Abstract
Background
Transjugular intrahepatic portosystemic shunt (TIPS) is a treatment for portal hypertension‐related complications. Accurate prediction of the outcome of patients treated with TIPS is important, because some patients have very short survival. Diastolic dysfunction is frequently observed in patients with cirrhosis.
Aim
To investigate whether or not diastolic dysfunction can predict the outcome after TIPS.
Methods
Echocardiography with Doppler exploration was performed before and 28 days after TIPS insertion in 32 patients with cirrhosis. Several echocardiographic measures, including the early maximal ventricular filling velocity/late filling velocity (E/A) ratio as indicative of diastolic function, as well as laboratory, clinical and demographic variables were evaluated as predictors of survival.
Results
Univariate analysis revealed that the presence of diastolic dysfunction observed 28 days after TIPS (E/A ratio ⩽1) and baseline model of end‐stage liver disease score were related to survival. Multivariate analysis identified diastolic dysfunction as an independent predictor of death (RR 8.9, 95% CI 1.9 to 41.5, p = 0.005). During the first year of follow–up, six out of 10 patients with an E/A ratio ⩽1 died, whereas all 22 patients with E/A ratio >1 survived.
Conclusions
Diastolic dysfunction estimated using E/A ratio is a promising predictor of death in patients with cirrhosis who are treated with TIPS.
Diastolic dysfunction is often found in cirrhotic cardiomyopathy.1,2,3,4 It is caused by stiffness in the ventricle, and might impair the cardiac ability to handle an increased preload.5 However, knowledge about the clinical relevance of this alteration is still incomplete, and until now the usefulness of investigating diastolic dysfunction in the management of patients with cirrhosis had not been defined.
The transjugular intrahepatic portosystemic shunt (TIPS) is widely used to treat portal hypertension‐related complications, such as refractory variceal bleeding and refractory ascites.6 TIPS has also been successfully used in some rare and severe conditions such as Budd–Chiari syndrome and cirrhotic hydrothorax.6 TIPS has a marked effect on systemic haemodynamics. In particular, it rapidly shifts a large volume of blood from the splanchnic area to the heart, thus increasing the cardiac preload. This can pose a challenge to the cirrhotic heart, the consequences of which have been sparsely investigated.7
We previously demonstrated that the ratio between the early maximal ventricular filling velocity and the late filling velocity (E/A), a marker of diastolic function, was found to improve in many, but not all, patients with cirrhosis treated with TIPS.8 In a setting of increased venous return to the heart, the persistence of diastolic dysfunction after TIPS could affect the global cardiac performance and so the patient outcome. Therefore, we investigated whether or not there is any relationship between diastolic dysfunction after TIPS and the clinical outcome of patients with cirrhosis treated with TIPS.
Materials and methods
Patients
Forty‐four consecutive patients with cirrhosis admitted to the Department of Internal Medicine (IRCCS Policlinico San Donato, Università degli Studi, San Donato Milanese, Milano, Italy) for treatment with elective TIPS were considered for the present study. Of these, 12 patients were excluded, owing to unsuccessful stent insertion (n = 4), early and irreversible stent occlusion by thrombosis (n = 2), death within the first month (n = 2), liver transplantation within the first month (n = 1) or refusal to participate (n = 3). The remaining 32 patients (21 men and 11 women, mean (SD) age 61 (1.6) years, range 41–76) participated in the study. Twenty‐two of these patients had also participated in our previous investigation.8 The diagnosis of cirrhosis was based on clinical, laboratory and ultrasonographic criteria, and was also confirmed by liver biopsy in 11 cases. The causes of liver disease were hepatitis B or C virus (n = 14), alcohol consumption (n = 11), non‐alcoholic steatohepatitis‐related (n = 2), sclerosing cholangitis (n = 1), α‐1‐antitrypsin deficiency (n = 1) or unknown (n = 3). All patients with alcoholic cirrhosis had been teetotallers for at least 6 months before inclusion. All patients had a chest x ray, electrocardiography, echocardiography and a cardiological check‐up to exclude cardiovascular diseases. Other criteria of exclusion were renal or pulmonary organic diseases, serum bilirubin >102 μmol/l, serum creatinine >265 μmol/l, hepatocellular carcinoma, total portal vein thrombosis, Child–Pugh score >11 and ongoing bacterial infection.
All patients were in a stable condition, with no gastrointestinal bleeding being recorded during the 15 days preceding TIPS insertion. TIPS treatment was performed to treat recurrent variceal bleeding in 10 patients, and for recurrent or refractory ascites in 22 patients, as diagnosed by the International Ascites Club definitions.9 The follow‐up ended 6 months after the last patient was enrolled.
Diuretic drugs were kept constant during the week before TIPS insertion. Drugs affecting haemodynamics, such as β‐blockers and vasodilators, were stopped for at least 10 days before TIPS. Other drugs were omitted only in the morning hours of the days of investigation.
The local ethics committee approved the study, and informed consent was obtained from all participants. The study was conducted according to the guidelines of Good Clinical Practice.
Protocol
At 3 days before and 28 days after TIPS insertion, patients underwent a study that included: (1) measurement of arterial blood pressure and heart rate; (2) transthoracic cardiac echography with colour Doppler; and (3) determination of plasma renin activity (PRA), plasma aldosterone and plasma atrial natriuretic peptide (ANP).
A standard procedure was used for TIPS insertion, which was performed under sedation after administration of remifentanyl (Ultiva® GlaxoSmithKline).1 Uncovered stents (Wallstent, Boston Scientific Corporation, Natick, Massachusetts, USA; or Sinus stent, OptiMed GmbH, Ettlingen, Germany; or Memotherm, Angiomed, Karlsruhe, Germany) were used in the first 22 cases, whereas covered stents (Gore and ass., Bercy Int., Paris, France) were used in the other 10 cases. The final function of the stent was confirmed by portography, and by measuring the portosystemic pressure gradient. When the patency was considered to be insufficient, the stent was dilated and/or a new stent was placed coaxially.
Procedures
Arterial blood pressure was measured three times at intervals of 2 min using a mercury sphygmomanometer, and the three values were then averaged. The mean arterial pressure (MAP) was calculated as diastolic pressure plus one‐third of the pulse pressure. Heart rate was recorded by cardiac auscultation and confirmed by electrocardiography. Then an indwelling catheter was placed in an antecubital vein and kept patent by slow saline infusion. After 2 h of supine rest, blood was collected in ice‐chilled tubes and immediately centrifuged at 4°C. The supernatant was stored at −20°C until assay. PRA, aldosterone and ANP concentrations were measured by radioimmunoassay methods as described previously, using reagents purchased from Biodata (Milan, Italy), Sclavo (Siena, Italy) and Nichols Diagnostic Institute (San Juan Capistrano, California, USA), respectively.1 Normal values (means (SD)) obtained in our laboratory are: 0.33 (0.14) ng/l⋅s for PRA, 466 (105) pmol/l for aldosterone and 8.4 (5.2) pmol/l for ANP. Hormones were determined in 29 of 32 cases at baseline, and in 23 of 32 cases at 28 days after TIPS.
Echocardiography was performed using a 2.5 or 3.5 MHz phased array transducer probe through the left parasternal view (B‐mode and M‐mode) and the apical four‐chamber subcostal view (B‐mode), according to the conventions of the American Society of Echocardiography.12,13 In the apical four‐chamber view, a Doppler recording of diastolic transmitral flow was obtained by positioning the sample volume on the inflow area of the left ventricle, just below the level of the mitral annulus. The left ventricular output tract flow was obtained by an apical five‐chamber view and by positioning the Doppler sample volume just below the aortic leaflets.14 Measurements derived from at least three cardiac cycles were averaged.
The echocardiographic measures reported are: (a) left ventricular end diastolic volume (LVEDV), (b) left ventricular end systolic volume (LVESV), (c) left ventricular ejection fraction, (d) stroke volume (SV), (e) cardiac output (CO), (f) systemic vascular resistance (SVR), (g) right ventricular systolic pressure (RVSP), (h) early maximal ventricular filling velocity (E) and late ventricular or maximal filling velocity (A) during atrial systole, (i) E/A ratio and (j) deceleration time (DT). LVEDV and LVESV were calculated using the Simpson biplane method. SV, CO and SVR were calculated by the following formulas:
SV = (left ventricular outflow tract area)×(mean blood velocity across aortic valve)×(ejection time); CO = SV×HR; SVR = (MAP×80)/CO.
E and A waves are indicators of the ventricular filling dynamics. Hence, the E/A ratio is used to estimate the diastolic function of the ventricle. In normal subjects, the E wave is greater than the A wave, and the E/A ratio is greater than 1. In case of the contrary, the diastolic ventricular function is considered to be impaired, and the atrial component of the ventricular filling to have become preponderant.15 DT is the time elapsing from the peak and the end of the E wave, and is longer when the ventricular filling time is prolonged. Hence, an increase in DT indicates a reduction in ventricular relaxation due to impaired decay of left ventricular pressure during diastole.
The same operator (GP) performed all examinations. The intraobserver coefficient of variability in the E/A echocardiographic measure was 7%.
The baseline echocardiographic data of the patients with cirrhosis studied were compared with those previously measured in 16 healthy subjects (median age 58 years, range 36–80).8
Statistical analysis
All data are expressed as means (SEM), or as absolute numbers and percentages. Echocardiographic and haemodynamic data were compared between different subgroups of patients with cirrhosis, as well as between patients with cirrhosis and 16 healthy subjects, with the Mann–Whitney U test or the χ2 test. Comparisons between pre‐TIPS and post‐TIPS values of patients with cirrhosis were made using the Wilcoxon test or the χ2 test.
The probability of survival without liver transplantation was estimated using the Kaplan–Meier method and compared using the log‐rank test. Continuous variables were dichotomised according to clinically relevant cut‐off or median values. Univariate and multivariate analyses were performed using Cox's regression model. Only variables in the univariate analysis that significantly related to survival were introduced in the multivariate model. Survival at fixed times (3, 6 and 12 months) was also evaluated, and both the sensitivity and the specificity of the post‐TIPS E/A ratio were estimated.
The Spearman correlation was used to compare percentage changes in E/A with percentage changes in other variables.
A p value <0.05 was considered to be significant. All calculations were processed using the SPSS software package for Macintosh (SPSS V11.0.2).
Results
Table 1 shows the demographic data from the 32 patients with cirrhosis included in the study. Four patients belonged to Child class A, 19 to Child class B and 9 to Child class C. Out of 32 patients, two had a model of end‐stage liver disease (MELD) score >18, and four had a creatinine level >132 μmol/l.
Table 1 Clinical, laboratory and demographic features of 32 patients with cirrhosis treated with transjugular intrahepatic portosystemic shunt.
| Variable | |
|---|---|
| Age (years) | 61 (1.6) |
| Sex (M/F) | 21/11 |
| Aetiology (viral/alcohol/other) | 14/11/7 |
| TIPS indication (bleed/ascites) | 10/22 |
| Child–Pugh class (A/B/C) | 4/19/9 |
| Child–Pugh score | 8 (0.3) |
| MELD score | 10 (0.8) |
| Serum bilirubin (μmol/l) | 35.9 (3.4) |
| Serum albumin (g/l) | 30 (1.2) |
| INR (ratio) | 1.23 (0.02) |
| ALT (U/l) | 33 (3) |
| Serum creatinine (μmol/l) | 90.1 (6.2) |
| Serum sodium (mmol/l) | 135 (1) |
| Ascites (absent/mild/severe) | 5/7/20 |
ALT, alanine aminotransferase; F, female; INR, international normalised ratio; M, male; MELD, model of end‐stage liver disease; TIPS, transjugular intrahepatic portosystemic shunt.
Values are mean (SD) unless they are otherwise defined.
In terms of haemodynamic/echocardiographic characteristics, the 32 patients with cirrhosis significantly differed from 16 healthy subjects, in having lower MAP and SVR values, a lower E/A ratio, and a longer DT (table 2). An E/A ratio ⩽1 was present in 18 patients (8 with alcoholic cirrhosis and 10 with non‐alcoholic cirrhosis).
Table 2 Echocardiographic and haemodynamic measures obtained in 16 healthy subjects and in 32 patients with cirrhosis.
| Variable | Healthy subjects (n = 16) | Patients with cirrhosis (n = 32) | p Value |
|---|---|---|---|
| Mean arterial pressure (mm Hg) | 98 (2) | 85 (2) | <0.001 |
| Heart rate (bpm) | 66 (3 | 73 (2) | 0.07 |
| LVEDV (ml) | 89 (5) | 94 (6) | 0.94 |
| LVESV (ml) | 30 (3) | 34 (3) | 0.91 |
| LVEF (%) | 66 (3) | 66 (2) | 0.61 |
| Stroke volume (ml) | 59 (3) | 61 (3) | 0.85 |
| Cardiac output (l/min) | 4.0 (0.3) | 4.4 (0.2) | 0.29 |
| E/A ratio | 1.15 (0.06) | 0.97 (0.05) | 0.04 |
| Deceleration time (ms) | 191 (7) | 234 (8) | 0.001 |
| RVSP (mm Hg) | 19 (1) | 23 (1) | 0.07 |
| SVR (dyne s/cm5 m2) | 2094 (166) | 1639 (77) | 0.01 |
E/A, early maximal ventricular filling velocity/late filling velocity; LVEDV, left ventricular end diastolic volume; LVESV, left ventricular end systolic volume; LVEF, left ventricular ejection fraction; RVSP, right ventricular systolic pressure; SVR, systemic vascular resistance.
Table 3 compares the haemodynamic/echocardiographic and hormonal values measured before and after TIPS insertion. At 28 days after TIPS, LVEDV, LVESV, SV, CO and ANP mean values had significantly increased, whereas SVR and PRA values had significantly decreased. The post‐TIPS E/A ratio was also significantly increased (p = 0.008).
Table 3 Echocardiographic, haemodynamic and humoral measures obtained before and 28 days after transjugular intrahepatic portosystemic shunt implantation in 32 patients with cirrhosis.
| Variable | Before TIPS | After TIPS | p Value |
|---|---|---|---|
| Mean arterial pressure (mm Hg) | 85 (2) | 86 (2) | 0.18 |
| Heart rate (bpm) | 73 (2) | 78 (2) | 0.043 |
| LVEDV (ml) | 94 (6) | 111 (5) | 0.001 |
| LVESV (ml) | 34 (3) | 42 (3) | 0.008 |
| LVEF (%) | 66 (2) | 63 (2) | 0.11 |
| Stroke volume (ml) | 61 (3) | 68 (3) | 0.010 |
| Cardiac output (l/min) | 4.4 (0.2) | 5.5 (0.2) | <0.001 |
| E/A ratio | 0.97 (0.05) | 1.19 (0.08) | 0.008 |
| Deceleration time (ms) | 234 (8) | 216 (8) | 0.16 |
| RVSP (mm Hg) | 23 (1) | 26 (2) | 0.43 |
| SVR (dyne s/cm5 m2) | 1639 (77) | 1310 (54) | <0.001 |
| Plasma renin activity (ng/l⋅s) | 3.2 (0.6)* | 2.0 (0.47)† | 0.026 |
| Aldosterone (pmol/l) | 1642 (319)* | 971 (164)† | 0.26 |
| Atrial natriuretic peptide (pmol/l) | 29 (3.9)* | 47 (7.46)† | 0.021 |
E/A, early maximal filling velocity/late filling velocity; LVEDV, left ventricular end diastolic volume; LVESV, left ventricular end systolic volume; LVEF, left ventricular ejection fraction; RVSP, right ventricular systolic pressure; SVR, systemic vascular resistance; TIPS, transjugular intrahepatic portosystemic shunt.
*The reported data were obtained from 29 patients.
†The analysis was performed on 23 patients. In these patients, at baseline, plasma renin activity was 3.47 (0.78) ng/l⋅s, aldosterone 1548 (355) pmol/l and atrial natriuretic peptide 28 (4.2) pmol/l.
After TIPS, the number of patients with a normal E/A ratio (>1) increased from 14 to 22, whereas that of patients with a low E/A ratio (⩽1) decreased from 18 to 10. Percentage changes of E/A ratio at 28 days after TIPS were directly related to percentage changes of ANP (r = 0.46, p = 0.029), LVEDV (r = 0.37, p = 0.042) and SV (r = 0.42, p = 0.023). In contrast, they were inversely related to the percentage changes of PRA (r = −0.51, p = 0.013) and DT (r = −0.60, p = 0.005).
Outcome of patients
During a median follow‐up of 19 months (range 2–63), 15 patients died, four received orthotopic liver transplantation, and three dropped out after 9, 13 and 32 months, respectively. Nine patients (6 had a post‐TIPS E/A ratio <1) died from end‐stage liver failure and hepatorenal syndrome (after a mean (SD) of 19 (7) months, range 2–63), two from hepatocellular carcinoma complications (after 5 and 35 months, respectively), one from sepsis (after 34 months), one from gastrointestinal bleeding (after 20 months) and two from causes unrelated to liver disease (after 6 and 18 months). No deaths were caused by cardiac failure.
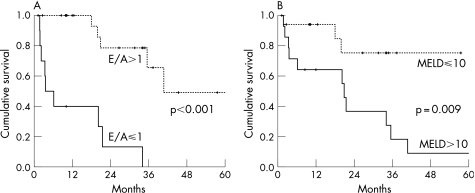
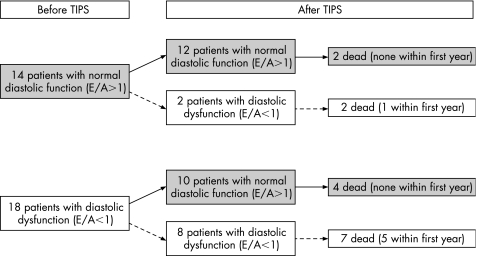
All variables reported in tables 1 and 3 were considered for the prediction of survival. Univariate analysis revealed two variables significantly related to death: an E/A ratio ⩽1 at 28 days (RR 11.9, 95% CI 3.18 to 45, p<0.001) and a baseline MELD score >10 (RR 4.67, 95% CI 1.3 to 16.8, p<0.02). These variables also maintained their predictive value after censoring of the four patients with liver‐unrelated deaths (E/A ratio ⩽1: RR 14, 95% CI 2.8 to 69, p<0.001; baseline MELD score >10: RR 5.0, 95% CI 1.1 to 23.7, p<0.04) or excluding them from the analysis (E/A ratio ⩽1: RR 14, 95% CI 2.9 to 68, p<0.001; baseline MELD score >10: RR 6.0, 95% CI 1.3 to 28.6, p<0.023). Figure 1 shows the cumulative probability of survival of patients stratified for the respective cut‐off values of these two predictors. On including these two variables in a multivariate analysis, it was found that post‐TIPS E/A ratio is independently related to survival (RR 8.9, 95% CI 1.9 to 41.5, p = 0.005). Figure 2 shows a flow chart of patient outcomes according to the diastolic function, estimated as E/A ratio both before TIPS and 28 days after TIPS. All of the six patients who died during the first year of follow‐up had a post‐TIPS E/A ratio ⩽1. This accurately predicted the outcome at 3, 6 and 12 months of follow‐up. Specificity ranged from 0.74 to 0.84, with a sensitivity value of 1.0.
Figure 1 Actuarial curves showing the survival probability of patients stratified for the post‐transjugular intrahepatic portosystemic shunt E/A (early maximal ventricular filling velocity/late filling velocity) ratio (A), and baseline model of end‐stage liver disease score (B). p Values were estimated by the log‐rank test. MELD, model and end‐stage liver disease.
Figure 2 Flow chart showing the outcome of 32 patients with cirrhosis according to baseline and post‐transjugular intrahepatic portosystemic shunt (TIPS) diastolic function. E/A, early maximal ventricular filling velocity/late filling velocity.
Comparison of patients with low (⩽1) and normal (>1) post‐TIPS E/A ratio
At baseline, patients with a post‐TIPS E/A ratio ⩽1 (group 1) differed from patients with an E/A ratio >1 (group 2) in having a higher MELD score (14 (1) vs 9 (1), p = 0.012) and higher serum creatinine levels (1.3 (0.15) vs 0.9 (0.07) mg/dl, p = 0.027). In particular, no significant differences were found according to age (65 (1.6) vs 59 (2) years, p = 0.10), aetiology of liver disease (alcoholics: 30% vs 36%, p = 0.72; viral: 60% vs 54%, p = 0.77) or portosystemic pressure gradient, measured both before and after TIPS insertion (pre‐TIPS portosystemic pressure gradient: 22 (1) vs 24 (1) mm Hg, p = 0.26; post‐TIPS PPG: 7 (1) vs 9 (1) mm Hg, p = 0.2).
No significant differences were found in the haemodynamic measurements, even though MAP and CO tended to be lower in patients of group 1 (table 4). Furthermore, changes after TIPS were significantly different for DT, which improved only in group 2, and for left ventricular ejection fraction, which decreased only in group 1. Lastly, regarding changes in hormonal values, plasma ANP significantly increased (from 26 (4.9) to 61 (10.7) pmol/l, p = 0.004), whereas PRA only significantly decreased (from 2.83 (0.66) to 1.17 (0.25) ng/l⋅s, p = 0.006) in group 2 patients (fig 3).
Table 4 Comparison of patients with and without diastolic dysfunction at 28 days after transjugular intrahepatic portosystemic shunt implantation.
| Variables | Before TIPS | After TIPS (%) | ||||
|---|---|---|---|---|---|---|
| Group 1 (E/A <1) | Group 2 (E/A >1) | p Value | Group 1 (E/A <1) | Group 2 (E/A >1) | p Value | |
| Mean arterial pressure (mm Hg) | 79 (4) | 87 (2) | 0.06 | +10 (4) | +1 (3) | 0.13 |
| Heart rate (bpm) | 73 (5) | 73 (3) | 0.79 | +11 (4) | +9 (5) | 0.90 |
| LVEDV (ml) | 99 (13) | 92 (5) | 0.84 | +22 (11) | +22 (5) | 0.89 |
| LVESV (ml) | 36 (6) | 32 (4) | 0.57 | +69 (27) | +38 (15) | 0.42 |
| LVEF (%) | 65 (3) | 66 (2) | 0.76 | −11 (6) | 0 (3) | 0.046 |
| Stroke volume (mL) | 63 (7) | 60 (3) | 0.85 | +6 (9) | +22 (6) | 0.15 |
| Cardiac output (l/min) | 4.0 (0.4) | 4.6 (0.2) | 0.18 | +32 (9) | +29 (5) | 0.87 |
| E/A ratio | 0.87 (0.10) | 1.02 (0.05) | 0.14 | +11 (13) | +40 (15) | 0.22 |
| Deceleration time (ms) | 227 (14) | 238 (11) | 0.73 | +8 (11) | −12 (4) | 0.043 |
| RVSP (mm Hg) | 22 (2) | 24 (2) | 0.59 | +21 (15) | +16 (14) | 0.53 |
| SVR (dyne s/cm5 m2) | 1713 (171) | 1606 (82) | 0.68 | −13 (7) | −20 (4) | 0.36 |
E/A, early maximal filling velocity/late filling velocity; LVEDV, left ventricular end diastolic volume; LVESV, left ventricular end systolic volume; LVEF, left ventricular ejection fraction; RVSP, right ventricular systolic pressure; SVR, systemic vascular resistance; TIPS, transjugular intrahepatic portosystemic shunt.
Baseline haemodynamic measures and the relative post‐TIPS percentage changes.
Figure 3 Plasma renin activity (PRA, A), aldosterone (ALDO, B) and atrial natriuretic peptide (ANP, C) values before and 28 days after transjugular intrahepatic portosystemic shunt (TIPS) implantation in patients with cirrhosis, stratified according to post‐TIPS early maximal ventricular filling velocity/late filling velocity (E/A) ratio. Data were obtained from 23 patients. *p<0.01 versus respective baseline values.
Discussion
The outcome of patients treated with TIPS is often unpredictable, because the favourable effects of stenting on bleeding and ascites can be negated by the risk of progressive liver failure that leads to death within a few months or even weeks. The most likely cause of this negative event is a reduction in portal vein liver perfusion not compensated for by an increase in arterial perfusion. This makes it plausible that cardiac and haemodynamic dysfunction and their features can be related to the probability of post‐TIPS survival.
The present study shows that a post‐TIPS E/A ratio ⩽1, a feature of diastolic dysfunction, is significantly related to the death of patients with cirrhosis treated with TIPS. The only other variable associated with death in the univariate analysis was a high baseline MELD, a score originally obtained as a predictor of the outcome of patients with cirrhosis treated with TIPS,16 and recently validated in other clinical contects of liver cirrhosis.17,18,19 Cox's regression analysis showed that the post‐TIPS E/A ratio was independently related to death. However, owing to the low number of patients and end points, the confidence of this result, as suggested by the wide confidence interval, is limited.
It is worth mentioning that no patients with a post‐TIPS E/A ratio >1 died during the first year of follow‐up, whereas 6 of 10 patients with E/A ⩽1 died during the same period (fig 2). This could mean that the E/A ratio might be a useful predictor in patients who receive TIPS as a bridge to liver transplantation, because patients with a post‐TIPS E/A ratio ⩽1 should be transplanted sooner than those with a normal E/A ratio. However, any potential clinical application of E/A ratio in this setting should be preceded by confirmation of the present results in an independent cohort of patients with cirrhosis.
As no patient participating in this study died of cardiac failure, the reason why the presence of post‐TIPS diastolic dysfunction was related to shorter survival is uncertain. The most favoured hypothesis is that diastolic dysfunction can simply identify patients with more advanced liver disease, who have a high risk of dying after TIPS because of progressive liver failure caused by the reduction of hepatic blood perfusion, or who have a high risk of developing classic cirrhotic complications. This hypothesis is supported by the association found between a low post‐TIPS E/A value and a baseline elevated MELD score, which encompasses variables estimating both liver and kidney functions. A strict relationship between cardiac diastolic dysfunction and liver function is also supported by the evidence that the E/A ratio is lower in patients with ascitis than in those with compensated cirrhosis,8 and by the recent demonstration that diastolic dysfunction can be completely reversed after liver transplantation.20
However, a different explanation is possible, involving the concept that, although patients with diastolic dysfunction do not show overt cardiac failure, they have a substantial limitation in exercise tolerance, owing to a limited ability to use the Frank–Starling mechanism.21 Indeed, impaired cardiac response and a reduction in anaerobic capacity in patients with cirrhosis during physical exercise were demonstrated by Wong et al.22 Accordingly, patients with cirrhosis with diastolic dysfunction might have a subtle cardiac dysfunction that makes them more fragile when they develop serious complications such as renal failure or sepsis. This hypothesis is supported by our finding that six out of the nine patients who died because of hepatorenal syndrome had a post‐TIPS E/A ratio ⩽1. A role played by the heart in the occurrence and outcome of hepatorenal syndrome was also suggested by Ruiz del Arbol et al,23 who found that, in patients with cirrhosis with spontaneous bacterial peritonitis, the risk of hepatorenal syndrome and death was inversely related to the cardiac output.
The origin of diastolic dysfunction in patients with cirrhosis is also a topic of debate.24 The study presented here found no relationship between the presence of diastolic dysfunction and the alcoholic or viral aetiology of liver disease, thus confirming that cirrhotic cardiomyopathy is independent of alcohol aetiology. As the prevalence of diastolic dysfunction varies directly with the mean age of the population,21 it cannot be excluded that older age adversely affected the E/A ratio of some patients, considering that there was a slight but insignificant correlation of E/A ratio with age (p = 0.1) in the study.
Conceptually, diastolic dysfunction occurs when the process of ventricular relaxation is prolonged, slowed or incomplete.21 This abnormality can be caused by increased stiffness in the ventricle,25 and also by any event that reduces the left atrial pressure, including low blood volume and low preload.5,12 Some investigators suggested that the increased stiffness of the myocardium, which causes diastolic dysfunction in cirrhosis, is due to thickening of the ventricular walls and of the interventricular septum,4,26,27 but others did not find any modification in the width of the ventricular walls.2 However, the structural characteristics of the hearts of the patients in this study were not investigated. Hyperaldosteronism is a common finding in patients with decompensated cirrhosis and has been shown to have a direct effect on the heart by way of causing fibrosis, stiffness and diastolic dysfunction,28 but a significant relationship between plasma aldosterone levels and the E/A ratio was not found in this study. Recently, Pozzi et al29 showed that a 6‐month administration of an aldosterone receptor antagonist to patients with Child A cirrhosis did not improve the low E/A ratio but reduced the end LVEDV and the left ventricular wall thickness. However, the inefficacy of the E/A ratio could have been due to the inadequate period of treatment.
In the study presented here, the changes in E/A ratio after TIPS were directly correlated with the changes in ANP concentrations and inversely correlated with the changes of PRA. Taking into account the relationships of these hormones with the effective blood volume, it is conceivable that, at least in patients in whom TIPS insertion normalised the E/A ratio, the low pre‐TIPS E/A ratio was partly due to central hypovolaemia and low atrial pressure, which were corrected after TIPS. An increase in central blood volume was also suggested by the observation that, after TIPS cardiac output, LVEDV and LVESV significantly increased but the blood pressure did not change. Conversely, in patients in whom TIPS did not normalise the E/A ratio, diastolic dysfunction might have been caused by structural alterations of the myocardium, involving a limited ability to use the Frank–Starling mechanism to increase SV.30 Indeed, unlike their counterparts with a normal E/A ratio, patients with a post‐TIPS E/A ratio ⩽1 showed a reduction in SV and a failure in ANP increase after TIPS insertion (table 4). This interpretation could also explain why the post‐TIPS E/A ratio, but not the pre‐TIPS E/A ratio, was able to predict patient outcome in this study.
The main limitation of the present study is the relatively small number of patients; hence, the possibility of type 2 error cannot be excluded. In this case, the statistical analysis could have overlooked evidence for other predictive factors and differences. These limitations mean that further evaluation of the E/A ratio in a larger and independent cohort of patients is necessary before it can be adjudged a useful predictor in patients with TIPS.
In conclusion, a low E/A ratio, a feature of diastolic dysfunction that may be easily measured by pulsed Doppler during echocardiography, is shown to independently predict death in patients with TIPS. Measuring the E/A ratio is a simple, non‐invasive and cheap investigative technique that can be repeated as often as necessary and is a good prerequisite for a predictive test. Moreover, this result corroborates the hypothesis that cirrhotic cardiomyopathy is actively involved in the clinical outcome of patients with cirrhosis and deserves to be studied in other complications of portal hypertension.
Acknowledgements
ED is a recipient of a research grant from COPEV (Comitato per la prevenzione dell'epatite virale). IC is a recipient of a grant from Ospedale Maggiore Policlinico IRCCS, Milano, Italy.
Abbreviations
A - atrial maximal filling velocity
ANP - atrial natriuretic peptide
CO - cardiac output
DT - deceleration time
E - early maximal ventricular filling velocity
LVEDV - left ventricular end diastolic volume
LVESV - left ventricular end systolic volume
MAP - mean arterial pressure
MELD - model of end‐stage liver disease
PRA - plasma renin activity
SV - stroke volume
SVR - systemic vascular resistance
TIPS - transjugular intrahepatic portosystemic shunt
Footnotes
Competing interests: None.
References
- 1.Ma Z, Lee S. Cirrhotic cardiomyopathy: getting to the heart of the matter. Hepatology 199624451–459. [DOI] [PubMed] [Google Scholar]
- 2.Valeriano V, Funaro S, Lionetti R.et al Modification of cardiac function in cirrhotic patients with and without ascites. Am J Gastroenterol 2000953200–3205. [DOI] [PubMed] [Google Scholar]
- 3.Finucci G, Desideri A, Sacerdoti D.et al Left ventricular diastolic function in liver cirrhosis. Scand J Gastroenterol 199631279–284. [DOI] [PubMed] [Google Scholar]
- 4.Wong F, Liu P, Lily L.et al Role of cardiac structural and functional abnormalities in the pathogenesis of hyperdynamic circulation and renal sodium retention in cirrhosis. Clin Sci 199997259–267. [PubMed] [Google Scholar]
- 5.Zile M R, Brutsaert D L. New concepts in diastolic dysfunction and diastolic heart failure: part I. Diagnosis, prognosis and measurements of diastolic function. Circulation 20021051387–1393. [DOI] [PubMed] [Google Scholar]
- 6.Boyer T D, Haskal Z J. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology 200541386–400. [DOI] [PubMed] [Google Scholar]
- 7.Braverman A C, Steiner M A, Picus D.et al High‐output congestive heart failure following transjugular intrahepatic portal‐systemic shunting. Chest 19951071467–1469. [DOI] [PubMed] [Google Scholar]
- 8.Salerno F, Cazzaniga M, Pagnozzi G.et al Humoral and cardiac effects of TIPS in cirrhotic patients with different “effective” blood volume. Hepatology 2003381370–1377. [DOI] [PubMed] [Google Scholar]
- 9.Arroyo V, Gines P, Gerbes A L.et al Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology 199623164–176. [DOI] [PubMed] [Google Scholar]
- 10.Salerno F, Merli M, Riggio O.et al Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 200440629–635. [DOI] [PubMed] [Google Scholar]
- 11.Salerno F, Badalamenti S, Moser P.et al Atrial natriuretic factor in cirrhotic patients with tense ascites. Effect of large volume paracentesis. Gastroenterology 1990981063–1070. [DOI] [PubMed] [Google Scholar]
- 12.Sahn D J, DeMaria A, Kisslo J.et al Recommendations regarding quantitation in M‐mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978581072–1083. [DOI] [PubMed] [Google Scholar]
- 13.Henry W L, DeMaria A, Gramiak R.et al Report of the American Society of Echocardiography: nomenclature and standards in two‐dimensional echocardiography. Circulation 198062212–217. [DOI] [PubMed] [Google Scholar]
- 14.Sunagawa K, Maugham W L, Burkhoff D.et al Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol 1983245H773–H780. [DOI] [PubMed] [Google Scholar]
- 15.Gibson D G, Francis D P. Clinical assessment of left ventricular diastolic function. Heart 200389231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malinchoc M, Kamath P S, Gordon F D.et al A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 200031864–871. [DOI] [PubMed] [Google Scholar]
- 17.Kamath P S, Wiesner R H, Malinchoc M.et al A model to predict survival in patients with end‐stage liver disease. Hepatology 200133464–470. [DOI] [PubMed] [Google Scholar]
- 18.Said A, Williams J, Holden J.et al Model of end stage liver disease score predicts mortality across a broad spectrum of liver disease. J Hepatol 200440897–903. [DOI] [PubMed] [Google Scholar]
- 19.Dunn W, Jamil L H, Brown L S.et al MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology 200541353–358. [DOI] [PubMed] [Google Scholar]
- 20.Torregrosa M, Aguade S, Dos L.et al Cardiac alterations in cirrhosis: reversibility after liver transplantation. J Hepatol 20054268–74. [DOI] [PubMed] [Google Scholar]
- 21.Aurigemma G P, Gaasch W H. Diastolic heart failure. N Engl J Med 20043511097–1105. [DOI] [PubMed] [Google Scholar]
- 22.Wong F, Girgrath N, Graba J.et al The cardiac response to exercise in cirrhosis. Gut 200149268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz del Arbol L, Urman J, Gonzales M.et al Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology 2003381210–1218. [DOI] [PubMed] [Google Scholar]
- 24.Blendis L, Wong F. Is there a cirrhotic cardiomyopathy? Am J Gastroenterol 2000113026–3028. [DOI] [PubMed] [Google Scholar]
- 25.Gilbert J C, Glantz S A. Determinants of left ventricular filling and of the diastolic pressure–volume relation. Circ Res 198964827–852. [DOI] [PubMed] [Google Scholar]
- 26.Pozzi M, Carugo S, Boari G.et al Evidence of structural and functional cardiac abnormalities in cirrhotic patients with and without ascites. Hepatology 1997261131–1137. [DOI] [PubMed] [Google Scholar]
- 27.Wong F, Siu S, Liu P.et al Brain natriuretic peptide: is it a predictor of cardiomyopathy in cirrhosis? Clin Sci 2001101621–628. [PubMed] [Google Scholar]
- 28.Weber K T. Aldosterone in congestive heart failure. N Engl J Med 20013451689–1697. [DOI] [PubMed] [Google Scholar]
- 29.Pozzi L, Grassi G, Ratti L.et al Cardiac, neuroadrenergic, and portal hemodynamic effects of prolonged aldosterone blockade in postviral Child A cirrhosis. Am J Gastroenterol 20051001110–1116. [DOI] [PubMed] [Google Scholar]
- 30.Little W C, Kitzman D W, Cheng C P. Diastolic dysfunction as a cause of exercise intolerance. Heart Fail Rev 20005301–306. [DOI] [PubMed] [Google Scholar]