DU RÉDACTEUR
La consultation d’un médecin pour un mal de gorge entraîne presque toujours la prescription d’un antibiotique.
Les tests de détection rapide de l’antigène offrent une spécificité de 95% permettant ainsi d’exclure rapidement la plupart de faux positifs.
Ces tests se révèlent supérieurs aux lignes directrices pour convaincre le patient de l’inutilité de prendre des antibiotiques.
EDITOR’S KEY POINTS
Mentioning a sore throat to a doctor almost guarantees a prescription for antibiotics.
Rapid antigen detection tests have a 95% specificity, allowing rapid exclusion of false-positive results.
These tests are superior to guidelines for persuading patients that antibiotics will not be useful.
Footnotes
This article has been peer reviewed.
Contributors: Drs Worrall, Hutchinson, and Sherman and Mr Griffiths contributed to concept and design of the study; data gathering, analysis, and interpretation; and preparing the article for submission.
Competing interests
None declared
References
- 1.National Centre for Health Statistics. Data from the National Ambulatory Care Survey 1999. Hyattsville, Md: National Centre for Health Statistics; 2000. [Accessed 2007 March 15]. Available from: www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm. [Google Scholar]
- 2.Schippert SM. Ambulatory care visits to physicians’ offices, hospital outpatients and emergency departments in the United States, 1996. Hyattsville, Md: National Centre for Health Statistics; 1998. [PubMed] [Google Scholar]
- 3.Britt H, Miller GC, Knox S. General practice activity in Australia 2000–2001. Canberra, Aust: Australian Institute of Health and Welfare; 2001. [Google Scholar]
- 4.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections and bronchitis, by ambulatory care physicians. JAMA. 1997;278:901–4. [PubMed] [Google Scholar]
- 5.Touw-Otten F, Johansen KS. Diagnosis, antibiotic treatment and outcome of tonsillitis: report of a WHO office for 17 European countries. Fam Pract. 1992;9:255–62. doi: 10.1093/fampra/9.3.255. [DOI] [PubMed] [Google Scholar]
- 6.Pichichero ME, Disney FA, Talpey WB, Green JL, Francis AB, Roghmann KJ, et al. Adverse and beneficial effects of immediate treatment for group A beta-hemolytic streptococcal pharyngitis with penicillin. Pediatr Infect Dis J. 1987;6:635–43. doi: 10.1097/00006454-198707000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Del Mar CB, Glasziou PP, Spinks AB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2006;4:CD000023. doi: 10.1002/14651858.CD000023. [DOI] [PubMed] [Google Scholar]
- 8.Patterson CA, Mackeson JM, Weekes LM. Antibiotic prescribing for upper respiratory tract infections in primary care. Commun Dis Intell. 2003;27(Suppl):S39–41. doi: 10.33321/cdi.2003.27.19. [DOI] [PubMed] [Google Scholar]
- 9.Linder JA, Stafford RS. Antibiotic treatment of adults with sore throat by community primary care physicians: a national survey 1989–99. JAMA. 2001;286:1181–6. doi: 10.1001/jama.286.10.1181. [DOI] [PubMed] [Google Scholar]
- 10.Hutchinson JM, Jelinski S, Hefferton D, Desaulniers G, Parfrey PS. Role of diagnostic labeling in antibiotic prescription. Can Fam Physician. 2001;47:1217–24. [PMC free article] [PubMed] [Google Scholar]
- 11.Demelker RA, Kuyvenhovven MM. Management of upper respiratory tract infections in Dutch general practice. Br J Gen Pract. 1991;41:507–10. [PMC free article] [PubMed] [Google Scholar]
- 12.Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making. 1981;1:239–46. doi: 10.1177/0272989X8100100304. [DOI] [PubMed] [Google Scholar]
- 13.McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat rule in family practice. CMAJ. 2000;163:811–5. [PMC free article] [PubMed] [Google Scholar]
- 14.Gerber MA. Comparison of throat cultures and rapid streptococcal tests for diagnosis of streptococcal pharyngitis. Pediatr Infect Dis J. 1989;8:820–4. doi: 10.1097/00006454-198911000-00032. [DOI] [PubMed] [Google Scholar]
- 15.Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin Infect Dis. 2002;35:113–25. doi: 10.1086/340949. [DOI] [PubMed] [Google Scholar]
- 16.Dagnelie CF, Bartelink ML, van der Graaf Y, Goessens W, de Melker RA. Towards a better diagnosis of throat infections (with group A beta-hemolytic streptococci) in general practice. Br J Gen Pract. 1998;48:959–62. [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffman S, Henrichsen J. Detection of group A streptococcal antigen from throat swabs by use of a latex agglutination test kit in general practice. Acta Pathol Microbiol Immunol Scand. 1987;95:89–94. doi: 10.1111/j.1699-0463.1987.tb03093.x. [DOI] [PubMed] [Google Scholar]
- 18.Hart AP, Buck LL, Morgan S, Saverio S, McLaughlin JC. A comparison of the Biostar Strep A OIA rapid antigen assay, group A Selective Strep Agar (ssA), and Todd-Hewitt broth cultures for the detection of group A streptococcus in an outpatient family practice setting. Diagn Microbiol Infect Dis. 1997;29:139–45. doi: 10.1016/s0732-8893(97)81803-2. [DOI] [PubMed] [Google Scholar]
- 19.Hasin M, Furst A. Sore throat in family practice: comparison of blood agar throat culture with a rapid enzyme immunoassay test for diagnostic purposes. J R Coll Gen Pract. 1989;39:332–4. [PMC free article] [PubMed] [Google Scholar]
- 20.Diaz-Berenguer JA, Ibrahim F. Evaluation of a rapid technique for detecting the type A streptococcus antigen (Test Pack Strep A) Aten Primaria. 1992;9:245–9. [PubMed] [Google Scholar]
- 21.Humair JP, Revaz SA, Bovier P, Stalder H. Management of acute pharyngitis in adults: reliability of rapid streptococcal tests and clinical findings. Arch Intern Med. 2006;166:640–4. doi: 10.1001/archinte.166.6.640. [DOI] [PubMed] [Google Scholar]
- 22.McIsaac WJ, White D, Tannenbaum D, Lowe DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ. 1998;158:75–83. [PMC free article] [PubMed] [Google Scholar]
- 23.Walsh BT, Bookheim WW, Johnson RC, Tompkins RK. Recognition of streptococcal pharyngitis in adults. Arch Intern Med. 1975;135:1493–7. [PubMed] [Google Scholar]
- 24.McIsaac WJ, Goel V, To T, Permaul JA, Low DE. Effect on antibiotic prescribing of repeated clinical prompts to use a sore throat score: lessons from a failed community intervention study. J Fam Pract. 2002;51:339–44. [PubMed] [Google Scholar]
- 25.Park SV, Gerber MA, Tanz RR, Hickner JM. Clinicians’ management of children and adolescents with acute pharyngitis. Pediatrics. 2006;117:1871–8. doi: 10.1542/peds.2005-2323. [DOI] [PubMed] [Google Scholar]
- 26.Poses RM, Cebul RD, Wigton RS. You can lead a horse to water—improving physicians’ knowledge of probabilities may not affect their decisions. Med Decis Making. 1995;15:65–76. doi: 10.1177/0272989X9501500110. [DOI] [PubMed] [Google Scholar]