An intraneural location for benign granular cell tumours, as well as plexiform architecture with perineural localisation of granular cell tumours of the skin, has been described. We describe the first case of a plexiform intraneural granular cell tumour, morphologically akin to a plexiform neurofibroma. It presented in a 23‐year‐old woman who had multiple soft‐tissue digital lesions on her right hand and one lesion on her left hand. The lesions presented with sensory neurological changes on physical examination. A plexiform architecture with an elongated mass with lobular growth, entirely encased within a fibrovascular connective tissue epineurial/perineurial coat, was noted. The histological findings of a monotonous polygonal and spindle cell proliferation with banal nuclear morphology and granular eosinophilic cytoplasm was typical of a granular cell tumour. The tumour was positive for the usual markers including periodic acid Schiff (PAS), S100 and CD68, and the intraneural location was demonstrated with recognition of the residual nerve bundles and myelinated axons on Luxol fast blue (LFB) staining. There was no history of neurofibromatosis type 1 or 2 in this patient. Recognition of this entity is important, as the natural history of this plexiform lesion is unknown, and the presence of multiple additional nodules in this patient requires further clinical follow‐up.
Granular cell tumours are benign neoplasms of presumed peripheral nerve, Schwann cell origin. They have been described in numerous locations including the skin and soft tissue, breast, tongue, oesophagus and many other sites.1,2,3,4 They have also been reported to be multiple in many cases1,3,5,6 and associated with other malignant neoplasms.7 Plexiform granular cell tumours have been described in the skin, which are characterised by a lobular growth pattern with perineural involvement,8 but to the best of our knowledge, an entirely intraneural granular cell tumour with a plexiform pattern reminiscent of plexiform neurofibroma has not been described previously.
Case report
A woman in her 20s, with no medical history or family history of neurofibromatosis type 1 or 2, presented to a plastic surgeon with multiple small nodules on the digits of her right hand and one nodule on her left hand. The lesions were found on the volar and dorsal surfaces of multiple digits. There was no known history of trauma to her hand. On physical examination, the lesions were smooth, mobile subcutaneous masses and there was a Tinel's sign, raising suspicion of cutaneous sensory nerve involvement. The patient consented to have one of the nodules from the dorsum of the right index finger removed for diagnosis, which, at the time of surgery, grossly appeared to be a sausage‐shaped smooth tan–white mass measuring 0.8×0.2×0.2 cm.
Materials and methods
The specimen was submitted in toto after being fixed in 10% neutral buffered formalin, and was processed in a routine fashion. In addition to H&E stains, PAS and PAS/LFB, immunohistochemistry was performed on the formalin‐fixed, paraffin wax‐embedded tissue using the liquid streptavidin–biotin complex immunoperoxidase method, with diaminobenzidine as chromogen. S100, CD68 and epithelial membrane antigen immunostains were performed.
Results
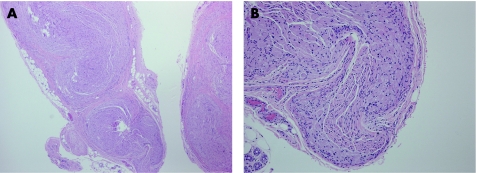
Microscopically, the lesion was an elongated mass with a plexiform architecture and was surrounded by a thin layer of epineurial or perineurial fibrovascular tissues with a small amount of normal adipose tissue around it (fig 1A). Within the lesion small remnants of the nerve were still intact, but most of the nerve was replaced by a proliferation of polygonal and spindle‐shaped cells with voluminous pink granular cytoplasm. The nuclei were monotonous with small central nucleoli. There were no granular cells within the fibrovascular tissue or adipose tissue. There was no necrosis or mitotic activity. The entirely intraneural location of the proliferation and the plexiform, or multilobulated, architecture of the lesion was reminiscent of a plexiform neurofibroma. However, the lesion was entirely made up of granular cells, with no myxoid stroma or wavy neurofibroma type cells. Similar to a neurofibroma, the granular cells could be seen between the epineurial/perineurial nerve sheath and the central residual nerve bundle (fig1B).
Figure 1 (A) H&E stain of an encapsulated mass with a fibrovascular connective tissue perineurial coat, demonstrating lobularity/plexiform architecture (magnification 25×). (B) H&E stain of the granular cells proliferating between the epineurial/perineurial fibrovascular tissues and the central residual nerve bundle (magnification 100×).
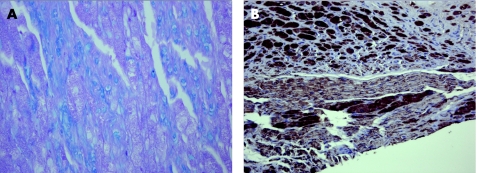
The lesion was examined with histochemical stains for PAS and a combined PAS/LFB to differentiate the granular cells from the myelin sheaths of the remaining axons in the nerve. The granular cells were strongly positive for PAS, demonstrating the granular cytoplasm, and the LFB demonstrated the remaining nerve bundles as well as individual axons scattered throughout the lesion (fig 2A). Granular cells could be seen inside the remaining nerve bundles. The presence of residual axons and sheaths throughout the lesion demonstrates the intraneural location of the lesion, rather than granular cells just surrounding small soft‐tissue nerves. The lesion was also stained with an immunohistochemical marker for S100, which diffusely stained both the granular cells and the residual nerve bundles, with stronger staining of the granular cells (fig 2B). It was also stained for CD68, which stained the granular cells, but not the residual nerve bundles. The epithelial membrane antigen showed focal and faint staining of the epineurial or perineurial fibrovascular tissues surrounding the lesion.
Figure 2 (A) Periodic acid Schiff (PAS)/Luxol fast blue stain showing residual blue myelinated axons interspersed among eosinophilic PAS‐positive cells (magnification 400×). (B) S100 staining of granular cells (strong) and a residual nerve bundle in the lower part of the image (weak; magnification 200×).
Discussion
Granular cell tumours in an intraneural location are rare. Four cases have been described previously, with two cases in the ulnar nerve, one in the breast and one in the S1 nerve root.9,10,11,12 None of these had a plexiform pattern. The age range for patients presenting with these tumours is 16–66 years old. Some have been easily dissected off the nerve, with the majority of the intraneural growth in nerve twigs outside the major nerve trunks, whereas others could not be resected with nerve salvage.
We report the case of a 23‐year‐old patient with multiple nodules in the digits of both hands, one of which showed an entirely intraneural granular cell tumour with lobular plexiform architecture. The digital sensory cutaneous nerve was entirely involved and therefore removed. The remaining nodules in this patient have been asymptomatic to date, and are currently being followed. Multiple granular cell tumours in the same patient have been described previously.1,3,5,6 Interestingly, the tumour described here had a lobular growth pattern mimicking a plexiform neurofibroma, with fibrovascular connective tissue separating and surrounding the entirety of each lobule. There were no wavy buckled nuclei, ropey collagen or myxoid ground substance, typical of a neurofibroma. No granular cells were found within or beyond the fibrovascular connective tissue coat. The description of a plexiform granular cell tumour of this nature has not been described. Lee et al8 described two cases of plexiform granular cell tumour of the skin, which were also not associated with neurofibromatosis type 1, but used the term plexiform to describe the lobular growth around, and not within, nerve bundles. Their description implies perineural involvement of nerves in the skin as opposed to pure intraneural growth. The presence of residual nerve trunks with granular cells inside them and individual myelinated axons (on LFB stain) scattered throughout the lesion demonstrates the intraneural location of the entire tumour in our case. This is in keeping with the clinical presentation of sensory nerve findings (Tinel's sign) and the gross finding of an elongated lesion with no granular cells in the adipose tissue around it microscopically. Most typical granular cell tumours are not elongated masses and usually have infiltrative margins as opposed to circumscription.
The plexiform nature of this lesion is of uncertain significance. The patient has no personal or family history of neurofibromatosis type 1. The natural history of this tumour and its potential for transformation to malignancy is unknown, but is presumed to be similar to a typical granular cell tumour rather than to a plexiform neurofibroma. However, neurofibromas with focal granular cells within them have been described in patients with neurofibromatosis, and in one case in the literature a malignant granular cell tumour arose in a patient who had previous neurofibromas containing granular cells.13,14 Follow‐up of the remainder of our patients' lesions will therefore be essential. The existence of plexiform intraneural granular cell tumours as distinct from typical granular cell tumours and the previously mentioned plexiform tumours of the skin described by Lee et al should be recognised, owing to this uncertainty.
Footnotes
Competing interests: None declared.
References
- 1.Gross V L, Lynfield Y. Multiple cutaneous granular cell tumors: a case report and review of the literature. Cutis 200269343–346. [PubMed] [Google Scholar]
- 2.Adeniran A, Al‐Ahmadie H, Mahoney M C.et al Granular cell tumor of the breast: a series of 17 cases and review of the literature. Breast J 200410528–531. [DOI] [PubMed] [Google Scholar]
- 3.Esaki M, Aoyagi K, Hizawa K.et al Multiple granular cell tumors of the esophagus removed endoscopically: a case report. Gastrointest Endosc 199848536–539. [DOI] [PubMed] [Google Scholar]
- 4.Billeret Lebranchu V. Granular cell tumor. Epidemiology of 263 cases. Arch Anat Cytol Pathol 19994726–30. [PubMed] [Google Scholar]
- 5.Janouskova G, Campr V, Konkol'ova R.et al Multiple granular cell tumour. J Eur Acad Derm Venereol 200418347–349. [DOI] [PubMed] [Google Scholar]
- 6.Blandamura S, Altavilla G, Castoro C.et al Combined granular cell tumour of the esophagus and stomach: a case report and review of the literature. Ital J Gastroenterol 199325259–264. [PubMed] [Google Scholar]
- 7.Vinco A, Vettoretto N, Cervi E.et al Association of multiple granular cell tumors and squamous carcinoma of the esophagus: case report and review of the literature. Dis Esoph 200114262–264. [DOI] [PubMed] [Google Scholar]
- 8.Lee J, Bhawan J, Wax F.et al Plexiform granular cell tumor. A report of 2 cases. Am J Dermatopathol 199416537–541. [DOI] [PubMed] [Google Scholar]
- 9.Dahlin L B, Lorentzen M, Besjakov J.et al Granular cell tumour of the ulnar nerve in a young adult. Scand J Plast Reconstr Surg Hand Surg 20023646–49. [DOI] [PubMed] [Google Scholar]
- 10.Yasutomi T, Koike H, Nakatsuchi Y. Granular cell tumour of the ulnar nerve. J Hand Surg J Br Soc Surg 199924122–124. [DOI] [PubMed] [Google Scholar]
- 11.Altmeyer P. On the encapsulated intraneural granular cell tumor. Dermatologica 1980161270–279. [PubMed] [Google Scholar]
- 12.Haku T, Hosoya T, Hayashi M.et al Granular cell tumor of the spinal nerve root: MR findings. Radiat Med 200220137–140. [PubMed] [Google Scholar]
- 13.Finkel G, Lane B. Granular cell variant of neurofibromatosis: ultrastructure of benign and malignant tumors. Hum Pathol 198213959–963. [DOI] [PubMed] [Google Scholar]
- 14.Muller W, Dahmen H G. A combined neurofibroma‐granular cell tumor of the middle cranial fossa. Pathol Res Pract 1978163378–386. [DOI] [PubMed] [Google Scholar]