Abstract
Aim
To identify the presence, and origin, of any “dissociating factors” inherent to the techniques for evaluating progression that mask the relationship between structural and functional progression in open‐angle glaucoma (OAG).
Methods
23 patients (14 with OAG and 9 with ocular hypertension (OHT)) who had received serial Heidelberg Retina Tomograph (HRT II) and Humphrey Field Analyser (HFA) examinations for ⩾5 years (mean 78.4 months (SD 9.5), range 60–101 months) were identified. Evidence of progressive disease was retrospectively evaluated in one eye of each patient using the Topographic Change Analysis (TCA) and Glaucoma Progression Analysis (GPA) for the HRT II and HFA, respectively.
Results
Six patients were stable by both techniques; four exhibited both structural and functional progression; seven exhibited structural progression, only, and six showed functional progression, only. Three types of dissociating factors were identified. TCA failed to identify progressive structural damage in the presence of advanced optic nerve head damage. GPA failed to identify progressive functional damage at stimulus locations, with sensitivities exhibiting test‐retest variability beyond the maximum stimulus luminance of the perimeter, and where a perimetric learning effect was apparent.
Conclusion
The three dissociating factors accounted for nine of the 13 patients who exhibited a lack of concordance between structural and functional progressive damage.
Open‐angle glaucoma (OAG) is associated with structural change to the optic nerve head (ONH) and functional deficit to the visual field. In the earliest stages, structural damage seemingly precedes perimetrically detectable functional loss,1although in the later stages, functional progression is more readily apparent than structural progression.2 The precise temporal relationship of the clinical course in terms of structural and functional damage remains equivocal.
The advent of digital imaging systems such as confocal scanning laser ophthalmoscopy, optical coherence tomography, nerve fibre layer polarimetry and retinal thickness analysis provides an opportunity for objective quantification of progressive structural damage to the ONH and peripapillary retina.3,4,5,6 The technology in longest clinical use, and therefore the current standard, is confocal scanning laser ophthalmoscopy using the Heidelberg Retina Tomograph (HRT; Heidelberg Engineering, Dossenheim, Germany).
The identification of progressive functional damage to the visual field from serial examinations derived by standard automated perimetry (SAP) is based on a variety of subjective clinical criteria.7,8,9,10,11
The relationship between structural and functional progressive damage assessed using the HRT and Humphrey Field Analyser (HFA; Carl Zeiss Meditec, Dublin, CA, USA), respectively, has received little attention, but is equivocal.12,13 The relationship derived by these technologies may be confounded by the presence of one or more dissociating factors inherent to the given investigative technique.12,13 Such confounding factors are yet to be described.
The aim of the study was to identify, using the HRT and the HFA, dissociating factors that confound the relationship between structural and functional progressive damage in patients with OAG and with “high‐risk” ocular hypertension (OHT).
Materials and methods
Material for the study was obtained from an on‐going prospective longitudinal investigation of structural and functional progression in OAG undertaken at the Glaucoma Out‐patients Clinic at Birmingham Heartlands Hospital, Birmingham, UK. A total of 23 patients (14 with OAG and 9 with “high‐risk” OHT) were identified who had been followed up for ⩾5 years (mean 78.4 months (SD 9.5), range 60–101 months). The mean number of examinations with the HRT was 5.45 (SD 0.8, range 4–7) and the mean number of examinations with the HFA was 7.41 (SD 1.4, range 5–10).
At entry into the study, all patients had exhibited a best‐corrected visual acuity of 6/9 or better and a distance refractive error within ±6DS and <2.5DC. The crystalline lens appearance, graded according to a photographic classification system, the Lens Opacity Classification System III,14 was not greater than Nuclear Colour 3, Nuclear Opalescence 3, Cortical 1 or Posterior Subcapsular 1. Two patients, one with OAG and one with OHT, were pseudophakic at the time of enrolment. None of the 23 patients were receiving systemic medication known to affect the visual field and none had a history of diabetes mellitus.
OAG was defined as a characteristic ONH appearance with, or without, a characteristic visual field defect by SAP and with, or without, elevated intraocular pressure (IOP). A characteristic ONH appearance was considered as one or more of the following: an increase in cup size, an increase in cup‐to‐disc (CD) ratio, disc asymmetry, changes in the lamina cribrosa, loss of neuroretinal rim, pallor, evidence of peripapillary atrophy, vessel changes or optic disc haemorrhage.15 A characteristic glaucomatous visual field defect was considered as a cluster of three or more locations, on the same side of the horizontal midline and in a location typical for OAG, exhibiting abnormality on two successive examinations by pattern deviation probability analysis at the p<0.05 level, with at least one location exhibiting abnormality at the p<0.01 level.16
High‐risk OHT was defined as a presenting IOP >24 mm Hg, or a presenting IOP ⩾22 mm Hg and a vertical CD ratio >0.5, or a presenting IOP ⩾22 mm Hg, a vertical CD ratio <0.5 and a family history of OAG. The IOP was not corrected for the effects of central corneal thickness (CCT).
None of the patients had a history of other ocular disorder, with the exception of pseudophakia, and all had undertaken at least one examination with SAP before enrolment. One eye from each patient had been examined for the study: the eye with the more advanced glaucomatous disease or, for the participants with OHT, the eye with the greatest risk of developing OAG.
At baseline, each participant had undergone, at each of two sessions separated by a 2‐week interval, imaging of the ONH using the HRT I and visual field examination using SAP with HFA Program 24‐2 and either the Full Threshold or the Swedish Interactive Threshold Standard algorithm. Once commercially available, the HRT II was used for all follow‐up examinations. The follow‐up intervals for HRT and visual field examination were determined in accordance with the management criteria of the lead clinician (IAC).
The study had approval from the Research and Ethics committee of Birmingham Heartlands and Solihull (Teaching) NHS Trust, Birmingham, UK, and all patients had given written informed consent.
Structural progression was assessed using the Topographic Change Analysis (TCA) for the HRT II (software V.1.7). The TCA identifies significant reductions in the topographic height from the mean retinal height of two baseline examinations (p<0.05) by means of a probability map, which superimposes magenta superpixels onto the corresponding region of the reflectance image. Structural progression was defined as a cluster of at least 20 magenta superpixels (1 superpixel describes an area of 4×4 pixels) present in each of 3 consecutive images.13
Functional progression was assessed using the Glaucoma Progression Analysis (GPA) of the HFA. The GPA defines “likely” visual field progression when three stimulus locations exhibit significant reductions (p<0.05) in sensitivity from a baseline comprising the average of two examinations, by Pattern Deviation analysis, on at least each of three consecutive examinations.11 By employing Pattern Deviation analysis, the GPA separates visual field changes due to progressive OAG from those due to increasing media opacity.9
Table 1 specifies the group mean age, mean duration of follow‐up, mean number of examinations with the HRT and HFA, and mean interval between examinations for each of the two groups.
Table 1 Demographic characteristics of the cohort.
| OAG (n = 14) | OHT (n = 9) | |
|---|---|---|
| Age (range), years | 69.0 (9.5); (51–80) | 63.8 (12.2); (46–85) |
| Duration of follow‐up, months | 77.2 (10.0) | 80 (9.0) |
| Number of examinations | ||
| HRT | 5.6 (0.8) | 5.3 (0.9) |
| HFA | 7.5 (1.3) | 6.9 (1.3) |
| Interval between examinations, months | ||
| HRT | 13.8 (3.1) | 15 (2.7) |
| HFA | 10.3 (6.0) | 11.6 (7.0) |
HFA, Humphrey Field Analyser; HRT, Heidelberg Retina Tomograph; OAG, open‐angle glaucoma; OHT, ocular hypertension.
Values are mean (SD).
The mean ONH area for those with OAG, derived by the HRT II, was 2.11 mm2 (SD 0.38; range 1.67–2.90 mm2) and for those with OHT 2.19 mm2 (SD 0.37; range 1.74–2.79 mm2). Of the 14 patients with OAG, 7 exhibited a small (<1.99 mm2)17 and 7 a normal‐sized ONH (2–3 mm2). Four of the nine patients with OHT had a small and five had a normal‐sized ONH. The vertical CD ratio in the four patients with OHT and a small ONH ranged from 0.5 to 0.7.
Results
Structural and functional concordance
Six patients (two with OAG and four with OHT) were stable by both TCA and GPA.
Four patients exhibited progression by both techniques (three with OAG and one with OHT). Topographical correspondence between the visual field progression and the ONH progression was present in all four patients.
Structural progression only
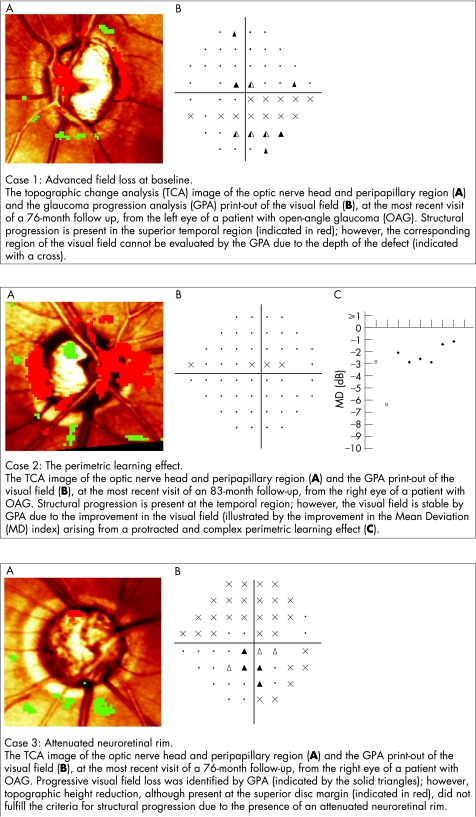
Five patients with OAG and two with OHT exhibited progression by TCA only. Four of these seven patients manifested localised field loss, designated as “out of range” by GPA, which corresponded to the region of structural progression (fig 1, case 1). An out‐of‐range designation indicates that the measured sensitivity at the given location is associated with a wide range of test‐retest variability such that the statistical cut‐off for progressive field loss lies beyond the maximum stimulus luminance of the HFA. Such locations are excluded by the GPA from the analysis of progressive field loss.
Figure 1 Three types of dissociating factor influencing the relationship between structural and functional progression. Top panel: Deep localised visual field loss. Middle panel: The perimetric learning effect. Bottom panel: A grossly attenuated neuroretinal rim.
Of the remaining three patients, one exhibited functional progression over the last two visits of the series, and thus did not meet the GPA criterion for “likely” progressive damage, and one showed a protracted perimetric learning effect (fig 1, case 2). No explanation could be found for the lack of functional progression in the remaining patient.
Functional progression only
Four patients with OAG and two with OHT exhibited progression by GPA only. All four of the patients with OAG exhibited an extensively cupped ONH at baseline (one or more HRT sectors exhibiting a neuroretinal rim area‐to‐disc area ratio of ⩽0.2). The attenuated rim width reduced the available area for assessment of reduction in the topographical height within the ONH. Advanced OAG also reduces the available height of the peripapillary retina. Thus, structural progression with the HRT becomes more difficult to determine as the disease advances (fig 1, case 3).
In the two patients with OHT, no explanation could be found for the lack of structural progression. One patient with OAG and one with OHT underwent four HRT examinations; both exhibited functional progression in the presence of stable structural damage at each of the two follow‐up examinations.
Discussion
The study has identified three dissociating factors attributable to either TCA or GPA that limit the identification of progressive damage to the ONH or visual field, respectively. These three factors accounted for 9 of the 13 patients who exhibited a lack of concordance between the two analytical techniques.
The three factors may explain some of the discordance between the TCA and HFA glaucoma change probability (based on Total Deviation analysis) progression analyses in a larger cohort study over a similar follow‐up period.12,13
The dissociating factor for the HRT (fig 1, case 3) is in addition to the limitation arising from suboptimal image quality due to factors such as media opacity, fixation instability and pupil miosis, which also impair the identification of progressive damage.18 The manufacturer of the HRT defines “high quality” images as those exhibiting a standard deviation for the height measurements of ⩽30 μm. All images in the study were within this magnitude. It would be expected that the sensitivity of TCA to identify progression would decline with reduction in HRT image quality even within the acceptable range of image quality.
The detection of functional progression with the HFA is limited by the two dissociating factors illustrated in fig 1, cases 1 and 2. Inability to evaluate progressive loss at a stimulus location designated as out of range could conceivably be overcome by the use of a size V stimulus. Such an approach would require the development of a new GPA based on the larger stimulus size.
Caution should be exercised when accepting baseline data for use with GPA, particularly in patients inexperienced in SAP. The GPA alerts the clinician to a statistically significant learning effect between the first two examinations and, in such cases, recommends that the second and third examinations be used as the baseline. However, the appropriate baseline fields for GPA should only be designated when it is apparent that the learning effect is no longer operative. The learning effect can last beyond the third examination and, as illustrated in case 2, can be associated with large variations in Mean Deviation.
The time to detection of progressive functional damage should also, theoretically, be retarded by any examination in the series deemed to be unreliable on the basis of an unacceptable number of incorrect responses to one or more of the various catch trials. With the exception of those examinations exhibiting ⩾15% incorrect responses to the false‐positive catch trials, recorded by either of the Swedish Interactive Threshold Algorithms, which are excluded from the baseline, the GPA software incorporates all other examinations into the analysis irrespective of reliability outcome. The criteria for low reliability for any given type of catch trial are empirically derived, and the utility of incorporating an unreliable field into the GPA analysis is yet to be determined. In this study, all patients exhibited reliable responses to the false‐negative (⩽30%) and false‐positive (⩽15%) catch trials across all examinations. Six patients each exhibited one examination at which the incorrect responses to the fixation loss catch trials was beyond 30%. One patient with OAG exhibited an unacceptable number of incorrect responses to the fixation loss catch trials in 7 of 10 examinations. This was attributed to difficulty in locating the blind spot, which was, in turn, due to difficulty in fixating as a consequence of a small focal defect close to the macula; however, fixation mediated by the gaze tracker was stable. This patient was stable by GPA, owing to the depth of the central focal defect lying out of range, but showed structural progression by TCA.
Topographical correspondence of the ONH and visual field was present in all four patients exhibiting both structural and functional progression. The topographical relationship between structural damage to the ONH and functional damage to the visual field has been investigated previously.19,20 Although the findings in this study do not further the understanding of the topographical correspondence in progressive OAG, they do serve to corroborate the likelihood of “true” progression having occurred in these four patients.
The TCA and GPA criteria for the identification of structural and functional progression, respectively, do not consider the severity of the disease. The reduction in sensitivity, in dBs, for each retinal ganglion cell lost in OAG, increases exponentially as the total number of remaining ganglion cells declines.21 Thus, the amount of structural damage producing an equivalent amount of functional damage will vary depending on the severity of the condition. The amount of neuronal damage required to produce a given functional deficit is likely to be smaller in advanced stages of OAG than in earlier stages. This invariance is likely to further explain, in addition to that arising from the lack of remaining neuroretinal rim, the apparent insensitivity of the TCA to identify structural progression in advanced ONH damage. The current TCA software (V.3.0) is unlikely to overcome these issues.
The presence of an ONH haemorrhage is associated with progressive OAG.22 None of the 23 patients exhibited an ONH haemorrhage at any of the follow‐up examinations.
Three patients (two with OAG and one with OHT) underwent cataract extraction and intraocular lens implantation during the study. The visual acuity immediately before surgery in these three patients was 6/18, 6/12 and 6/9, respectively. A further patient with OAG, pseudophakic at the time of enrolment, underwent a capsulotomy following a decline in acuity to 6/18. All four patients exhibited functional progression only; the outcomes of the structural and functional evaluations were independent of the media quality at any evaluation and of the time series at which the surgical intervention occurred. Of the remaining 19 patients, 5 exhibited no change between the entry and exit acuities, 13 a one‐line or less reduction, and one a two‐line reduction.
CCT was not measured at baseline or at follow‐up.23 At the time of enrolment, all nine patients with OHT were receiving medical treatment as a consequence of a presenting IOP of ⩾26 mm Hg. Therefore, to exhibit an IOP within the normal range, these nine patients would have to have manifested a CCT approximately 4.8 standard deviations above the mean CCT of the normal population.24,25
In summary, the three dissociating factors identified in this study highlight some of the potential limitations of TCA and GPA in the identification of progressive structural and functional glaucomatous damage. Two of the three dissociating factors arise from an interaction of the analytical technique with the severity of the OAG.
Abbreviations
CCT - central corneal thickness
CD - cup‐to‐disc
GPA - Glaucoma Progression Analysis
HFA - Humphrey Field Analyser
HRT - Heidelberg Retina Tomograph
IOP - intraocular pressure
OAG - open‐angle glaucoma
OHT - ocular hypertension
ONH - optic nerve head
SAP - standard automated perimetry
TCA - Topographic Change Analysis
Footnotes
Competing interests: JMW has received Honoraria from Carl Zeiss for occasional lectures.
References
- 1.Quigley H A, Addicks E M, Green W R. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol 1982100135–146. [DOI] [PubMed] [Google Scholar]
- 2.Caprioli J. Automated perimetry in glaucoma. Am J Ophthalmol 1991111235–239. [DOI] [PubMed] [Google Scholar]
- 3.Bowd C, Zangwill L M, Medeiros F A.et al Confocal scanning laser ophthalmoscopy classifiers and stereophotograph evaluation for prediction of visual field abnormalities in glaucoma‐suspect eyes. Invest Ophthalmol Vis Sci 2004452255–2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sihota R, Sony P, Gupta V.et al Diagnostic capability of optical coherence tomography in evaluating the degree of glaucomatous retinal nerve fiber damage. Invest Ophthalmol Vis Sci 2006472006–2010. [DOI] [PubMed] [Google Scholar]
- 5.Saito H, Tomidokoro A, Sugimoto E.et al Optic disc topography and peripapillary retinal nerve fiber layer thickness in nonarteritic ischemic optic neuropathy and open‐angle glaucoma. Ophthalmology 20061131340–1344. [DOI] [PubMed] [Google Scholar]
- 6.Cvenkel B. Retinal thickness at the posterior pole in glaucoma and ocular hypertension. Graefes Arch Clin Exp Ophthalmol 2004242920–925. [DOI] [PubMed] [Google Scholar]
- 7.The AGIS Investigators Advanced Glaucoma Intervention Study. 2. Visual field test scoring and reliability. Ophthalmology 19941011445–1455. [PubMed] [Google Scholar]
- 8.Katz J. Scoring systems for measuring progression of visual field loss in clinical trials of glaucoma treatment. Ophthalmology 1999106391–395. [DOI] [PubMed] [Google Scholar]
- 9.Bengtsson B, Lindgren A, Heijl A.et al Perimetric probability maps to separate change caused by glaucoma from that caused by cataract. Acta Ophthalmol Scand 199775184–188. [DOI] [PubMed] [Google Scholar]
- 10.Gordon M O, Kass M A. The Ocular Hypertension Treatment Study: design and baseline description of the participants. Arch Ophthalmol 1999117573–583. [DOI] [PubMed] [Google Scholar]
- 11.Heijl A, Leske M C, Bengtsson B.et al Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Ophthalmol Scand 200381286–293. [DOI] [PubMed] [Google Scholar]
- 12.Artes P H, Chauhan B C. Longitudinal changes in the visual field and optic disc in glaucoma. Prog Retin Eye Res 200524333–354. [DOI] [PubMed] [Google Scholar]
- 13.Chauhan B C, McCormick T A, Nicolela M T.et al Optic disc and visual field changes in a prospective longitudinal study of patients with glaucoma: comparison of scanning laser tomography with conventional perimetry and optic disc photography. Arch Ophthalmol 20011191492–1499. [DOI] [PubMed] [Google Scholar]
- 14.Chylack L T, Jr, Wolfe J K, Singer D M.et al The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 1993111831–836. [DOI] [PubMed] [Google Scholar]
- 15.Airaksinen P J, Tuulonen A, Werner E B. Clinical evaluation of the optic disc and retinal nerve fibre layer. In: Ritch R, Shields B, Krupin T, eds. The glaucomas basic sciences. 2nd edn. St Louis, MI: Mosby‐Year Book, 1996
- 16.Hodapp E, Parrish RK I I, Anderson D R. The asymptomatic patient with elevated pressure. In: Craven L, ed. Clinical decisions in Glaucoma. St Louis, MI: Mosby‐Year Book, 1993
- 17.Iester M, Mickelberg F S, Drance S M. The effect of optic disc size on diagnostic precision with the Heidelberg Retina Tomograph. Ophthalmology 1997104545–548. [DOI] [PubMed] [Google Scholar]
- 18.Zangwill L, Irak I, Berry C C.et al Effect of cataract and pupil size on image quality with confocal scanning laser ophthalmoscopy. Arch Ophthalmol 1997115983–990. [DOI] [PubMed] [Google Scholar]
- 19.Bowd C, Zangwill L M, Medeiros F A.et al Structure‐function relationships using confocal scanning laser ophthalmoscopy, optical coherence tomography, and scanning laser polarimetry. Invest Ophthalmol Vis Sci 2006472889–2895. [DOI] [PubMed] [Google Scholar]
- 20.Garway‐Heath D F, Poinoosawmy D, Fitzke F W.et al Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology 20001071809–1815. [DOI] [PubMed] [Google Scholar]
- 21.Harwerth R S, Carter‐Dawson L, Smith EL I I I.et al Neural losses correlated with visual losses in clinical perimetry. Invest Ophthalmol Vis Sci 2004453152–3160. [DOI] [PubMed] [Google Scholar]
- 22.Kim S H, Park K H. The relationship between recurrent optic disc hemorrhage and glaucoma progression. Ophthalmology 2006113598–602. [DOI] [PubMed] [Google Scholar]
- 23.Gordon M O, Beiser J A, Brandt J D.et al The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open‐angle glaucoma. Arch Ophthalmol 2004122714–720. [DOI] [PubMed] [Google Scholar]
- 24.Gunvant P, O'Leary D J, Baskaram M.et al Evaluation of tonometric correction factors. J Glaucoma 200514337–343. [DOI] [PubMed] [Google Scholar]
- 25.Feltgen N, Leifert D, Funk J. Correlation between central corneal thickness, applanantion tonometry, and direct intracameral IOP readings. Br J Ophthalmol 20018585–87. [DOI] [PMC free article] [PubMed] [Google Scholar]