Abstract
Objective
To examine the impact of the Short Stay Transfer Policy (SSTP) on practice patterns.
Data Sources
This study uses data from the Centers for Medicare and Medicaid Services Medicare Provider Analysis and Review (MEDPAR) file, Home Health Standard Analytical File, 1999 Provider of Service file, and data from the 2000 United States Census.
Study Design
An interrupted time-series analysis was used to examine the length of stay (LOS) and probability of “early” discharge to post acute care (PAC).
Data Collection
Separate 100percent samples of all fee-for-service Medicare recipients undergoing either elective joint replacement (JR) surgery or surgical management of hip fracture (FX) between January 1, 1996 and December 31, 2000 were selected.
Principal Findings
Prior to implementation of the SSTP. LOS had been falling by 0.37 and 0.30 days per year for JR and FX patients respectively. After implementation of the SSTP, there was an immediate increase in LOS by 0.20 and 0.17 days, respectively. Thereafter, LOS remained flat. The proportion of patients discharged “early” to PAC had been rising by 4.4 and 2.6 percentage points per year for JR and FX patients respectively, to a peak of 28.8percent and 20.4percent early PAC utilization in September 1998. Immediately after implementation of the SSTP, there was a 4.3 and 3.0 percentage point drop in utilization of “early” PAC. Thereafter utilization of early PAC increased at a much slower rate (for JR) or remained flat (for FX). There was significant regional variation in the magnitude of response to the policy.
Conclusion
Implementation of the SSTP reduced the financial incentive to discharge patients early to PAC. This was accomplished primarily through longer LOS without meaningful change in PAC utilization. With the recent expansion of the SSTP to 29 DRGs (representing 34percent of all discharges), these findings have important implications regarding patient care.
Keywords: Medicare, Short Stay Transfer Policy, hip fracture, joint replacement, length of stay, post-acute care
Since the implementation in 1983 of the acute care prospective payment system, hospitals have had a strong financial pressure to reduce costs. These cost reductions have been achieved primarily through reduced length of stay (LOS) (Meyers et al. 1996; Metz and Freiberg 1998; Healy et al. 2002) and a greater reliance on postacute care (PAC) (Kenney and Holahan 1991; Manton et al. 1993; Prospective Payment Assessment Commission 1996; Forrest, Roque, and Dawodu 1999; Huusko et al. 1999). The initial substitution of PAC for longer LOS was first seen as an efficient transfer of care from the more expensive inpatient care setting to less expensive PAC settings. However, as the growth in PAC outpaced reductions in LOS, Congress became concerned that PAC was no longer cost saving (MEDPAC: Medicare Payment Advisory Commission 2000).
Therefore, to reduce the financial incentive to discharge patients “early” and thus reduce the utilization of potentially unnecessary PAC, in 1998 the Centers for Medicare and Medicaid Services (CMS) targeted 10 diagnosis-related groupings (DRGs) with the highest rate of PAC utilization for modifications to the DRG reimbursement system (Prospective Payment Assessment Commission 1997). At that time, these 10 DRGs represented 8.8 percent of all hospital discharges (Medicare Payment Advisory Commission 1999). By defining the relative odds of PAC use among short versus long hospitalizations, Cromwell, Donoghue, and Gilman (2002) demonstrated that these 10 DRGs were well chosen.
On October 1, 1998, Congress implemented the Short Stay Transfer Policy (SSTP) as part of the Balanced Budget Act of 1997 (One-hundred-fifth Congress of the United States of America 1997). Under this policy, hospital payments for these 10 DRGs were discounted for patients discharged “early” to a PAC setting. “Early” discharge was defined as any patient transferred to a PAC facility before the national geometric mean LOS for the related DRG. Qualifying PAC stays include transfer to skilled nursing facility or rehabilitation hospital or discharge to home with home health care beginning within 3 days of discharge. Despite well-documented regional variation in LOS (Chassin et al. 1986; Chassin et al. 1987) CMS purposefully selected a national geometric LOS rather than regional means as “national standardized [DRG payment] amounts … reflect costs across all regions” and “one of the reasons for this variation [in LOS] is the greater reliance on postacute care earlier in the stay in those areas with lower average lengths of stay” (Health Care Financing Administration 1998). In October 2003, CMS expanded this policy to include a total of 29 DRGs, bringing the proportion of all discharges subject to the transfer policy to 34 percent (Centers for Medicare and Medicaid Statistics 2004).
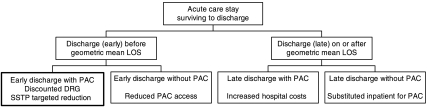
By discouraging “early” discharge to PAC with discounted payments, CMS had hoped to realize further cost savings through an increase in “late” discharge without PAC (substituting inpatient for postacute care; Health Care Financing Administration 1998; see Figure 1 for conceptual discharge decision model).
Figure 1.
Conceptual Model for Nested Logistic Statistical Design
A preferential increase in patients discharged “early” without PAC would suggest that hospitals were discouraging access to PAC. As authors have suggested beneficial effects of PAC and the rehabilitative care (Kane et al. 1996; Intrator and Berg 1998; Munin et al. 1998), reduction in PAC could have a potential harmful impact on patient care.
Alternatively, hospitals could simply keep patients in hospital longer without change in PAC utilization. Slowing the trend in shorter LOS could potentially improve patient care as some researchers have raised the concern that patients may be discharged too early after joint replacement (Mauerhan et al. 1998).
MEDPAC reported to Congress that the crude mean LOS for the 10 SSTP DRGs continued to fall between 1997 and 1999, but at a slower rate than non-SSTP DRGS (MEDPAC: Medicare Payment Advisory Commission 2000). However, during this same timeframe, Medicare implemented policy changes that affected skilled nursing and home health care markets potentially restricting access to PAC (One-hundred-fifth Congress of the United States of America 1997), which in turn could affect hospital LOS and use of early PAC.
To examine the impact of the SSTP and discern its effects from other concurrent policies, we selected a 100 percent sample of select Medicare fee-for-service claims between January 1, 1996 and December 31, 2000 for an interrupted time-series analysis so that month-to-month change in practice patterns could be correlated with the date of SSTP implementation. We hypothesized that implementation of the SSTP would attenuate or perhaps even reverse the historical trend for shorter hospital LOS, resulting in a smaller proportion of patients discharged “early” to PAC. We also tested for differential effects of the policy by patient, hospital, and regional characteristics.
METHODS
Patient Selection
Claims for all indexed hospital admissions, related skilled nursing facility, rehabilitation hospital and home health bills for patients undergoing joint replacement (JR) or surgical repair of hip fracture (FX) were requested. The major orthopedic procedures were selected as they represent half of all the original SSTP DRG discharges and have the highest utilization of PAC (MEDPAC: Medicare Payment Advisory Commission 2000). Analyses were performed separately for these two discrete clinical groups, which represent a broad range of the clinical spectrum from the relatively functional to the frail and vulnerable patient, each with unique PAC needs.
Patients undergoing JR were identified by either DRG (209) “Major joint and limb reattachment procedures of lower extremity,” which includes both hip- and knee-replacements or DRG (471), “bilateral or multiple major joint procedures of lower extremity.” Verification of surgery and inclusion in the study sample was confirmed by ICD-9 procedure codes 81.51–81.53 for hip replacement and 81.54–81.55 for knee replacement surgery.
Patients undergoing bilateral JR (DRG 471) and not covered under the SSTP were subsequently excluded from the primary analyses. Patients were also excluded from the sample if the elective nature of the surgery was unclear from the coded diagnoses. Sensitivity analyses were performed separately with and without the above restrictions. As the analysis yielded similar results, findings from the more narrowly defined elective JR sample are presented.
Patients undergoing surgical repair of hip fracture were identified with an ICD-9 diagnosis of 820.xx in the admitting or any one of the 10 diagnostic code positions. Surgical repair of hip fracture was confirmed with the hip replacement codes 81.51–81.53 or pinning codes 79.35, 79.15, or 78.55. Analyses were conducted on samples restricted to discharges covered by the SSTP: DRG 209 (detailed above) and DRG 210 or 211 (hip and femur procedures except major joint age greater than 17 with or without complications or comorbidities, respectively).
Dependent Variables
Hospital LOS was extracted from the annual MEDPAR files. For the less than 0.5 percent of patients with transfers between inpatient hospitals, the stays were collapsed into a single episode so that total LOS was summed. The hospital provider characteristics for the final discharging hospital were retained for analysis of hospital characteristics in the multivariate models.
To further examine whether hospitals were responding to the discounted DRG transfer policy, the probability of a patient being discharged “early” to a PAC venue was modeled. Qualifying PAC included contiguous-skilled nursing facility and rehabilitation hospital stays (identified from the MEDPAR files) as well as home health care beginning within 3 days of hospital discharges (as defined by the SSTP and identified from the Home Health Standard Analytic Files).
Main Independent Variables
To examine the temporal change in hospital LOS and probability of early discharge to PAC setting, 60 dummy variables were created to indicate the month of discharge (January 1996–December 2000) from the acute care hospital and included in the regression model. Due to censoring, the first 2 weeks of data were dropped from the sample.
To describe the before and after SSTP linear per annum change in LOS and probability of early discharge, separate models were run using one spline for each of the policy periods (Marsch and Cormier 2001) and a single dichotomous policy variable.
To examine whether the discharge to Home Health was delayed beyond the 3 days after discharge so as to avoid the SSTP discount, the conditional probability of Home Health beginning within 3 days was modeled among the sample of Home Health users.
Other Covariates
The analyses controlled for patient, hospital, and regional characteristics. Patient demographic factors included age at the time of surgery (by pentile), gender and race (Caucasian, African American and Other). A crude proxy for patient socioeconomic status was constructed by matching median income for each five-digit zip code from the 2000 U.S. Census to the patient's home zip code. Patient receipt of state aid (buy-in) for the Medicare program was also included in the model.
Patient medical characteristics included original reason for Medicare entitlement categorized as aged, disabled, end-stage renal disease, or disabled and end-stage renal disease. Medical comorbidities identified from the 10 MEDPAR diagnostic codes were categorized into 17 hierarchical categories using the Charlson comorbidity index (Deyo, Cherkin, and Ciol 1992).
Covariate surgical characteristics varied by indication. For patients undergoing JR, the indications included hip versus knee and revision versus primary replacement. For patients undergoing FX, the indications included replacement versus pinning and whether in-hospital complications were noted. As LOS is correlated with day of the week for discharge (attributable to constraints around weekend services) and the distribution of days of the week varies monthly, for better smoothing of the month-to-month trend, day of week of discharge was included in the model.
The analyses adjusted for the following hospital characteristics: teaching status, size, and rural versus urban status. The 10 CMS regions were used to both control for regional variation in national models and examine variation in outcomes across CMS region. More detailed regional variables included number of skilled nursing facility beds, number of rehabilitation hospital beds, number of home health nurses, and number of home health aides per hospital zip code. As there is little year-to-year variation in these institutional variables, these covariates were simply abstracted from the 1999 Provider of Service file. Regional PAC supply variables by zip code were matched to hospital zip codes. All values were per capita adjusted by including the hospital per zip code total population aged greater than or equal to 65 years in the model from the 2000 U.S. Census data. (For the less than 10 percent of hospitals with no associated census population, population counts from the patient zip code was used in its place as proxy for the local population.) County-level Medicare managed care market penetration for 1999 as reported by the Centers for Medicare and Medicaid Statistics was also included in the model (Centers for Medicare and Medicaid Services 1999).
Statistical Analysis
Linear regression was used to estimate LOS as a function of either the 59 calendar month dummy variables (with January 1996 as the reference period) or the two spline and single dummy policy variables. All models controlled for the aforementioned patient, hospital, and regional characteristics. Random effects models were used to adjust standard errors for correlation of observations within hospitals.
For patients surviving the hospital discharge, four discrete hospital discharge dispositions were modeled as outlined in Figure 1 using nested logistic models (Econometric Software Inc. 1995; Green 1999). Estimates from separate random effects logistic regressions for the probability of early discharge and the probability of PAC utilization, conditional on the timing of discharge, were combined to derive the probability for each of the four discrete discharge possibilities (Duan et al. 1983). As the estimates are products of separate models, to evaluate statistical significance the models were bootstrapped 500 times to approximate the sampling distributions of the estimates (Efron 1993; Mooney and Duval 1993). The maximum and minimum values generated from bootstrapping were used as the upper and lower bounds of confidence intervals.
Based on the post-SSTP reimbursement schedule, we hypothesized that patients with higher expected hospital costs might be preferentially discharged early under the SSTP. Therefore, to examine for differential treatment under the SSTP, additional models separately examined the interaction between policy variables and either medical comorbidities or patient age. To examine regional variation in response to the policy, stratified analyses were conducted using bootstrap methods to determine statistical significance as described above.
STATA version 7.0 (STATA 2002) and SAS version 8.2 (SAS Institute 2000) were used to perform all statistical analyses. Due to the size of the study cohort, to make the reporting of the statistical tests more clinically meaningful, tests are only reported when p<.0001 or when the range defined by the maximum and minimum values of the bootstrap estimate distribution do not include the null hypothesis value.
RESULTS
Sample Selection and Description (Joint Replacement Patients)
From the MEDPAR database, 1,369,842 cases of joint replacement surgery (for indication other than hip fracture) with hospital discharge dates between January 16, 1996 and December 31, 2000 were identified. From this sample, 59,874 discharges (4.3 percent) were excluded where the discharge was coded under a non-SSTP DRG (primarily DRG 471–bilateral JR). An additional 160,512 discharges were excluded where the indication for surgery was either clearly not elective or where the elective nature of the surgery was from the coded diagnoses unclear (includes a majority of revisions). Sensitivity analyses with and without the above patients did not reveal meaningful differences. For the multivariate LOS analyses, 98 percent of the cases had complete covariate data, leaving a final multivariate analytic sample of 1,121,494 patients. An additional 38 patients who died before discharge were excluded for the early discharge to PAC analysis.
Among the JR patients, the median patient age was 73 years. Two-thirds of the patients were female, 91 percent Caucasian, 87 percent entitled to Medicare based on age. Only 9 percent of patients were simultaneously receiving state aid. Using the census median income for the matched zip code of residence for each JR patient, the mean of this proxy income was $42,830.
One-third of the JR patients underwent hip replacement, with 2 percent of all cases being revisions. The prevalence of medical comorbidities, as abstracted using the Charlson index, was very low. Nine percent of all cases were performed at private, for-profit hospitals, 10 percent at government-owned hospitals, and the remainder at private, not-for-profit hospitals.
Although most of the pre- versus post-SSTP differences across covariates were trivial in magnitude, the following were notable exceptions. A lower proportion of the cases came from either California or Nevada (the CMS San Francisco region) after implementation of the SSTP (10.4 versus 8.2 percent). This was not explained by either a differential change in county-level Medicare managed care market share or population aged ≥65). There were more Friday discharges (23.1 versus 20.3 percent) and fewer Tuesday discharges (12.8 versus 15.0 percent) under SSTP.
Sample Selection and Description (Hip Fracture Patients)
A total of 1,145,677 FX patients were identified. Of these patients, 96 percent of patients were covered under one of the three SSTP DRG codes (209, 210, 211). There was a small shift in the proportion of patients discharged under DRG 210 hip and femur procedure (with complications or comorbidities) to DRG 211 (without complications or comorbidities). However, this shift was gradual across the years and not correlated with implementation of the SSTP. There were complete data on 97 percent of patients and therefore 1,071,010 patients available for the multivariate LOS analysis. The 366 patients who died in the hospital were excluded from analysis for the probability of early discharge multivariate analysis.
As expected given the burden of osteoporosis, FX patients were more likely to be female (76 percent), older (83 median years of age), and more likely caucasian than JR patients. FX patients were less likely to have disability as an entitlement for Medicare. Using the census median income for the matched zip code of residence for each FX patient, the mean of this proxy income was $38,841. FX patients were twice as likely as JR patients to be receiving state aid (18 versus 9 percent). FX patients had a higher prevalence of medical comorbidities with notably higher cardiovascular and cerebrovascular disease, as well as higher prevalence of dementia and psychoses. However, there were no notable differences in covariates before or after implementation of the SSTP with the exception again of lower prevalence of cases in the San Francisco region after the SSTP.
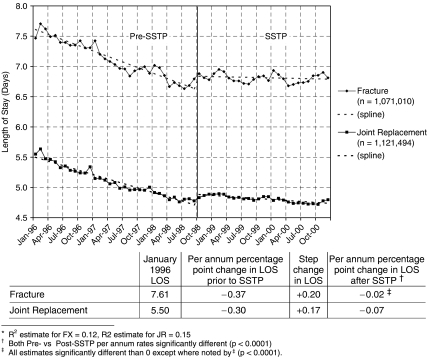
Change in LOS
For each of these two clinical conditions, the historical trend of ever-shortening hospital LOS continues through September 1998, at which time the SSTP was implemented. Thereafter, for each condition, there is a small step increase in mean LOS and then stabilization (see Figure 2). For JR patients, the adjusted mean LOS fell from 5.5 in January 1996 to 4.7 in September 1998 (a mean decline of 0.3 days per annum, p<.0001). After implementation of the SSTP policy, there was a small step increase in LOS to 4.9 days. Thereafter, LOS was essentially stable, declining less than 0.1 days per annum (p<.0001). Both the step change between policy periods and the change in slope between policy periods (pre-SSTP versus post-SSTP) were significant (p<.0001).
Figure 2.
Length of Stay after Elective Joint Replacement Surgery and Surgical Management of Hip Fracture (Multivariate Results*)
For FX patients, the adjusted mean LOS fell from 7.6 in January 1996 to 6.6 in September 1998 (mean decline of 0.4 days per annum, p<.0001). After implementation of the SSTP policy, LOS increased to 6.8 days (p<.0001). Thereafter, LOS was essentially stable (post-SSTP change in LOS not statistically different from 0). The difference between the pre-SSTP versus post-SSTP slope change was significant, as was the step change between periods (p<.0001 for both comparisons).
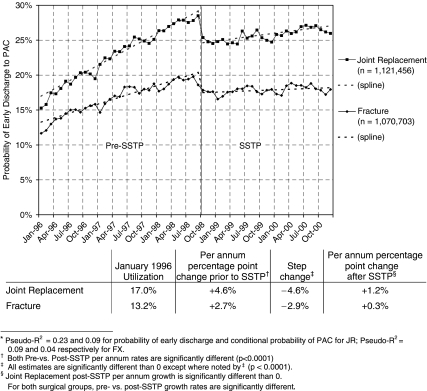
Change in “Early” Discharge to PAC
As Figure 3 indicates, there had been a steady increase in early discharge to PAC between January 1996 and September 1998. The larger proportion and more rapid growth in “early” PAC for JR patients was due to a more robust growth in “early” discharge (see Table 1) and likely attributable to the notable clinical differences between the groups.
Figure 3.
Proportion of Patients Discharged “Early” to Postacute Care Utilization after Elective Joint Replacement Surgery and Surgical Management of Hip Fracture (Multivariate Results*)
Table 1.
Probability of Discharge Disposition by Time of Discharge and Destination (Multivariate Results)
| Per Annum Percentage Point Change before SSTP (%) | Step Percentage Point Change between Periods (%) | Per Annum Percentage Point Change after SSTP* (%) | Adjusted Probability of Utilization by Calendar Month (%) | ||||
|---|---|---|---|---|---|---|---|
| 1/96 | 9/98 | 10/98 | 12/00 | ||||
| Joint replacement | |||||||
| Early discharge | +5.2 | −4.9 | +1.2 | 20.7 | 34.6 | 29.7 | 32.7 |
| PAC utilization | +1.2 | −1.0 | +0.8 | 77.1 | 80.2 | 79.2 | 80.9 |
| Early discharge with PAC | +4.6 | −4.6 | +1.2 | 17.0 | 28.8 | 24.6 | 27.1 |
| Early discharge without PAC | +0.6 | −0.3† | +0.3 | 3.8 | 5.4 | 5.1 | 5.6 |
| Late discharge with PAC | −3.4 | +3.6 | −0.4† | 60.1 | 51.0 | 54.6 | 53.8 |
| Late discharge without PAC | −1.8 | +1.3 | −1.1 | 19.1 | 14.4 | 15.7 | 13.5 |
| Hip fracture | |||||||
| Early discharge | +2.8 | −3.3 | +0.0† | 17.0 | 24.6 | 21.3 | 21.4 |
| PAC utilization | +1.0 | +0.2† | +1.1 | 82.7 | 85.2 | 85.4 | 87.7 |
| Early discharge with PAC | +2.7 | −2.9 | +0.3 | 13.2 | 20.4 | 17.5 | 18.2 |
| Early discharge without PAC | +0.2 | −0.4 | −0.3 | 3.8 | 4.2 | 3.8 | 3.2 |
| Late discharge with PAC | −1.7 | +3.1 | +0.7 | 69.4 | 64.8 | 68.0 | 69.5 |
| Late discharge without PAC | −1.1 | +0.2† | −0.8 | 13.6 | 10.6 | 10.8 | 9.2 |
Each 1% change represents roughly 2,000 patients.
All pre-SSTP versus post-SSTP comparisons are significantly different bootstrap estimations.
All estimates are significantly different than 0 except where noted by dagger.
SSTP, Short Stay Transfer Policy; PAC, postacute care.
Among JR patients, utilization of “early” PAC increased from 17 to 29 percent of all discharges (pre-SSTP growth of 4.6 percentage points per year). Immediately after implementation of the SSTP, the proportion of early discharges to PAC fell to 25 percent (significant change as evaluated by bootstrap estimation). Thereafter, post-SSTP growth in early discharge to PAC was only 1.2 percentage points/year (significantly lower than the pre-SSTP rate).
For FX patients, the proportion of patients discharged early to PAC increased from 13 to 20 percent (pre-SSTP growth of 2.7 percentage points per year) before falling back down to 17 percent immediately after the SSTP (growth rate and step change both significant). Thereafter, growth of early discharge to PAC was essentially flat at 0.3 percent per year (significantly different than pre-SSTP growth).
Reduction in early discharge to PAC was brought about primarily through a change in timing of discharge rather than change in PAC utilization (see Table 1). Probability of early discharge was reduced by 4.9 and 3.3 percentage points while utilization of PAC was changed by −1.0 and +0.2 percentage points respectively for JR and FX surgeries.
Among JR patients, to offset the 4.6 percentage points of patients no longer discharged early to PAC, there was a 3.6 percentage point increase in the proportion of patients discharged late with PAC. There was a smaller (1.3 percentage point) increase in proportion of patients discharged late without PAC. All step changes were similar in magnitude to the pre-SSTP per annum percentage point changes.
To offset the 2.9 percentage points of FX patients no longer discharged early to PAC, there was a 3.1 percentage point increase in the proportion of patients discharged late with PAC. There was little change in the other alternate responses.
Differential Treatment
There were no differential changes in LOS or early discharge with PAC for patients with more medical comorbidities or greater age. Nor were results affected by sensitivity analyses with patients undergoing bilateral JR (non-SSTP DRG 471) or with patients whose elective nature of JR was unclear (many revision JR cases). Nor did we observe a strategy to avoid the SSTP discount by delaying home health care until after the third day after discharge.
Before implementation of the SSTP, there was significant regional variation in LOS and utilization of early PAC (see Tables 2a and 2b). For example, in September 1998, the CMS Kansas City region (KS, NE, IA, and MO) had shorter adjusted mean LOS prior to SSTP (4.4 and 5.9 days for JR and FX patients, respectively) and corresponding higher rates of early discharge to PAC (32.7 percent of JR and 23.0 percent of FX patients). In contrast, in the New York region (NY and NJ) had the longest adjusted mean LOS (5.9 and 9.6 days for JR and FX, respectively) and lowest utilization of early discharge to PAC (18.1 percent of JR and 8.0 percent of FX patients).
Table 2a.
Regional Length of Stay and Probability of Early Discharge to Postacute Care for Patients Undergoing Elective Joint Replacement Surgery
| Length of Stay | Probability of Early Discharge to Postacute Care | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Per Annum Change in Mean LOS before SSTP | Step Change Between periods | Per Annum Change in Mean LOS after SSTP | Adjusted Length of Stay by Calendar Month | Per Annum Percentage Point Change before SSTP (%) | Step Change Between Periods (%) | Per Annum Percentage Point Change after SSTP (%) | Adjusted Probability of Utilization by Calendar Month (%) | |||||||
| 1/96 | 9/98 | 10/98 | 12/00 | 1/96 | 9/98 | 10/98 | 12/00 | |||||||
| National | −0.30 | +0.17 | −0.07 | 5.5 | 4.7 | 4.8 | 4.7 | +4.6 | −4.6 | +1.2 | 17.0 | 29.2 | 24.6 | 27.1 |
| CMS region | ||||||||||||||
| Boston | −0.34* | +0.11 | −0.06 | 5.3* | 4.4* | 4.5* | 4.4* | +6.5* | −2.9* | +2.0 | 13.0 | 30.4 | 27.4* | 31.8 |
| New York | −0.56* | +0.09 | −0.19* | 7.3* | 5.9* | 5.9* | 5.5* | +4.1* | −1.4* | +3.2 | 7.2* | 18.1* | 16.8* | 24.0* |
| Philadelphia | −0.33* | +0.25* | −0.15* | 5.2* | 4.4* | 4.6* | 4.3* | +5.6 | −3.3* | +4.1* | 17.9* | 32.9* | 29.6* | 38.7* |
| Atlanta | −0.34* | +0.18 | −0.07 | 5.6* | 4.7 | 4.8 | 4.7 | +5.3 | −4.4 | +0.7 | 16.5 | 30.5* | 26.2* | 27.8* |
| Chicago | −0.29 | +0.16 | −0.04 | 5.2* | 4.4* | 4.6* | 4.5* | +4.9 | −5.1 | +1.1 | 14.1* | 27.2* | 22.1* | 24.5* |
| Dallas | −0.25* | +0.16 | −0.07 | 5.3* | 4.7 | 4.8 | 4.7 | +3.9 | −4.5 | 0.0 | 21.9* | 32.4* | 27.9* | 27.8 |
| Kansas City | −0.27 | +0.30* | −0.03 | 5.2* | 4.4* | 4.7* | 4.7 | +4.3 | −10.4* | +0.1* | 21.3* | 32.7* | 22.3* | 22.6* |
| Denver | −0.17* | +0.18 | −0.01* | 4.7* | 4.3* | 4.5* | 4.4* | +2.8* | −6.3* | +0.7 | 24.7* | 32.3* | 26.0* | 27.7 |
| San Francisco | −0.13* | +0.18 | 0.00* | 4.9* | 4.5* | 4.7* | 4.7 | +2.9* | −3.0 | +0.4 | 20.9* | 28.7 | 25.6* | 26.6 |
| Seattle | −0.18* | +0.00* | 0.00* | 4.9* | 4.4* | 4.4* | 4.4* | +2.5* | 0.0* | +0.2 | 11.3* | 18.0* | 18.1* | 18.5* |
Regional estimate significantly different than national estimate.
SSTP, Short Stay Transfer Policy; LOS, length of stay; CMS, Centers for Medicare and Medicaid Services.
Table 2b.
Regional Length of Stay and Probability of Early Discharge to Postacute Care for Patients Undergoing Surgical Repair of HIP Fracture
| Length of Stay | Probability of Early Discharge to Postacute Care | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Per Annum Change in Mean LOS before SSTP | Step Change between Periods | Per Annum Change in Mean LOS after SSTP | Adjusted Length of Stay by Calendar Month | Per Annum Percentage Point Change before SSTP (%) | Step Change between Periods (%) | Per Annum Percentage Point Change after SSTP (%) | Adjusted Probability of Utilization by Calendar Month (%) | |||||||
| 1/96 | 9/98 | 10/98 | 12/00 | 1/96 | 9/98 | 10/98 | 12/00 | |||||||
| National | −0.37 | +0.20 | −0.02 | 7.6 | 6.6 | 6.8 | 6.8 | +2.7 | −2.9 | +0.3 | 13.2 | 20.4 | 17.5 | 18.2 |
| CMS region | ||||||||||||||
| Boston | −0.49* | +0.21 | −0.03 | 7.1* | 5.8* | 6.0* | 6.0* | +3.8* | −1.3 | +0.4 | 12.9 | 23.2* | 21.9* | 22.8* |
| New York | −0.93* | −0.16* | −0.30* | 12.1* | 9.6* | 9.5* | 8.9* | +1.7* | −0.1* | +0.4 | 3.3* | 8.0* | 7.8* | 8.7* |
| Philadelphia | −0.47* | +0.22 | −0.03 | 7.9* | 6.6 | 6.8 | 6.8 | +3.2 | −2.1 | +1.1 | 10.6* | 19.3* | 17.2 | 19.6 |
| Atlanta | −0.37 | +0.26 | −0.02 | 7.5 | 6.5 | 6.8 | 6.8 | +2.8 | −3.2 | +0.6 | 12.2* | 20.0 | 16.9* | 18.2* |
| Chicago | −0.32* | +0.24 | 0.00 | 7.0* | 6.1* | 6.4* | 6.4* | +3.1 | −3.5 | +0.6 | 12.3* | 20.8 | 17.4 | 18.7 |
| Dallas | −0.24* | +0.27 | +0.01 | 6.9* | 6.2* | 6.5* | 6.5* | +2.2* | −3.7 | −0.4* | 15.6 | 21.7* | 18.0 | 17.0* |
| Kansa City | −0.24* | +0.28 | +0.06 | 6.5* | 5.9* | 6.1* | 6.3* | +3.0 | −5.0* | −0.9* | 14.7* | 23.0* | 18.0 | 16.0* |
| Denver | −0.14* | +0.27 | +0.02 | 5.8* | 5.4* | 5.7* | 5.8* | +2.2 | −6.9* | +0.6 | 22.5* | 28.5* | 21.6* | 22.9* |
| San Francisco | −0.09* | +0.26 | +0.12* | 6.2* | 5.9* | 6.2* | 6.4* | +1.3* | −1.9 | −0.1 | 21.1* | 24.8* | 22.9* | 22.6* |
| Seattle | −0.16* | +0.15 | +0.05 | 5.8* | 5.4* | 5.5* | 5.6* | +2.7 | −1.7 | +0.0 | 19.3* | 26.8* | 25.1* | 25.1* |
Regional estimate significantly different than national estimate.
SSTP, Short Stay Transfer Policy; LOS, length of stay; CMS, Centers for Medicare and Medicaid Services.
Not surprisingly, hospitals in the Kansas City region responded with much larger increases in LOS (+0.30 and +0.28 days for JR and FX) and greater reductions in utilization of early PAC (−10.4 and −5.0 percentage points). In contrast, in the New York region there was little or no increase in mean LOS (+0.09 and −0.16 days) and negligible reductions in early discharge to PAC utilization (−1.4 and −0.1 percentage points).
DISCUSSION
The SSTP effectively changed hospital discharge practice patterns. After implementation of the policy, there was an immediate increase in hospital LOS, followed by a stabilization of the LOS. Utilization of early discharge to PAC underwent a step reduction followed by stabilization.
While eliminating the incentive to discharge patients early to PAC, hospitals responded simply by keeping patients in hospital longer rather than significantly altering PAC use. A strategy to avoid the SSTP discount by withholding PAC from patients discharged early was not observed. However, nor did we observe a substitution of longer LOS for PAC utilization (a stated goal of the SSTP policy; Health Care Financing Administration 1998).
Transfers to PAC with longer LOS (e.g., New York region, home health patients) were partly shielded from this policy and continued to experience further shortening in LOS. As a result, this policy should help eliminate some of the historical regional variation in LOS.
While we observed variation in response based upon region and discharge disposition, this was not observed for clinical covariates associated with longer LOS. Hospitals did not differentially discharge sicker or older patients after implementation of the policy. Nor did we observe delay of home health care beyond 3 days after discharge to avoid the SSTP penalty. While the discounted payments offer short-term savings to Medicare, the long-term fiscal implications to Medicare will require further study as these findings suggest that there is little reduction in PAC but increased use of acute care services. Furthermore, as mean LOS continues to fall, albeit at a slower rate, more transfers will fall/under the SSTP discount until a time when the national geometric mean LOS falls across a day threshold (e.g., 4.1–3.9). At this point the definition of “early” will be shortened, reducing the number of patients covered under the SSTP. This will reduce and redistribute the fiscal impact of the SSTP (e.g., relieving pressure from regions with higher proportion of early PAC).
These results should be interpreted with some caution. Under the Balanced Budget Act of 1997, several other PAC policies were simultaneously initiated (skilled nursing facility transition to prospective payment, home health interim payment system reductions, etc.). The observed reductions in utilization of early discharge to PAC are likely not attributable to other Medicare policy changes for the following reasons. As noted above, there was little change in overall PAC utilization. Other authors have described reductions in home health care during the same study years (McCall et al. 2001). In analyses not shown, we were able to separately examine changes in the components of PAC (home health, skilled nursing, and rehabilitation). While there was reduction in probability of home health care, this reduction preceded the reduction in early PAC utilization reported here. Furthermore, reductions in home health care were offset by increases in other PAC venues. No other Medicare policy implementation dates coincided with the SSTP date with the exception of a relaxation in the Home Health Interim Payment System reimbursement cuts (Committee on Ways and Means 1999). It is unlikely this relaxation in cuts biased the observed results as there was no change in early use of PAC associated with the implementation of the parent Interim Payment Policy implementation date, October 1, 1997. Finally, changes to home health reimbursement were phased in whereas the change in early PAC utilization reported here was sharp.
Time series analyses are always limited by potential bias from secular trends. However, the magnitude of the month-to-month change in utilization correlating with policy implementation makes this threat less likely. It would have been ideal to have a comparator group with similar pre-SSTP early PAC growth and utilization. However, as this was Medicare's selection criteria for the DRGs covered under the SSTP, similar DRGs would have been included under the policy as well.
Given practical limitations, we faced the choice of studying a few DRGs in depth (100 percent sampling, permitting us to study month-to-month changes) versus studying more DRGs in less detail (e.g., 5 percent sampling, which would only support analyses of annual rather than monthly changes). As MEDPAC had already performed analyses based on the latter strategy, we opted to focus in detail on the most prevalent DRGs susceptible to the SSTP, to better correlate the change in practice pattern with SSTP implementation.
The interpretations of these results are further constrained by the limits of administrative datasets. The socioeconomic status of Medicare beneficiaries is limited by the acceptability of using the median income all residents in the zip codes as a proxy. The density of PAC supply markets is complex to calculate. Using hospital zip code has inherent limitations, e.g., some hospitals have their own zip code. However, this affected only a small proportion of hospitals and measurement error in the supply and population density variables is unlikely to cause significant bias as they are not correlated with the time trends that are the main focus of interest in our analysis.
CONCLUSIONS
The SSTP better aligned hospital marginal revenues and marginal costs, implementing penalties for early transfer to PAC thereby counterbalancing the strong financial pressure to discharge patients early to PAC. Hospitals responded by keeping patients in hospital longer without significant change PAC use. In aggregate, we did not observe withholding of PAC from patients. However, nor did we observe a change in care that suggested elimination of potentially unnecessary PAC (a CMS secondary objective). Certain groups of patients with longer mean LOS were shielded from the effects of this program (regions with long LOS and patients first discharged to HH). These factors permitted LOS to continue to fall varying with exposure to the policy. Continued fall in LOS will expose further discharges to the policy until a point where the geometric mean LOS value falls across a whole integer value. At that point, the portion of transfers that would have been exposed to the policy will no longer be penalized thereby ameliorating and redistributing the impact of the policy.
Acknowledgments
Drs. FitzGerald and Boscardin are supported by the Agency for Healthcare Research and Quality, Mentored Scientist Development Award (K08 HS13168). Drs. FitzGerald and Ettner are supported by the Arthritis Foundation, Arthritis Investigator Award. Dr. FitzGerald is also supported by the UCLA, Specialty Training and Advanced Research Program.
The authors would like to acknowledge Rachel Louie for her assistance in preparing the analytical files and Drs. Thomas Rice, Gerald Kominski, and Carol Mangione for their thoughtful review of the manuscript. The authors would also like to acknowledge, Research Data Assistance Center (ResDAC), located at the University of Minnesota, for their help facilitating work with the Centers for Medicare and Medicaid Services and answering questions regarding the data. ResDAC is funded by CMS contract 500-01-0043.
Disclosures: None.
Disclaimers: None.
REFERENCES
- Centers for Medicare and Medicaid Services. 1999 Medicare Managed Care Market Penetration for All Medicare Plan Contractors—Quarterly State/County Data Files.” Available at http://www.cms.hhs.gov/healthplans/statistics/mpsct/default.asp? Centers for Medicare & Medicaid Services.
- Centers for Medicare and Medicaid Statistics. Medicare Provider Analysis and Review (MEDPAR) of Short-Stay Hospitals: 2002 DRG Description. 2004.
- Chassin MR, Brook RH, Park RE, Keesey J, Fink A, Kosecoff J, Kahn K, Merrick N, Solomon DH. Variations in the Use of Medical and Surgical Services by the Medicare Population. New England Journal of Medicine. 1986;314:285–90. doi: 10.1056/NEJM198601303140505. [DOI] [PubMed] [Google Scholar]
- Chassin MR, Kosecoff J, Park RE, Winslow CM, Kahn KL, Merrick NJ, Keesey J, Fink A, Solomon DH, Brook RH. Does Inappropriate Use Explain Geographic Variations in the Use of Health Care Services? A Study of Three Procedures [see Comments] Journal of the American Medical Association. 1987;258:2533–7. [PubMed] [Google Scholar]
- Committee on Ways and Means. Medicare Balanced Budget Refinement Act of 1999. 1999;(Part 1):32–150. Report 106–436. [Google Scholar]
- Cromwell J, Donoghue S, Gilman BH. Expansion of Medicare's Definition of Post-Acute Care Transfers. Health Care Finance Review. 2002;24:95–113. [PMC free article] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Comorbidity Index for use with ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Duan N, Manning W, Morris C, Newhouse J. A Comparison of Alternative Models for the Demand for Medical Care. Journal of Business and Economic Statistics. 1983;1:115–26. [Google Scholar]
- Econometric Software, Inc. LIMDEP Version 7.0 User's Manual. Bellport, NY: Econometric Software Inc.; 1995. Nested Logit Models; pp. 511–60. [Google Scholar]
- Efron B. An Introduction to the Bootstrap. New York: Chapman & Hall; 1993. [Google Scholar]
- Forrest GP, Roque JM, Dawodu ST. Decreasing Length of Stay after Total Joint Arthroplasty. Effect on Referrals to Rehabilitation Units, Archives of Physical Medicine and Rehabilitation. 1999;80:192–4. doi: 10.1016/s0003-9993(99)90120-x. [DOI] [PubMed] [Google Scholar]
- Green WH. Models with Discrete Dependent Variables. In: Boyd J, editor. Econometric Analysis. Upper Saddle River, NJ: Prentice Hall; 1999. pp. 118–195. Chapter 19. [Google Scholar]
- Health Care Financing Administration. Medicare Program: Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 1999 Rates; Final Rule. 1998:40953–47163. Federal Register 42(CFR Parts 405, 412, and 413) [Google Scholar]
- Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of Cost Reduction Programs on Short-Term Patient Outcome and Hospital Cost of Total Knee Arthroplasty. Journal of Bone Joint Surgery Am JID—0014030. 2002;84-A:348–53. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- Huusko T, Karppi P, Avikainen V, Kautiainen H, Sulkava R. Significant Changes in the Surgical Methods and Length of Hospital Stay of Hip Fracture Patients Occurring over 10 years in Central Finland. Annales chirurgiae et gynaecologie. 1999;88:55–60. [PubMed] [Google Scholar]
- Intrator O, Berg K. Benefits of Home Health Care after Inpatient Rehabilitation for Hip Fracture. Health Service Use by Medicare Beneficiaries, 1987–1992, Archives of Physical Medicine and Rehabilitation. 1998;79:1195–9. doi: 10.1016/s0003-9993(98)90261-1. [DOI] [PubMed] [Google Scholar]
- Kane RL, Chen Q, Blewett LA, Sangl J. Do Rehabilitative Nursing Homes Improve the Outcomes of Care? Journal of American Geriatric Society. 1996;44:545–54. doi: 10.1111/j.1532-5415.1996.tb01440.x. [DOI] [PubMed] [Google Scholar]
- Kenney G, Holahan J. Nursing Home Transfers and Mean Length of Stay in the Prospective Payment Era. Medical Care. 1991;29:589–609. doi: 10.1097/00005650-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Manton KG, Woodbury MA, Vertrees JC, Stallard E. Use of Medicare Services before and after Introduction of the Prospective Payment System. Health Services Research. 1993;28:269–92. [PMC free article] [PubMed] [Google Scholar]
- Marsch CL, Cormier DR. Spline Regression Models. Thousand Oaks, CA: Sage Publications Inc.; 2001. [Google Scholar]
- Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between Length of Stay and Manipulation Rate after Total Knee Arthroplasty. Journal of Arthroplasty. 1998;13:896–900. doi: 10.1016/s0883-5403(98)90196-6. [DOI] [PubMed] [Google Scholar]
- McCall N, Komisar HL, Petersons A, Moore S. Medicare Home Health before and after the BBA. Health Affairs. 2001;20:189–98. doi: 10.1377/hlthaff.20.3.189. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. 1999. pp. 1–98.
- MEDPAC: Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. 2000.
- Metz CM, Freiberg AA. An International Comparative Study of Total Hip Arthroplasty Cost and Practice Patterns. Journal of Arthroplasty. 1998;13:296–8. doi: 10.1016/s0883-5403(98)90175-9. [DOI] [PubMed] [Google Scholar]
- Meyers SJ, Reuben JD, Cox DD, Watson M. Inpatient Cost of Primary Total Joint Arthroplasty. Journal of Arthroplasty. 1996;11:281–5. doi: 10.1016/s0883-5403(96)80079-9. [DOI] [PubMed] [Google Scholar]
- Mooney C, Duval R. Bootstrapping: A Nonparametric Approach to Statistical Inference. In: Lewis-Beck M, editor. Quantitative Applications in Social Science. Vol. 95. Newbury Park, CA: Sage University Press; [Google Scholar]
- Munin MC, Rudy TE, Glynn NW, Crossett LS, Rubash HE. Early Inpatient Rehabilitation after Elective Hip and Knee Arthroplasty [see Comments] Journal of the American Medical Association. 1998;279:847–52. doi: 10.1001/jama.279.11.847. [DOI] [PubMed] [Google Scholar]
- One-Hundred-Fifth Congress of the United States of America. Balanced Budget Act of 1997. 1997. H.R. 2015-147, 4401-11723.
- Prospective Payment Assessment Commission. Washington, DC: 1996. Report and Recommendations to the Congress. [Google Scholar]
- Prospective Payment Assessment Commission. Washington, DC: 1997. Report and Recommendations to the Congress. [Google Scholar]
- SAS Institute. SAS Software Version 8.2. [8.2] Cary, NC: The SAS Institute; 2000. [Google Scholar]
- STATA. Stata. [Intercooled 7.0 for Windows 98/95/NT] College Station, TX: Stata Corporation; 2002. [Google Scholar]