Abstract
Objective
To measure the relationship between time spent waiting for health care services and patients' mortality.
Data Source
Data on the number of days until the next available appointment at 89 Veterans Affairs (VA) medical centers in 2001 were extracted from a VA administrative database. These facility-level data were merged with individual-level data for a sample of veterans who visited a VA geriatric outpatient clinic in 2001. The merged dataset includes facility-level data on waiting times and individual-level data on demographics, health status (e.g., diagnoses), and mortality.
Study Design
This was a retrospective observational study using secondary data from administrative sources. The dependent variable was mortality within a 6-month follow-up period. The main explanatory variable of interest was VA facility-level wait times for outpatient visits measured in number of days. Random effects logistic regression models were risk adjusted for prior individual health status and facility-level differences in case mix.
Principal Findings
Veterans who visited a VA medical center with facility-level wait times of 31 days or more had significantly higher odds of mortality (odds ratio = 1.21,p = 0.027) compared with veterans who visited a VA medical center with facility-level wait times of < 31 days.
Conclusions
Our findings support the largely assumed association between long wait times for outpatient health care and negative health outcomes, such as mortality. Future research should focus on the causes of long waits for health care (e.g., physician reimbursement levels), the consequences of long waits in other populations, and effective policies to decrease long waits for health care services.
Keywords: Delayed access to care, mortality, wait times
Ensuring timely access to health care is a major policy concern in the United States. Delayed access has been found to increase the use of emergency rooms for nonurgent conditions (Shesser et al. 1991; Cunningham et al. 1995) and to decrease patient satisfaction (United States Government Accounting Office [U.S. GAO] 1993; VanDeusen Lukas et al. 2004). Most importantly, delayed access to health care is assumed to negatively affect health outcomes due to delays in diagnosis and treatment (Kenagy, Berwick, and Shore 1999; Institute of Medicine 2004). For these reasons, the IOM's Committee on the Quality of Health Care in America (2004) chose reducing delays for health care as one of six aims to improve the quality of America's health care system. However, despite the declared importance of ensuring timely access to care, little research has actually examined the empirical association between waiting for outpatient care and health outcomes.
The lack of empirical research on wait times and health outcomes is likely due to a lack of data on wait times. A commonly used definition of wait times for medical care is the time between when an appointment is requested and when the appointment is scheduled (U.S. GAO 2001; Center for Medicare and Medicaid Services [CMS] 2004). Estimates of how long individuals wait for medical appointments are largely based on self-reported survey data (e.g., Community Tracking Study [CTS], Medicare Current Beneficiary Survey) where patients are asked how long they had to wait for their most recent physician or outpatient clinic appointment (CMS 2004; Center for Studying Health Systems Change 2005). A few studies of specific specialties (e.g., dermatology) have measured wait times by contacting providers at a point in time and asking when the next available appointment for a new or established patient could be scheduled (Resneck, Pletcher, and Lozano 2004), but in general, health care systems have not systematically collected data on how long individuals wait for appointments.
The Veterans Affairs (VA) health care system is an important exception because it has invested substantial resources and effort into monitoring and decreasing wait times. In response to reports of long wait times, the VA implemented a policy that by 1998, 90 percent of veterans seeking care would be seen in both primary and specialty care within 30 days of the appointment request (U.S. GAO 2001). To help medical centers meet this goal, the VA began automatically extracting data from its outpatient scheduling system so that wait times could be easily monitored.
The VA has also implemented and evaluated policies to decrease wait times. In 2000, the VA began a nationwide initiative to implement the advanced access model for certain appointment types (e.g., primary care) (U.S. GAO 2001; VanDeusen Lukas et al. 2004). The advanced access model changes how appointments are scheduled by evaluating the supply of appointment availability relative to demand for appointments and adjusting scheduling procedures so that demand is met as soon as it is requested. Clinics work down the backlog of patients waiting for appointments and then attempt to see patients the same day appointments are requested. As all physicians have open slots in their schedule, patients see their regular physician, eliminating recheck appointments that result when a patient goes to a different clinician because of a long wait to see their regular clinician (Murray and Berwick 2003). In the VA, greater implementation of the advanced access model was significantly associated with decreased wait times in primary care, urology, and orthopedics but not in eye care, audiology, or cardiology, probably because the initiative was implemented later in the three latter types of appointments (VanDeusen Lukas et al. 2004). A limited number of case studies suggest this model can be implemented in a variety of health care settings outside of the VA. It has been found to decrease wait times in several different types of primary care settings, such as community health centers, outpatient departments of large urban teaching hospitals, and small fee-for-service practices (Murray et al. 2003; Gordon and Chin 2004).
This article makes use of the VA waiting time data and tests the assumption that long waits for appointments have a negative effect on health outcomes. Specifically, we examine the association between waiting for outpatient care and mortality.
METHODS
Study Population
The study population included VA patients 65 or older who visited at least one of three types of geriatric outpatient clinics during the 2001 federal fiscal year (FFY; October 2000 to September 2001). The three types of geriatric outpatient clinics are (1) geriatric primary care, (2) geriatric clinic and (3) geriatric evaluation and management. Appointments at geriatric outpatient clinics are focused on preventing, evaluating and managing illnesses and conditions that are specifically associated with aging (e.g., incontinence), featuring providers who are trained in the management of these conditions (Veterans Health Administration 2004). Therefore, by using geriatric outpatient clinic visits to select the study population we ensured that the sample was more frail and elderly than the general population. This sample was ideal for examining whether long wait times were associated with negative health outcomes because these patients ought to be particularly sensitive to variation in the timeliness of access to medical care.
Waiting Time Data
We hypothesized that individuals who wait longer for medical care are at an increased risk of experiencing negative health outcomes. Thus, the main explanatory variable of interest was the average wait until the next available appointment at a VA facility. The VA keeps monthly data on the average number of days between the request for an appointment and when the appointment is actually scheduled. Services in the VA can be provided at a parent station, such as a medical center, or a sub-station, such as a community-based outpatient clinic, which organizationally operates under a parent station. Wait times are kept for each type of clinic appointment (e.g., urology, primary care, and laboratory) within a parent station and for all clinic appointments at sub-stations under a parent station. To create a performance measure for tracking wait times, the VA aggregates wait times by appointment type up to the parent station level on a monthly basis using a weighted average (Baar 2005b).1 For FFY 2001, wait time data are available for November 2000 and January to September 2001 but are missing for October and December 2000.
Although, there are data available on all types of appointments, the VA focuses on the wait times for 49 types of appointments to monitor how quickly parent stations are providing appointments to patients. These 49 clinic appointment types are used because they are (1) appointment types with high volumes, (2) appointment types that cover 93 percent of office-based patient-provider interactions in the VA (versus other services, such as labs or telephone consultations) and (3) appointment types that represent all major sub-specialties of medicine (e.g., mental health, orthopedics; Baar 2005a). Our wait time measure was based on these 49 appointment types in addition to appointments in a geriatric clinic or for geriatric evaluation and management because the study population was based on visiting a geriatric outpatient clinic (49+2 = 51 appointment types). Note that geriatric primary care was already included as one of the 49 appointment types.
If no appointments were requested as next available within a month for a certain type of clinic appointment, the wait time is missing. These wait times were imputed with zero under the assumption that if no next available appointments were requested, individuals could use these services right away.2 Clinic types missing 20 percent or more of their wait time data were excluded because they would require a large amount of zeroes to be imputed if these clinics were included. These clinic types include opioid substitution, speech pathology, radiation therapy treatment, recreational therapy services, and intensive substance abuse treatment for a final total of 46 appointment types (51–5 = 46).3
Individual-Level Wait Times
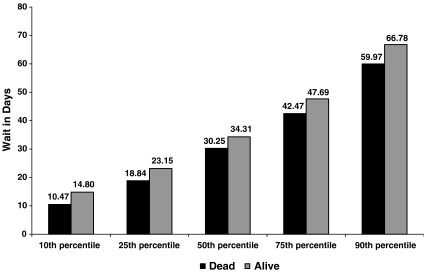
Data are available on the date, the facility, and the appointment type used by each patient in the study population. Thus, it was tempting to calculate a wait time measure based on services each individual actually used in 2001 and to associate this measure with health outcomes. This approach is problematic, however, because unobserved individual health status differences are likely to affect individual wait times as well as outcomes, confounding any attempt to study the effect of wait times on outcomes. To illustrate the problem we averaged together the wait times in days for all types of clinic visits made by an individual between July and September 2001.4Figure 1 shows the distribution of these individualized wait times by mortality status between July and September 2001. Those who died had consistently shorter individualized wait times. For example, the mean individualized wait in days for those who died was significantly lower at 33.4 days compared with 38.4 days for those who did not die (t = 4.45,p < 0.0001).
Figure 1.
Distribution of Individual-Level Wait Times between July 1, 2001 and September 30, 2001 by Mortality Status (n = 33,043)*.
*Individualized wait times were calculated by averaging together the wait times in days for all types of clinic visits made by an individual between July 1, 2001 and September 30, 2001.4 Three hundred and seventy-four individuals died in this time period.
The finding that those who died had shorter individualized wait times can likely be explained by a triage effect. Medical providers identify those who are in poorer health when calling to request an appointment and refer these patients to clinics with shorter waits. Thus, individual health status is affecting individualized wait time and potentially obscuring the effect of wait times on health status. Although statistical controls for observable differences in health status will reduce the severity of this problem, we are not able to measure health status precisely enough to eliminate it. Consequently, to properly isolate the effect of waiting on outcomes we calculated a wait time that is exogenous to the individual (not affected by prior individual health status).
Exogenous Wait Time Measure
To calculate wait times at the parent-station level that were exogenous to the individual we set out to construct a wait time that would apply to the same “representative” patient at all stations, eliminating the simultaneous effect of unmeasured prior individual health status on both wait time and outcome. We computed the proportion of each type of the 46 clinic appointments used by the entire sample between October 2000 and June 2001.5 For each month, this proportion was multiplied by the wait in days for each type of appointment at a parent station, and these products were summed for all appointment types in the parent station. Multiplying the wait time for an appointment type by its proportion in the whole sample gives greater weight to the wait times of appointment types that were used more frequently by the sample. An example of this wait time calculation is given in Appendix A. All individuals who visited the same parent station were assigned the same exogenous wait time in each month. Therefore, wait times could vary only between parent stations and over time.
Sample Selection
A second way that prior unobserved health status could affect both waiting times and outcomes is through sample selection. If, for example, facilities with relatively long wait times attract fewer severely ill patients (because they choose to go elsewhere rather than wait), then long wait times could be associated with relatively favorable outcomes because of unobserved and uncontrolled casemix differences. One way to address this problem is to separate in time the selection of the sample and the measurement of outcomes. For example if the sample were selected 5 years ago and the outcome were measured today, we could study the effect of recent waiting times on outcomes without worrying that sample selection might be correlated with either one. Waiting times might have been related to sample selection 5 years ago, but the distribution of waiting times would have changed enough over time to break any link between selection and current waiting time, leaving the relationship between current waiting time and outcome to be measured free of bias. Unlike in the example, our data would not support selecting the sample 5 years before the outcome. However, we were able to separate in time the selection of the study sample (October 2000–June 2001), the computation of wait times (July–September 2001), and the assessment of outcomes (October 2001–March 2002).6 Wait times changed substantially in this amount of time. The correlation between average parent station wait times during the first third of the year (January–March) and the last third (July–September) was only 0.60.
The study population consisted of patients who (1) visited a geriatric outpatient clinic between October 2000 and June 2001 and (2) survived through September 2001. Patients could only enter the sample through June 30, 2001. Facility-level exogenous wait times (discussed in the previous section) from the following 3 months (July, August, and September 2001) were averaged together to produce our measure of wait times. Finally, for each patient we calculated the odds of dying between October 1, 2001 and March 31, 2002 (the next 6 months) as the outcome.7
Therefore, there is one observation per person in our model. Each individual is assigned the 3-month average facility-level wait time for the facility they visited in 2001. Individuals who visited more than one parent station and would have had more than one wait time were excluded from the sample (n = 1,823, 5 percent of the sample). The final sample size is 37,489.
Risk Adjustment
Models were risk adjusted to control for observable differences in prior individual health status based on similar models in the literature (Berlowitz et al. 1997; Porell et al. 1998; Mukamel and Spector 2000; Selim et al. 2002). Explanatory variables include age, gender, principal diagnoses, and the Charlson index as a measure of the number and seriousness of comorbid conditions (Charlson et al. 1987; Deyo, Cherkin, and Ciol 1992).8 Diagnosis codes from VA inpatient encounters in the 365 days before the date of each patient's first geriatric clinic visit were grouped according to the classification system developed by Rosen et al. (2000). Some of the diagnosis categories developed by Rosen et al. (2000) overlap with diagnosis categories used in the Charlson index. We ran models that only included either the Charlson index or the diagnosis categories as a test for collinearity. Results were similar so both measures were included.
Models also included indicators for preventable hospitalization in the 365 days before the first observed geriatric visit (Agency for Healthcare Research and Quality 2001) and for 50 percent or greater service-connected disability.9 These two variables are included as further measures of prior individual health status. Veterans with a 50 percent or more service-connected disability rating are likely in poorer health, and veterans experiencing a preventable hospitalization in the prior year likely have poorer management of health conditions.10 Finally, to control for differences in case mix between facilities, a historical 3-month average mortality rate (October–December 2000) per facility was included as an explanatory variable. Facilities that generally treated patients with a greater burden of illness would be expected to have higher mortality rates.
Outcome
The outcome of interest is mortality. Death dates are reported in the VA National Patient Care Database (NPCD), the Beneficiary Identification and Record Locator Subsystem (BIRLS) file, or in the Medicare Denominator file. For those without dates of death, their status as “alive” was confirmed by checking NPCD utilization records in subsequent periods. Ninety-six percent of cases were confirmed in this manner, and the rest are excluded from the analysis. Death dates were confirmed through March of 2002, which is 6 months after the end of FFY 2001.
Analyses
Data were analyzed using STATA 8.0 (Statacorp 2003). We report results from a random effects logistic regression model that predicts the odds of dying. This model included individual-level risk adjustment measures and a lagged facility-level mortality rate. To account for heteroskedasticity, a random effect at the facility level was included. In the random effects logistic regression model presented, wait time was dichotomized into < and ≥31 days.
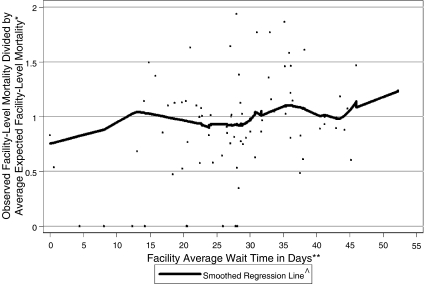
Two analyses led us to dichotomize the wait time. First, we graphically examined the relationship between continuous wait time and facility-level mortality. We calculated the ratio of observed facility level mortality rate to the average expected risk-adjusted facility-level mortality rate. In this ratio, the numerator was the number who died at each station divided by the number who visited each station (observed). For the denominator, we predicted the probability of dying for each individual by using all of the risk adjustors (e.g., historical facility-level mortality rates, age, Charlson index) except wait time. This probability was averaged for all individuals in a facility to get the average expected facility-level risk-adjusted mortality rate (Figure 2).
Figure 2.
Ratio of Observed Facility-Level Mortality Rates to Expected Facility-Level Mortality Rates by Wait Time, Weighted by Individuals (n = 37,489)
*In the y-axis, the observed facility-level mortality rate was the number of individuals who died at each VA facility over the number of individuals who visited each VA facility (numerator). For the denominator, we predicted mortality rates by the individual risk adjustors and for each individual we predicted the probability of dying. This probability was averaged for all individuals in a facility to get the average expected facility-level risk-adjusted mortality rate. **Wait times for each facility between July and September 2001 were averaged together. ^All individual-level data points were used to compute the smoothed regression line. However, to highlight the regression line, we excluded from the figure points where this ratio was > 2 (n = 524; 1.3 percent). The smoothed regression line was calculated using lowess smoothing (lowess command in STATA) with a bandwidth of 0.4.
Therefore, facilities with observed mortality rates higher than the expected mortality rates will have a ratio > 1, and facilities with lower observed mortality rates compared with the expected mortality rates will have a ratio < 1.11 The graph also includes a smoothed regression line of the values in the scatterplot, locally weighted by the number of patients associated with each facility. This regression line increases gradually as wait times increase. However, the smoothed regression line generally stays above 1 at wait times of 31 days or more indicating that the observed mortality is greater than the expected mortality at these waits (Figure 2).
In the second analysis, we used a heteroskedastic probit model to predict the probability of dying. Clinics with fewer observations had greater residual variance, and a function of the natural log of the number of observations per clinic was found to explain this heteroskedacity well (Greene 1993). First, we included wait time as a linear function and this significantly predicted the probability of dying as seen in Appendix B. However, the linear function of wait time may not be the best way to characterize the relationship as there appeared to be a step function after 30 days in Figure 2. Therefore, we categorized the 3-month average wait time into < 26, 26.00–28.59, 28.60–31.99, 32.00–40.99, and ≥41 days, which are approximately quintiles, and predicted the probability of dying. In this model, which is presented in Appendix C, veterans with wait times of 32 days or greater had a higher probability of dying than veterans who visited facilities where the wait time was < 32 days. As these results provided evidence of a step function, we then tested several alternative dichotomizations: 30, 30.5, 31, 31.5, and 32 days. A significant increase in the probability of dying was found at 31 days or more. To simplify the presentation and interpretation of results, we tested the same dichotomization of wait times in the random effects logistic regression. Results were qualitatively similar so we present results as odds ratios from the random effects logistic regression.
Sensitivity Analyses
To check the robustness of the results, we ran several sensitivity tests. First we excluded all clinic appointment types where > 10 percent of the wait time data was missing (n = 9 clinic types). Second, as a sensitivity test of the weighting used in the exogenous wait time measure, we averaged together all wait times for all clinic appointment types reported by a parent station in a month. Thus, each appointment type had an equal weight in the wait time calculation. For both of these wait time measures, the wait time distribution was split into quintiles and the probability of dying was predicted with a heteroskedastic probit. Results are qualitatively similar and are available from the authors upon request.
RESULTS
Of the 153 VA medical centers with wait time data, 89 had patients that visited a geriatric outpatient clinic in FFY 2001. The median wait time in days varies between 26.0 and 31.4 days between January and September 2001. There is slight seasonal variation with wait times generally peaking between February and April and decreasing through the summer months. However, most of the variation in wait times appears to be between facilities. There is at least a 20-day difference in each month between parent stations with wait times in the 10th percentile and the 90th percentile (see Appendix D).
Table 1 gives the descriptive statistics for the geriatric sample, which is elderly, predominantly male and in generally poor health. Ninety-seven percent of the sample was male, and the mean age was 78 years. Twelve percent of the sample had a service-connected condition that was rated as 50 percent or more disabling. About a third of the patients had endocrine disease, neurological disease, psychiatric disease, or sensory disease and about 20 percent of the sample had cancer or pulmonary disease. Eighty-two percent of the sample had been diagnosed with heart disease. The average patient in the sample was diagnosed with almost three of these disease categories, and the mean rating on the Charlson comorbidity index was 0.73. Seven percent of the sample had experienced a preventable hospitalization in the previous year. Finally, four percent of the sample died within 6 months following September 2001.
Table 1.
Individual Characteristics of Sample That Visited a Geriatric Outpatient Clinic, 2001 (n = 37,489)
| Independent Variables | Percent or Mean (Standard Deviation) |
|---|---|
| Male | 97.40 |
| Age | 78.35 (5.78) |
| Experienced a preventable hospitalization in year before geriatric clinic visit | 6.83 |
| Had a ≥50 percent service-connected disability | 12.06 |
| Charlson index score | 0.73 (1.63) |
| Diagnosed with cancer | 19.39 |
| Diagnosed with endocrine disease | 31.41 |
| Diagnosed with heart disease | 82.46 |
| Diagnosed with neurological disease | 31.41 |
| Diagnosed with psychiatric disease | 31.47 |
| Diagnosed with pulmonary disease | 19.62 |
| Diagnosed with sensory disease | 32.00 |
| Diagnosed with muscular disease | 11.92 |
| Diagnosed with other disease | 16.23 |
| Number of disease categories | 2.76 (1.47) |
| Outcome measure | |
| Died in 6-month follow-up period | 3.88 |
Figure 2 shows the scatterplot of the ratio of facility-level observed to expected mortality by continuous wait time with the smoothed regression line. As wait times increase the regression line predicting the ratio of observed to expected mortality also increases. The smoothed regression line generally stays above 1 at wait times of 31 days or more indicating a greater proportion of patients died in these facilities than was expected.
The top section of Table 2 shows the odds ratios, standard errors, and p-values for the random effects logistic regression model explaining the odds of dying within 6 months after September 30, 2001. Veterans who visited a facility with a 3-month average wait of 31 days or more were 21 percent more likely to die compared with veterans who visited a facility with a 3-month average wait of < 31 days. Other explanatory variables to control for facility-level case mix and individual health status have the expected effects on mortality. Females were significantly less likely to die than males. Age and the Charlson index of comorbidity both had a significant positive association with the likelihood of dying. As well, individuals with a 50 percent or more service-connected disability, individuals experiencing a preventable hospitalization in the prior year, and individuals diagnosed with cancer, endocrine disease, neurological disease, psychiatric disease, pulmonary or other disease in the prior year had significantly higher odds of dying compared with individuals with less than a 50 percent service-connected disability, individuals who had not experienced a preventable hospitalization, and individuals who were not diagnosed with each of these diseases.
Table 2.
Random Effects Logistic Regression Predicting 6-Month Mortality in 2001 (n = 37,489)
| Independent Variables | Odds Ratio | Standard Error | Z | P value |
|---|---|---|---|---|
| Facility average wait time ≥31 days (ref. < 31 days)* | 1.21 | 0.1042 | 2.20 | .027 |
| Facility average mortality rate per 1,000† | 1.02 | 0.0080 | 1.90 | .058 |
| Female (ref. = male) | 0.64 | 0.1309 | −2.18 | .029 |
| Age | 1.05 | 0.0051 | 10.50 | < 0.001 |
| Preventable hospitalization (ref. = no)‡ | 1.65 | 0.1387 | 5.94 | < 0.001 |
| ≥50% service-connected disability (ref. = no) | 1.36 | 0.0997 | 4.22 | < 0.001 |
| Charlson Index | 1.07 | 0.0168 | 4.32 | < 0.001 |
| Cancer (ref. = no)§ | 1.48 | 0.1535 | 3.74 | < 0.001 |
| Endocrine disease (ref. = no) | 1.22 | 0.1241 | 1.96 | .050 |
| Heart disease (ref. = no) | 1.00 | 0.1126 | 0.04 | .967 |
| Neurological disease (ref. = no) | 1.91 | 0.1901 | 6.50 | < 0.001 |
| Psychiatric disease (ref. = no) | 1.26 | 0.1288 | 2.26 | .024 |
| Pulmonary disease (ref. = no) | 1.68 | 0.1775 | 4.88 | < 0.001 |
| Sensory disease (ref. = no) | 0.95 | 0.0995 | −0.45 | .655 |
| Other disease (ref. = no) | 1.43 | 0.1561 | 3.28 | .001 |
| Number of disease categories | 0.93 | 0.0768 | −0.91 | .361 |
| Alternative dichotomizations of wait time¶ | ||||
| Facility average wait time ≥30 days (ref. < 30 days)a | 1.14 | 0.0990 | 1.47 | .142 |
| Facility average wait time ≥30.5 days (ref. < 30.5 days)b | 1.16 | 0.1007 | 1.70 | .090 |
| Facility average wait time ≥31.5 days (ref. < 31.5 days)c | 1.20 | 0.1030 | 2.07 | .038 |
| Facility average wait time ≥32 days (ref. < 32 days)d | 1.22 | 0.1048 | 2.37 | .018 |
Wait times for each facility between July and September 2001 were averaged together. The marginal effect from the heteroskedastic probit model was 0.0053,p-value = 0.034.
Mortality rates in each facility between October and December 2000 were averaged together.
Patients who had a preventable hospitalization or were diagnosed with each of the diseases within a year before his or her first geriatric clinic in FY2001 were categorized as yes.
Muscular disease was dropped due to collinearity with the other disease categories.
The same model was fit with different dichotomizations of wait times. All other variables gave qualitatively similar results to the 31 days or more versus < 31 days model.
The marginal effect from the heteroskedastic probit model was 0.0039,p-value = 0.119.
The marginal effect from the heteroskedastic probit model was 0.0041,p-value = 0.099.
The marginal effect from the heteroskedastic probit model was 0.0052,p-value = 0.035.
The marginal effect from the heteroskedastic probit model was 0.0058,p-value = 0.023.
The bottom section of Table 2 gives the odds ratio, standard errors, and p-values for the same random effects logistic regression model with the wait time variable dichotomized at several different points. The probability of dying increases as the dichotomization of wait time changes from 30 to 32 days and the effect becomes significant at 31 days.
DISCUSSION
To our knowledge, this is the first study to examine the association between waiting for outpatient care and mortality using administrative data. Longer waits for outpatient health care are associated with an increased risk of individual mortality even when controlling for prior individual health status and facility-level case-mix differences in this sample of geriatric veterans. Veterans who visited facilities with wait times of 31 days or more were significantly more likely to die within the 6-month follow-up period compared with veterans who visited facilities where the wait time was < 31 days (Table 2). In general, this research supports the VA's policy of limiting waits for outpatient care to 30 days or less. However, we also found a significant association between the linear form of wait time and the probability of dying (Figure 2 and Appendix B). Therefore, reducing wait times below 30 days may also decrease mortality in this population.
Wait time is not the strongest predictor of mortality in the model. Being diagnosed with a variety of conditions (e.g., pulmonary disease; neurological disease), experiencing a preventable hospitalization, or having a 50 percent or greater service-connected disability all had larger effects on mortality. As one would expect, individual health status plays a primary role in determining an individual's mortality. Nonetheless, wait time has a significant association with mortality and can be addressed through changes in health care policy. For example, several studies have found that wait times can be shortened by implementing the Advanced Clinic Access model (Murray et al. 2003; Gordon and Chin 2004; VanDeusen Lukas et al. 2004). Therefore, the association between wait times and mortality in this population is important because there are known successful interventions to decrease wait times, which may then influence mortality.
Extensive future research is needed to determine whether the relationship between wait times and mortality exists in healthier patient populations and other health care settings. Veterans who use the VA tend to be older, sicker and be diagnosed with more diseases than veterans nationally and the general U.S. population (Kazis et al. 1999). Patients with chronic diseases may be especially vulnerable to long waits in care because these waits could delay diagnosis of chronic conditions, making them harder to manage and resulting in negative health effects that could have been avoided if individuals had been getting access to timely health care. Healthier patient populations are not likely to face the same risks when waiting for health care.
Wait times in this study may also be a proxy for poor quality of care at certain facilities. Facilities that have consistent waits of 30 days or more may be poorly managed in other ways, and this poor management may affect patient health, such as through patient safety errors. In future work, we hope to include both facility quality of care characteristics and wait times in the same model to see if the effect of wait times remains.
However, if longer waits are associated with poorer health outcomes in patient populations outside of the VA, there is cause for concern in recent trends. Self-reported data from the CTS suggest that wait times have been increasing among the Medicare population. In 2001, 37 percent of elderly Medicare beneficiaries waited > 21 days for a check-up compared with 32 percent in 1997. Similarly, forty percent of elderly Medicare beneficiaries waited > 1 week for an appointment to address a specific illness compared with 35 percent in 1997 (Trude and Ginsburg 2002). The privately insured near elderly (aged 55–64) also experienced significant increases in the average number of days they waited for both check-ups and illness-related appointments between 1997 and 2003 (Trude and Ginsburg 2005). The near elderly are more likely to suffer from chronic conditions (e.g., diabetes) than younger individuals (National Center for Health Statistics 2004).
More extensive research is also needed on the causes of long wait times. The advanced access model argues that long waits for appointments are often due to inefficient scheduling of patient appointments and provides concrete ways to meet the demand for appointments. This model will be successful as long as the physician capacity to schedule appointments is in balance with the demand for appointments (Murray and Berwick 2003). Thus, a greater understanding is needed of the factors beyond scheduling procedures that influence physician capacity and patient demand. For example, findings from studies focused on dermatologists found female dermatologists had significantly longer waits, perhaps because female physicians work fewer hours per week than their male counterparts and patients are willing to wait longer in order to see a female provider. As well, these studies have found the supply of physicians and Medicare and Medicaid reimbursement levels in an area affect how long patients wait for appointments (Suneja et al. 2001; Resneck, Pletcher, and Lozano 2004). In contrast, findings from the CTS suggest that the 2002 reduction in Medicare physician reimbursement rates did not affect wait times because wait times increased for the privately insured nonelderly as well as Medicare seniors (Trude and Ginsburg 2002). Further studies of the causes of long wait times may be needed before effective policies can be designed to shorten them.
An important limitation of this work is that we only have VA utilization data and we do not know how health care use outside of the VA affects the results. By separating in time the selection of the sample from the measurement of the independent variable we have reduced the danger of selection bias, but we have not eliminated it. In future research, we hope to formally model the process by which veterans choose among VA and non-VA options. If we are successful, we will be able to more fully correct future estimates for possible selection bias.
Findings from this study support the idea that U.S. health care policy makers should be concerned about delays in accessing care and the potential negative effects on health. If the association found in this study is replicated in future work, the health of patients ought to improve if health care systems begin to monitor wait times and work to reduce them where necessary. Because the VA has already undertaken this task, it can provide valuable lessons to other health care systems facing the same challenge.
Acknowledgments
Salary support for Dr. Prentice was provided by a Health Services Research Fellowship from the Center for Health Quality, Outcomes and Economic Research in the Department of Veterans Affairs. Additional support was provided under Grant No. IIR-04-233-1 from the Department of Veterans Affairs, Health Services Research & Development Service.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs.
NOTES
For ease of presentation, “facility” and “parent station” are used interchangeably throughout the paper to refer to a VA parent station.
The exception to this is intensive substance abuse treatment. After consulting with VA officials, we learned that veterans either get services right away or are referred elsewhere but appointments are not usually scheduled. This explains the large percentage of missing wait-time data (48 percent) for this clinic stop. This clinic type was excluded from the wait time measure.
In the final sample, 11 percent of the clinic appointments were imputed with 0.
Note this is still not the actual time individual patients waited for appointments. The VA averages together the individual wait times and reports an average wait for the entire parent station for each appointment type. We averaged together this parent station-level wait time for all clinic appointments used by each individual.
Only 34 percent of the clinic visits in the entire sample were to a geriatric outpatient clinic. Thus, the sample used a wide range of health care services beyond geriatric outpatient clinics.
The standard correction for selection bias involves estimating a first-stage selection model and explicitly accounting for the expected value of the disturbance term from that model in the second stage equation of interest. Because we do not have veterans in our sample who chose not to come to a VA medical center for care, we cannot take this approach.
A potential disadvantage of separating the sample selection period from the wait time measurement is that individuals might not have used outpatient services during the wait time measurement period. For example, the health of some individuals might have declined after they entered the sample and they might have been in a nursing home during the 3 month period when wait times were measured. If this were the case then outpatient wait times ought not to affect their outcomes and our analysis would be inappropriate for this group. A few simple tabulations of our data suggest that this is not a serious problem. Eighty percent of the sample had at least one clinic visit during the wait time measurement period. The 20 percent that did not have a visit had lower mortality rates in the 6 month follow-up period compared to individuals who had a clinic visit (4.38 percent versus 5.24 percent, respectively) suggesting that the lack of clinic visits may have been due to better health and consequently a reduced need for clinic visits. The lack of a clinic visit does not imply that differences in wait times would have no effect on outcomes provided the group in question is not institutionalized. For example, a patient might not have a visit because the wait time was high, and the health consequences could be serious.
Following previous work (e.g.,Selim et al. 2002), the Deyo, Cherkin and Ciol (1992) translation of the original Charlson index that identifies conditions by ICD-9-CM codes was used. Conditions were weighted using the original Charlson weighting system (Charlson et al. 1987).
Service-connected disability is a condition or disability that the VA has determined was incurred in or aggravated by military service.
The inclusion of previous preventable hospitalizations in the model also controls for differences in parent station quality that are independent of parent station wait times. All preventable hospitalizations developed by AHRQ were included except for those ntended for pediatric populations. Please refer to AHRQ (2001) for a complete list of these preventable hospitalizations.
Note that model misspecification and measurement error can also cause this ratio to deviate from 1.
Supplementary material
The following supplementary material for this article is available online:
Example of Wait Time Calculation.
Marginal Effects, Standard Errors, and p-Values of a Heteroskedastic Probit Model with Linear Wait Time Predicting Six Month Mortality, 2001 (n537,489).
Marginal Effects, Standard Errors, and p-Values of a Heteroskedastic Probit Model with Categorized Wait Time Predicting Six Month Mortality, 2001 (n537,489).
Distribution of Wait Times across Months and Parent.
REFERENCES
- Agency for Healthcare Research and Quality. AHRQ Quality Indicators-Guide to Prevention Quality Indictors: Hospital Admission for Ambulatory Care Sensitive Conditions. AHRQ Publication No. 02-R0203. Rockville, MD: Agency for Healthcare Research and Quality; 2001. [Google Scholar]
- Baar B. New Patient Monitor: Data Definitions. Veteran Health Administration Support Services Center; 2005a. [cited 2005 May 16]. Available at http://vssc.med.va.gov/WAITTIME/HELP/NEWPATIENTMONITORHELP.HTM. [Google Scholar]
- Baar B. Performance Wait Time Data Definitions. Veterans Health Administration Support Services Center; 2005b. [cited 2004 December 13]. Available at http://Klfmenu.med.gov/WAITTIME/HELP/CLINIC_PERFORMANCEHELP.HTM. [Google Scholar]
- Berlowitz DR, Brandeis GH, Anderson J, Du W, Brand H. Effect of Pressure Ulcers on the Survival of Long-Term Care Residents. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences. 1997;52(2):M106–10. doi: 10.1093/gerona/52a.2.m106. [DOI] [PubMed] [Google Scholar]
- 2001 Community Interview: Access to Care. Baltimore: Center for Medicare and Medicaid Services; 2004. Center for Medicare and Medicaid Services (CMS); Research Development and Information: Information and Methods Group. [Google Scholar]
- Community Tracking Study: Household Survey Instrument 2003 (Round Four) Washington, DC: Center for Studying Health System Change; 2005. Center for Studying Health Systems Change. [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. Journal of Chronic Disease. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, Clancy CM, Cohen JW, Wilets M. The Use of Hospital Emergency Departments for Non-Urgent Health Problems: A National Perspective. Medical Care Research and Review. 1995;52:453–74. doi: 10.1177/107755879505200402. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Greene WH. Econometric Analysis. 2. Upper Saddle River, NJ: Prentice-Hall; 1993. [Google Scholar]
- Gordon P, Chin M. Achieving a New Standard in Primary Care for Low-Income Populations: Case Studies of Redesign and Change through a Learning Collaborative. New York: The Commonwealth Fund; 2004. [Google Scholar]
- Institute of Medicine (IOM): The Committee on the Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine; 2004. [Google Scholar]
- Kazis LE, Ren XS, Lee A, Skinner K, Rogers W, Clark J, Miller DR. Health Status in VA Patients: Results from the Veterans Health Study. American Journal of Medical Quality. 1999;14(1):28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- Kenagy JW, Berwick DM, Shore MF. Service Quality in Health Care. Journal of the American Medical Association. 1999;281(7):661–5. doi: 10.1001/jama.281.7.661. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD. Nursing Home Costs and Risk-Adjusted Outcome Measures of Quality. Medical Care. 2000;38(1):78–89. doi: 10.1097/00005650-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Murray M, Berwick DM. Advanced Access: Reducing Waiting and Delays in Primary Care. Journal of the American Medical Association. 2003;289:1035–40. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- Murray M, Bodenheimer T, Rittenhouse D, Grumbach K. Improving Timely Access to Primary Care: Case Studies of the Advanced Access Model. Journal of the American Medical Association. 2003;289(8):1042–6. doi: 10.1001/jama.289.8.1042. [DOI] [PubMed] [Google Scholar]
- Health, United States, 2004, with Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2004. National Center for Health Statistics. [PubMed] [Google Scholar]
- Porell F, Caro FG, Silva A, Monane M. A Longitudinal Analysis of Nursing Home Outcomes. Health Services Research. 1998;33(4):835–65. [PMC free article] [PubMed] [Google Scholar]
- Resneck J, Jr, Pletcher MJ, Lozano N. Medicare, Medicaid, and Access to Dermatologists: The Effect of Patient Insurance on Appointment Access and Wait Times. Journal of the American Academy of Dermatology. 2004;50:85–92. doi: 10.1016/s0190-9622(03)02463-0. [DOI] [PubMed] [Google Scholar]
- Rosen A, Wu J, Chang BH, Berlowitz D, Ash A, Moskowitz M. Does Diagnostic Information Contribute to Predicting Functional Decline in Long-Term Care? Medical Care. 2000;38(6):647–59. doi: 10.1097/00005650-200006000-00006. [DOI] [PubMed] [Google Scholar]
- Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, Cong Z, Lee A, Kazis L. Risk-Adjusted Mortality Rates as a Potential Outcome Indicator for Outpatient Quality Assessments. Medical Care. 2002;40(3):237–45. doi: 10.1097/00005650-200203000-00007. [DOI] [PubMed] [Google Scholar]
- Shesser R, Kirsch T, Smith J, Hirsch R. An Analysis of Emergency Department Use by Patients with Minor Illness. Annals of Emergency Medicine. 1991;20(7):743–8. doi: 10.1016/s0196-0644(05)80835-2. [DOI] [PubMed] [Google Scholar]
- StataCorp. STATA (Release 8.0) Statistical Software. College Station, TX: StataCorp; 2003. [Google Scholar]
- Suneja T, Smith ED, Chen GJ, Zipperstein KJ, Alan J, Fleischer B, Feldman SR. Waiting Times to See a Dermatologist Are Perceived as Too Long by Dermatologists. Archives of Dermatology. 2001;137:1303–7. doi: 10.1001/archderm.137.10.1303. [DOI] [PubMed] [Google Scholar]
- Trude S, Ginsburg P. Growing Physician Access Problems Complicate Medicare Payment Debate. Washington, DC: Center for Studying Health System Changes; 2002. [cited 2005 June 15]. Available at http://hschange.org/CONTENT/466/466/pdf. [PubMed] [Google Scholar]
- Trude S, Ginsburg PB. An Update on Medicare Beneficiary Access to Physician Services. Washington, DC: Center for Studying Health System Change; 2005. [cited 2005 June 15]. Available at http://hschange.org/CONTENT/731/731/pdf. [PubMed] [Google Scholar]
- VA Health Care: Restructuring Ambulatory Care System Would Improve Services to Veterans. Washington, DC: United States General Accounting Office: GAO/HRD94-4; 1993. United States Government Accounting Office (U.S. GAO) [Google Scholar]
- More National Action Needed to Reduce Waiting Times, but Some Clinics Have Made Progress. Washington, DC: United States General Accounting Office. GAO-01-953; 2001. United States Government Accounting Office (U.S. GAO) [Google Scholar]
- VanDeusen Lukas C, Meterko M, Mohr D, Seibert MN. The Implementation and Effectiveness of Advanced Clinic Access. Boston: Health Services Research and Development Management Decision and Research Center, Office of Research and Development, Department of Veterans Affairs; 2004. [Google Scholar]
- Veterans Health Administration (VHA); Decision Support Office. 2004. [cited 2005 January 15]. “Summary of Active Stop Codes; Reference I.”. Available at http://vaww.dss.med.va.gov/programdocs/pd_oident.asp. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Example of Wait Time Calculation.
Marginal Effects, Standard Errors, and p-Values of a Heteroskedastic Probit Model with Linear Wait Time Predicting Six Month Mortality, 2001 (n537,489).
Marginal Effects, Standard Errors, and p-Values of a Heteroskedastic Probit Model with Categorized Wait Time Predicting Six Month Mortality, 2001 (n537,489).
Distribution of Wait Times across Months and Parent.