Abstract
Objectives
To review estimates of U.S. nurse supply and demand, document trends in nurse immigration to the United States and their impact on nursing shortage, and consider strategies for resolving the shortage of nurses in the United States without adversely affecting health care in lower-income countries.
Principal Findings
Production capacity of nursing schools is lagging current and estimated future needs, suggesting a worsening shortage and creating a demand for foreign-educated nurses. About 8 percent of U.S. registered nurses (RNs), numbering around 219,000, are estimated to be foreign educated. Eighty percent are from lower-income countries. The Philippines is the major source country, accounting for more than 30 percent of U.S. foreign-educated nurses. Nurse immigration to the United States has tripled since 1994, to close to 15,000 entrants annually. Foreign-educated nurses are located primarily in urban areas, most likely to be employed by hospitals, and somewhat more likely to have a baccalaureate degree than native-born nurses. There is little evidence that foreign-educated nurses locate in areas of medical need in any greater proportion than native-born nurses. Although foreign-educated nurses are ethnically more diverse than native-born nurses, relatively small proportions are black or Hispanic. Job growth for RNs in the United States is producing mounting pressure by commercial recruiters and employers to ease restrictions on nurse immigration at the same time that American nursing schools are turning away large numbers of native applicants because of capacity limitations.
Conclusions
Increased reliance on immigration may adversely affect health care in lower-income countries without solving the U.S. shortage. The current focus on facilitating nurse immigration detracts from the need for the United States to move toward greater self-sufficiency in its nurse workforce. Expanding nursing school capacity to accommodate qualified native applicants and implementing evidence-based initiatives to improve nurse retention and productivity could prevent future nurse shortages.
Keywords: Nurse migration, U.S. immigration
The United States plays a pivotal role in the global migration of nurses. It has the largest professional nurse workforce of any country in the world, numbering almost 3 million in 2004 (USDHHS 2006). The United States has almost one-fifth of the world's stock of professional nurses and about half of English-speaking professional nurses. With a nurse labor force of this size, even modest supply–demand imbalances exert a strong pull on global nurse resources. A looming projected shortage of nurses in the United States that could reach 800,000 by 2020 (USDHHS 2002) is thus cause for concern among other countries also experiencing nurse shortages.
The United Kingdom has been more in the spotlight in recent years than the United States regarding its international nurse recruitment policies and practices because, at one point, nurse migrants outnumbered domestically educated nurses among nurses entering the U.K. workforce (Aiken et al. 2004; Ross, Polsky, and Sochalski 2005). However, the United Sates recently became the world's largest importer of nurses, with almost 15,000 foreign-educated nurses passing the licensing exam for registered nurses (RNs) in 2005 (National Council on State Boards of Nursing [NCSBN] 2006), compared with an estimated 13,000 foreign-educated nurses entering the United Kingdom (see Buchan 2007). Moreover, economic constraints in the National Health Service in the United Kingdom have recently limited immigration, while demand for nurses in the United States continues to grow. Altogether in 2000, just over 300,000 U.S. nurses were foreign born. After taking into account foreign-born nurses who immigrated before the age of 22, and thus probably received their nursing education in the United States, close to 219,000 nurses currently residing in the United States are estimated to have received their nursing education abroad, constituting close to 8 percent of the nation's RN stock (Table 1).
Table 1.
Registered Nurses by Nativity and Citizenship Status, U.S. 2000
| Frequency | % All RNs | |
|---|---|---|
| Born in the United States or Territories | 2,369,185 | 88 |
| Born abroad of American parent | 18,249 | 1 |
| Immigrated before age 21 | 83,807 | 3 |
| U.S. citizen by naturalization (immigration age 21+) | 124,968 | 5 |
| Not a U.S. citizen (immigration age 21+) | 93,752 | 3 |
| Estimated number of foreign-educated RNs | 218,720 | 8 |
Source: Author's calculation from the U.S. Department of Commerce, Bureau of the Census, Census of Population and Housing (2000), Public Use Micro data, 1% sample.
RNs, registered nurses.
The United States is the destination of choice for many migrating nurses from both developed and lower-income countries because of high wages, opportunities to pursue additional education, and a high standard of living (Kingma 2006). Nurses do not emigrate from the United States in substantial numbers or permanently. The prolonged recent nurse shortage and the large shortage projected for the future have motivated more aggressive nurse recruitment abroad by hospital employers and commercial recruiting firms (Brush, Sochalski, and Berger 2004). Almost 34,000 foreign-educated nurses took the NCLEX-RN registered nurse license exam in 2005, with 44 percent passing the exam, suggesting a great deal of interest among foreign-educated nurses in working in the United States (NCSBN 2006). Increasingly, physicians and others in developing countries are retraining as nurses because of the potential opportunities for migration. Since 2000, 3,500 Filipino doctors have retrained as nurses and left for nurse jobs abroad, and 4,000 Filipino doctors are currently in nursing schools.
This paper (1) examines trends and projections in the U.S. RN workforce; (2) reviews recent trends in nurse immigration; (3) explores the extent to which nurse immigration contributes to national health care workforce goals, including diversity and care of underserved populations; and (4) considers policy options that could contribute to solving nurse shortages in the United States, while minimizing adverse impact on global human resources for health.
ESTIMATED NEED FOR RNS IN THE UNITED STATES
An estimated 703,000 new jobs for RNs will be created between 2004 and 2014; RNs are second among the top 10 occupations with the largest job growth (U.S. Department of Labor, Bureau of Labor Statistics 2005http://www.bls.gov/news.release/ecopro.t06.htm). The average age of RNs was 46.8 years in 2004, and has been increasing steadily since 1980 (USDHHS 2006). Some 478,000 nurses can be expected to retire between 2002 and 2012. New jobs plus retirements lead to predictions of 1.1 million additional nurses needed to be added to the stock of RNs between 2002 and 2012 to maintain a steady state. Meeting that target would require graduations of around 110,000 RNs a year between 2002 and 2012.
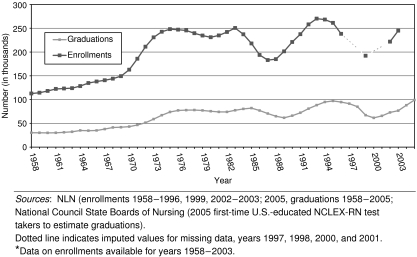
Figure 1 portrays the overall upward trend in nursing school enrollments and graduations since 1958, as well as cyclical increases and decreases. The increase in enrollments and graduations from 1965 to 1976 were associated with significant federal investments in nursing education over the decade, following the introduction of Medicare and Medicaid. Enrollments in nursing schools in the absence of federal subsidies have been very sensitive to market conditions for nurses. Applications to nursing schools declined for 6 consecutive years from 1995 through 2000 during a period of highly publicized nurse layoffs associated with employer adaptations to managed care. Graduations fell from over 95,000 in 1994 to below 70,000 by 2001, causing the domestic production of nurses to fall behind the 2012 target by about a cumulative total of 110,000 nurses between 2002 and 2005. Indeed, Buerhaus, Staiger, and Auerbach (2004) suggest that most of the increase in nurses over this period was from foreign-educated nurses and older nurses returning to the workforce.
Figure 1.
Graduations and Enrollments in Registered Nurse Programs, 1958–2005.*
The tight job market was short-lived, and escalating demand for nurses was associated with real wage growth of 12.8 percent between 2000 and 2004, the first significant upturn in real wages since 1988 (USDHHS 2006). The nursing school applicant pool grew in response to improved employment opportunities and increased wages. Graduations in 2003 were back to 73,000, and between 2003 and 2004 graduations increased by 26 percent to about 88,000 (NLN 2005), and to close to 99,000 in 2005 (NCSBN 2006). The applicant pool became so robust by 2004 that many qualified applicants for RN programs were turned away. The American Association of Colleges of Nursing reported that more than 30,000 applicants seeking baccalaureate education could not be accommodated and the National League for Nursing estimates that as many as 150,000 applicants were turned away from all nursing programs because of shortages of faculty, resources, space, and clinical education opportunities (AACN 2005; NLN 2005). While these estimates are possibly inflated by multiple applications, there is little doubt that the number of qualified applicants to nursing schools is much larger than the number of positions.
The single greatest challenge to expanding domestic production of RNs—a large, qualified applicant pool—is not presently a problem. If the large applicant pool can be sustained, and if most qualified applicants could be accommodated in nursing schools, it would be feasible to graduate most of the 125,000 nurses a year needed to meet projected future needs, assuming that nurses currently in the workforce could be retained until retirement age. To date, however, the federal response to the nurse shortage has been minimal, and employers have not been fully engaged in participating in efforts to increase the domestic supply of nurses.
TRENDS IN U.S. NURSE IMMIGRATION
Health care organizations in the United States have actively recruited professional nurses from abroad for more than 50 years in response to cyclical nurse shortages in hospitals and nursing homes (Brush and Berger 2002; Aiken et al. 2004). Until the early 1990s, the inflow of RNs trained abroad generally did not exceed 3,000–4,000 a year (Buerhaus, Staiger, and Auerbach 2004). Between 1994 and 2005, however, the annual number of foreign-educated nurses passing the NCLEX-RN exam tripled to almost 15,000 in 2005. Two concurrent factors shaped recent trends in nurse migration: changes in the demand for nurses in the hospital sector and changes in immigration policies.
Demand for nurses fell in the hospital sector in the early 1990s as health care organizations adapted to increased penetration of managed care and predictions of decreased inpatient days. Sixty percent of hospital CEOs reported reducing nurse staffing by attrition and layoffs, and use of supplemental and foreign-educated nurses declined (Aiken, Clarke, and Sloane 2001; Aiken et al. 2001). These changes were short lived, and, within a few years, hospitals began adding nurse positions. Enrollments in nursing schools, however, had fallen significantly in the interim, and nurses were in short supply, motivating greater interest in international recruitment. Buerhaus, Staiger, and Auerbach (2003) peg the beginning of the current nurse shortage, the longest lasting in recent decades, at 1998, the point at which nurse immigration began its steady increase. Foreign-born nurses accounted for about a third of the increase in employed nurses between 2000 and 2002.
Changes in immigration policy may have also had an impact on the trends in nurse immigration. In 1995, the H-1A visa for temporary employment for foreign RNs was allowed to sunset. It is difficult to know how much of the decline in nurse immigration in 1996 and beyond was due to the visa change, versus lower employer demand for nurses. Additionally, in 1996, the Immigration and Naturalization Service (INS) required foreign-educated nurses to complete a screening program to qualify for permanent residence through employment. The INS did not issue rules for the implementation of the screening provision until 1999 when the Commission on Graduates of Foreign Nursing Schools (CGFNS) won a lawsuit requiring the rules to be issued. The more recent increase in immigration may be due to more aggressive recruitment of nurses from abroad and more creative utilization of existing immigration provisions. In an unusual decision, Congress in 2005 approved the “recapture” or carryover of 50,000 unused employment-based visas for nurses (and physical therapists) that had been authorized in previous years but not filled. Hospital employers urged Congress in 2006 to make available 90,000 additional unused employment-based visas for which skilled professionals, such as nurses, qualify. Representatives from the American Hospital Association (AHA) note that the additional visas for nurses approved by Congress in 2005 will have little impact on ameliorating the national shortage of hospital nurses but could bring temporary relief to some institutions (Fong 2005). Data from the U.S. Census reveal that 63 percent of foreign-born RNs residing in the United States in 2000 were U.S. citizens by naturalization suggesting that the majority of nurses who come to the U.S. stay.
Data Sources
There is no ideal source of information on nurse immigration to the United States and, thus, this paper relies on multiple sources, each with some limitations. The four main data sources are the U.S. Department of Homeland Security, the National Sample Survey of Registered Nurses (NSSRN), the U.S. Population Census, and the NCSBN. This paper focuses on RNs (professional nurses) only.
Immigration statistics reported by the U.S. Department of Homeland Security do not include complete information on occupational status except for those entering the United States on an occupational visa. Many nurses enter the country on other types of visas, for example, as family members or students. Thus, Department of Homeland Security statistics appears to significantly underestimate the number of foreign-educated nurses entering the United States.
The NSSRN, a national probability sample of 35,724 RNs drawn from 50 states and the District of Columbia in 2004 (USDHHS 2006), has the greatest detail on foreign-educated nurses residing in the United States. The survey has been conducted every 4 years since 1977. The 2004 NSSRN estimated that 3.5 percent of RNs in the United States, or 100,791 RNs, were trained abroad (Xu and Kwak 2005).
The U.S. Population Census, conducted every 10 years, is another source of information on foreign-born nurses. Its major limitation is the absence of data on countries in which professional education took place. Analyses of the 2000 U.S. Population Census (1 percent Public Use Data file) reveal over 300,000 foreign-born RNs. After deleting foreign-born nurses who immigrated before age 21, and, thus, probably received their nursing education in the United States, Census data suggest that close to 218,000 nurses in the United States are likely to have been educated abroad.
The NSSRN appears to significantly underestimate the number of foreign-educated nurses in the United States. Also, it finds little change in the number of foreign-educated nurses between 2000 and 2004, despite evidence from the NCSBN of more than a tripling of the number of foreign-educated nurses who passed the licensing exam over that period, most of whom presumably immigrated. The undercount of foreign-educated nurses in NSSRN may result from the geographic concentration of foreign-educated nurses in five states.
The NCSBN reports on an annual basis the number of nurses taking and passing the licensing exam (NCLEX-RN) by country of nursing education. The NCSBN data provide proxy measures of immigration potential (numbers taking the test the first time) and of the number of new foreign-educated nurses entering the United States (numbers passing the exam). Licenses to practice nursing are issued by the states, however, and NCSBN does not have a complete listing of newly licensed foreign-educated nurses from every state. The actual number of nurses immigrating is less, by an unknown amount, than the number passing the exam.
In this paper, NCSBN data are used to estimate annual trends in nurse migration. The NSSRN is used to explore the individual characteristics and qualifications of foreign-educated nurses and their practice patterns. The U.S. Census is used to estimate the number of foreign-educated nurses residing in the United States.
Primary Source Countries
Primary source countries and regions can be viewed in two ways: (1) the countries/regions that have contributed the largest number of nurses to the U.S. stock of RNs and (2) the countries that provide the largest number of nurses currently. Table 2 examines the current population of U.S. nurses born abroad and presumed to have been educated abroad because they migrated as adults. Close to a third of the estimated 218,720 foreign-educated nurses in the United States are from the Philippines. The second most important source regions for foreign-born nurses are the Caribbean and Latin America, which have contributed almost 50,000 nurses. Western developed countries including Canada, Western Europe, Australia, and New Zealand rank third with a total of almost 33,000 nurses. Overall, almost 60 percent of foreign-educated nurses have become citizens. Nurses from Western developed countries are less likely to become citizens.
Table 2.
Foreign-Educated* Registered Nurses by Region of Birth and Citizenship Status, U.S., 2000
| Citizen | |||
|---|---|---|---|
| Place of Birth | Yes | No | Total |
| The Philippines | 52,745 | 27,994 | 80,739 |
| Caribbean and Latin America | 30,707 | 16,214 | 46,921 |
| Western Europe, Canada, Australia, and New Zealand | 8,864 | 23,663 | 32,527 |
| Asia | 13,674 | 7,762 | 21,436 |
| Sub-Saharan Africa | 5,527 | 6,726 | 12,253 |
| India | 6,992 | 6,268 | 13,260 |
| Eastern Europe, Russian Federation | 5,649 | 4,949 | 10,598 |
| Other | 810 | 176 | 986 |
| Total | 124,968 | 93,752 | 218,720 |
Source: Author's calculation from the U.S. Deptartment of Commerce, Bureau of the Census, Census of Population and Housing (2000), Public Use Micro data, 1% sample.
Foreign-educated estimated by eliminating RNs born abroad who immigrated to the United States before age 22.
RNs, registered nurses.
Table 3 presents a snapshot of current nurse immigration to the United States by the 10 source countries contributing the largest number of nurses in 2005. As noted earlier, the number of nurses passing the NCLEX-RN is used as a proxy for the number of nurses who immigrate. The pass rate for first time NCLEX-RN test takers is also included, as it suggests the relative difficulty of a migration by country, and possibly is a reflection of the comparability of education and/or English language comprehension of nurses from various countries. The first time pass rate for U.S. nurses in 1995 was 87 percent. The Philippines continues to contribute more nurses than any other source country, although almost half fail to pass the NCLEX-RN the first time. This relatively low pass rate has been consistent for Philippine test takers and is not a new phenomenon to be attributed to the rapid growth in nursing schools in the Philippines. Three other countries contribute over 1,000 nurses a year: India, South Korea, and Canada. The remaining source countries, even among the top 10, contribute <300 a year. Nigeria is the only sub-Saharan African country among the top 10 source countries for the United States.
Table 3.
Top 10 Source Countries for NCLEX-RN Exam Passers and First-Time Pass Rates for 2005
| Source Country | Number Passing | First-Time NCLEX Pass Rate % |
|---|---|---|
| The Philippines | 6,852 | 55 |
| India | 1,927 | 72 |
| South Korea | 1,587 | 72 |
| Canada | 1,168 | 69 |
| China | 288 | 65 |
| Nigeria | 275 | 34 |
| United Kingdom | 226 | 61 |
| Taiwan | 222 | 53 |
| Cuba | 217 | 32 |
| Russian Federation | 144 | 44 |
| Top 10 total/average | 12,906 | 60 |
| Total all countries/average | 14,750 | 44 |
Source: Author's analysis of National Council of State Boards of Nursing data.
RNs, registered nurses.
Demographic Characteristics
The demographic and work characteristics of native- and foreign-educated nurses are compared in Table 4. Average age is very similar for both groups, close to 43 years of age in 2000, suggesting that immigration has had little impact on lowering the average age of U.S. nurses. The majority of foreign-educated nurses are married, as are native-born nurses. Foreign-educated nurses are somewhat more likely to have a baccalaureate degree, or higher, and to work full time than native-born nurses. Overall, foreign-educated nurses have higher incomes than native-born nurses, but the difference seems to be explained by the longer hours worked by foreign-educated nurses (Lowell and Gerova 2004) and, possibly, by their concentration on the two coasts, where nurses' wages are higher.
Table 4.
Characteristics of U.S. Registered Nurses by Nativity, 2000
| Native Born | Foreign Born | |
|---|---|---|
| Age (average) in years | 42.5 | 42.8 |
| Female (%) | 92.4 | 90.9 |
| Married (%) | 68.1 | 70.2 |
| Hold BSN (%)* | 43.6 | 48.9 |
| Work full-time (%)* | 58.0 | 72.5 |
| Work outside metropolitan area (%) | 17.8 | 1.5 |
| Work in metropolitan area, not central (%) | 60.3 | 52.7 |
| Central city (%) | 21.9 | 45.9 |
Source: Author's calculation from the U.S. Department of Commerce, Bureau of the Census, Census of Population and Housing (2000), Public Use Micro data, 1% sample.
Author's calculation from 2000 National Sample Survey of Registered Nurses.
Geographic Distribution
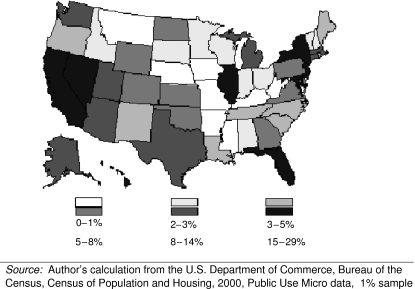
Figure 2 shows the uneven distribution of foreign-educated nurses by state. California, New York, New Jersey, Florida, and Illinois have the highest density of foreign-educated nurses, with foreign-educated nurses comprising as much as 29 percent of the nurse workforce in California and 24 percent in Florida. These states all report acute shortages of nurses, particularly in hospitals. Both California and Florida have particularly low nurse to population ratios. California's shortage has been exacerbated by enactment of legislation that took effect from January 1, 2004, mandating minimum licensed nurse staffing ratios in all hospitals. Nurse workloads cannot exceed five patients per nurse on medical and surgical units and two in ICUs (Coffman, Seago, and Spetz 2002).
Figure 2.
Proportion of all Registered Nurses that Are Foreign-Born by State, 2000.
Urban/Rural Location
Foreign-educated nurses are less likely to reside in rural areas than are native-born nurses, as noted in Table 4, and they are much more likely to reside in central city locations. Less than 2 percent of foreign-educated nurses reside outside of metropolitan areas, compared with 18 percent of native-born nurses. Thus, foreign-educated nurses are not likely to have had much of an impact on rural–urban health services gaps or nurse shortages in rural areas. This is noteworthy given the immigration provisions that favor visas for nurses to work in rural nurse shortage areas. Foreign-educated nurses are twice as likely as native-born nurses to reside in central city locations where safety-net hospitals and other services for the poor tend to be located.
Employment Setting
Foreign-educated nurses are more likely to work in hospitals and in intensive care (not shown), settings in which the nurse shortage has been greatest (see Table 5). Almost 72 percent of foreign-educated nurses work in hospitals, compared with 59 percent of native-born nurses. An estimated 15,000 foreign-educated RNs work in nursing homes and extended care. While foreign-educated nurses are only slightly more likely to practice in nursing homes and extended care than native-born RNs (9 versus 7 percent), the numbers are important in a sector of health care that is experiencing 15 percent vacancy rates for RNs (National Commission on Nursing Workforce for Long-Term Care 2005). Foreign-educated nurses are distributed across clinical specialties, much like native-born nurses, except for their higher presence in intensive care. Foreign-educated nurses are no more likely to practice in psychiatry, for example, than native-born nurses, and are less likely to be employed in primary care.
Table 5.
Characteristics of Registered Nurses by U.S. Education and Foreign Education
| United States (%) | Foreign-Educated (%) | |
|---|---|---|
| Employment setting | ||
| Hospital | 58.7 | 71.6 |
| Nursing home, extended care | 6.9 | 9.2 |
| Community health | 13.1 | 8.4 |
| Ambulatory care | 9.8 | 5.2 |
| Ethnic background | ||
| White (non-Hispanic) | 90.1 | 32.4 |
| Black | 4.8 | 8.1 |
| Hispanic | 1.9 | 3.7 |
| Asian/Pacific Island | 1.4 | 54.5 |
Source: Author's calculation from 2000 National Sample Survey of Registered Nurses.
Workforce Diversity
Ninety percent of U.S. nurses are white, and blacks and Hispanics are underrepresented in relation to their proportion of the U.S. population. As noted in Table 5, foreign-educated nurses are less likely to be white than native-born nurses, but not much more likely to be black or Hispanic. The major difference in ethnicity between native and foreign-educated nurses is that half of all foreign-educated nurses are Asian compared with 1 percent of native-born nurses. Thus, while nurse immigration contributes somewhat to ethnic and cultural diversity of the U.S. nurse workforce, it does not contribute substantially to increasing the number of black and Hispanic nurses, the major underrepresented minorities. This finding must be viewed in the context of thousands of qualified American applicants to nursing school being turned away, including black and Hispanic applicants. If achieving greater representation of blacks and Hispanics in the nurse workforce is the objective, efforts to accommodate the American applicant pool would appear be a worthy strategy, and one without adverse consequences for lower-income countries.
Professional Values
U.S. nurses have expressed concerns about the employment of nurses educated abroad, particularly in relation to their competence to practice in a highly technological environment and their ability to communicate. To some extent, competence and communications issues have been addressed by CGFNS via examinations in nursing knowledge and English proficiency (Xu, Xu, and Zhang 1999). Nurses' concerns have persisted about the extent to which differences in cultural values held by nurses from more collectivistic cultures such as the Philippines, which comprise the majority of new nurse immigrants to the United States, would undermine U.S. nurses' quests for increased autonomy, control, and professional status (Brush 1994, 1999). However, Flynn and Aiken (2002) confirmed that U.S.- and foreign-educated nurses share a set of core nursing values that embrace professional nursing practice models, such as Magnet Hospitals (McClure and Hinshaw 2002), and include professional values, such as clinical autonomy and collegiality with physicians. Indeed, the Flynn and Aiken study found that the absence of a positive professional nurse practice environment has the same negative outcomes of job dissatisfaction, burnout, and turnover among foreign-educated nurses as among native-born nurses. Health care organizations with poor work environments are likely to have problems retaining foreign-educated nurses once their contract obligations have been fulfilled, just as they experience high turnover of native-born nurses.
NURSE IMMIGRATION REQUIREMENTS
The United States has stringent requirements for licensing nurses compared with most other countries. A VisaScreen™ certificate must be received before the U.S. Citizenship and Immigration Services will issue an occupational visa. To obtain the certificate, the following are required: (1) a credentials review of the applicant's professional education and licensure to ensure comparability with U.S. requirements, especially to make certain that nursing education was at the post-secondary level; (2) successful completion of required English language proficiency examinations; and (3) successful completion of either the CGFNS qualifying examination or the NCLEX-RN examination. As a point of comparison, the United Kingdom does not have a licensure examination, and credential reviews are up to employers. The CGFNS has a comprehensive program of services for foreign-educated nurses, designed to help ensure safety in patient care, as well as to facilitate the application process for graduates of foreign nursing schools who wish to immigrate to the United States (Davis and Nichols 2002). CGFNS undertakes the required credentials review and offers tests of nursing knowledge and English proficiency. CGFNS offers its nursing knowledge examination in many locations throughout the world; the exam provides nurses interested in migrating to the United States a good indication of their likelihood of passing the required licensure exam (NCLEX-RN), which until 2005 was offered only in the United States. For the first time, in 2005 the NCLEX-RN was offered in three sites outside the United States: London, Hong Kong, and Seoul. In 2006, NCSBN planned to expand test sites to Australia, India, Japan, Mexico, Canada, Germany, and Taiwan, in order to lessen the financial burdens on qualified candidates who intend to apply for licensure in the United States.
The North American Free Trade Agreement (NAFTA) facilitated the migration of Canadian nurses to the United States. Contrary to expectations, however, NAFTA has not substantially influenced the migration of nurses from Mexico. Most nursing education in Mexico takes place at the secondary-school level, which does not meet U.S. requirements for licensure. English language proficiency is another barrier. A total of 77 Mexican nurses took the NCLEX-RN exam for the first time in 2003 and the pass rate was 17 percent compared with 2,126 Canadian nurses who had a pass rate of 75 percent (NCSBN 2006).
POLICY AND PRACTICE IMPLICATIONS
The United States lacks a national capacity to monitor nurse labor market dynamics and has no national nurse workforce policy, despite dire predictions about impending shortages. Indeed, health workforce policy was not ranked among the top 10 policy priorities in a recent survey of experts by the Commonwealth Fund (2004). The implications of health care cost containment policies for nursing supply and demand are rarely, if ever, considered prospectively. Immigration policies are not part of a broader strategy to ensure sufficient availability of nurses to meet national needs. There is little coherence between international development and immigration policies.
Unlike many other countries where the government fully funds nursing students to become qualified nurses, U.S. nurses pay for their own education, helped by tax subsidies to public educational institutions and limited scholarship and student loan programs. In recent years, out-of-pocket costs of higher education have increased significantly. Enrollments in nursing schools are thus sensitive to nurse labor market dynamics, as exemplified by the reduction in graduations between 1995 and 2001 of up to 25,000 nurses a year. Public policy, at a minimum, should establish the capacity to monitor changes in nurse labor market dynamics, consider how changes might impact on long-term availability of nursing services, and offer suggestions when indicated for public and/or private sector responses.
In view of future projected large shortages of nurses, public policy interventions and private sector actions warrant consideration. They fall into four interrelated categories: (1) transition to greater self-sufficiency in domestic nurse labor; (2) diminishing the rate of growth in demand for nurses by improving retention and achieving greater productivity; (3) managed nurse migration; and (4) achieving more coherence between international development and immigration policies.
Self-Sufficiency
The United States has the capacity, in terms of human and economic resources, to become largely self-sufficient in its nurse workforce. There are large numbers of Americans who want to become nurses, thousands more than can be accommodated by nursing schools because of faculty shortages and other capacity limitations. The United States has a large enough labor pool and enough resources to expand higher education to increase nurse supply. Moreover, greater representation in nursing by blacks, Hispanics, and men could be achieved by expanding nursing school capacity at a time when the applicant pool is strong.
Expanding nurse supply is in the interest of nurse employers. Indeed, hospitals, the major employers of nurses, have been making significant investments in nurse education through tuition support in exchange for work commitments for new graduates, facilitating access to education for their nurse employees, providing space in their facilities for nursing education, and enabling their employed nurses with graduate education to serve as clinical faculty for nursing schools (Cheung and Aiken 2006). However, hospitals are unlikely to substantially increase their support of nursing education beyond current levels without provisions to include these costs in reimbursement rates. The State of Maryland is currently implementing such an initiative where the State Health Services Cost Review Commission increased hospital rates by a tenth of 1 percent, raising about $100 million over 10 years to be used in solving the hospital nursing shortage by investing in the expansion of nursing faculty and nursing school enrollments.
Investments by hospitals in nursing education have helped nursing schools expand enrollments substantially over the past 5 years resulting in the highest number of new nurse graduates ever, at close to 100,000 a year. However, most estimates suggest that increases in enrollments will have to be considerably higher to avert the nurse shortage projected to occur in a decade when increasing demand collides with increasing retirements of an aging nurse workforce (AACN 2005). Title VIII funding under the Public Health Service Act provides an annual federal appropriation ($149.68 million in FY 2006) for nurse workforce development programs, including advanced practice in nurse training (i.e., nurse practitioners, nurse anesthetists, nurse administrators), grant support to increase nursing workforce diversity and improve retention, and loan repayment and scholarship funds. These funds were only modestly increased by the Nurse Reinvestment Act, passed in 2002 as a response to the nursing shortage. In 2004, 82 percent of applicants for the loan repayment program and 98 percent of the applicants for scholarships were turned away due to insufficient funding (AACN 2005). The federal Nurse Training Act in 1974 is credited with increasing the nation's nurse to population ratio by 100 percent in the period 1974–1983 (Eastaugh 1985). In today's dollars, a comparable investment would require over $400 million a year in addition to the existing funding levels for Title VIII, an amount that would be insignificant as a percent of federal health expenditures.
Times of nurse shortage tend to lead to calls for shortened education for nurses. There is ample evidence, however, that a more educated nurse workforce is associated with better patient outcomes and higher nurse productivity (Aiken et al. 2003; Estabrooks et al. 2005). Indeed, the recent position statement of the American Organization of Nurse Executives (AONE), representing the employers of nurses, which favors baccalaureate education (Bowcutt 2005), can be expected to aid in the transition to a more highly educated nurse workforce. Innovations in nursing education have created options to produce nurses with a baccalaureate degree in about 1 year for students who hold a baccalaureate or higher degree in another field. These accelerated programs are among the most popular in nursing schools today and speak to the high level of interest of Americans in becoming nurses. In many states, the length of associate degree programs has increased to 3 years or more to meet the requirements for practice, thus, reducing the difference in the time it takes to produce nurses with associate versus baccalaureate degrees. Nursing schools need incentives and/or mandates to create more efficient educational pathways that will permit the extensive network of community colleges to participate in baccalaureate nursing education, thus producing a larger cadre of nurses with baccalaureate degrees without extending substantially the time it takes students to complete their education.
Improving Retention and Increasing Productivity
Nurse turnover rates, particularly in hospitals and nursing homes, are high. Additionally, more nurses are opting to work in jobs outside of hospitals and nursing homes and in nonclinical roles. A substantial body of research links poor work environments with nurse job dissatisfaction, burnout, turnover, and increased costs (Aiken et al. 2002; Vahey et al. 2004; Waldman et al. 2004). Every blue-ribbon expert committee convened over the past 25 years to make recommendations on how to solve the U.S. nursing shortage recommended modifications in nurses' practice environments to retain nurses in clinical roles and facilitate their productivity (AHA 2002; The Joint Commission 2002; Kimball and O'Neil 2002; Steinbrook 2002). Progress has been slow but growth of the Magnet Recognition Program suggests that positive change is occurring (Aiken 2002). Ultimately the long-term solution to the projected future shortage of nurses is to redesign work, particularly in hospitals, to enable nurses to be more productive in their care of patients (The Joint Commission 2005), potentially resulting in the need for fewer nurses than would be required in the absence of changes in work design and better organizational support of nursing care. Improving work environments is largely an agenda that must be taken on within health care organizations by management and clinicians, although there is the possibility that new payment incentives, such as Pay for Performance, might provide an impetus for change.
Managed Nurse Migration
The projected size of the long-term nurse shortage in the United States appears too large to be resolved primarily through recruitment of nurses from other countries. To place the projected shortage of 800,000 nurses in perspective, Canada currently has a nurse workforce of fewer than 250,000 nurses and a projected shortage of 100,000 (see Little 2007). India, a country with a very large overall workforce and therefore the potential to produce large number of nurses for export, currently has a low density of nurses relative to its population, and the majority of its current 600,000 nurses (Chen and Evans 2004) would not meet U.S. educational standards. Nevertheless, Indian nurses, as well as nurses from other low-income countries, are interested in working in the United States. Entrepreneurial activities to produce more nurses abroad for export to the United States can be expected.
At present, there is little “management” of international nurse recruitment that would ideally include provisions to balance the rights of individual nurse migrants and their families, the interests of their countries of origin, patient concerns about quality and communication, and employers' needs. The services of CGFNS are designed to contribute to achieving such a balance but many important aspects of nurse immigration remain largely unaddressed. Given the decentralized and largely private nature of health care in the United States, private sector entities should develop and enforce ethical and quality standards for nurse recruitment and involvement of U.S. educational institutions in training nurses for export to the United States. The Joint Commission sets and enforces quality standards in settings that employ international nurses and has a program of accreditation for supplemental staffing firms. The Joint Commission is an example of a type of private sector organization that could play a more active role in protecting the public interest in international nurse recruitment. Nursing education accreditation bodies could play more central roles in the oversight of educational programs preparing nurses for export to the United States, especially those involving American nursing schools. Another potential strategy to manage the ethical and quality dimensions of nurse recruitment would be through provisions to the Medicare requirements for provider conditions of participation. There could be other strategies, as well, but the point is that insufficient attention has been given to managing the ethical and quality concerns pertaining to the use of international workers in health care, which is bound to increase in the future.
International Development and Immigration Policies
Employers, professional associations, and other stakeholders with interests in having an adequate supply of nurses in the future should work together with the federal government to promote more coherence between international development and foreign aid and immigration policies. With modest, targeted investments, the U.S. foreign aid funds could have a substantial impact on expanding the capacity of low-income countries with high illness burden to increase their production of nurses and improve nurse retention. The focus should be on developing a self-sustaining nursing educational infrastructure with capacity to produce nurse leaders and faculty, as well as clinical nurses.
Research suggests that the differentials in wages between low-income source and high-income destination countries are so large that small increases in source country wages do not affect migration. Thus, nonwage interventions in source countries are likely to be more successful in retaining nurses (Vujicic et al. 2004). Creating safer and more rewarding professional nurse roles and settings in source countries could be very important in stemming the flight of nurses. Initiatives are needed to find ways to make professional nursing more attractive in source countries. A recently completed demonstration supported by the United States Agency for International Development involving “twinning” is an exemplar worthy of replication (Aiken 2005). The Nursing Quality Improvement Program paired U.S. hospitals that had been accredited for nursing excellence in the Magnet Recognition Program with hospitals in Russia and Armenia, countries that have historically underinvested in professional nursing. Over a 3-year period involving the exchange of nurses and hospital managers between the countries, the professional roles of nurses in the participating Russian and Armenian hospitals expanded, nurses were more satisfied with their jobs, patients were more satisfied with their care, and adverse patient outcomes were reduced. This model needs to be replicated in countries experiencing more nurse emigration to know whether increased job satisfaction would translate into greater retention within source countries. This model and others like it are worthy of investment by the United States and other developed countries as a strategy to reduce the “push” factors associated with the lack of professional roles and opportunities for nurses in low-income countries.
The United States clearly plays an important role in global nurse migration because of the size of its nurse workforce and its ever-growing demand for more nurses. The size of its projected future shortage of nurses, if not contained by increases in domestic production of nurses and policies to dampen growing demand, threatens to undermine health care delivery in the United States as well as in low-income countries whose nurses would migrate to the United States in significant numbers. By developing and implementing an action plan to ensure the availability of enough nurses to meet future needs in the United States, we will ensure access and quality of care for our own citizens in addition to making a very important contribution to global health.
Acknowledgments
This research was supported by the Robert Wood Johnson Foundation and the Agency for Healthcare Research and Quality. The author gratefully acknowledges the analytic assistance of Tim Cheney, the provision of data by the NCSBN, and the comments of an anonymous reviewer.
REFERENCES
- AHA Commission on Workforce for Hospitals and Health Systems. In Our Hands: How Hospital Leaders Can Build a Thriving Workforce. Chicago: American Hospital Association; 2002. [Google Scholar]
- Aiken LH. Superior Outcomes for Magnet Hospitals: The Evidence Base. In: McClure ML, Hinshaw AS, editors. Magnet Hospitals Revisited: Attraction and Retention of Professional Nurses. Washington, DC: American Nurses Publishing; 2002. pp. 61–81. [Google Scholar]
- Aiken LH. Extending the Magnet Concept to Developing and Transition Countries: Journey to Excellence. Reflections on Nursing Leadership. 2005;31(1):16–9. [PubMed] [Google Scholar]
- Aiken LH, Buchan J, Sochalski J, Nichols B, Powell M. Trends in International Nurse Migration. Health Affairs. 2004;23(3):69–77. doi: 10.1377/hlthaff.23.3.69. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational Levels of Hospital Nurses and Surgical Patient Mortality. Journal of the American Medical Association. 2003;290(12):1617–23. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM. Hospital Restructuring: Does It Adversely Affect Care and Outcomes? Journal of Health and Human Services Administration. 2001;23(4):416–40. [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty AM, Shamian J. Nurses' Reports of Hospital Quality of Care and Working Conditions in Five Countries. Health Affairs. 2001;20(3):43–53. doi: 10.1377/hlthaff.20.3.43. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout and Job Dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- American Association of Colleges of Nursing (AACN) “With Enrollments Rising for the 5th Consecutive Year, U.S. Nursing Schools Turn Away 30,000 Qualified Applications in 2005”. [March 1, 2007];2005 Press release, December 12, 2005. Available at http://www.aacn.nche.edu/Media/NewsReleases/2005/enrl05.htm.
- Bowcutt M. Voice of Nursing Leadership. Chicago: American Organization of Nurse Executives; 2005. [March 1, 2007]. Letter from the Leadership. May 2005, pp. 1–12. Available at http://www.aone.org/aone/pdf/Voice?20Newsletter-May?20final-for?20web.pdf. [Google Scholar]
- Brush BL. Philadelphia: Unpublished Doctoral Dissertation, University of Pennsylvania; 1994. “Sending for Nurses: Foreign Nurse Immigration to American Hospitals: 1945–1980”. [Google Scholar]
- Brush BL. Has Foreign Nurse Recruitment Impeded African American Access to Nursing Education and Practice? Nursing Outlook. 1999;34(1):67–73. doi: 10.1016/s0029-6554(99)90093-3. [DOI] [PubMed] [Google Scholar]
- Brush BL, Berger AM. Sending for Nurses: Foreign Nurse Migration, 1965–2002. Nursing and Health Policy Review. 2002;1(2):103–15. [Google Scholar]
- Brush BL, Sochalski J, Berger AM. Imported Care: Recruiting Foreign Nurses to U.S. Health Care Facilities. Health Affairs. 2004;23(3):78–87. doi: 10.1377/hlthaff.23.3.78. [DOI] [PubMed] [Google Scholar]
- Buchan J. International Recruitment of Nurses: Policy and Practice in the United Kingdom. Health Services Research. 2007 doi: 10.1111/j.1475-6773.2007.00710.x. DOI: 10.1111/j.1475-6773.2007.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buerhaus PI, Staiger DO, Auerbach DI. Is the Current Shortage of Hospital Nurses Ending? Health Affairs. 2003;22(6):191–8. doi: 10.1377/hlthaff.22.6.191. [DOI] [PubMed] [Google Scholar]
- Buerhaus PI, Staiger DO, Auerbach DI. New Signs of a Strengthening U.S. Labor Market? Health Affairs. 2004;23:526–33. doi: 10.1377/hlthaff.w4.526. (Web exclusive) [DOI] [PubMed] [Google Scholar]
- Chen LC, Evans T. Human Resources for Health: Overcoming the Crisis. Boston: Harvard University; 2004. [DOI] [PubMed] [Google Scholar]
- Cheung R, Aiken LH. Hospital Initiatives to Support a Better-Educated Workforce. Journal of Nursing Administration. 2006;36(7/8):357–62. doi: 10.1097/00005110-200607000-00007. [DOI] [PubMed] [Google Scholar]
- Coffman JM, Seago JA, Spetz J. Minimum Nurse-to-Patient Ratios in Acute Care Hospitals in California. Health Affairs. 2002;21:53–64. doi: 10.1377/hlthaff.21.5.53. [DOI] [PubMed] [Google Scholar]
- Commonwealth Fund. “The Commonwealth Fund Health Care Opinion Leaders Survey: Assessing Health Care Experts' Views on Policy Priorities”. [March 1, 2007];2004 Available at http://www.cmwf.org/surveys/surveys_show.htm?doc_id=254281.
- Davis CR, Nichols BL. Foreign-Educated Nurses and the Changing U.S. Nursing Workforce. Nursing Administration Quarterly. 2002;26(2):43–51. [Google Scholar]
- Eastaugh SR. The Impact of the Nurse Training Act on the Supply of Nurses, 1974–1983. Inquiry. 1985;22(4):404–17. [PubMed] [Google Scholar]
- Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The Impact of Hospital Nursing Characteristics on 30-Day Mortality. Nursing Research. 2005;54(2):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Flynn L, Aiken LH. Does International Nurse Recruitment Influence Practice Values in U.S. Hospitals? Journal of Nursing Scholarship. 2002;34(1):65–71. doi: 10.1111/j.1547-5069.2002.00067.x. [DOI] [PubMed] [Google Scholar]
- Fong T. Nurse Visa Crisis Eases. Modern Healthcare. 2005;35(24):28. [Google Scholar]
- The Joint Commission. Health Care at the Crossroads: Strategies for Addressing the Evolving Nursing Crisis. Oak Brook Terrace, IL: The Joint Commission; 2002. [Google Scholar]
- The Joint Commission. Issues and Strategies for Nurse Leaders: Meeting Hospital Challenges Today. Oak Brook Terrace, IL: The Joint Commission; 2005. [Google Scholar]
- Kimball B, O'Neil E. Health Care's Human Crisis: The American Nursing Shortage. Princeton, NJ: The Robert Wood Johnson Foundation; 2002. [Google Scholar]
- Kingma M. Nurses on the Move: Migration and the Global Health Care Economy. Ithaca, NY: Cornell University Press; 2006. [Google Scholar]
- Little L. Nurse Migration: A Canadian Case Study. Health Services Research. 2007 doi: 10.1111/j.1475-6773.2007.00709.x. DOI: 10.1111/j.1475-6773.2007.00709.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowell L, Gerova SG. Immigrants and the Healthcare Workforce: Profiles and Shortages. Work and Occupations. 2004;31(4):474–98. [Google Scholar]
- McClure ML, Hinshaw AS. Magnet Hospitals Revisited. Washington, DC: American Nurses Publishing; 2002. [Google Scholar]
- National Commission on Nursing Workforce for Long-Term Care. “Act Now for Your Tomorrow”. [August 15, 2006];2005 Available at http://www.ahca.org/research/workforce_rpt_050519.pdf.
- National Council of State Boards of Nursing (NCSBN) 2005 Nurse Licensee Volume and NCLEX Examination Statistics. Chicago: NCSBN; 2006. [Google Scholar]
- National League for Nursing. “Despite Encouraging Trends Suggested by the NLN's Comprehensive Survey of all Nursing Programs, Large Number of Qualifies Applications Continue to be Turned Down. NLN News. 2005 December 9, 2005. [Google Scholar]
- Ross SJ, Polsky D, Sochalski J. Nursing Shortages and International Nurse Migration. International Nursing Review. 2005;52:253–62. doi: 10.1111/j.1466-7657.2005.00430.x. [DOI] [PubMed] [Google Scholar]
- Steinbrook R. Health Policy Report: Nursing in the Crossfire. New England Journal of Medicine. 2002;346(22):1757–65. doi: 10.1056/NEJM200205303462225. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Projected Supply, Demand, and Shortages of Registered Nurses: 2000–2020. Washington, DC: USDHHS; 2002. [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Preliminary Findings the Registered Nurse Population: National Sample Survey of Registered Nurses March 2004. Washington, DC: Health Resources and Services Administration; 2006. [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics. “Occupational Outlook Handbook: 2004–05 Edition”. [June 27, 2005];2005 Available at http://www.bls.gov/news.release/ecopro.t06.htm.
- Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse Burnout and Patient Satisfaction. Medical Care. 2004;42(2, suppl):II57–66. doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujicic MP, Zurn P, Kiallo K, Adams O, Poz MK. The Role of Wages in the Migration of Health Care Professionals from Developing Countries. [March 1, 2007];Human Resources for Health. 2004 2(3) doi: 10.1186/1478-4491-2-3. April 28, 2004. Available at http://www.human-resources-health.com/content/pdf/1478-4491-2-3.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman JD, Kelly F, Arora S, Smith HL. The Shocking Cost of Turnover in Health Care. Health Care Management Review. 2004;29:2–7. doi: 10.1097/00004010-200401000-00002. [DOI] [PubMed] [Google Scholar]
- Xu Y, Kwak C. Characteristics of Internationally Educated Nurses in the United States. Nursing Economics. 2005;23(5):233–8. [PubMed] [Google Scholar]
- Xu Y, Xu Z, Zhang J. International Credentialing and Immigration of Nurses: CGFNS. Nursing Economics. 1999;17(6):325–31. [PubMed] [Google Scholar]