Optical coherence tomography (OCT) is a noninvasive optical imaging technique that provides high‐resolution, cross‐sectional, in vivo imaging of the human retina from which estimates of retinal layers thickness can be made.1 OCT is capable of scanning the peripapillary retina, optic nerve head (ONH), and macular region. Previous studies have documented the ability of OCT to image the retinal nerve fibre layer (RNFL) of patients with glaucoma or other optic neuropathies including indirect optic nerve trauma.2,3,4
Although OCT has for the most part been used to evaluate RNFL thickness, recent software improvements have made it possible to measure macular thickness as well. The purpose of this paper is to report a case of indirect optic nerve injury which illustrates the efficacy of macular thickness measurements in documenting progressive neural damage in a longitudinal study using OCT.
Case report
A 25‐year‐old woman was admitted to the hospital after injuring her right temple in a car accident. Her visual acuity was hand motion in the right eye (OD) and 20/20 in the left eye, with moderate periorbital edema in OD. The slitlamp examination disclosed only a mild subconjunctival hemorrhage in OD. The ocular motility was normal and the intraocular pressure was 12 mm Hg in both eyes. Pupils were equal in size and a 2+ relative afferent defect was observed in OD. The fundus examination was normal in both eyes. A computed tomographic scan of the head and orbits detected multiple fractures at the right optic canal area. Indirect optic nerve trauma was diagnosed and the patient was treated with high‐dose intravenous steroids. Visual acuity improved to 20/200 in OD but a dense visual field defect remained and moderate optic disc pallor developed.
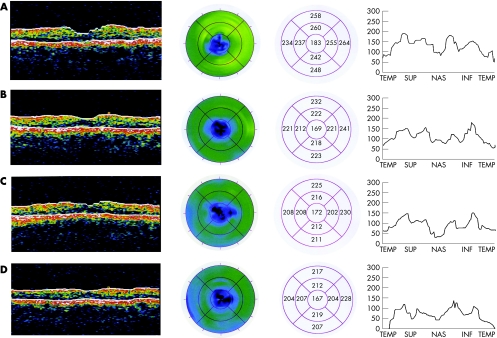
Macular thickness measurements based on radial scans passing through the fovea and peripapillary RNFL measurements using optical coherence tomography (OCT, Carl Zeiss Meditec, Inc., Dublin, CA) were taken at 7 days, 28 days, 49 days, and 77 days after injury. A progressive macular thinning could be detected on the macular scan, the color‐coded map and the macular thickness map (figs 1A‐D). Concomitantly to macular thinning, a marked decrease in peripapillary RNFL thickness measured by OCT was observed in the RNFL thickness profile (fig 1).
Figure 1 Optical coherence tomography scans on days 7 (A), 28 (B), 49 (C) and 77 (D) after injury. There is progressive thinning of the macular thickness as shown by the (left) color‐coded map, by (left circle) the color‐coded circle and by (right circle) the mean macular thickness measurements. There is also progressive loss of peripapillary nerve fibers as shown by the (right) retinal nerve fiber layer thickness profile.
Comment
As the ganglion cell layer accounts for up to 40% of the thickness in the macular area, estimates of macular thickness could be considered as a surrogate for the determination of ganglion cell loss. In fact, previous studies have shown that OCT macular thickness measurements are significantly thinner in glaucomatous compared with healthy eyes.5,6,7,8 However, no study has yet evaluated the role of macular thickness measurements in conditions associated with acute ganglion cell loss, such as optic nerve trauma. Previous studies have documented peripapillary RNFL thickness reduction after indirect traumatic optic neuropathy.4,9 Our case is interesting because it draws attention to the fact that macular thickness measurements may also be a potential indicator of neural damage in the eye and may prove to have clinical value in the detection of damage and monitoring of patients with acute and chronic optic neuropathies.
References
- 1.Huang D, Swanson E A, Lin C P.et al Optical coherence tomography. Science 19912541178–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medeiros F A, Zangwill L M, Bowd C.et al Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol 2004122827–837. [DOI] [PubMed] [Google Scholar]
- 3.Monteiro M L, Leal B C, Rosa A A.et al Optical coherence tomography analysis of axonal loss in band atrophy of the optic nerve. Br J Ophthalmol 200488896–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medeiros F A, Moura F C, Vessani R M.et al Axonal loss after traumatic optic neuropathy documented by optical coherence tomography. Am J Ophthalmol 2003135406–408. [DOI] [PubMed] [Google Scholar]
- 5.Greenfield D S, Bagga H, Knighton R W. Macular thickness changes in glaucomatous optic neuropathy detected using optical coherence tomography. Arch Ophthalmol 200312141–46. [DOI] [PubMed] [Google Scholar]
- 6.Lederer D E, Schuman J S, Hertzmark E.et al Analysis of macular volume in normal and glaucomatous eyes using optical coherence tomography. Am J Ophthalmol 2003135838–843. [DOI] [PubMed] [Google Scholar]
- 7.Guedes V, Schuman J S, Hertzmark E.et al Optical coherence tomography measurement of macular and nerve fiber layer thickness in normal and glaucomatous human eyes. Ophthalmology 2003110177–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medeiros F A, Zangwill L M, Bowd C.et al Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol 200513944–55. [DOI] [PubMed] [Google Scholar]
- 9.Medeiros F A, Susanna R., Jr Retinal nerve fiber layer loss after traumatic optic neuropathy detected by scanning laser polarimetry. Arch Ophthalmol 2001119920–921. [DOI] [PubMed] [Google Scholar]