Abstract
Objective
To evaluate the changes in correlations of higher order aberrations of the first corneal surface with halo phenomena, a form of image degradation, under night vision conditions measured objectively after successful LASIK (laser in situ keratomileusis) surgery.
Methods
A prospective, observational, analytical study of 110 eyes that had undergone successful LASIK surgery for myopia and astigmatism. Preoperative sphere was (mean (SD)) −3.48 (1.70) D (0 to −8.00 D) and preoperative cylinder was −0.86 (0.87) D (0 to −4.00 D). Visual disturbance caused by halo phenomena was measured with the Starlights v1.0, and pupil size was measured with Colvard pupilometry after adaptation to a dark environment (0.17 lux). Corneal aberrations were computed for a corneal diameter representative of the eye's entrance pupil under night vision conditions.
Results
The halo disturbance index increased in this study by a factor of 2.15 after successful LASIK surgery. Total root mean square for monochromatic higher order aberration displayed a significant correlation with halo disturbance index (r = 0.42; p<0.01). However, only secondary astigmatism (r = 0.36; p<0.01), coma (r = 0.25; p = 0.02) and spherical aberration (r = 0.40; p<0.01) were responsible for such behaviour, with the remaining corneal aberrations up to the sixth order not displaying any significant correlation when considered individually.
Conclusion
Patients undergoing LASIK procedures display an increase of halo phenomena around lights in night vision conditions, even when the results of the surgery are considered entirely satisfactory according to current international standards of predictability, efficacy and safety. Secondary astigmatism, coma and spherical aberration are the higher order aberrations up to the sixth order that significantly correlated with halo disturbance index.
Different forms of night vision disturbance (NVD) have been described among patients who had undergone refractive surgery procedures.1 Early reports attributed starburst to a typically transient loss of transparency in the postoperative period (haze), while halo phenomena will be caused by the margin of corneal ablation within the pupillary area.2,3
The difficulty in distinguishing different forms of NVD by patients and practitioners has been highlighted by Fan‐Paul et al4 According to their description, NVDs include glare disability, decrease in visual contrast sensibility, and image degradation. In a retrospective study, Jabbur et al5 documented NVD as a leading cause of complaint for patients undergoing different refractive surgical procedures, with 43.5% of patients having such difficulties.
Different approaches have been proposed to minimise NVD after refractive surgery, including creation of artificial pupils with contact lenses, surgical re‐treatments to enlarge the optical zone,6 overminussing of the optical prescription and miotic drugs.2 Furthermore, our clinical experience told us that rigid gas‐permeable (RGP) contact lenses are also effective in reducing symptoms in patients with NVD. This empirical finding, along with the fact that LASIK (laser in situ keratomileusis) surgery affects primarily the anterior corneal surface, supports the rationale that the first corneal surface must be the primary factor behind NVDs as halo phenomena after LASIK surgery.
The aim of the present study was to quantify the halo phenomena objectively by measuring the distortion in size and shape of a light source reported by a population of myopic eyes that had undergone successful LASIK refractive surgery, and to find which aberrations are more directly implicated in halo phenomena under night vision conditions.
Materials and methods
Patients and laser procedures
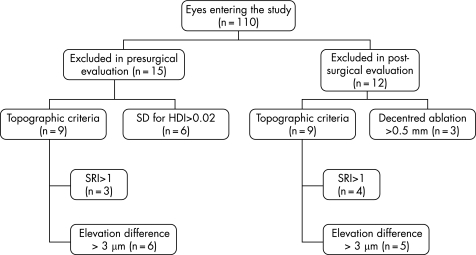
One hundred and ten eyes from 55 patients underwent LASIK surgery. Surgical routine for LASIK surgery was according to international standards, and the commonly accepted criteria for refractive surgery procedures were followed. Of the 110 initially entering the study, 83 remained for inclusion in the subsequent statistical analysis to evaluate correlations between the halo disturbance index (HDI) and monochromatic aberrations (60% males, 40% females). Fifteen eyes were excluded in the presurgical examination and 12 were excluded in the postsurgical examination. Figure 1 shows patients excluded from the study according to exclusion criteria.
Figure 1 Flow‐chart indicating the number of eyes excluded at different stages of the study and the reasons.
After a 160 μm, 9.0 mm diameter flap creation with a Hansatome (Chiron Vision, model 2765; Bausch & Lomb, Claremont, California, USA) microkeratome, spherical (n = 16 eyes), central elliptical (n = 50 eyes) and mixed bitoric (n = 17 eyes) ablations were produced according to Munnerlyn's algorithm (not customised ablations) using a VisX Star S2 Smoothscan modified wide angle excimer laser (Santa Clara, California, USA) centred with the centre of the pupil.
The study followed the tenets of the Declaration of Helsinki, and informed consent was obtained from all patients after the nature of the study had been explained to them.
Topographic evaluation
Three sets of topographic data were obtained with Orbscan II (v3.12; Bausch & Lomb, Rochester, New York, USA) before and after surgery and then compared in pairs. By pair comparison, the two maps with differences in elevation topography no higher than 3 μm across the 5 mm central map area were selected and that with the closer and most centred localisation of the pupillary centre and ablation centre was used for subsequent calculations. This criterion agrees with the procedures recommended by the manufacturer to choose presurgical corneal topography for topography‐guided ablations. Additionally, the surface regularity index (SRI) was measured with a Placido disk videokeratoscope (TMS‐2; Tomey, Egen, Germany). Procedures were repeated after surgery.
Exclusion criteria and follow‐up
According to the study's follow‐up protocol, patients were examined once postoperatively. This examination was carried out within the period of 3–6 months after surgery was performed (mean (SD), 127.1 (34.1) days). Exclusion criteria included a significant degree of variability on HDI, significant surface irregularity or decentred ablation. Patients displaying an SD>0.02% preoperatively from three consecutive measurements of HDI were excluded from the study. This value was established as a threshold because it was the maximum variability from three repeated measurements in a group of 20 emmetropic control patients. However, postoperatively, this value is expected to increase to 0.03%. A significant degree of surface irregularity (SRI>1); more than 0.5 mm decentred ablation (distance from pupil centre to ablation geometric centre) and inconsistent repeatability of elevation maps from Orbscan II were also considered as causes of exclusion from the study. Biomicroscopic findings were also investigated in order to exclude cases of haze, striae, flap wrinkling or epithelial defects.
Measurement of visual HDI and pupil size
The Starlights system (Novosalud, Valencia, Spain) consists of a black screen with a central light which acts as a fixation stimulus and source of light. This stimulus subtends an angle of 0.34° (1.2 cm) and is surrounded by white light‐emitting diodes (LEDs) distributed radially along 12 semimeridians with maximum amplitude of 30°; each one of them subtends an angle of 0.06° at a distance of 2.5 m between observer and screen. At this distance, with the room in total darkness, the luminance is about 0.17 lux or 0.054 cd m–2, which is slightly above the scotopic level of luminance (10−6–10−3 cd m–2) but is still in the range of what could be considered night vision (10−4–10−1 cd m–2). Exposure time (ON period) was 0.25 s. Time between stimuli (OFF period) was 1 s. This instrument set‐up allows us to shorten the examination time compared with definitions used in previous studies,7 and it is not expected to affect the reliability of the examination.
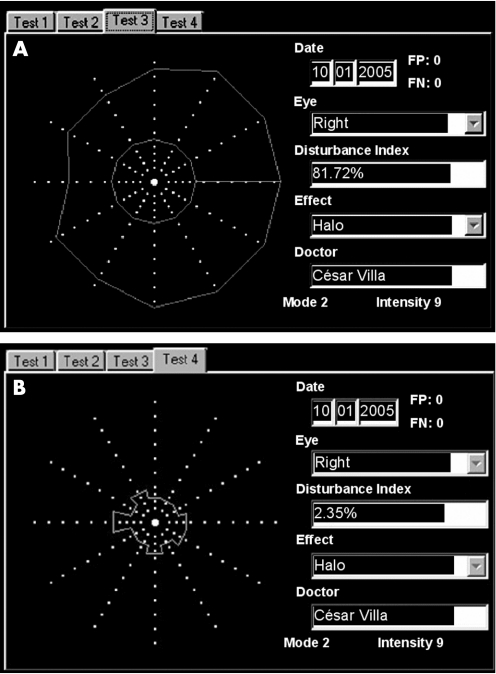
The device provides an index of light disturbance called the “disturbance index” (in this study, called the HDI) which represents the percentage of the total area explored where the peripheral stimuli are not seen due to the light distortion induced by the central source on the patient's retina under scotopic conditions. This instrument has proven to be sensitive enough to quantify halo phenomena in patients who had undergone LASIK in a recent study.7 An example of Starlights exam is shown in fig 2. In the present study, the procedure was repeated three times for each eye, and the values obtained were averaged to obtain a unique measure of the HDI.
Figure 2 Pair of examinations simulating the HDI before (A) and after (B) rigid gas‐permeable contact lens fitted for postsurgical irregular astigmatism, showing a reduction in HDI from 81.72% without the lens to 2.35% with the contact lens in place. FP, false positive; FN, false negative.
After completion of the measurement of HDI, while the patient remained under the same night vision conditions, pupil diameter was measured using a Colvard pupillometer (Oasis Medical, Glendora, California, USA).
Computing corneal monochromatic aberrations
Topographic data from Orbscan II were downloaded onto floppy disks in ASCII files, which contained information about corneal elevation, curvature, power and position of the pupil. Higher order aberrations were expressed as Zernike polynomials z6 to z21 which comprise corneal aberrations up to the sixth order using the Calculations facility of Vol‐CT 6.20 software (Sarver & Associates, Inc., Carbondale, Illinois, USA) with reference for centration at the centre of the pupil. A wavelength of 505 nm was used as this is the peak sensibility of the human eye under night vision conditions.
The corneal diameter at which corneal aberrations were obtained was different for each individual. This diameter was chosen considering his/her pupil diameter as measured with Colvard pupillometer compensated for the effect of magnification according to Alexandridis and Bauman.8
Statistical analysis
Data were analysed using the statistical package SPSS version 12.0. Bi‐variate correlation analysis was used to evaluate correlations of HDI with pupil size and higher order aberrations (total and partial root mean square (Rms) values). The level of significance was established at α = 0.05. Normal distribution of variables was assessed by the Kolmogorov–Smirnov normality test.
Results
Surgical parameters and outcomes
Patient age ranged from 20 to 54 years (32.81 (7.13)). Preoperative sphere was −3.48 (1.70) D (0 to −8 D) and pre‐operative cylinder was −0.86 (0.87) D (0 to −4 D). Mean preoperative flat keratometry was 43.12 (1.4) D (range 39.7 to 45.6 D) and mean central corneal thickness (CCT) was on average 546.8 (30.6) μm (range 498–631 μm). Ablation depth was on average 51.4 (19.1) μm (range 13–91 μm). On average, the programmed optical zone diameter was 6.2 (0.6) mm in the horizontal direction and 5.6 (0.9) mm in the vertical direction, with the transition zone at 8 mm.
Refractive and visual outcomes in terms of predictability were satisfactory, with 98.79% of patients within a ±1.0 D sphere, and 93.97% within a ±0.5 D sphere. Indices of efficacy and safety were 0.95 and 0.99, respectively.
HDI, pupil size and high order aberrations
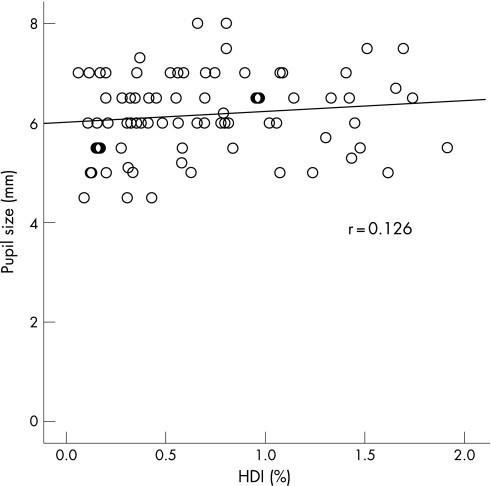
Presurgical HDI was 0.32 (0.23) for a pupil size of 6.27 (0.84) as measured with the Colvard pupillometer, which corresponds to an entrance pupil of 7.05 (0.97) mm. At postsurgical consultation, HDI increased to 0.69 (0.47) for an average pupil size of 6.16 (0.81) mm, which corresponds to an entrance pupil of 6.99 (0.91) mm. Differences in pupil size do not justify changes in HDI, as shown in fig 3.
Figure 3 Linear regression postsurgery between pupil size and halo disturbance index (HDI).
Table 1 presents the descriptive statistics of the presurgical and postsurgical HDI, pupil size and average changes in the monochromatic high order aberrations of the cornea. The main result is the increase in the HDI by a factor of 2.15 despite the success of the LASIK procedures as demonstrated by the current standards of predictability, efficacy and safety. All aberrations change after LASIK surgery in this population; however, only spherical aberration and secondary astigmatism displayed statistically significant changes.
Table 1 Descriptive statistics and statistical comparison of the halo disturbance index, pupil size and higher order aberrations for the clinical population (n = 83 eyes) before and after surgery.
| Preoperative mean (SD) | Postoperative mean (SD) | p Value | |
|---|---|---|---|
| Pupil size (mm) | 6.27 (0.84) | 6.16 (0.81) | NS |
| HDI (%) | 0.32 (0.23) | 0.69 (0.47) | <0.001** |
| Total Rms (μm) | 0.78 (0.36) | 1.36 (0.61) | <0.001** |
| Trefoil (μm) | 0.34 (0.29 | 0.34 (0.21) | NS |
| Coma (μm) | 0.44 (0.25) | 0.65 (0.39) | <0.001** |
| Tetrafoil (μm) | 0.15 (0.15) | 0.14 (0.09) | NS |
| Secondary astigmatism (μm) | 0.17 (0.14) | 0.24 (0.18) | 0.004** |
| Spherical (μm) | 0.36 (0.17) | 0.99 (0.58) | <0.001** |
| Pentafoil (μm) | 0.10 (0.11) | 0.10 (0.06) | NS |
HDI, halo disturbance index; NS, non significant; Rms, root mean square.
**Statistically significant at α = 0.01.
Table 2 displays the correlations of presurgical and postsurgical HDI with presurgical and postsurgical pupil size and higher order aberrations. Total Rms was significantly correlated with HDI (Pearson correlation, r = 0.426; p<0.01) and pupil size (r = 0.397; p<0.01). Partial Rms after surgery was significantly correlated with HDI for spherical aberration ‐z12, z24‐ (r = 0.41; p<0.001); coma‐like ‐z7, z8, z17, z18‐ (r = 0.25; p = 0.02) and secondary astigmatism ‐z11, z13, z23, z25‐ (r = 0.37; p<0.001). Conversely, trefoil ‐z6, z9, z16, z19‐ and pentafoil ‐z15, z20‐ had no significant correlation with HDI (p>0.05). Figure 4 presents the correlations of partial Rms with HDI separately.
Table 2 Preoperative and postoperative correlations of halo disturbance index (%) with pupil size (mm) and high order aberration (μm) of the front corneal surface (n = 83 eyes).
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| Pearson correlation | p Value | Pearson correlation | p Value | |
| HDI vs pupil size | 0.098 | 0.381 | 0.126 | 0.258 |
| HDI vs total Rms | 0.299 | 0.006** | 0.426 | <0.001** |
| HDI vs trefoil | 0.128 | 0.248 | 0.142 | 0.200 |
| HDI vs coma | 0.180 | 0.104 | 0.250 | 0.023* |
| HDI vs tetrafoil | 0.218 | 0.048* | 0.129 | 0.245 |
| HDI vs secondary astigmatism | 0.101 | 0.366 | 0.368 | 0.001** |
| HDI vs spherical aberration | 0.397 | <0.001 | 0.408 | <0.001** |
| HDI vs pentafoil | 0.195 | 0.077 | 0.134 | 0.228 |
*Statistically significant at α = 0.05; **statistically significant at α = 0.01.
HDI, halo disturbance index; Rms, root mean square.
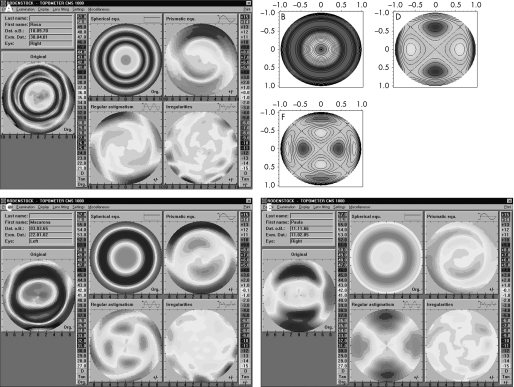
Figure 4 Linear regression of halo disturbance index (HDI) with postsurgical root means square (Rms) for different aberrations of the front corneal surface including trefoil (A), coma (B), tetrafoil (C), secondary astigmatism (D), spherical aberration (E) and pentafoil (F).
Attempted correction, ablation type and its impact on postsurgical spherical aberration and secondary astigmatism
A positive correlation was found between spherical aberration and degree of attempted spherical refraction for myopia corrections above −3.5 D (n = 35; r = 0.49; p<0.01), being slightly weaker for myopic corrections below −3.5 D (n = 48; r = 0.32; p<0.05). Conversely, the lower the astigmatic attempted correction, the higher the weight of the spherical aberration. This was true for eyes with attempted cylindrical corrections lower than −0.75 D (n = 28; r = 0.63; p<0.01) and attempted cylindrical corrections higher than −0.75 D (n = 55; r = 0.30; p<0.05).
The same analysis applied to the secondary astigmatism revealed that the change in this aberration showed a greater increase for higher degrees of attempted astigmatic correction and at a lower amount as the spherical component becomes more important compared with the cylindrical component. In fact, higher indices of secondary astigmatism were found in elliptical and mixed ablations (n = 50; r = 0.31; p<0.05 and n = 17; r = 0.52; p<0.05, respectively), than in spherical ablations (n = 16; r = 0.18; p>0.05).
Discussion
Relationships between surgically induced aberrations and halo phenomena have been established previously.9 However, such disturbances have been attributed to small treatment zones and postsurgical irregular astigmatism.10,11,12 Nowadays, with more precise objective methods to measure quality of vision, it is possible to find correlations among those variables with a scientific basis, in order to develop effective methods to limit their impact on a patient's quality of life.
To investigate the amount of aberrations induced after refractive surgery and the related degree of NVD experienced by the patient is of major interest in order to develop strategies to minimise patient complaints.13 However, to date, no studies have addressed this question. In this study, we have provided evidence that the first surface corneal aberration after LASIK is responsible for the halo phenomenon that causes night vision distortions even when procedures can be considered fully successful. The rationale of analysing solely the first surface corneal aberrations instead of total aberrations of the eye is based on the clinical findings that suggest that the cornea must be primarily responsible for NVD, including halo phenomena. For this reason, to consider total aberrometry would include other changes in the inner aberration structure of the eye that could confound the actual weight of the effect of corneal aberrations on halo phenomena after LASIK.
The impact of halo phenomena on the visual system has been evaluated objectively, and subjective perception of these symptoms is associated with an abnormal hyperactivity of the visual cortex under monocular stimulation of the eye affected.14
Despite association between pupil size and ocular aberrations, which is in agreement with the findings of previous studies,15,16,17 pupil size, when considered alone, was not a significant contributor to HDI in the present study. Moreover, looking at average values of pupil size presurgery and postsurgery, there was a slight decrease from 6.27 to 6.16 mm. Ignoring diffractive effects that would not be relevant for this diameter, any change in ocular aberrations or halo phenomena would be towards a decrease in both factors. Indirectly, this reinforces the fact that the increase in halo phenomena after surgery is not dependent on pupil size. Although pupil size by itself does not account for larger indices of halo phenomena in our sample, pupil size programmed for LASIK ablation should be kept greater than the Colvard pupil size compensated for according to Alexandridis and Baumnan.8 Keeping this in mind and if the treatment zone is well centred, pupil size would not be a significant source of HDI, as our results suggest.
Conversely, our findings suggest that there is a significant correlation between the measured HDI and the amount of attempted correction. Both facts agree with other studies investigating different forms of night vision distortion.18,19 This was expected, as Lee et al19 suggested that with uniform corneal topography and pupil diameter <7 mm, pupil size does not play a significant role in visual function.19
Comparing present values of HDI with those found in previous works published by the authors,7,20 there are marked differences in average values and SD, and this warrants discussion.
First, the fact that the order of magnitude is different in the present study has to do with the reference area. The instrument has two options for the area of inspection (circle 1 and circle 2). As postsurgically, many patients experience halos that exceed the area of circle 1, in the present study the area shaded by the halo is referred to circle 2 (a larger circle for the same area shaded by the halo gives lower HDI values, even when the halo size is of the same order of magnitude as those quoted in previous publications, which would be expected as surgical procedures and refractive correction were similar).
Secondly, the higher SD could be explained by the different experimental conditions: differences in time of exposure (ON period), latency between stimuli (OFF period) and working distance. In previous works, a shorter distance (2 m) was used, compared with the 2.5 m used in the present study. Also, the ON period was 1.25 s, instead of the 0.25 s used here. Finally, the OFF period was 2 s in previous works and only 1 s in the present study. As quoted in the work where the instrument was calibrated, these changes should not have a negative impact on the reliability of the instrument.7 The larger sample and the greater heterogeneity of the group in terms of refractive correction or types of ablation could explain the higher SD compared with previous works. The experimental conditions used in this work were maintained presurgery and postsurgery. Lack of reliability was avoided by ensuring that each patient did not display an SD higher than 0.02% preoperatively from three consecutive HDI readings.
The results of this study support the assumption that different components of monochromatic corneal front surface aberrations play a different role in retinal image quality.21 Considering the results of the present study, greater attention should be paid to vision distortion under night vision conditions (ie, driving at night) even in patients with a history of successful LASIK surgery. Furthermore, new algorithms for laser ablation should be designed not only to maintain an aspheric corneal shape after surgery in order to limit spherical aberration,22,23,24,25 but also to limit the amount of secondary astigmatism that arises as a consequence of elliptical and bitoric ablations for astigmatic compensation. Bitoric ablations are performed with the aim of preserving a higher degree of prolateness in the postsurgical cornea and reducing spherical aberration, which in fact seems to be true in this study (a lower correlation between spherical aberration and HDI for higher degrees of attempted astigmatic correction). However, higher correlations between HDI and secondary astigmatism were found in this study among subjects who had undergone mixed and bitoric ablations for astigmatism. This is evident in fig 5 which shows three examples of decomposition of postsurgical corneal topography into the main aberration components (spherical‐like, coma‐like, secondary astigmatism and irregular astigmatism) for the three types of corneal ablations performed in this sample. While fourth and sixth order secondary astigmatic components are not evident for spherical ablation, these patterns are present with elliptical and bitoric ablations, respectively.
Figure 5 Decomposition of corneal topography (by Fourier analysis) into the four main aberration components (spherical‐like, coma‐like, regular astigmatism and irregular astigmatism) for a spherical (A), an elliptical (B) and a mixed ablation (C). Note the similarity between the regular astigmatic component and the pure secondary regular astigmatism (horizontal) representations in the Zernike pyramid on the right side for the elliptical ablation (sixth order horizontal astigmatism, B) and mixed ablation (fourth order horizontal astigmatism, C).
In summary, the present study has demonstrated that halo phenomena that interfere with night vision occur even after successful LASIK procedures, and pupil size seems not to be important for the subjectively perceived night vision distortion, with spherical‐like, coma and secondary astigmatic higher order aberrations being the most significant predictors of postsurgical halo phenomena under scotopic conditions even when LASIK procedures are considered successful. In a similar way as happens with spherical aberration that increases as the spherical attempted correction increases according to Munnerlyn's algorithm, secondary astigmatism increases as the astigmatic attempted correction increases. Further studies will be important in reaching a compromise between limitations in an increase in spherical aberration with toric ablations and the degree of secondary astigmatism induced by such procedures. Measurement of visual disturbance caused by halo phenomena with Startlights under night vision conditions is proposed as a control factor to guide investigators and surgeons towards optimisation of visual outcomes after refractive surgery.
Abbreviations
HDI - halo disturbance index
LASIK - laser in situ keratomileusis
NVD - night vision disturbance
Rms - root mean square
SRI - surface regularity index
Footnotes
Competing interests: None.
References
- 1.Brunette I, Gresset J, Boivin J F.et al Functional outcome and satisfaction after photorefractive keratectomy. Part 2: survey of 690 patients. Ophthalmology 20001071790–1796. [DOI] [PubMed] [Google Scholar]
- 2.O'Brart D P, Lohmann C P, Fitzke F W.et al Night vision after excimer laser photorefractive keratectomy: haze and halos. Eur J Ophthalmol 1994443–51. [DOI] [PubMed] [Google Scholar]
- 3.O'Brart D P, Lohmann C P, Fitzke F W.et al Disturbances in night vision after excimer laser photorefractive keratectomy. Eye 19948(Pt 1)46–51. [DOI] [PubMed] [Google Scholar]
- 4.Fan‐Paul N I, Li J, Miller J S.et al Night vision disturbances after corneal refractive surgery. Surv Ophthalmol 200247533–546. [DOI] [PubMed] [Google Scholar]
- 5.Jabbur N S, Sakatani K, O'Brien T P. Survey of complications and recommendations for management in dissatisfied patients seeking a consultation after refractive surgery. J Cataract Refract Surg 2004301867–1874. [DOI] [PubMed] [Google Scholar]
- 6.Lafond G. Treatment of halos after photorefractive keratectomy. J Refract Surg 19971383–88. [DOI] [PubMed] [Google Scholar]
- 7.Gutierrez R, Jimenez J R, Villa C.et al Simple device for quantifying the influence of halos after lasik surgery. J Biomed Opt 20038663–667. [DOI] [PubMed] [Google Scholar]
- 8.Alexandridis E, Baumann C H. Und scheinbare pupillenweiten des menschlichen auges. Optica Acta 196714311–316. [DOI] [PubMed] [Google Scholar]
- 9.Holladay J T, Dudeja D R, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg 199925663–669. [DOI] [PubMed] [Google Scholar]
- 10.Seo K Y, Lee J B, Kang J J.et al Comparison of higher‐order aberrations after LASEK with a 6.0 mm ablation zone and a 6.5 mm ablation zone with blend zone. J Cataract Refract Surg 200430653–657. [DOI] [PubMed] [Google Scholar]
- 11.Mok K H, Lee V W. Effect of optical zone ablation diameter on LASIK‐induced higher order optical aberrations. J Refract Surg 200521141–143. [DOI] [PubMed] [Google Scholar]
- 12.Nepomuceno R L, Boxer Wachler B S, Scruggs R. Functional optical zone after myopic LASIK as a function of ablation diameter. J Cataract Refract Surg 200531379–384. [DOI] [PubMed] [Google Scholar]
- 13.Pop M, Payette Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 20041113–10. [DOI] [PubMed] [Google Scholar]
- 14.Malecaze F J, Boulanouar K A, Demonet J F.et al Abnormal activation in the visual cortex after corneal refractive surgery for myopia: demonstration by functional magnetic resonance imaging. Ophthalmology 20011082213–2218. [DOI] [PubMed] [Google Scholar]
- 15.Martinez C E, Applegate R A, Klyce S D.et al Effect of pupillary dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol 19981161053–1062. [DOI] [PubMed] [Google Scholar]
- 16.Endl M J, Martinez C E, Klyce S D.et al Effect of larger ablation zone and transition zone on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol 20011191159–1164. [DOI] [PubMed] [Google Scholar]
- 17.Oshika T, Klyce S D, Applegate R A.et al Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol 19991271–7. [DOI] [PubMed] [Google Scholar]
- 18.Haw W W, Manche E E. Effect of preoperative pupil measurements on glare, halos, and visual function after photoastigmatic refractive keratectomy. J Cataract Refract Surg 200127907–916. [DOI] [PubMed] [Google Scholar]
- 19.Lee Y C, Hu F R, Wang I J. Quality of vision after laser in situ keratomileusis: influence of dioptric correction and pupil size on visual function. J Cataract Refract Surg 200329769–777. [DOI] [PubMed] [Google Scholar]
- 20.Jimenez J R, Villa C, Anera R G.et al Binocular visual performance after LASIK. J Refract Surg 200622679–688. [DOI] [PubMed] [Google Scholar]
- 21.Applegate R A. Glenn Fry award lecture 2002: wavefront sensing, ideal corrections, and visual performance. Optom Vis Sci 200481167–177. [DOI] [PubMed] [Google Scholar]
- 22.Anera R G, Jimenez J R, Jimenez d B.et al Changes in corneal asphericity after laser in situ keratomileusis. J Cataract Refract Surg 200329762–768. [DOI] [PubMed] [Google Scholar]
- 23.Jimenez J R, Anera R G, Jimenez d B. Equation for corneal asphericity after corneal refractive surgery. J Refract Surg 20031965–69. [DOI] [PubMed] [Google Scholar]
- 24.Jimenez J R, Anera R G, Diaz J A.et al Corneal asphericity after refractive surgery when the Munnerlyn formula is applied. J Opt Soc Am A Opt Image Sci Vis 20042198–103. [DOI] [PubMed] [Google Scholar]
- 25.Gatinel D, Malet J, Hoang‐Xuan T.et al Analysis of customized corneal ablations: theoretical limitations of increasing negative asphericity. Invest Ophthalmol Vis Sci 200243941–948. [PubMed] [Google Scholar]