Abstract
Objective
The purpose of this study is to determine whether patient activation is a changing or changeable characteristic and to assess whether changes in activation also are accompanied by changes in health behavior.
Study Methods
To obtain variability in activation and self-management behavior, a controlled trial with chronic disease patients randomized into either intervention or control conditions was employed. In addition, changes in activation that occurred in the total sample were also examined for the study period. Using Mplus growth models, activation latent growth classes were identified and used in the analysis to predict changes in health behaviors and health outcomes.
Data Sources
Survey data from the 479 participants were collected at baseline, 6 weeks, and 6 months.
Principal Findings
Positive change in activation is related to positive change in a variety of self-management behaviors. This is true even when the behavior in question is not being performed at baseline. When the behavior is already being performed at baseline, an increase in activation is related to maintaining a relatively high level of the behavior over time. The impact of the intervention, however, was less clear, as the increase in activation in the intervention group was matched by nearly equal increases in the control group.
Conclusions
Results suggest that if activation is increased, a variety of improved behaviors will follow. The question still remains, however, as to what interventions will improve activation.
Keywords: Self-care methods, self-care statistics and numerical data, self-care trends, patient participation, patient engagement, patient activation, health coaching
The Patient Activation Measure (PAM), which assesses patient knowledge, skill, and confidence for self-management, was developed using qualitative methods, Rasch analysis, and classical test theory psychometric methods. The resulting measure is a unidimensional, interval-level, Guttman-like scale. The research to date has found the PAM to have strong psychometric properties, including content, construct, and criterion validity. These initial findings indicate the PAM predicts a range of behaviors, including: healthy behaviors (e.g., exercise, diet); disease-specific self-management behaviors; and consumeristic type behaviors (e.g., reading about risks with a new drug); (Hibbard et al. 2004, 2005).
Because patient self-management is so critical to health outcomes, measuring activation and using the information to improve processes that support patient self-management could be an important key to improving outcomes of care. However, to be a useful tool for improvement, it must be demonstrated that activation is something that can change, and once changed, that behaviors will also change in the same direction.
Thus, the purpose of this study is to determine if activation is mutable and to examine whether changes in activation scores predict changes in actual health behaviors.
BACKGROUND
The chronic illness care model emphasizes patient-oriented care, with patients and their families integrated as members of the care team (Von Korff 1997). Thus, a critical element needed for the successful implementation of the model is a knowledgeable and activated patient as a collaborative partner in managing their health. Activated patients who are prepared to take on this key role in their care are central to achieving improvements in the quality of care, and ultimately, better health outcomes and less costly health care service utilization.
While patient activation is a central concept in the chronic illness care model, it is also the least well-developed element. The inability to measure activation has been a limiting factor in the development of this crucial aspect in the model. As with other areas of health care quality, measurement capability is a necessary precondition to improvement.
The evidence to date suggests that there are four stages (based on PAM scores) that people go through in the process of becoming fully competent managers of their own health (Hibbard et al. 2005).
At stage 1, people do not yet grasp that they must play an active role in their own health, they may still believe that they can just be a passive recipient of care. Example items from stage 1: [“When all is said and done, I am the person who is responsible for managing my health condition” and “Taking an active role in my own health care is the most important factor in determining my health and ability to function.”] (12 percent of a national sample ages 45+).
At stage 2, people may lack the basic facts or have not connected the facts into a larger understanding about their health or recommended health regimens. Example items: [“I know the different medical treatment options available for my health condition” and “I know what each of my prescribed medications does.”] (29 percent of a national sample ages 45+).
At stage 3, people have the key facts and are beginning to take action but may lack confidence and skill to support new behaviors. Example item: [“I know how to prevent further problems with my health condition.” And, “I have been able to maintain the lifestyle changes for my health that I have made.”] (37 percent of a national sample ages 45+).
At stage 4, people have adopted new behaviors but may not be able to maintain them in the face of life stress or health crises. Example items: [“I am confident I can figure out solutions when new situations or problems arise with my health condition” and “I am confident that I can maintain lifestyle changes, like diet and exercise, even during times of stress.”] (22 percent of a national sample ages 45+).
These stages of activation provide insight into possible strategies for supporting activation among patients at different points along the continuum.
The apparent developmental nature of activation, suggests that strategies for increasing activation can be tailored to the stage of activation of an individual patient. The measure has the potential of providing a guide to economical interventions targeted to a patient's needs by precisely identifying their stage of activation with a brief questionnaire. Clinicians able to effectively support activation in their patients, and take fuller advantage of the patient as a key team member, could potentially deliver more effective and efficient care (delivering outcomes for less costs). Also, because of its strong psychometric properties, the measure can be used to evaluate interventions designed to encourage consumer and patient activation, and provide feedback to clinicians on how well their efforts at supporting patient self-management are paying off.
Ultimately, the utility of the PAM depends not only on the precision of the measure but also on the mutability of activation. This study assesses the mutability of activation, as it is measured by PAM, and its power in predicting health behaviors over time.
METHODS
The primary research questions are whether activation is changeable and whether changes in activation result in changes in behavior. To obtain the necessary variability in both activation and self-management behaviors over a relatively short period of time, an intervention is required that has a relatively high probability of creating improvement in actual self-management behavior.
Therefore, the Chronic Disease Self-Management Program (CDSMP) is used as the intervention. Studies evaluating the impact of the CDSMP (Lorig, Sobel, Stewart et al. 1999; Lorig, Sobel, Ritter et al. 2001) indicate that while improved self-management behaviors are not universal among course participants, the intervention is sufficiently successful to generate the variability in self-management behavior. We thus employ the CDSMP intervention for the purpose of creating change and variability in self-management in the study sample. The purpose is not to evaluate the efficacy of the CDSMP.
Research Design
The research design employs a randomized clinical trial with participants randomly assigned into either intervention, a CDSMP or control condition (no intervention). Patients were recruited from PeaceHealth Medical Group in Lane County, Oregon, using the following eligibility criteria: must have at least one of the specified chronic conditions (diabetes, arthritis, hypertension, heart disease, chronic obstructive pulmonary disease, or hyperlipidemia); must be 50–70 years old; and must not be participating in any other of the intervention studies at PeaceHealth.
The Intervention
The CDSMP is a workshop given once a week, for two and a half hours, over 6 weeks, in community settings. People with different chronic health problems attend together. Two trained leaders facilitate the workshops, one or both of whom are nonhealth professionals. Session topics include: (1) techniques to deal with problems such as frustration, fatigue, pain, and isolation, (2) appropriate exercise for maintaining and improving strength, flexibility, and endurance, (3) appropriate use of medications, (4) communicating effectively with family, friends, and health professionals, (5) nutrition, and (6) how to evaluate new treatments. Classes are highly participative, where mutual support and success build the participants' confidence in their ability to manage their health and maintain active and fulfilling lives. Each participant in the workshop received a copy of the companion book, Living a Healthy Life with Chronic Conditions, 2d Edition, and an audio relaxation tape, Time for Healing. Participants randomized to control condition were offered the CDSMP course at the end of the study period.
Evaluating the Impact of the Intervention
Survey data were collected at baseline, at 6 weeks (at the end of the intervention), and at 6 months from both intervention and control participants. Intervention participants responded to the baseline and 6 weeks surveys using self-administered questionnaires. Telephone surveys were used for all 6 months data collection and for any intervention participants who failed to complete a self-administered questionnaire at baseline or at 6 weeks. Telephone surveys were used to collect data from the participants in the control condition at all three data collection points. A previous randomized trial assessing mode effects on responses to the PAM, showed no significant differences between self-administered and interviewer administered versions of the PAM (Speizer et al. 2006).
Sample
The recruitment process began with a list 8,796 people who were identified as possibly eligible to participate. Of those 540 were contacted and found to be not eligible. Another 1,442 were on the eligible list, but contact was never attempted. Two thousand one hundred twenty-eight people were called but contact was never completed. Another 3,951 were contacted but refused participation. Of the 735 who agreed to participate at the outset of the study, 256 were excluded because they never signed an informed consent, leaving a sample of 479 participants. Eighty-seven percent of the 479 participants completed all three surveys. Twenty-eight participants completed only the baseline survey and no follow-up surveys, and 34 participants completed the baseline, but only one of the two follow-up surveys, and 12 completed only the two follow-up surveys and no baseline survey.
Growth Model Analysis of Activation
In addition to evaluating the impact of the intervention on activation and subsequent behavioral and health outcomes, we also examine changes in activation that occur in the total sample. Within any sample there is likely to be a great deal of variability in both magnitude and direction of change over time. Unless the structure of that variability can be identified and taken into account in the analysis, it tends to simply add noise or error to any assessments of change over time. As the principle purpose of this study is to evaluate how change in activation is associated with change in health behavior, it is important to determine if there are groups of respondents exhibiting clearly different patterns of change in activation over time.
Using the Mplus growth models, activation latent growth classes were identified and used in the analysis to predict changes in health behaviors and health outcomes. The use of latent growth class models allows for the identification of groups of persons characterized by different growth trajectories in activation over time. In the current analysis we identify these different activation growth trajectories, assess how well they predict changes in behaviors, and examine the factors, including intervention or control group status, that are related to membership in the different growth classes.
Research Questions
Does activation change over time?
Does the intervention increase activation?
Are there different trajectories of change in activation (latent growth classes)?
Does the intervention predict activation growth class membership?
Do changes in activation predict changes in behavior?
What factors predict activation growth class membership?
Predictor and Outcome Measures
PAM: In this analysis we used the 13 item version of the PAM. The PAM is a unidimensional, interval-level, Guttman-like scale assessing patient knowledge, skill, and confidence for self-management (Hibbard et al. 2004, 2005).
Eighteen health related behaviors are included as outcome variables in the study. These behaviors fall into two major categories: self-management behaviors and disease-specific self-management behaviors.
Self-Management Behaviors include:
Engage in regular exercise.
Follow a low fat diet.
Read food labels for content.
Manage stress in a healthy way.
Know recommended weight.
Able to maintain recommended weight.
Ask about medication side effects when taking a new prescription.
Read about side effects when taking new prescription medication.
Disease Specific Self-Management Behaviors include:
Hypertension
Take blood pressure (BP) medications as recommended.
Know what BP physician would like me to have.
Check BP at least once a week.
Keep written diary of BP readings.
Arthritis
Have a personal plan to manage arthritis.
Exercise regularly to manage arthritis.
Diabetes
Test glucose at least three times a week.
Check feet for cracks and calluses.
Keep a written diary of glucose levels.
Take diabetes medications as recommended.
All the behavioral variables are statements with degrees of agreement. The items are coded from 1 to 4 with 1 representing “strongly disagree” and 4 representing “strongly agree.”
Other variables included in the analysis are a measure of health related quality of life (HRQoL), a measure of depression, and a measure of social desirability. The measure of social desirability was included to control for the possible biasing effect of respondents' desire to present themselves and their behaviors in a positive light.
HRQoL adapted from the SF8 and calibrated using Rasch Modeling (Mahoney and Stock 2000). The items included are:
How often were you limited in the kind of work or other activities you could do as a result of your physical health?
How often have you accomplished less than you would like as a result of any emotional problems, such as feeling depressed or anxious?
How often have you done work or other activities less carefully than usual as a result of any emotional problems, such as feeling depressed or anxious?
How much of the time during the past 4 weeks have you felt calm and peaceful?
How much of the time during the past 4 weeks did you have a lot of energy?
How much of the time during the past 4 weeks have you felt downhearted and depressed?
How often has your physical health or emotional problems interfered with your social activities, like visiting with friends or relatives?
How much did pain interfere with your normal work, including both work outside the home and housework? (Cronbach's α values are baseline, 0.897; 6 weeks, 0.891; 6 months, 0.887.)
And a Measure of Depression (Mahoney and Stock 2001):
I have felt full of energy.
I have worried a lot about the past.
I sometimes have felt that my life is empty.
I have dropped many of my activities and interests.
I often have felt downhearted and blue.
I have felt that my situation is hopeless.
I have felt pretty worthless.
I frequently have felt like crying.
I often have felt helpless.
I have enjoyed getting up in the morning and starting a new day.
I have found life very exciting. (Cronbach's α values are baseline, 0.933; 6 weeks, 0.925; 6 months, 0.938.)
The Short Marlowe–Crowne Social Desirability Scale (Strahan and Gerbasi 1972) includes:
I never hesitate to go out of my way to help someone in trouble.
I have never intensely disliked anyone.
There are times when I was quite jealous of the good fortune of others.
I would never think of letting someone else be punished for my wrong doings.
I sometimes feel resentful when I do not get my way.
There have been times when I felt like rebelling against people in authority even though I know they were right.
I am always courteous, even to people who are disagreeable.
When I do not know something, I do not at all mind admitting it.
I am sometimes irritated by people who ask favors of me.
I can remember playing sick to get out of something.
After items were all coded in the same direction, Rasch analysis was used to create linear scales from the depressions and quality of life variables. For the health variables a mean score was calculated. Measures were calculated for baseline, 6 weeks, and 6 months.
Demographic factors are also included as descriptive variables and as control variables in the multivariate analyses.
FINDINGS
Table 1 shows the characteristics of the intervention and control groups at baseline. The control group had significantly more married participants than the intervention group. Three behaviors are significantly different at baseline, regular exercise, managing stress, and attention to fat in the diet and were more likely to be performed by members of the control group. No other significant differences between the two groups were observed.
Table 1.
Baseline Characteristics by Intervention/Control Status
| Control (N = 235) | Intervention (N = 244) | ANOVA Values | |
|---|---|---|---|
| Average age (range 50–70) | 60.0 | 59.6 | F = 0.07, p = 0.80 |
| Gender (% female) | 69.6% | 69.0% | F = 0.45, p = 0.50 |
| Race (% white) | 95.6% | 97.5% | F = 0.34, p = 0.56 |
| Employment | 26.0% | 31.0% | F = 0.20, p = 0.66 |
| Marital status (% married) | 72.1% | 61.5% | F = 5.66 p = 0.02 |
| Number of chronic conditions | 2.8 | 2.9 | F = 0.70, p = 0.40 |
| Average patient activation score | 60.2 | 60.1 | F = 0.02, p = 0.90 |
| Diagnoses | |||
| Diabetes | 38.0% | 42.1% | F = 0.45, p = 0.51 |
| High blood pressure (BP) | 80.6% | 76.8% | F = 0.98, p = 0.32 |
| Lung disease | 30.9% | 26.7% | F = 1.01, p = 0.32 |
| High cholesterol | 66.7% | 66.0% | F = 0.03, p = 0.87 |
| Arthritis | 55.6% | 62.8% | F = 2.45, p = 0.12 |
| Heart disease | 26.5% | 30.1% | F = 0.74, p = 0.39 |
| Self-management behaviors (% agree strongly) | |||
| Exercise on regular basis | 25.2% | 16.0% | F = 6.00, p = 0.02 |
| Able to manage stress in healthy way | 25.1% | 17.0% | F = 4.61, p = 0.03 |
| Ask physician, pharmacist about medication side effects and how to avoid them | 35.6% | 40.2% | F = 1.00, p = 0.32 |
| Read about side effects when prescribed new medication | 39.0% | 40.0% | F = 0.02, p = 0.90 |
| Pay attention to amount of fat in diet | 31.1% | 18.9% | F = 9.28, p = 0.00 |
| Read food labels for content | 48.7% | 46.0% | F = 0.32, p = 0.57 |
| Know recommended weight | 30.9% | 27.5% | F = 0.64, p = 0.42 |
| Able to maintain recommended weight | 6.0% | 5.1% | F = 0.13, p = 0.72 |
| Disease specific self-management behaviors | |||
| Hypertension (n = 359) | |||
| Take BP medications as physician recommends | 72.5% | 72.7% | F = 0.00, p = 0.97 |
| Check BP at least once a week | 22.4% | 18.5% | F = 0.79, p = 0.37 |
| Keep written diary of BP readings | 14.5% | 9.6% | F = 2.03, p = 0.16 |
| Know what BP physician would like me to have | 35.6% | 34.1% | F = 0.09, p = 0.76 |
| Diabetes (n = 193) | |||
| Test glucose at least three times a week | 47.7% | 61.0% | F = 3.41, p = 0.07 |
| Check feet for cracks and calluses | 36.8% | 44.2% | F = 1.08 p = 0.30 |
| Keep written diary of glucose levels | 29.6% | 33.0% | F = 0.26, p = 0.61 |
| Take diabetes medications as physician recommends | 62.0% | 69.2% | F = 0.96, p = 0.33 |
| Arthritis (n = 273) | |||
| Have personal plan to manage arthritis | 10.8% | 12.9% | F = 0.27, p = 0.60 |
| Regular exercise to manage arthritis | 9.8% | 13.9% | F = 1.05, p = 0.31 |
Does Activation Change?
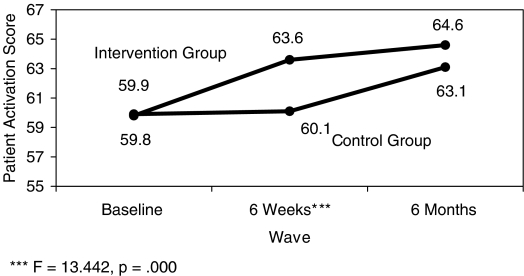
The findings indicate that activation levels increased over time. Using a repeated measures general linear model, and assessing the total study population, time was a statistically significant predictor of activation levels (F = 45.1, p < 0.001). An assessment of the impact of the intervention on activation levels was also conducted. Figure 1 shows changes in activation levels for the intervention and control groups. No difference in activation were observed at baseline, however, the intervention group increased activation scores significantly above those in the control group by 6 weeks (F = 13.44, p < 0.001). By 6 months differences in activation between intervention and control group members had declined, largely because the control group also gained in activation over the study period. Because both groups gained in activation, differences were no longer statistically significant by 6 months (F = 2.344, p = 0.127). The impact that the intervention had on changes in activation and changes in behavior are examined in more depth in the multivariate portion of the analysis (Table 3).
Figure 1.
Changes in Activation Scores by Intervention and Control Group, ***F = 13.442, p = 0.000
Table 3.
Repeated Measures General Linear Model, Self-Management Behavior Change over 6 Months (F-Values with Significance)
| Main Effects | Interactions | ||||||
|---|---|---|---|---|---|---|---|
| General Self-Management Behaviors | Growth Class | Intervention Group | Time | Growth Class × Time | Growth Class × Group | Group × Time | Class × Group × Time |
| Exercise on regular basis | 12.0*** | 2.1 | < 1.0 | 4.6* | < 1.0 | 9.2*** | < 1.0 |
| Able to manage stress in healthy way | 5.0* | < 1.0 | 1.1 | 4.0* | < 1.0 | 1.3 | < 1.0 |
| Ask physician or pharmacist about medication side effects and how to avoid them | 7.9** | 1.9 | 2.5† | < 1.0 | < 1.0 | < 1.0 | < 1.0 |
| Read about side effects when prescribed new medication | 10.8*** | 3.4† | 1.0 | < 1.0 | 2.8† | < 1.0 | < 1.0 |
| Pay attention to amount of fat in diet | 6.1* | < 1.0 | < 1.0 | 6.4** | 1.8 | < 1.0 | < 1.0 |
| Read food labels for content | 6.1* | < 1.0 | < 1.0 | < 1.0 | < 1.0 | < 1.0 | < 1.0 |
| Know recommended weight | 16.3*** | < 1.0 | < 1.0 | 2.8† | < 1.0 | 3.9* | < 1.0 |
| Able to maintain recommended weight | 3.4† | 4.6* | < 1.0 | 1.8 | 2.1 | 1.4 | < 1.0 |
| Disease Specific Self-Management Behaviors | |||||||
| Hypertension | |||||||
| Take BP medications as physician recommends | < 1.0 | < 1.0 | 3.3* | 2.5† | < 1.0 | < 1.0 | < 1.0 |
| Know what BP physician would like me to have | 1.9 | < 1.0 | < 1.0 | 2.7† | < 1.0 | 2.6† | 2.2 |
| Check BP at least once a week | 2.4 | 1.0 | 3.4* | 2.3 | < 1.0 | 3.6* | 4.2* |
| Keep written diary of BP readings | < 1.0 | 3.9* | < 1.0 | 4.2* | < 1.0 | < 1.0 | < 1.0 |
| Diabetes | |||||||
| Test glucose at least three times a week | < 1.0 | < 1.0 | < 1.0 | 2.5† | < 1.0 | < 1.0 | < 1.0 |
| Check feet for cracks and calluses | 3.5† | < 1.0 | < 1.0 | 1.9 | < 1.0 | 1.3 | 1.9 |
| Keep written diary of glucose levels | 3.8* | < 1.0 | < 1.0 | 8.2*** | < 1.0 | 1.1 | < 1.0 |
| Take diabetes medications as physician recommends | 12.0*** | 2.1 | < 1.0 | 4.6* | < 1.0 | 9.2*** | < 1.0 |
| Arthritis | |||||||
| Have personal plan to manage arthritis | 12.9*** | < 1.0 | < 1.0 | < 1.0 | < 1.0 | 2.3 | < 1.0 |
| Regular exercise to manage arthritis | 13.6*** | 2.2 | < 1.0 | 2.4 | < 1.0 | 2.7 | < 1.0 |
The model is growth class and group as fixed factors; age, HRQoL, social desirability, and depression as covariates.
p < 0.05.
p < 0.01.
p < 0.001.
p < 0.1.
BP, blood pressure; HRQoL, health related quality of life.
Are There Different Trajectories of Change in Activation?
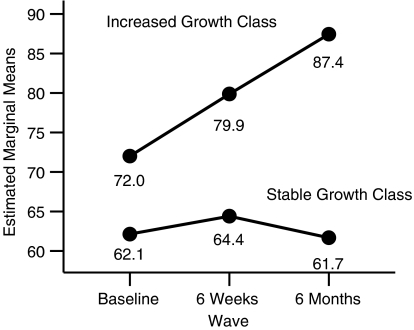
Mplus growth mixture model analysis with continuous latent class indicators (linear PAM-13 scores) was conducted to determine if useful activation growth classes could be identified. Four different growth class models were evaluated (the model fit indices are available on request). While the difference in fit of the four models was not large, the two class model was selected for use in this analysis on the pragmatic criteria of having a sufficient number of cases in the activation growth classes to conduct an analysis of how activation growth class membership is related to behavior change over time. These two growth classes are labeled stable or no change in activation and increased activation. Figure 2 shows the mean activation score of these two growth classes at each wave.
Figure 2.
Estimated Marginal Means of Activation by Wave by Activation Growth Class
In a repeated measures general linear model there was a significant wave by growth class interaction for activation (F = 47.71, p < 0.0001; Figure 2). Post hoc tests (95 percent CI) for the growth class effect indicated that in the increased growth class activation significantly increased at each wave while the stable growth class significantly increased from baseline to 6 weeks and significantly decreased from 6 weeks to 6 months. The “increased” class was significantly more activated at baseline than was the stable class by an observed difference of almost nine points. By 6 months, however, the difference was almost 26 points. It is informative that only about 10 percent of all respondents were in the “increased” activation growth class.
Does the Intervention Predict Activation Growth Class Membership?
Table 2 shows the cross tabulation of growth classes and intervention and control groups. The chances of being in the “increased” growth class do not significantly differ between the intervention and control groups (χ2 = 0.11, p = 0.80).
Table 2.
Activation Growth Classes by Intervention/Control and Groups
| Growth Class PAM Increased | Growth Class PAM Stable | Total | |
|---|---|---|---|
| Control group | 46.8% (22) | 49.3% (213) | 49.1% (235) |
| Intervention group | 53.2% (25) | 50.7% (219) | 50.9% (244) |
| Total | 100% (47) | 100% (432) | 100% (479) |
(χ2 = 0.11, p = 0.8).
PAM, Patient Activation Measure.
The effect of the intervention on membership in growth class was also examined using a multivariate approach. A repeated measures general linear model with activation growth class and intervention/control group status as fixed factors was examined. There was no significant within subjects group (intervention/control) effect on activation over time (F = 1.98, p = 0.139), and no significant growth class and group (intervention/control) interaction (F < 1).
Do Changes in Activation Predict Changes in Behavior?
In this portion of the analysis we assess both the impact of the intervention and membership in a growth class on self-management behavior change over time. A repeated measures general linear model analysis was conducted for each of the 18 self-management behaviors. The same model was used for all analyses with group (intervention versus control) and activation growth class (stable versus increased) as fixed factors and age, baseline HRQoL, baseline depression, and a measure of social desirability as covariates (HRQoL is significantly higher at baseline for the “increased” class and depression is significantly lower for them. There are no differences at baseline in social desirability in the growth classes).
The interaction effects of group (intervention/control) × activation growth class × time were evaluated for each behavior. As these effects are all interaction terms the null hypothesis being tested is that there are no differences in behavior over time. A significant within subjects effect means that the mean behavior over time differs by the categories of the fixed factor variable(s). Apart from the usual difficulties of repeated measures post hoc tests with estimated marginal means, the small number of participants in the “increased” activation growth class creates cell sizes in examining the effects of activation growth class and group on behaviors that seriously limit the power of any post hoc test as well as the within subjects effects tests. Even if these statistical power issues were not present, we are far less interested in inference about the difference between individual behavior means at discrete time points than in determining if self-management behavior change over time has any consistent pattern by activation growth class and the intervention. The analysis, therefore, focuses on the within and between subjects effects of group and activation growth class.
The repeated measures general linear model analysis was applied to each of the 18 discrete self-management behaviors. The results of these tests are shown in Table 3. For six of the 18 behaviors there was a significant (p < 0.05) difference between the activation growth classes in the behavior pattern over time (growth class × time effect). These self-management behaviors included: engaging in regular exercise, managing stress, paying attention to amount of fat in diet, keeping a BP diary, keeping a glucose diary, and taking diabetes medications as recommended.
To examine overall differences on the 18 behaviors between the two growth classes, change scores were calculated for the 18 behaviors. Although both groups saw increases in positive behaviors, the “increasing” growth class saw a greater degree of increase in 14 of the 18 behaviors, compared with the stable growth class. Using the sign test (Siegel and Castellan 1988) we tested whether the differences in improved behaviors are statistically significant. Assuming the null hypothesis, or no differences in increases, the chance that 14 out of the 18 behaviors would show greater improvements for the increasing growth class, as compared with the stable growth class, are 996 out of 1,000 or p < 0.01.
We also examined the initiation of behaviors after the baseline among both growth classes. Members of the “increased” growth class were more likely to initiate two behaviors: maintaining recommended weight and attention to fat in the diet, than those in the “stable” growth class during the study period. Among the “increased” growth class, who did not pay attention to fat in their diet at baseline, 85 percent initiated the behavior over the 6 months study period. Among members of “stable” growth class, 53 percent of those not paying attention to fat in their diet at baseline, began to attend to it over the study period (χ2 4.8, p < 0.03). A similar pattern was observed for maintaining recommended weight. Among the members of the “increasing” growth class who were not maintaining recommended weight at baseline, 30 percent had initiated this behavior over the 6 months study period. Among “stable” growth class members, only 14 percent initiated this behavior over the study period (χ2 5.5, p < 0.02).
There was a significant between subjects growth class effect for 11 of the 18 behaviors in that the mean behavior over the three waves differed by growth class. In all 11 behaviors the overall mean was higher (better self-management behavior) in the “increased” activation growth class. The significant between subjects effect for activation growth class occurred for six behaviors for which there was no significant within subjects growth class effect. There were high rates of in engaging in four of these behaviors, (ask about complications 78 percent; read about complications 90 percent; read food labels 90 percent; and know recommended weight 88 percent) at baseline among the “increased” growth class. Part of the reason for no significant within subjects change over time for the increased growth class in these four behaviors is that there was little improvement available (a ceiling effect) and with the small sample size a difference in behavior patterns between the “increased” and “stable” classes is not statistically detectable. For the two arthritis-specific behaviors the observed patterns of behavior over time were very different for the “increased” and “stable” activation growth classes, but the lack of statistical power results in failure to identify a significant within subjects effect by growth class.
Group (intervention/control) had a significant within subjects effect, that was not modified by an interaction with growth class, for two self-management behaviors (regular exercise and taking diabetes medication as recommended). The behavior change patterns over time are somewhat less clear than those for the growth classes. For regular exercise the intervention group increased over time while the control group did not (control: baseline behavior score = 2.9; 6 weeks = 2.8, and 6 months = 2.9; intervention: baseline score 2.8; 6 weeks = 3.2 and 6 months = 3.2). For taking diabetes medication as physician recommends the control group improved over time while the intervention group slightly increased at 6 weeks and then declined (control: baseline behavior score = 2.7; 6 weeks = 2.6, and 6 months = 3.0; intervention: baseline score 2.5; 6 weeks = 2.7 and 6 months = 2.6). There was also a significant between subjects group effect for two self-management behaviors. For ability to maintain recommended weight, the mean behavior over all three waves was significantly (F = 4.59, p = 0.033) better in the control group (M = 2.47) than in the intervention group (M = 2.14). For keeping a written diary of BP the overall mean behavior was also significantly better (F = 3.89, p = 0.05) in the control group (M = 2.47) than in the intervention group (M = 2.14).
For one behavior (check BP at least once a week), there was a significant within subjects group × class × time interaction (Table 3). Inspection of the mean behavior scores revealed that of the four group × class combinations only one had any sign of change in behavior over time; the increased activation growth class in the control group had a notable improvement in behavior from baseline to 6 months (baseline M = 2.69; 6 months M = 3.31).
What Factors Predict Activation Growth Class Membership?
With the identification of two activation growth classes that have clearly different activation trajectories over the three waves of the study, it is important to investigate the characteristics of these growth classes. It is reasonable to suggest that activation and subclinical depression are related as depressive symptoms entail a general deactivation. At each of the three waves greater depression is associated with lower activation (baseline r = −0.365, 6 weeks r = −0.444, 6 months r = −0.408 p < 0.0001 all waves). Better HRQoL is also associated with greater activation (baseline r = 0.301, 6 weeks r = 0.326, 6 months r = 0.345, p < 0.001 all waves). Further, depression and HRQoL are strongly negatively correlated (baseline r = −0.731, 6 weeks r = −0.711, 6 months r = −0.708, p < 0.001 all waves).
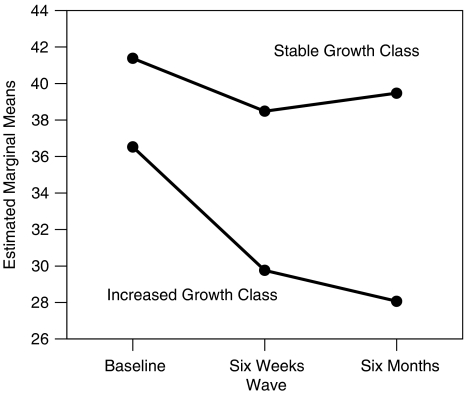
To examine the relationship between activation growth class and depression over the three waves a repeated measures general linear model analysis was conducted with activation growth classes and group (intervention/control) as fixed factors, depression as the repeated measure, and age, baseline HRQoL, and social desirability as covariates. This model evaluates group and activation growth class “effects” on depression over time while controlling for the effects of the covariates. The within subjects effects revealed that only activation growth class (F = 4.84, p = 0.009, Greenhouse–Geisser adjusted) and HRQoL (F = 4.13, p = 0.013) had a significant “effect” on depression over time. HRQoL had a large between subjects effect (F = 441.51, p < 0.0001, partial η2 = 0.53). The only other between subjects effect was for activation growth class (F = 25.94, p < 0.0001, partial η2 = 0.06). As shown in the profile plot (Figure 3) the “increased” activation growth class not only started with less depression than the stable class, but steadily declined in depression (6 months < baseline, 95 percent CI). The “stable” activation growth class remained relatively stable in depression (6 months and baseline not significantly different, 95 percent CI). We also examined the relationship between simple depression change score and behavior change score for each of the tested behaviors. For nine of the 18 behaviors there was a significant (p < 0.05) negative correlation (decreased depression baseline to 6 months related to increased behavior baseline to 6 months). The significant correlations were small to moderate (−0.139 to −0.338). For eight of the 18 behaviors there was a significant positive (better HRQoL and increased behavior) correlation between change in HRQoL and baseline to 6 months behavior change with the significant correlation ranging from 0.104 to 0.308.
Figure 3.
Estimated Marginal Means of Depression by Wave by Activation Growth Class
DISCUSSION
The findings indicate that activation levels do change and that individuals exhibit different change trajectories. Despite the limited statistical power, the findings indicate that changes in activation are accompanied by changes in self-management behaviors.
The findings indicate that a increase in activation is related to a positive change in a variety of self-management behaviors. This is true even when the behavior in question is not being performed at baseline. When the behavior is already being performed at baseline, an increase in activation is related to maintaining a relatively high level of the behavior over time. Finally, positive activation change appears to be sustained over time both when gains are made from baseline to 6 weeks and when they are already high at baseline. The results suggest that if activation is increased, behaviors will follow.
The intervention, showed an impact on a limited number of behaviors over the full study period. Further, the intervention group showed a positive sustained change in activation. However, the control group also increased in activation over the study period, reducing the differences in activation between the intervention and control group to below statistical significance. In fact, for a few of the behaviors the control group showed greater gains in self-management as compared with the intervention group over the course of the study. Why this should have occurred is not clear. The findings do suggest, however, that rather than a failure of the intervention, something stimulated change in the control group over the study period.
The results also reveal the central role that depression plays in activation and in behavior. Those who have depressive symptoms (including subclinical depression) were much less likely to gain in activation and to improve in their self-management behaviors. It appears that as long as depressive symptoms persist, activation is unlikely to occur. These findings have implications for identifying those who face serious barriers to becoming activated. Screening for depression and subclinical depression, and treating the problem is a likely necessary prerequisite to successful interventions aimed at stimulating activation.
CONCLUSIONS
Having a reliable and valid measurement tool to assess patient activation, opens up a number of possibilities for improving care and health outcomes. The study results suggest that if activation is increased, a variety of improved behaviors will follow. This means that activation is an intermediate outcome of interest to many potential users, including public health practitioners, clinicians, those who manage care delivery systems, as well as the payers of health care. Patient activation can be tracked over time and used to assess individual patient progress, as well as monitor whole populations. The measure could be used to give feedback to clinicians about how their patients' progress. It might also allow the early identification of patients before chronic disease develops.
Similarly, PAM could be used to segment large populations and target interventions to those who have both clinical risk factors and insufficient skills to self-manage. It could be used to make referrals to disease management and to determine when patients are ready to leave disease management. These are all uses that the PAM is beginning to be used for.
Even though the findings show that activation levels do change over time, the results did not show that the intervention used in the study, was effective in increasing activation over the gains observed in the control group. Thus, the question remains, what interventions will be most effective in increasing activation? Given the four stages of activation, it is likely that what will help to move a patient from stages 1 to 2 is a different intervention than will facilitate their move them from stages 3 to 4. If we are to take full advantage of the strong measurement represented in the PAM to improve care and outcomes, it is essential to develop and test effective interventions.
Understanding what interventions will work will enable us to use the PAM to tailor care plans to better fit individual needs of patients. Using the four stages of PAM, it may be possible to be much more targeted in supporting patient self-management. Research assessing the impact of different interventions on activation is just beginning. In addition, research is needed to understand the factors that stimulate spontaneous increases in activation, as was observed in this study. Replications of the current investigation, using larger samples and more diverse populations, would help to illuminate the factors that stimulate activation.
Acknowledgments
Support for this study was provided by The Robert Wood Johnson Foundation.
Disclosures: The University of Oregon owns the intellectual property of the PAM. The University is in the process of licensing the PAM to a private company who will issue commercial and research licenses to users. The authors of the PAM will have an equity share in the new company.
REFERENCES
- Hibbard JH, Mahoney E, Stockard J, Tusler M. Development and Testing of a Short Form of the Patient Activation Measure (PAM) Health Services Research. 2005;40(6, part 1):1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Services Research. 2004;39:1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a Self-Management Program on Patients with Chronic Disease. Effective Clinical Practice. 2001;4:256–62. [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, Gonzalez VM, Laurent DD, Holman HR. Evidence Suggesting that a Chronic Disease Self-Management Program Can Improve Health Status While Reducing Hospitalization: A Randomized Trial. Medical Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Mahoney E, Stock R. 2000. “Transformation of the SF-24 into a True Interval Measure of Health-Related Quality of Life.” PeaceHealth Research Report, available on request.
- Mahoney E, Stock R. 2001. “A Brief Linear Measure of Subclinical Depression: The PeaceHealth Depression Scale.” PeaceHealth Research Report, available on request.
- Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioral Sciences. New York: McGraw Hill; 1988. [Google Scholar]
- Speizer H, Greene J, Baker R, Wiitala W. 2006. “Telephone and Web: The Mixed-Mode Challenge.” Presented at the Second International Conference on Telephone Survey Methodology. Miami, FL, January.
- Strahan R, Gerbasi KC. Short, Homogeneous Versions of the Marlowe–Crowne Social Desirability Scale. Journal of Clinical Psychology. 1972;28:191–3. [Google Scholar]
- Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative Management of Chronic Illness. Annals of Internal Medicine. 1997;127:1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]