Abstract
Aim
To determine the prevalence and causes of visual impairment and blindness in the Sistan‐va‐Baluchestan Province of Iran.
Methods
A population‐based cross‐sectional study with a multistage cluster sampling technique was used to identify the study subjects. Visual acuity (VA) was defined for all participants aged ⩾10 years. Participants with a VA of <20/60 were examined by an ophthalmologist to determine the causes of low vision or blindness.
Results
5446 (84.0%) of the invited people were examined. The prevalence of visual impairment (VA <20/60) was 6.81% (95% CI 5.91% to 7.71%) and of bilateral blindness (VA <3/60) was 0.79% (95% CI 0.50% to 1.08%). Visual impairment increased with age and illiteracy. Bilateral blindness doubled in women aged >40 years. The causes of visual impairment and blindness were cataract (37.7%), corneal opacity (15.0%), amblyopia (15.0%), glaucoma (5.7%) and hyperopia (5.0%). 39.5% of the visual impairment cases were potentially curable.
Conclusion
The estimated magnitude of visual impairment and blindness was much higher than our expectations. Further investigation of the pattern of vision loss in women and children, particularly as a result of trachoma and amblyopia, is warranted. Implementation of measures to treat curable cases of the study population can improve the situation in the region dramatically.
According to the World Health Organization, 37 million people are blind and 124 million have visual impairement worldwide.1 Blindness and visual impairment represent a public health, social and economic problem for countries, especially developing countries, where 9 of 10 of the world's blind people live. Moreover, there is increasing evidence that women have a disproportionately higher burden of visual disability.2 Every minute, one child becomes blind somewhere in the world. Half of these cases are curable or preventable, which means that blindness can be prevented in about 250 000 children every year.3 Approximately 50% of the world's blind have cataract. As an age‐related disease, cataract is a disease of the older population, but childhood blindness accounts for almost as many “blind years” as cataract, even though many of its causes are either preventable or treatable.4
Recently, several studies were initiated in Iran, the largest being the Tehran Eye Study that analysed the causes of blindness in the densely populated capital of Iran.5,6
The main objective of the present study was to determine the prevalence and causes of visual impairment and blindness in Sistan‐va‐Baluchestan Province, one of the most underprivileged regions of the country.
Materials and methods
Study site and population
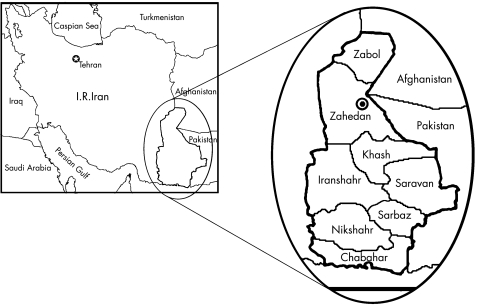
The study was carried out in the Sistan‐va‐Baluchestan Province in the southwest of Iran. The Province is located in the neighbourhood of Afghanistan and Pakistan to the east. According to the last population census of 1996, 52.7% of the population lives in the rural regions. In all, 1.1% of the population is composed of nomads who are scattered all over the Province. The Province territory is divided into eight districts. Zahedan, the largest district with a population of about 620 000 (95% of them residing in the urban regions), is the capital of the Province (fig 1). The median of the age distribution of the population is about 16.5 years.
Figure 1 Map of Iran and Sistan‐va‐Baluchestan Province.
The primary healthcare network, with a stepwise structure consisting of rural health houses, rural and urban health clinics and general district hospitals and headquarters of the district health centre, has a coverage of about 65% in some districts to >95% in some others. The entire primary healthcare network is under the supervision of the Zahedan University of Medical Sciences. Four of the districts have at least one ophthalmologist and one or two optometrists and the others have only optometrists.
Sample size and sampling
There was no area restriction for sampling and the sampling method was the classic probability‐proportional‐to‐size cluster sampling. To determine the sample size, we estimated the prevalence of visual impairment (<20/60) to be 8% for people aged ⩾10 years. We assumed a design effect of 1.5 (for cluster sampling), a confidence interval (CI) of 95% and a response rate of 90%. These assumptions led to a sample size of 4713. Considering an average household size of 5 individuals (with at least 2.5 eligible people in each household) and a cluster size of 10 households, about 190 clusters were needed to generate the sampled population.
A cumulative list of the study population was produced and a systematic sample from a random start was selected. We obtained the sampling interval by dividing the total population of the communities by the number of communities to be selected. Then we chose a random number between one and the result of the division. This should be fitted into position in the list to identify the first community in the sample. Then, by adding the sampling interval to the initial random number, the other communities were selected. In all districts there is a nearly complete health register of all households and household members. From each selected community we chose the first household of the cluster at random. Enumeration was continued for 10 neighbouring households by proceeding systematically in a clockwise direction from the initial household within the cluster.
All the study staff including the optometrists and ophthalmologists took part in training sessions before the initiation of the survey. There were four teams, each being lead by an optometrist and assisted by an expert health worker from the headquarters of each district health centre.
Definitions
The following definitions were used for classification of the patients:
Visual impairment: a visual acuity (VA) of <20/60 using a pinhole. Visual impairment was categorised to blindness and low vision.
Blindness: a VA of <3/60 in the better eye using a pinhole.
Low vision: a VA of <20/60 to 3/60 using a pinhole.8
In this way each participant was categorised into one the following groups:
normal vision in both eyes: corrected VA >20/60 in both eyes (with pinhole)
unilateral low vision: VA >20/60 in one eye and low vision (VA between 20/60 and 3/60 with pinhole) in another
blindness in one eye (VA <3/60 with pinhole) and normal vision in the other (VA >20/60 with pinhole)
blindness in one eye (VA <3/60 with pinhole) and low vision (VA between 20/60 and 3/60 with pinhole) in the other
bilateral low vision: VA <20/60 to 3/60 with pinhole in both eyes
bilateral blindness: VA <3/60 with pinhole in both eyes.
Examinations
The steps involved in the study were as follows. All selected households were enumerated. Enumeration included name, age, sex and education level of each household member. After enumeration, all household members who were aged ⩾10 years were invited to visit a local clinic (usually a rural health house, or urban and rural health clinic) where VA was measured. Enumerated subjects who did not attend the examination process after the initial invitation were contacted twice in the subsequent week by a local health worker in charge of the local health services. Those who failed to appear even after the third invitation were considered non‐respondents. There was no replacement for non‐participation. Participants who were too ill to come to the clinic were visited in their home, by a team composed of a local health worker and an optometrist.
VA was measured using an “E” chart in outdoor light at 6 m. Individuals with VA <20/60 were rechecked with pinhole, and if improved, the improved VA was recorded. An ophthalmologist examined all participants with VA <20/60 (with a time lag of at most 1 week in the nearest hospital) using an ophthalmoscope, a biomicroscope (slit lamp) and an applanation tonometer to find the main causes of blindness and low vision.
Humanity and ethics
The research and ethics committee of the Al‐Zahra Eye Centre and ethics committee of the Zahedan University of Medical Sciences approved the study. All subjects included in this study were informed about the project and the procedures in their native language before being enrolled. The participant's agreement for examination was obtained verbally.
Data analysis
A computerised data bank was produced based on the completed data sheets. The data were analysed using SPSS V.9.0 and Stata statistical software, V.6.0. The prevalence of visual impairment and blindness were estimated, and multiple logistic regression modelling was used to investigate associations with age, sex and education level. Rates have been age and sex standardised to the results of the last national census of 1996 by the direct method.7
In calculating standard errors and 95% CI, the cluster sampling design was taken into account and adjusted for.9 The 95% CIs were calculated by assuming a normal approximation of binomial distribution for rates with five or more outcome observations, and a Poisson distribution for rates with fewer outcome observations. All p values <0.05 were considered significant.
Results
From October 2004 to November 2005, 5446 of 6483 (84.0%) individuals invited for examinations came to the clinic and were examined. Table 1 shows the response rate by districts of the Sistan‐va‐Baluchestan Province. The last district that had to be sampled was Khash with a population of about 80 000. Since the examined people in the other districts had outnumbered the estimated required sample size, Khash was not sampled. The mean age of men and women up to one decimal point is equal to each other (27.7 years) and the SEs of the mean, respectively, are 0.35 and 0.27.
Table 1 Response rate of study population.
| District | Invited | Examined | Response rate (%) |
|---|---|---|---|
| Zahedan | 2044 | 1664 | 81.41 |
| Zabol | 1420 | 1199 | 84.44 |
| Iranshahr | 820 | 793 | 96.71 |
| Saravan | 645 | 563 | 87.29 |
| Sarbaz | 354 | 342 | 96.61 |
| Nikshahr | 604 | 355 | 58.77 |
| Chabahar | 596 | 530 | 88.93 |
| Total | 6483 | 5446 | 84.00 |
Considering the corrected vision (using a pinhole), the estimated prevalence of visual impairment would be 6.81% (95% CI 5.91 to 7.71). Table 2 shows the prevalence of visual impairment by age and sex categories, based on the corrected vision and adjusted for age and sex distribution of the last national census of 1996.7
Table 2 Prevalence of visual impairment, low vision and blindness by sex and age, based on corrected visual acuity (using pinhole)*.
| Age groups (years) | Number of participants | Visual impairment | One eye blind and the other normal | Both eyes blind | One eye low vision and the other normal | One eye blind and the other with low vision | Both eyes low vision | |
|---|---|---|---|---|---|---|---|---|
| Men | 10–19 | 1067 | 1.59 (0.81 to 2.37) | 0.56 (0.05 to 1.07) | 0.09 (0.01 to 0.68) | 0.75 (0.24 to 1.26) | 0.00 (0.00 to 0.00) | 0.19 (0.05 to 0.76) |
| 20–39 | 754 | 2.78 (1.60 to 3.96) | 1.19 (0.43 to 1.95) | 0.27 (0.04 to 1.92) | 0.93 (0.26 to 1.60) | 0.13 (0.02 to 0.95) | 0.27 (0.07 to 1.08) | |
| 40–59 | 351 | 6.84 (4.12 to 9.56) | 1.14 (0.43 to 3.05) | 0.28 (0.04 to 2.05) | 3.42 (1.40 to 5.44) | 0.57 (0.14 to 2.29) | 1.42 (0.20 to 2.64) | |
| >60 | 172 | 48.26 (40.32 to 56.20) | 7.56 (3.84 to 11.28) | 5.81 (2.36 to 9.26) | 12.21 (7.76 to 16.66) | 6.98 (3.00 to 10.96) | 15.70 (9.78 to 21.62) | |
| Women | 10–19 | 1240 | 1.45 (0.74 to 2.16) | 0.32 (0.12 to 0.85) | 0.00 (0.00 to 0.00) | 0.81 (0.28 to 1.34) | 0.00 (0.00 to 0.00) | 0.32 (0.12 to 0.85) |
| 20–39 | 1189 | 3.03 (1.95 to 4.11) | 0.92 (0.39 to 1.45) | 0.08 (0.01 to 0.60) | 1.26 (0.50 to 2.02) | 0.00 (0.00 to 0.00) | 0.76 (0.13 to 1.39) | |
| 40–59 | 523 | 11.47 (8.77 to 14.17) | 3.44 (1.97 to 4.91) | 0.57 (0.19 to 1.78) | 3.63 (2.14 to 5.12) | 1.15 (0.11 to 2.19) | 2.68 (1.39 to 3.97) | |
| >60 | 150 | 58.00 (49.91 to 66.09) | 6.67 (2.85 to 10.49) | 12.67 (6.69 to 18.65) | 13.33 (7.90 to 18.76) | 8.00 (3.81 to 12.19) | 17.33 (11.12 to 23.54) | |
| Men and women | 10–19 | 2307 | 1.51 (0.98 to 2.04) | 0.42 (0.15 to 0.69) | 0.04 (0.01 to 0.29) | 0.78 (0.39 to 1.17) | 0.00 (0.00 to 0.00) | 0.26 (0.02 to 0.50) |
| 20–39 | 1943 | 2.93 (2.19 to 3.67) | 1.04 (0.61 to 1.47) | 0.16 (0.04 to 0.71) | 1.12 (0.61 to 1.63) | 0.06 (0.01 to 0.40) | 0.55 (0.16 to 0.94) | |
| 40–59 | 874 | 9.40 (7.42 to 11.38) | 2.41 (1.45 to 3.37) | 0.44 (0.17 to 1.18) | 3.54 (2.32 to 4.76) | 0.89 (0.22 to 1.56) | 2.12 (1.20 to 3.04) | |
| >60 | 322 | 53.07 (46.90 to 59.24) | 7.12 (4.38 to 9.86) | 9.20 (5.40 to 13.00) | 12.76 (9.15 to 16.37) | 7.48 (4.48 to 10.48) | 16.50 (11.99 to 21.01) | |
| Men | All ages | 2344 | 6.69 (5.49 to 7.89) | 1.46 (0.97 to 1.95) | 0.66 (0.29 to 1.03) | 2.16 (1.53 to 2.79) | 0.71 (0.34 to 1.08) | 1.70 (1.11 to 2.29) |
| Women | All ages | 3102 | 6.90 (5.80 to 8.00) | 1.37 (0.98 to 1.76) | 0.89 (0.50 to 1.28) | 2.14 (1.57 to 2.71) | 0.65 (0.32 to 0.98) | 1.86 (1.33 to 2.39) |
| All | All ages | 5446 | 6.81 (5.91 to 7.71) | 1.40 (1.09 to 1.71) | 0.79 (0.50 to 1.08) | 2.15 (1.70 to 2.60) | 0.68 (0.43 to 0.93) | 1.79 (1.36 to 2.22) |
Values are presented as percentage (95% CI).
*Age and sex standardised to the 1996 national census results in the Province.
Multivariate analysis of the relationship between visual impairment and age, sex and education level, using logistic regression modelling, shows a positive relationship between the chance of having visual impairment with age and a negative relationship with education level (table 3). Table 4 compares the education levels of normal participants and those with visual impairement. There was no relationship between sex and visual impairment, nor between the prevalence of visual impairment and the area of residence (rural or urban).
Table 3 Relationship between age, sex and education level with visual impairment.
| OR* (95% CI) | |
|---|---|
| Age groups (years) | |
| 10–19 | 1 |
| 20–39 | 1.38 (0.88 to 2.17) |
| 40–59 | 3.43 (2.14 to 5.49) |
| >60 | 31.13 (19.01 to 50.97) |
| Sex | |
| Men | 1 |
| Women | 1.10 (0.84 to 1.44) |
| Education (years)† | |
| 0 | 1 |
| 1–5 | 0.42 (0.27 to 0.64) |
| 6–12 | 0.31 (0.20 to 0.48) |
| >12 | 0.45 (0.18 to 1.13) |
*Adjusted odds ratio (logistic regression).
†Years of successful education.
Table 4 Education level of the study population by involvement.
| Education | Normal | Visual impairment | Total |
|---|---|---|---|
| Illiterate | 1368 (26.8) | 263 (78.5) | 1631 (30.0) |
| 1–5 years | 1370 (26.9) | 33 (9.9) | 1403 (25.8) |
| 6–12 years | 2194 (43.1) | 34 (10.1) | 2228 (41.0) |
| >12 years | 163 (3.2) | 5 (1.5) | 168 (3.1) |
| Total | 5095 (100.0) | 335 (100.0) | 5430 (100.0) |
Table 5 shows the frequency of different causes of visual impairment. It is worth mentioning that final examination by an ophthalmologist (for definition of causes of visual impairment) was not possible in three districts, Nikshahr, Saravan and Sarbaz, owing to lack of facilities. Table 6 shows the age distribution of the most prevalent problems. Both cataract and corneal opacity showed the highest proportions in the age group >40 years. For corneal opacity the age group <20 years had higher involvement that may have been due to infection such as trachoma.
Table 5 Causes of visual impairment based on corrected vision (pinhole)*.
| Problem | n | % |
|---|---|---|
| Cataract | 106 | 37.72 |
| Corneal opacity | 42 | 14.95 |
| Amblyopia | 42 | 14.95 |
| Other lens problems | 19 | 6.76 |
| Retinitis pigmentosa | 3 | 1.07 |
| Retina detachment | 3 | 1.07 |
| Macular scar | 9 | 3.20 |
| Other retinal problems | 21 | 7.47 |
| Glaucoma | 16 | 5.69 |
| Hyperopia | 14 | 4.98 |
| Optic atrophy | 3 | 1.07 |
| Pterygium | 1 | 0.36 |
| Irregular astigmatism | 1 | 0.36 |
| Refractive error hypermetropia | 1 | 0.36 |
| Total | 281 | 100.00 |
*These data belong to four districts (Zahedan, Zabol, Iranshahr and Chabahar).
Table 6 Causes of visual impairment by age group*.
| Age groups (years) | Opacity, n (%) | Amblyopia, n (%) | Cataract, n (%) | Others, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| 10–19 | 3 (12.0) | 6 (24.0) | 2 (8.0) | 14 (56.0) | 25 (100) |
| 20–39 | 3 (8.8) | 15 (44.1) | 4 (11.8) | 12 (35.3) | 34 (100) |
| 40–59 | 12 (19.4) | 13 (21.0) | 26 (41.9) | 11 (17.7) | 62 (100) |
| >60 | 24 (18.9) | 8 (6.3) | 74 (58.3) | 21 (16.5) | 127 (100) |
| All | 42 (16.9) | 42 (16.9) | 106 (42.7) | 58 (23.4) | 248 (100) |
*Patients of Saravan, Nikshahr and Sarbaz did not pass the final examinations by ophthalmologist.
Discussion
The results of this study provide valuable population‐based data on the prevalence and causes of visual impairment and blindness in one of the deprived societies of Iran. A high response rate among invited people (84.0%) and the representativeness of the enumerated sample were acceptable. As table 1 shows, Nikshahr had the lowest response rate (58.8%). This low response rate was due to some local problems with transportation facilities in the outskirts. Since the size of examined people in the first seven districts outnumbered the required sample size, the Khash district (with a population of about 80 000) was not sampled. The probable reason for this situation could be our mistakes in the estimation of household size (household size of 5) and in the number of eligible people in each household (2.5 people in each household).
The methods of sampling and criteria for classification of the cases are similar to those of the Tehran Eye Study.5 Table 7 compares the results of the present study with those of the Tehran Eye Study. In the present study age groups <10 years were not entered in the study, whereas in the Tehran Eye Study there was no age limitation.
Table 7 Comparison of the results of the present study with the Tehran Eye Study.
| Age groups (years) | Prevalence of visual impairment/(95% CI) (Zahedan Study) | Proportion of visual impairment/(95% CI) (Tehran Eye Study) | |
|---|---|---|---|
| Men | 10–19 | 1.59 (0.81 to 2.37) | 0.26 (0.06 to 1.06)* |
| 20–39 | 2.78 (1.60 to 3.96) | 0.91 (0.13 to 1.70) | |
| 40–59 | 6.84 (4.12 to 9.56) | 0.72 (0.23 to 2.26) | |
| >60 | 48.26 (40.32 to 56.20) | 10.94 (6.86 to 15.01) | |
| Women | 10–19 | 1.45 (0.74 to 2.16) | 0.00 (0.00 to 0.00) |
| 20–39 | 3.03 (1.95 to 4.11) | 0.32 (0.10 to 1.01) | |
| 40–59 | 11.47 (8.77 to 14.17) | 1.69 (0.73 to 2.65) | |
| >60 | 58.00 (49.91 to 66.09) | 14.35 (9.13 to 19.57) | |
| Men and women | 10–19 | 1.51 (0.98 to 2.04) | 0.13 (0.03 to 0.54)* |
| 20–39 | 2.93 (2.19 to 3.67) | 0.56 (0.18 to 0.94) | |
| 40–59 | 9.40 (7.42 to 11.38) | 1.30 (0.64 to 1.96) | |
| >60 | 53.07 (46.90 to 59.24) | 12.70 (9.24 to 16.16) | |
| All ages | Men | 6.69 (5.49 to 7.89) | 1.37 (0.91 to 1.83) |
| Women | 6.90 (5.80 to 8.00) | 1.42 (0.98 to 1.86) | |
| All participants | 6.81 (5.91 to 7.71) | 1.39 (1.07 to 1.71) |
*In the Tehran Eye Study the first age group begins from 0 to 19 years.
Table 8 compares the results of the present study with those of similar population‐based studies in other countries.
Table 8 Comparison of the prevalence of blindness and visual impairment in the present study with those of the other population‐based studies.
| Age range (years) | Prevalence of visual impairment, % (95% CI) | Prevalence of blindness, % (95% CI) | |
|---|---|---|---|
| Present study | ⩾10 | 6.81 (5.91 to 7.71) | 0.79 (1.08 to 0.496) |
| Tehran Eye Study5 | All age groups | 2.52 (2.07 to 2.97) | 0.39 (0.23 to 0.56) |
| Lebanon study10 | ⩾3 | 3.9 | 0.6 |
| Malaysia study11 | All age groups | 2.44 (2.18 to 2.69) | 0.29 (0.19 to 0.39) |
| Oman study12 | All age groups | 1.1 (0.9 to 1.3) | |
| Present study | ⩾40 | 23.94 (20.94 to 26.94) | 3.36 (2.00 to 4.71) |
| Present study | ⩾60 | 53.07 (46.89 to 59.25) | 9.20 (5.40 to 13.00) |
| Bangladesh13 | ⩾30 | 1.08 (0.86 to 1.29) | |
| Ethiopia14 | ⩾40 | 12.1% (10.9 to 13.3) | 7.9 (6.9 to 8.9) |
| Hong Cong15 | ⩾60 | 34.5 (32.6 to 36.5) | 0.93 (0.52 to 1.33) |
| Barbados Eye Study16 | ⩾40 | 5.7 (5.1 to 6.5) | 1.7 (1.3 to 2.1) |
| Nigeria17 | ⩾60 | 45.4 | 5.6 |
In the multivariate analysis (logistic regression), there was no age adjusted difference in rates of blindness between men and women; however, as table 2 shows, >40 years rates of blindness (especially bilateral blindness) were higher for women than for men in each age group. The higher rate of blindness in women is supported by the findings of the Tirunelveli (India) Study,18 Medical Research Council Trial,19 the Rotterdam Study20 and the Melbourne Visual Impairment Project.21 However, other population‐based studies such as the Barbados Eye Study16 and the Blindness Study of Gurage Zone (Ethiopia)14 indicate a lower rate of blindness in women. Gender differences in rates of blindness and visual impairment, when noted, can be accounted by female longevity (women live longer), intrinsic factors (higher rates of some diseases with ophthalmological complications in women), inequality in access to healthcare for women in some societies, and behavioural and environmental factors.22
The three leading causes of visual impairment identified in our study were cataract, corneal opacity and amblyopia (tables 5 and 6). Below the age of 40 years, amblyopia is a leading cause of blindness versus cataract for subjects aged >40 years. Both cataract and corneal opacity increase with age, especially for subjects aged >40 years. Increasing prevalence of cataract with age was expected, and similar results are reported in almost all other population‐based studies.5,14,16,18,19,20,21,22 However an explanation for corneal opacity, which in this region is mostly a consequence of trachoma, could be that trachoma‐related corneal scar and vision loss is on the increase and we observed different effects of trachoma on different age cohorts.
Of 248 subjects who had ophthalmological examinations, 98 (39.5%) were considered as curable and 27 (10.9%) of these curable cases were blind in at least one eye. To ameliorate the present situation across Sistan‐va‐Baluchestan, specific measures need to be implemented. Such an action is principally oriented towards increasing the currently inadequate cataract surgical coverage. Included among these measures is the appointment of surgically trained ophthalmologists to each district hospital, as by the year 2006 some districts may not have a practising ophthalmologist and cataract surgery may not be performed there.
Another measure that needs to be implemented is the purchase and provision of essential surgical equipment to the district hospitals in order to provide fundamental logistical support to the district ophthalmologist. The development and integration of primary eye‐care services in the already well‐organised primary healthcare structure in the Province is another intervention that would facilitate community‐based eye health promotion and the referral of cases for treatment.
Finally, the ocular status of the sample in this part of Iran was worse than expected, and further investigations of the pattern of vision loss especially in women and children is warranted. This study strengthens the rationale of developing sight‐saving plans in the study area, and also provides a means to evaluate the effectiveness of such interventions.
Acknowledgements
We thank the following people: Dr Akbar Fotouhi (MD, PhD of epidemiology, Tehran University of Medical Sciences) for his valuable help with statistical analysis, Ms Monir Sargazi (optometrist), Mr Amin Sarabandi (optometrist), Ms Safieh Mohana (optometrist) and Mr Edris Pad (optometrist) for help with the implementation of the study in the Sistan‐va‐Baluchestan Province, Dr Mohammad‐Naeem Amini‐Fard (ophthalmologist), Dr Seyed‐Hashem Mousavi (ophthalmologist), Dr Khodadad Asadi (ophthalmologist) and Dr Zahra Khadem (ophthalmologist) for completion of the clinical examinations, and Dr Zahra Rezaee, Ms Fatemeh Sargazi and Dr Khodadad Sheikhzadeh (health officers) for administrative assistance.
Abbreviations
VA - visual acuity
Footnotes
Funding: Al‐Zahra Eye Centre and Zahedan University of Medical Sciences have funded the Zahedan Eye Study.
Competing interests: None.
References
- 1.World Health Organization Prevention of avoidable blindness and visual impairment. In: Fifty‐ninth World Health Assembly. Geneva: WHO; 2006, A59/12 p. 1–3. http://www.who.int/gb/e/e_wha59.html (accessed 20 Feb 2007)
- 2.Brundtland G H.World Blindness Day 2002. Geneva, Switzerland, 2002. http://www.who.int/dg/speeches/2002/geneva/en/ (accessed 20 Feb 2007)
- 3.World Health Organization WHO launches project to prevent blindness in children. Press release. Geneva: WHO, 2002, Report Number: WHO/48. http://www.who.int/mediacentre/news/releases/release48/en/print.html (accessed 20 Feb 2007)
- 4.Gilbert C, Foster A. Childhood blindness in the context of vision 2020: the right to sight. Bull World Health Organ 200179227–232. [PMC free article] [PubMed] [Google Scholar]
- 5.Fotouhi A, Hashemi H, Mohammad K.et al The prevalence and causes of visual impairment in Tehran: the Tehran Eye Study. Br J Ophthalmol 200488740–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mirdehghan S A, Dehghan M H, Mohammadpour M.et al Causes of severe visual impairment and blindness in schools for visually handicapped children in Iran. Br J Ophthalmol 200489612–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iranian Statistics Centre The report of the 1996 population census, Sistan‐va‐Baluchestan Province (in Persian). Tehran: Iranian Statistics Centre, 1998
- 8.World Health Organization International statistical classification of diseases and related health problems, 10th revised edn Geneva: WHO 1992
- 9.Bennett S, Woods T, Liyanage W M.et al A simplified general method for cluster‐sample surveys of health in developing countries. World Health Stat Q 19914498–106. [PubMed] [Google Scholar]
- 10.Mansour A M, Kassak K, Chaya M.et al National survey of blindness and low vision in Lebanon. Br J Ophthalmol 199781905–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zainal M, Ismail S M, Ropilah A R.et al Prevalence of blindness and low vision in Malaysian population: results from the National Eye Survey 1996. Br J Ophthalmol 200286951–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khandekar R, Mohammed A J, Negrel A D.et al The prevalence and causes of blindness in the Sultanate of Oman: the Oman Eye Study (OES). Br J Ophthalmol 200286957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dineen B P, Bourne R R A, Ali S M.et al Prevalence and causes of blindness and visual impairment in Bangladeshi adults: results of the National Blindness and Low Vision Survey of Bangladesh. Br J Ophthalmol 200387820–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melese M, Alemayehu W, Bayu S.et al Low vision and blindness in adults in Gurage Zone, central Ethiopia. Br J Ophthalmol 200387677–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michon J J, Lau J, Chan W S.et al Prevalence of visual impairment, blindness and cataract surgery in the Hong Kong elderly. Br J Ophthalmol 200286133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyman L, Wu S Y, Connell A M S.et al Prevalence and causes of visual impairment in the Barbados Eye Study. Ophthalmology 20011081751–1756. [DOI] [PubMed] [Google Scholar]
- 17.Adegbehingbe B O, Fajemilehin B R, Ojofeitimi E E.et al Blindness and visual impairment among the elderly in Ife‐Ijesha zone of Osun State, Nigeria. Indian J Ophthalmol 20065459–62. [DOI] [PubMed] [Google Scholar]
- 18.Nirmalan P K, Thulasiraj R D, Maneksha V.et al A population bases eye survey of older adults in Tirunelveli district of south India: blindness, cataract surgery, and visual outcomes. Br J Ophthalmol 200286505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans J R, Fletcher A E, Wormald R PL.et al Prevalence of visual impairment in people age 75 years and older in Britain: results from MRC trial of assessment and management of older in the community. Br J Ophthalmol 200286795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klaver C C, Wolfs R C, Vingerling J R.et al Age‐specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol 1998116653–658. [DOI] [PubMed] [Google Scholar]
- 21.Taylor H R, Livingston P M, Stanislavsky Y L.et al Visual impairment in Australia: distance visual acuity, near vision, and field findings of the Melbourne Visual Impairment Project. Am J Ophthalmol 1997123328–337. [DOI] [PubMed] [Google Scholar]
- 22.Gipson I K, Turner V M. Are women more likely to be blind or visually impaired than men? Arch Soc Esp Oftalmol 200580323–326. [PubMed] [Google Scholar]