Abstract
Objective
The purpose of this study is to compare the use of dental services for preschool aged children enrolled in North Carolina Medicaid, a traditional program based on a fee-for-service schedule, and North Carolina Health Choice (NCHC), an State Children's Health Insurance Program (S-CHIP) dental insurance program structured similarly to private insurance.
Study Population
All children (165,858) 1–5 years of age enrolled in Medicaid and S-CHIP (NCHC) at some time during one study year (October 1, 1999–September 30, 2000).
Data Sources/Extraction Methods
Medicaid and NCHC enrollment and dental claims files were obtained for individual children.
Study Design
An observational study with a retrospective cohort design. Use of dental services for each child was measured as having at least one dental claim during the outcome period (October 1, 1999–September 30, 2000). Multivariable logistic regression models were developed to compare the effect of two differently administered insurance programs on the use of dental services, controlling for demographic, enrollment, and county characteristics.
Principle Findings
Children enrolled solely in S-CHIP (NCHC) were 1.6 times more likely (95 percent confidence intervals (CI)=1.50–1.79) to have a dental visit than those enrolled solely in Medicaid. Prediction models for children enrolled for 12 months indicated that those enrolled in S-CHIP (NCHC) had a significantly higher probability of having a dental visit (50 percent) than those enrolled in both plans (44 percent) or Medicaid only (39 percent), a trend found in all age groups.
Conclusions
The S-CHIP (NCHC) program appears to provide children with increased access to dental care compared to children in the Medicaid program.
Keywords: Oral health, Medicaid, S-CHIP, dental services, access to dental care
Poor oral health remains a problem for many children despite the national decline in dental caries that has occurred over the past several decades. A national commitment to addressing this problem has developed in recent years and is embedded in U.S. health policies such as Healthy People 2010 and the National Call to Action to Promote Oral Health (U.S. Department of Health and Human Services 2000a, b, 2003).
Significant disparities in oral health exist according to race, ethnicity, education, income, and geography. Low-income and minority children have more dental disease than other children. They also have reduced access to dental care, resulting in fewer opportunities for prevention and more unmet treatment needs (Vargas, Crall, and Schneider 1998). These disparities are most notable in preschool-aged children (Edelstein, Manski, and Moeller 2000). In 2002, close to 29 million children living in low-income families in the United States were enrolled in the two major public insurance programs available to them, Medicaid or the State Children's Health Insurance Program (S-CHIP). The overall goals of Medicaid and S-CHIP are to help eliminate financial barriers to low-income children and thus improve access to care and resulting health. Even though funds for both programs are shared between the federal and state governments, one important distinction is that states are given more flexibility in their design and implementation of S-CHIP compared with Medicaid. Federal legislation allowed states to implement S-CHIP by expanding enrollment in their Medicaid programs, implementing new state child health plans that are unassociated with Medicaid, or some combination of the two (U.S. General Accounting Office 2000). Initially, 16 states chose S-CHIP programs that were unaffiliated with Medicaid (Almeida, Hill, and Kenney 2000).
The Medicaid program has never achieved expectations for promoting access to dental care during its 3 ½ decades of existence, and has fallen far short during the last decade (Brown 1996). The impact of S-CHIP on access to dental care is largely unknown, but may depend on the type of program chosen by the state. States that chose an expansion program are likely to continue policies that limit access to dental care. States that chose stand-alone programs that resemble private insurance may be more successful than Medicaid. Studies in two states support this conclusion. Lave et al. reported an increase in both the number of children reporting a regular source of dental care and the number of dental visits after 12 months enrollment in Pennsylvania's Children's Health Insurance Program. Self-reported unmet dental needs decreased from 43 percent at plan enrollment to 10 percent at 12 months (Lave et al. 2002). Children enrolled in Michigan's Healthy Kids Dental program had better access to dental care compared with the traditional Medicaid plan (Eklund and Clark 2002). Plan differences appear to have influenced utilization changes in these studies.
S-CHIP children belong to families with slightly higher incomes and possibly higher education levels than Medicaid children. One could assume that children enrolled in S-CHIP, therefore, have greater inherent demand for dental services than those enrolled in Medicaid that could account for utilization differences instead of plan influences. Yet numerous studies have found that children from “poor” and “near poor” families (0–200 percent FPL) are very similar, with almost no differences in utilization of dental care, unmet dental needs, or use of preventive dental services. All of these studies found “not poor” children (>200 percent FPL) to have significantly higher levels of utilization, less need for care, and greater use of preventive dental services than the “poor” and “near poor” children (Watson, Manski, and Macek 2001; National Health Interview Survey 2002–2003). The effects of educational levels followed the same trends as income.
The North Carolina S-CHIP program appears to have the potential to improve children's access to dental services. The program, known as North Carolina Health Choice for Children (NCHC), is administered by BlueCross/BlueShield of North Carolina. This plan is identical to the State Employees Health Insurance Plan where dentists are reimbursed on a fee-for-service basis at 95–100 percent of their usual fees depending on the service. At the time of this study, the NC Medicaid dental plan reimburses dentists on a fee-for-service schedule at only 44–62 percent of usual fees. Providers submit their Medicaid claims and negotiate settlements through the Department of Medical Assistance, a governmental agency, while they submit and negotiate their S-CHIP claims with the nonprofit company, NC BlueCross/BlueShield, in a similar fashion to their privately insured patients (NC Institute of Medicine 1999). Both plans provide statewide a comprehensive set of dental benefits including preventive, diagnostic, and restorative services. Because of key administrative and reimbursement differences, NCHC appears like private insurance to dental providers.
STUDY HYPOTHESIS
The primary aim of this study is to describe and compare the utilization of dental services for preschool-aged children enrolled in Medicaid and S-CHIP programs in North Carolina. Dental insurance promotes the use of dental services in children and results in improved patient outcomes (Manning et al. 1985; Manski, Edelstein, and Moeller 2001). However, the effects of private insurance, even on low-income populations, seem to exceed the effects of public insurance (Bailit, Newhouse, and Brook 1986; Lave et al. 1998; Keane et al. 1999). We hypothesized, therefore, that because of its administrative and reimbursement characteristics, children enrolled in S-CHIP will have a greater likelihood of dental use than those enrolled in Medicaid.
The basic assumption of this study is that the dental visit will provide a comparative indicator of performance for the two public insurance programs, and help to determine if public dental insurance for low-income children that mirrors commercial insurance performs better than Medicaid, known to perform poorly in providing access to care for low-income children.
METHODS
Cohort Selection and Study Design
A retrospective cohort design was used to compare the use of dental services by children enrolled in the NC Medicaid program with those enrolled in the S-CHIP (NC Health Choice) program. All children born between October 1, 1994 and September 30, 1998 with any enrollment in Medicaid or S-CHIP during a designated “outcome period” between October 1, 1999 and September 30, 2000 were selected for study. Thus a cohort of all children ages 1–5 years (12–60 months) who were eligible for dental services in the North Carolina Medicaid or S-CHIP programs during this 12 month outcome period were selected for study. Three enrollment scenarios are possible in the 12-month period: Medicaid only, Health S-CHIP only, and both Medicaid and S-CHIP. The plans were designed and administered in such a way that children could not be concurrently enrolled in both plans. However, national and state policies encouraged enrolling children who lose their Medicaid eligibility in S-CHIP. The main explanatory variable was a three-level variable classifying all children according to their enrollment in Medicaid only, S-CHIP only, or both during the 12 months under study.
Dental utilization was assessed for the 12-month period, October 1999–September 2000. Multiple logistic regression models were developed for this cohort to determine the effect of the public insurance program on the use of dental services, controlling for a number of demographic, enrollment, and ecological county-level characteristics.
Data Sources
The North Carolina Medicaid enrollment and dental claims files in the state's Medicaid Management Information System (MMIS) were used to create a person-level file for the purposes of this study. The enrollment file is a census of children 1–5 years of age enrolled in Medicaid at any point during the outcome period. Enrollment spells were available for Medicaid and S-CHIP subjects from the initiation of the NC Health Choice program (October 1, 1998) to the beginning of the outcome period (October 1, 1999) and through the end of the outcome period (September 30, 2000). These enrollment files provide demographic information about the children (date of birth, sex, race, and county of residence) and enrollment status for every month of enrollment during the 24 months. The Medicaid and S-CHIP dental claims files contained all paid dental claims for an enrolled child during the outcome period. The child's Medicaid/S-CHIP identification number was used to link claims and enrollment files across enrollment years and the outcome period, creating a person-level analytical file with unduplicated observations for each child.
The dataset was supplemented with county-level provider characteristics created from the Medicaid and S-CHIP files along with census type socioeconomic indicators published in Community Health Status Indicator Reports (Health Resources Service Administration 2000). These characteristics were linked to each person-level record using the Medicaid county identification code for each child.
Study Variables
The dependent variable used to measure dental utilization was any use of dental services defined as having at least one paid dental claim during the outcome period. The Annual Dental Visit is considered by NCQA to be a reliable and valid pediatric oral health performance measure. The NCQA also has suggested that dental visits be monitored beginning before the current recommended age of 4 years, and that age be stratified by year rather than aggregated as is presently done in the majority of national studies (Crall, Szlyk, and Schneider 1999).
The primary independent variable was the child's insurance program, categorized as Medicaid, S-CHIP, or sequential enrollment in both. The primary control variable was the number of months enrolled in each plan during the 12-month outcome period. Another enrollment variable measured gaps in enrollment (yes versus no) during the outcome period, a gap being defined as at least two consecutive months without enrollment. A final enrollment variable controlled for coverage before the study utilization period as Medicaid, S-CHIP, both, or neither. Additional control variables consisted of age of the child at the beginning of the outcome period in individual years 1–5, sex, race (black, Hispanic, Native American, white, and other), and county-level indicators of access and health status.
The county-level variables provide information for the 100 counties in North Carolina, and denote “ecological” variables representing the child's health care environment rather than their individual or family characteristics (Shi 2000). Area characteristics of a child's county of residence include: the percentage of individuals living below the federal poverty level; percentage with less than a high school education; and infant mortality rate. The county-level provider characteristic was the proportion of privately practicing dental providers providing care to publicly insured children per eligible children (dentists per 1,000 publicly insured children 1–5 years of age). To be considered a public insurance dental provider, a dentist must have submitted dental claims for at least three different children during the 12-month study period. “Three” children was used as the threshold for participation because it is the median number of children treated by the 1,603 providers submitting claims for this cohort of children. This dataset consisted of only private sector or privately practicing dentists. Health department clinics or federally qualified community health centers were not included in this analysis.
Statistical Methods
Statistical evaluation of the study aims began with descriptive and bivariate analyses of outcome and control variables, followed by the incremental building of a multivariate model to quantify the effect of health plan on dental utilization controlling for other child and county-level characteristics. Descriptive analyses examined the distribution of children across health plan, demographic characteristics, enrollment characteristics, and county-level variables. This assessment focused on the basic characteristics of the sample. Next, the likelihood of having a dental visit was analyzed descriptively according to these explanatory variables. Plots were generated and bivariate analyses were conducted by calculating odd ratios and correlation values for the association between health plan (Medicaid, S-CHIP, or both) and the outcome (dental visit), along with all control variables.
Results from the initial analysis revealed that duration of enrollment had such a strong effect on the likelihood of a dental visit that it was necessary to determine the most parsimonious and best fitting relationship between duration of enrollment and probability of use that could be used in the multivariate analyses. A previous study found significant bias in estimates of dental utilization when study samples are limited to children with 12-months of continuous enrollment (Hughes and Rozier 2002). Therefore, to find the most precise measure of enrollment, four regression models were created to examine goodness of fit (Breslow and Day 1980).
The first model was a class-level model created to represent the log odds of dental utilization for each individual month within the range 1–12 months, without specifying a linear function of months. We considered this model, which contained 11 degrees of freedom, the “gold standard” for describing utilization, because it explained the maximum amount of variation (quantified as −2 Log Likelihood for the model) in log odds of dental utilization. However, this gold standard model necessarily lacked precision because it had many degrees of freedom, and it could not define any linear or curvilinear trend between duration of enrollment and log odds of dental utilization.
Subsequently, three additional models were fit with linear (1 df), exponential (2 df), and cubic (3 df) functions for enrollment duration. These mathematical functions were chosen based on visual plots of the probability of dental utilization over the 12-month study period. The exponential and cubic functions were evaluated because the predicted probability of utilization appeared to depart from the linear function of enrollment, suggesting that the examination of other mathematical functions of enrollment were worth pursuing. In evaluating the three mathematical functions of enrollment against the gold-standard class-level model, three criteria were used: (1) qualitative—to identify the mathematical model that most closely resembled the class-level model when probability of utilization was plotted against months of enrollment; (2) quantitative—to identify the mathematical model that maximized variation (−2 Log Likelihood for the model) that was closest to the gold-standard model; and (3) precision—to identify the model that had the most precise estimates (i.e., smallest standard errors) of utilization across the range of enrollment. These three criteria compete with one another, so the model that was finally selected represented a trade-off between the models' qualitative fit, quantitative fit, and precision.
A stratified analysis was used to evaluate which, if any, variables modified or confounded the association between health plan and the likelihood of having a dental visit. The first step was to check for effect modification. For the continuous measure of enrollment duration, the percent difference in the predicted probabilities of dental utilization for each strata of health plan were examined and a designated magnitude of a 50 percent change was used to identify candidate effect modifiers. The data were then stratified by the potential effect modifiers from among the categorical variables and measures of association between health plan and dental utilization assessed for each stratum (Rothman and Greenland 1998). Differences in measures of association across the strata were assessed using the Breslow–Day Test for Homogeneity. When they were sufficiently different (i.e., the Breslow–Day test for homogeneity is p<.05), the variable was considered as a potential effect modifier and the interaction included in the regression analysis for confirmation (Breslow and Day 1980). Confounding of any explanatory variables was confirmed in multivariable regressions with the inclusion of explanatory variables based on statistical significance at the α=0.05 level.
Multivariate logistic regression was used to determine a model for the least biased estimate of effect of the health plan (Medicaid, S-CHIP, versus both) on the log odds of having a dental visit over the 12-month study period, controlling for enrollment time (months) and age (years). This method was employed to assess the predicted probabilities of a dental visit and 95 percent confidence intervals (CI) between the health plans.
Logistic regression models were then built to determine the effects of the other control variables: sex (female versus male), race (black, Hispanic, Native American, and other versus white), additional enrollment characteristics, and county-level indicators. Decisions to keep or drop variables in the logistic regression modeling process in the exploratory analyses of this study were based on statistical significance at the α =0.05 level, or if there was a significant influence of an explanatory variable, based on a 10 percent change in the parameter estimate of the health plan category (Rothman and Greenland 1998).
A simulation was used to create the probabilities of a dental visit and 95 percent CI according to health plan using the final regression model. SAS PROC LOGISTIC was used to generate an output dataset containing predicted probabilities and the 95 percent CI for selected values of covariates (age, race, and enrollment). The SAS statistical package was used for the analysis (SAS Institute 2001).
RESULTS
Enrollment Classification
The cohort consisted of 165,858 children ages 1–5 years, with enrollment in Medicaid, S-CHIP, or both programs during the study outcome period. The mean duration of enrollment for all children was 9.8 (SE=0.01) months. Children who switched from Medicaid to S-CHIP during the outcome period had the longest enrollment time of 11.03 (SE=0.02) months, followed by Medicaid only with 9.8 (SE=0.01) months, and S-CHIP only with 8.7 (SE=0.04) months.
The series of analyses examining the goodness-of-fit for different mathematical functions of enrollment duration identified a cubic relationship as the optimal function to predict the likelihood of a dental visit. Both the linear and exponential models departed significantly (p<.001) from the class-level model according to residual variances. The cubic function had a significantly smaller departure and qualitatively had the best fit to the class-level model of enrollment.
Enrollment duration was next examined as a potential effect modifier of the relationship between health plan and the likelihood of dental utilization. No statistically significant interactions (p<.10) between health plan and the three parameters of enrollment duration were observed in the cubic model (i.e., months, months squared, and months cubed). Because of this finding and the observation that the cubic function of enrollment duration appeared to adequately represent the data, regression models were built using the cubic function of enrollment and no interaction terms.
Dental Utilization
Overall, 19 percent of children had a dental visit during October 1, 1999–September 30, 2000. Children enrolled in S-CHIP were more likely to have had a dental visit compared with Medicaid enrolled children (crude OR=1.21; 95 percent CI 1.15–1.27). Table 1 provides descriptive information on the likelihood of a dental visit for the study cohort (n =165,858) according to its demographic, enrollment, and county characteristics, stratified by health plan. Age, race, enrollment duration, and enrollment continuity were associated with having a dental visit. A demographic indicator that was associated with varying levels of dental utilization was race. Hispanic children were less likely to have a dental visit, while Native-American children were more likely to have a dental visit than white, black, or children with race classified as “other.” The number of dentists providing care to publicly insured children was associated with having a dental visit (Table 1). Children from counties with less than five dentists filing public dental insurance claims were half as likely to have a dental visit compared with children from counties with greater then 10 public dental insurance providers (OR=0.50; 95 percent CI=0.48–0.52). In the bivariate analyses, children from counties with higher percentages of people falling below the federal poverty level, higher percentages of persons with less than a high school education, and higher infant mortality rates, had higher dental utilization (p<.001).
Table 1.
Descriptive Statistics of Dental Utilization Stratified by Health Plan
| Covariates | Medicaid | Health Choice | Both | p-value* | OR‡ |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 18% | 21% | 25% | <.001 | 1.01 (0.98–1.03) |
| Male (ref) | 18% | 22% | 25% | <.001 | 1.00 |
| Age (years) | |||||
| 1–2 | 5% | 6% | 8% | <.001 | 0.12 (0.11–0.12) |
| 2–3 | 14% | 17% | 21% | <.001 | 0.36 (0.35–0.37) |
| 3–4 | 26% | 30% | 36% | <.001 | 0.75 (0.73–0.78) |
| 4–5 (ref) | 31% | 37% | 43% | <.001 | 1.00 |
| Race | |||||
| Black | 18% | 20% | 25% | <.001 | 0.99 (0.97–1.02) |
| Hispanic | 15% | 13% | 18% | =.010 | 0.75 (0.72–0.79) |
| Native American | 26% | 29% | 25% | =.556 | 1.52 (1.40–1.64) |
| Other | 20% | 19% | 25% | =.030 | 1.10 (1.04–1.16) |
| White (ref) | 18% | 24% | 26% | <.001 | 1.00 |
| Gap in utilization period | |||||
| No | 19% | 21% | 25% | <.001 | 1.84 (1.75–1.93) |
| Yes | 11% | 20% | 29% | <.001 | 1.00 |
| Enrollment duration | |||||
| Number of months enrolled | 9.8 | 8.3 | 11.3 | <.001 | 1.24 (1.23–1.24) |
| Prior enrollment | |||||
| Both | 0% | 25% | 23% | † | 1.62 (1.44–1.82) |
| Medicaid | 19% | 0% | 24% | † | 1.86 (1.78–1.95) |
| Health choice | 0% | 23% | 32% | † | 1.52 (1.39–1.65) |
| None (ref) | 11% | 19% | 19% | <.001 | 1.00 |
| County-level variables | |||||
| Public providers per 1,000 eligible children | |||||
| <5 providers | 13% | 16% | 18% | <.001 | 0.50 (0.48–0.52) |
| 5–10 providers | 18% | 20% | 25% | <.001 | 0.77 (0.75–0.79) |
| ≥ 10 providers (ref) | 22% | 27% | 28% | <.001 | 1.00 |
| Percent of county population below the FPL | |||||
| ≥ 16% below FPL | 20% | 23% | 27% | <.001 | 1.19 (1.15–1.24) |
| 10–16% below FPL | 18% | 22% | 24% | <.001 | 1.01 (0.98–1.05) |
| <10% below FPL (ref) | 18% | 18% | 23% | <.001 | 1.00 |
| Percent of county with less than high school education | |||||
| ≥ 20% of population (0) | 19% | 20% | 25% | <.001 | 1.06 (1.04–1.09) |
| ≤20% of population (1) | 18% | 22% | 25% | <.001 | 1.00 |
| Infant mortality rate | |||||
| ≥ 10% infant mortality rate (0) | 21% | 22% | 28% | <.001 | 1.27 (1.24–1.31) |
| ≤10% infant mortality rate (1) | 17% | 21% | 23% | <.001 | 1.00 |
p-value is the χ2 difference between plans for each covariate.
χ2not valid due to zero cells.
Odds ratio is the likelihood of a dental visit for each covariate, controlling for plan with referent levels designated.
FPL, federal poverty level.
Multivariable Regression Results
According to the baseline regression model for the effect of health plan on the odds of having a dental visit during the 12-month outcome period, children enrolled in S-CHIP were more likely to have had a dental visit compared with Medicaid enrolled children (OR=1.5; 95 percent CI=1.45–1.61). Children enrolled in both plans at some point during the 12-month period also had a slight increase in the likelihood of having a dental visit (OR=1.2; 95 percent CI=1.17–1.31) compared with Medicaid enrolled children. This model controlled for only enrollment duration and age.
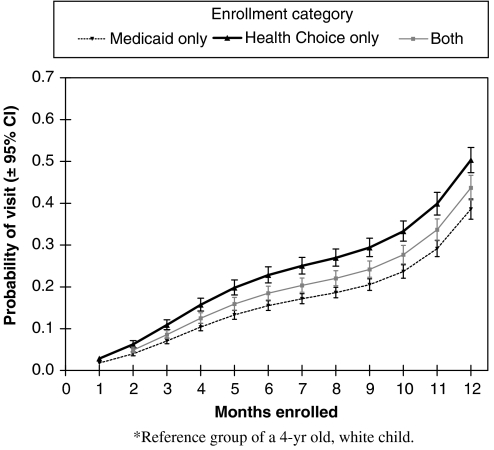
Table 2 presents the parameter estimates for the final model of the effect of health plan on dental utilization, controlling for enrollment duration during the study period, age, race, gap in enrollment, prior enrollment, and county-level indicators. Overall, children enrolled in S-CHIP were 1.6 times more likely (95 percent CI=1.50–1.79) to have a dental visit than those enrolled in Medicaid only. Children enrolled sequentially in Medicaid and then S-CHIP were 1.24 times more likely (95 percent CI=1.16–1.32) than the Medicaid only group. Figure 1 plots the probability estimates and 95 percent CI for having a dental visit during the 12-month study period according to the number of months enrolled. Those enrolled in S-CHIP had a significantly higher probability of having a dental visit when enrolled for 12 months (50 percent), than those enrolled in both plans (44 percent), or Medicaid only (39 percent), a trend found in all age groups.
Table 2.
Final Regression Model for a Dental Visit
| Final Regression Model | Parameter Estimate | SE | p | Odd's Ratio |
|---|---|---|---|---|
| Intercept | −4.2212 | 0.15 | <.0001 | |
| Individual-level variables | ||||
| Health plan | ||||
| Health choice | 0.4926 | 0.04 | <.0001 | 1.64 (1.50–1.79) |
| Both | 0.2160 | 0.03 | <.0001 | 1.24 (1.16–1.33) |
| Medicaid (ref) | 0.00 | 0.00 | 1.00 | |
| Age* | ||||
| 1 | −2.2655 | 0.02 | <.0001 | 0.10 (0.10–0.11) |
| 2 | −1.0883 | 0.02 | <.0001 | 0.34 (0.33–0.35) |
| 3 | −0.3069 | 0.02 | <.0001 | 0.74 (0.71–0.76) |
| 4 (ref) | 0.00 | 0.00 | 1.00 | |
| Enrollment duration | ||||
| Enrolled months (cubic) | 0.00672 | 0.0004 | <.0001 | 1.007 (1.006–1.008) |
| Race | ||||
| Black | −0.1583 | 0.02 | <.0001 | 0.85 (0.83–0.88) |
| Hispanic | −0.0914 | 0.03 | .0003 | 0.91 (0.87–0.96) |
| Native American | 0.2934 | 0.05 | <.0001 | 1.34 (1.23–1.47) |
| Other | −0.0603 | 0.03 | .0537 | 0.94 (0.89–1.001) |
| White (ref) | 0.00 | 0.00 | 1.00 | |
| Enrollment continuity | ||||
| No gap | −0.2239 | 0.03 | <.0001 | 0.80 (0.73–0.85) |
| Gap (ref) | 0.00 | 0.00 | 1.00 | |
| Prior enrollment | ||||
| Health choice | −0.2023 | 0.05 | <.0001 | 0.82 (0.74–0.90) |
| Both | −0.0437 | 0.07 | .5319 | 0.96 (0.84–1.10) |
| Medicaid | −0.0468 | 0.03 | .1067 | 0.95 (0.90–1.01) |
| Neither (ref) | 0.00 | 0.00 | 1.00 | |
| County-level variables | ||||
| Public providers/1,000 eligible children ratio | ||||
| <5 providers | −0.7096 | 0.02 | <.0001 | 0.49 (0.47–0.51) |
| 5–10 providers | −0.3263 | 0.02 | <.0001 | 0.72 (0.70–0.75) |
| ≥ 10 providers (ref) | 0.00 | 0.00 | 1.00 | |
| Percent of county population below the FPL | ||||
| ≥ 16% below FPL | −0.2395 | 0.03 | <.0001 | 0.79 (0.74–0.83) |
| 10–16% below FPL | −0.2308 | 0.02 | <.0001 | 0.79 (0.76–0.83) |
| <10% below FPL (ref) | 0.00 | 0.00 | 1.00 | |
| Percent with <high school education | ||||
| ≥ 20% of population | −0.0627 | 0.02 | <.0001 | 0.94 (0.91–0.97) |
| <20% of population (ref) | 0.00 | 0.00 | 1.00 | |
| Infant mortality rate | ||||
| ≥ 10% infant mortality rate | 0.2350 | 0.02 | <.0001 | 1.27 (1.23–1.31) |
| <10% infant mortality rate (ref) | 0.00 | 0.00 | 1.00 | |
Controlling for age, enrollment duration, race, gap in enrollment, prior enrollment, and county-level indicators.
FPL, federal poverty level.
Figure 1.
Final Regression Model with the Predicted Probabilities of Dental Visit.
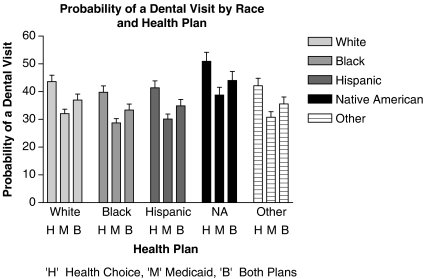
Figure 2 presents the predicted probabilities of dental visit for racial subgroups by health plan. The effect of plan type (Health Choice, Medicaid, Both plans) was the same regardless of race.
Figure 2.
Final Regression Model with the Predicted Probabilities of Dental Visit for Racial Subgroups by Health Plan.
DISCUSSION
Medicaid programs have performed poorly in providing effective dental coverage for the heterogeneous and dynamic populations they insure. The State Children's Health Insurance Program provides states with the opportunity to creatively expand health insurance for children in low-income families and experiment with innovative programs. This study examined the differences in utilization of dental services for a population of preschool-aged children enrolled in North Carolina Medicaid and NCHC, an S-CHIP dental insurance program structured similar to private insurance.
The primary finding from this study is that 1–5-year-old children enrolled in S-CHIP use dental services at a significantly greater rate than children enrolled in Medicaid. The use of dental services was 22 percent greater for children enrolled in this new insurance program than it was for children enrolled in Medicaid. This difference remained after controlling for a number of demographic characteristics of the child, their enrollment patterns and characteristics of the county in which they resided at the time of use. The 22 percent difference in utilization appears to be of clinical and public health significance, particularly when considered along with the approximate 20 million children enrolled in these public programs nationwide. This 22 percent higher utilization rate, achieved through alterations to program administration, including competitive reimbursement rates. This increase is made all the more meaningful when viewed against temporal patterns in children's use of preventive dental services that have remained chronically low or have even decreased from year-to-year (Brown 1996). Within the U.S. population at large, levels of dental services provision historically have remained static, even in periods of economic growth (Chattopadhyay, Slade, and Shugars 2003), which further highlights the significance of the 22 percent increase in utilization observed in this study. Based on these findings we conclude that separate S-CHIP and other public insurance programs designed like private insurance have the potential to improve access to dental care compared with traditional Medicaid programs.
Differences in utilization according to race were observed, but the effect of insurance plan remained the same. Black and Hispanic children overall had significant less utilization than children of other races, although black children still had significantly higher utilization in S-CHIP than in Medicaid. Native American children appear to have higher utilization than all other racial categories. This finding may be because Native American children have access to a delivery system that is different and more favorable than do enrolled children of other races. Living in specific geographic areas with access through the Indian Health Service or some other institutionalized programs specifically designed to serve Native Americans may increase their access to care. Regardless of racial subgroup, the effect of plan type was the same with S-CHIP having the highest utilization.
Control variables other than race, age, and enrollment duration found to be significant in the final regression model were county-level census measures of socioeconomic status. Children residing in a county with a higher percentage of individuals living below the poverty level, higher percentages of people with less than a high school education, and higher infant mortality rates had higher levels of dental utilization. This finding could mean that counties with these socioeconomic indicators have greater numbers of eligible children, therefore increasing rates of utilization due to the sheer numbers of children seeking care. The existence of safety-net clinics in these counties may also increase utilization. It should be noted that these county-level socioeconomic indicators did not contribute to the multivariate model as significantly as the county-level measures of provider availability. The availability of dental providers who participated in public insurance was strongly associated with utilization rates. The significant role that the availability of providers plays in the utilization of dental services has strong policy implications related to dental use in general, but also for interpretation of the results of this study. The effect of S-CHIP may have been even greater if demand did not exceed the supply of dentists in these North Carolina counties.
Little information on the impact of S-CHIP on access to dental care is available at this early stage of its implementation. The Urban Institute has provided results of a qualitative analysis of the experience of 18 states in implementing their S-CHIP dental programs (Almeida, Hill, and Kenney 2000). They conclude that separate S-CHIP programs result in improved dentists' participation and access to dental services. In addition, a compendium of state-level innovations (Schneider et al. 2003) has documented the positive contributions of unique public–private partnerships on the provision of dental services for low-income children. For example, a pilot program to improve dentist participation in Medicaid and access to care for low-income children was established in Michigan. The program consisted of an increase in reimbursement rates to marketplace levels, issuance of private insurance-like membership cards to enrollees and adjustments in billing procedures to mirror private insurance procedures. Dental visits in the Michigan Medicaid program increased from 18 percent of eligible children to 44 percent. The number of dentists participating in the program increased by more than 300 percent.
A recent evaluation of the NCHC program lends support to our conclusion that separate S-CHIP programs help increase access to dental care (Mofidi et al. 2001). In that study, caregivers of newly enrolled, “school-aged” children self-reported utilization of dental care after 12 months of enrollment. The percentage of children who received dental services increased from 47 percent in the year before enrollment to 64 percent in the year after enrollment. The percentage of children with an unmet dental need decreased from 43 to 18 percent. The extent of access to dental care for preschool-aged children reported in this study was less due to that it is based on claim data of much younger children who face increased barriers to care.
Under the controlled conditions of our study, S-CHIP children consistently had greater levels of dental utilization than Medicaid children. The primary reason for this difference may be the competitive reimbursement rates offered to dentists who participate in NCHC, which in effect may help reduce this barrier to dentists' participation. A previous study in North Carolina has shown that moderate fee increases on the order of 23 percent had little effect on dentists participation in the Medicaid program and only modest effects on the number of children that participating dentists accepted as patients (Mayer et al. 2000). Our results suggest that dentists will increase their participation in Medicaid if reimbursement levels are closer to their usual fees. They also suggest that the reimbursement levels for NCHC, which are about 100 percent of usual fees, are well within the range necessary to encourage dentists' participation in NCHC.
According to the 2002 National Health Interview Survey, dental visits for “poor” and “near poor” children 2–17 years of age were very similar (64.4 and 66.9 percent) and less than for the nonpoor (79.6 percent). “Poor” and “near poor” poverty status levels are family incomes that fall below the poverty threshold and up to 200 percent the federal poverty level, similar to income designations for eligibility for Medicaid and S-CHIP programs included in this study (U.S. Department of Health and Human Services 2002–2003). The similar rates of dental use among the poor and near poor in the national survey lend support to the conclusion of this paper that S-CHIP and Medicaid enrolled children have similar demands for dental services and that the utilization differences found between the two differently structured programs are significant enough that it can not be explained by differences in educational attainment, demand, or income of enrolled children and their families.
The major finding of this study also conforms to theory on physicians' participation in public insurance programs. According to the dual market theory, physicians operate in two distinct markets that are distinguished by source and level of payment. While providers act as price setters in the private market, they face an exogenously determined price in the public market (Kushman 1978; Sloan and Steinwald 1978). If marginal revenue in the private market exceeds marginal revenue in the public market at the quantity of services that the provider wishes to supply, then the provider will see only private-pay patients. However, if marginal revenue from public-pay patients exceeds the private marginal level at some point below the practice capacity, the provider will see both public- and private-pay patients. This theory is particularly relevant where excess demand for services exists, which is the situation for dental care in North Carolina.
Another difference between NC Medicaid and Health Choice that might help explain differences in dental utilization among covered children is the way in which claims and inquiries are processed administratively. NCHC is administered through BlueCross BlueShield of North Carolina. The North Carolina Department of Medical Assistance administers the Medicaid program. Cumbersome administrative procedures are documented in North Carolina and across the nation as an important barrier to provider participation in Medicaid (Venezie and Vann 1993; Brown 1996; NC Institute of Medicine 1999; U.S. General Accounting Office 2000a,b). Medicaid administrative procedures are one of the primary reasons dentists give for not participating in Medicaid. The administrative procedures used by BlueCross BlueShield may be more acceptable to dentists than those used by Medicaid, as they are similar to the other privately insured patients in their practice.
The NCQA recommended performance measure of a “dental visit” suggests that every child enrolled in EPSDT who is 1 year of age or older should have an annual dental visit. Yet, use of dental services in young children nationwide falls far short of this recommendation. One year of age is the “benchmark” of when children are supposed to have their first dental visit (Crall, Szlyk, and Schneider 1999; Hale 2003). These guidelines underscore the importance of including young preschool-aged children (1–2 year olds) in any analysis of children's dental utilization. Nationally, only about 21 percent of all children under the age of 6 had a dental visit in 1996. Only 15 percent of children who were at or below 200 percent of the federal poverty level had a dental visit in that year (Edelstein, Manski, and Moeller 2000). These poor utilization rates among very young children underscore the importance of public insurance programs incorporating innovative strategies to increase demand for dental care for these children.
Contributions, Limitations, and Future Research
This study is the first one to examine dental utilization using administrative data to determine the performance of two public dental insurance plans for preschool-aged, low-income children. A dental visit is a necessary health service to provide primary prevention and treatment for oral diseases. The NCHC program appears to have provided poor working families with increased access to dental care for their children compared with families in the Medicaid program. These findings suggest that S-CHIP dental programs resembling private insurance models and reimbursing dentists close to market rates hold the potential to partially address problems associated with dental access for low-income children.
Dental claims are based on payments to providers for services delivered, and we have no method for identifying the delivery of services for which reimbursement was not requested. We also have no way to measure the demand for dental care or understand care-seeking behavior of these children and their families. The S-CHIP program draws enrollment from a group of families with slightly higher incomes than Medicaid. Ideally, potential joint influences of socioeconomic status and program design should be evaluated using a factorial design, in which the two different insurance programs included in our study would be contrasted within poor and less-poor populations. However, program eligibility criteria precluded relatively less-poor families from the Medicaid program. Hence, we instead used county-level markers of income and education as surrogate covariates to control for socioeconomic status, with the results showing little confounding of program effects due to socioeconomic status (Table 2).
The use of different delivery systems (private sector) supported by competitive payments appears to be contributing to improved provider participation and better access to dental care in some state SCHIP programs. Additional studies are needed to evaluate other aspects of these programs and their effects such as; the impact of safety-net clinics, demand for care by enrollees, their relative satisfaction with the two insurance programs, program structure and reimbursement levels, dentists' willingness to serve low-income children insured by S-CHIP, and perhaps most importantly, the impact of the these two programs on oral health status.
Acknowledgments
This research was funded in part by AHRQ grant 1-R03-HS11514-01, MCH grant 5-T17 MC 00015, HRSA grant D13HP30002, and NIDCR grants 1-T32-DE-07191 and 1K22-DE-016084-01. The authors recognize Dr. Paul Buescher and the staff at the North Carolina State Center for Health Statistics for their help in obtaining the data and linkages.
REFERENCES
- Almeida R, Hill I, Kenney G. Does SCHIP Spell Better Dental Care Access for Children? An Early Look at New Initiatives. Assessing the New Federalism. Washington, DC: The Urban Institute; 2000. [Google Scholar]
- Bailit HL, Newhouse J, Brook R. Dental Insurance and the Oral Health of Preschool Children. Journal of the American Dental Association. 1986;113(5):773–6. doi: 10.14219/jada.archive.1986.0272. [DOI] [PubMed] [Google Scholar]
- Breslow N, Day N. Statistical Methods in Cancer Research: The Analysis of Case Control Data. Lyon: International Agency for Research on Cancer; 1980. [PubMed] [Google Scholar]
- Brown JG. Children's Dental Services under Medicaid: Access and Utilization. Washington, DC: Department of Health and Human Services, Office of Inspector General; 1996. [Google Scholar]
- Chattopadhyay A, Slade GD, Shugars DA. Charges for Oral Health Care during a Period of Economic Growth in the U.S.: 1987–1996. Journal of Public Health Dentistry. 2003;63(2):104–11. doi: 10.1111/j.1752-7325.2003.tb03483.x. [DOI] [PubMed] [Google Scholar]
- Crall JJ, Szlyk CI, Schneider DA. Pediatric Oral Health Performance Measurement: Current Capabilities and Future Directions. Journal of Public Health Dentistry. 1999;59(3):136–41. doi: 10.1111/j.1752-7325.1999.tb03262.x. [DOI] [PubMed] [Google Scholar]
- Edelstein BL, Manski RJ, Moeller JF. Pediatric Dental Visits during 1996: An Analysis of the Federal Medical Expenditure Panel Survey. Pediatric Dentistry. 2000;22(1):17–20. [PubMed] [Google Scholar]
- Eklund SA, Clark SJ. Healthy Kids Dental Demonstration Program. Ann Arbor, MI: Child Health Evaluation and Research Unit, Michigan Department of Community Health, University of Michigan; 2002. [Google Scholar]
- Hale KJ. Oral Health Risk Assessment Timing and Establishment of the Dental Home. Pediatrics. 2003;111:1113–6. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- Health Resources Service Administration (HRSA) Community Health Status Report: Community Health Status Indicators Project. 2000.
- Hughes TL, Rozier RG. The Influence of Dental Insurance Enrollment Characteristics on the Estimates of Dental Utilization. Journal of Dental Research. 2002;81 (Spec Issue)A–266. [Google Scholar]
- Keane CR, Lave JR, Ricci EM, LaVallee CP. The Impact of a Children's Health Insurance Program by Age. Pediatrics. 1999;104(5, part 1):1051–8. doi: 10.1542/peds.104.5.1051. [DOI] [PubMed] [Google Scholar]
- Kushman JE. Participation of Private Practice Dentists in Medicaid. Inquiry. 1978;15(3):225–33. [PubMed] [Google Scholar]
- Lave JR, Keane CR, Lin CJ, Ricci EM. The Impact of Dental Benefits on the Utilization of Dental Services by Low-Income Children in Western Pennsylvania. Pediatric Dentistry. 2002;24(3):234–40. [PubMed] [Google Scholar]
- Lave JR, Keane CR, Lin CJ, Ricci EM, Amersbach G, LaVallee CP. Impact of a Children's Health Insurance Program on Newly Enrolled Children. Journal of the American Medical Association. 1998;279(22):1820–5. doi: 10.1001/jama.279.22.1820. [DOI] [PubMed] [Google Scholar]
- Manning WG, Bailit HL, Benjamin B, Newhouse JP. The Demand for Dental Care: Evidence from a Randomized Trial in Health Insurance. Journal of the American Dental Association. 1985;110(6):895–902. doi: 10.14219/jada.archive.1985.0031. [DOI] [PubMed] [Google Scholar]
- Manski RJ, Edelstein BL, Moeller JF. The Impact of Insurance Coverage on Children's Dental Visits and Expenditures. Journal of the American Dental Association. 2001;132(8):1137–45. doi: 10.14219/jada.archive.2001.0341. [DOI] [PubMed] [Google Scholar]
- Mayer ML, Stearns SC, Norton EC, Rozier RG. The Effects of Medicaid Expansions and Reimbursement Increases on Dentists' Participation. Inquiry. 2000;37(1):33–44. [PubMed] [Google Scholar]
- Mofidi M, Slifkin R, Silberman P, Freeman V. Program on Health Care Economics and Finance. Chapel Hill, NC: Cecil G Sheps Center for Health Services Research, University of North Carolina at Chapel Hill; 2001. School-Aged Children Have Improved Access to Dental Care under NC Health Choice. [Google Scholar]
- NC Institute of Medicine (NC-IOM) Task Force on Dental Care Access. Chapel Hill, NC: NC-IOM/NC DHHS; 1999. [Google Scholar]
- Rothman K, Greenland S. Modern Epidemiology. 2. Philadelphia: Lippincott-Raven; 1998. [Google Scholar]
- SAS Institute. SAS User's Guide: Statistics Version 8. Cary, NC: SAS Institute; 2001. [Google Scholar]
- Schneider D, Crall JJ, Allen JS, Hayes K. State Innovations to Improve Dental Access for Low-Income Children: A Compendium. Chicago: American Dental Association; 2003. Available at http://www.prnewswire.com/mnr/ada/11207/ [Google Scholar]
- Shi L. Type of Health Insurance and the Quality of Primary Care Experience. American Journal of Public Health. 2000;90(12):1848–55. doi: 10.2105/ajph.90.12.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan FA, Steinwald B. Physician Participation in Health Insurance Plans: Evidence on Blue Shield. Journal Human Resources. 1978;13(2):237–63. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Oral Health in America. A Report of the Surgeon General. Rockville, MD: National Institutes of Health; 2000a. Available at http://www.nidcr.nih.gov/sgr/execsumm.htm. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010: Objectives for Improving Health. Washington, DC: The Office of Disease Prevention and Health Promotion; 2000b. Available at http://www.cdc.gov/OralHealth/topics/healthy_people.htm. [Google Scholar]
- U.S. Department of Health and Human Services. National Health Interview Survey (NHIS) 2002–2003 (Available at http://www.cdc.gov/nchs/nhis.htm)
- U.S. Department of Health and Human Services. National Call to Action to Promote Oral Health. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Dental and Craniofacial Research; 2003. NIH Publication No. 03-5303. [PubMed] [Google Scholar]
- U.S. General Accounting Office. Oral Health: Factors Contributing to Low Use of Dental Services by Low-Income Populations. Washington, DC: U.S. General Accounting Office; 2000. [Google Scholar]
- U.S. Public Health Service. Healthy People 2000: Progress Report for Oral Health. Washington, DC: National Center for Chronic Disease Prevention and Health Promotion; 2000. [Google Scholar]
- Vargas CM, Crall JJ, Schneider DA. Sociodemographic Distribution of Pediatric Dental Caries: NHANES III, 1988–1994. Journal of the American Dental Association. 1998;129(9):1229–38. doi: 10.14219/jada.archive.1998.0420. [DOI] [PubMed] [Google Scholar]
- Venezie RD, Vann WF. Pediatric Dentists' Participation in the North Carolina Medicaid Program. Pediatric Dentistry. 1993;15(3):175–81. [PubMed] [Google Scholar]
- Watson MR, Manski RJ, Macek MD. The Impact of Income on Children's and Adolescents' Preventive Dental Visits. Journal of the American Dental Association. 2001;132(11):1580–87. doi: 10.14219/jada.archive.2001.0093. [DOI] [PubMed] [Google Scholar]