Abstract
Aim
To evaluate whether aqueous humour levels of pigment epithelium‐derived factor (PEDF) are associated with monocyte chemoattractant protein‐1 (MCP‐1) in patients with uveitis.
Methods
Aqueous humour levels of MCP‐1 and PEDF were determined by ELISA in 34 uveitis samples and 9 cataract control samples.
Results
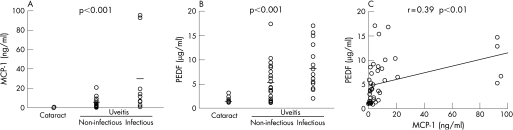
Aqueous humour MCP‐1 and PEDF levels were significantly higher in patients with infectious or non‐infectious uveitis than in controls (mean (SD) 32.3 (10.7) ng/ml vs 4.48 (1.10) ng/ml vs 0.47 (0.10) ng/ml, and 8.40 (1.30) μg/ml vs 5.01 (0.92) μg/ml vs 1.32 (0.22) μg/ml, respectively, p<0.001). A positive correlation between PEDF and MCP‐1 was found in patients with uveitis (r = 0.39, p<0.01).
Conclusion
The results demonstrated that aqueous humour levels of PEDF were positively associated with MCP‐1 in patients with uveitis. The present observations suggest that aqueous humour levels of PEDF may be a marker of inflammation in uveitis.
Pigment epithelium‐derived factor (PEDF) was first purified from the conditioned media of human retinal pigment epithelial cells with neuronal differentiating activity.1 Recently, PEDF has been shown to be the most potent inhibitor of angiogenesis in the mammalian eye; it inhibited retinal endothelial cell growth and migration, and suppressed ischaemia‐induced retinal neovascularisation.2 In addition, PEDF decreased retinal levels of proinflammatory cytokines in experimental diabetes, thus acting as an endogenous anti‐inflammatory factor as well.3 Since PEDF levels in vitreous humour are decreased in patients with diabetes with proliferative retinopathy,4 loss of PEDF in the eye could contribute to diabetic retinopathy. However, a role for PEDF in inflammatory eye diseases such as uveitis is not fully understood. In this study, we examined whether aqueous humour levels of PEDF were associated with an inflammatory biomarker, monocyte chemoattractant protein‐1 (MCP‐1), in patients with active uveitis.5
Patients and methods
Informed consent was obtained from all patients. Patients with various clinical entities of strictly diagnosed active uveitis with a mean (SD) age of 48.5 (2.7) years (n = 34; 13 with infectious uveitis, 21 with non‐infectious uveitis) were studied. Aqueous humour was collected from the patients under aseptic conditions. Nine aqueous humour samples were obtained during surgery from patients with cataract with a mean (SD) age of 65.2 (2.7) years, and served as controls. Aqueous humour levels of PEDF and MCP‐1 were measured as described previously.6 Inter‐assay (n = 17) and intra‐assay (n = 14) coefficients of variation of the PEDF ELISA were 4.7% and 7.3%, respectively.6 The data were analysed by the Kruskal–Wallis test and Pearson's correlation coefficient by the rank test.
Results and discussion
As shown in fig 1A,B, aqueous humour mean levels of MCP‐1 and PEDF were significantly higher in patients with infectious or non‐infectious uveitis than in controls (32.3 (10.7) ng/ml vs 4.48 (1.10) ng/ml vs 0.47 (0.10) ng/ml, and 8.40 (1.30) μg/ml vs 5.01 (0.92) μg/ml vs 1.32 (0.22) μg/ml, respectively, p<0.001). A positive correlation between PEDF and MCP‐1 was found in patients with uveitis (r = 0.39, p<0.01, fig 1C).
Figure 1 Aqueous humour levels of (A) monocyte chemoattractant protein‐1 (MCP‐1) and (B) pigment epithelium‐derived factor (PEDF) in patients with uveitis and controls. The horizontal line indicates the mean concentration (Kruskal–Wallis test). (C) Correlation between aqueous humour levels of PEDF and MCP‐1 in patients with uveitis. Pearson's correlation coefficient by rank test.
The present results demonstrate for the first time that aqueous humour levels of PEDF are positively correlated with those of MCP‐1 in patients with uveitis. We have recently found that PEDF inhibits advanced glycation end product‐induced MCP‐1 expression in endothelial cells through its antioxidative properties.7 In addition, Zhang et al3 reported that PEDF could act as an endogenous anti‐inflammatory factor in diabetic retinopathy. Taken together, our present findings suggest that aqueous humour levels of PEDF may be increased as a countersystem against inflammation in uveitis and may be a novel biomarker of inflammation in uveitis.
Abbreviations
MCP‐1 - monocyte chemoattractant protein‐1
PEDF - pigment epithelium‐derived factor
Footnotes
Competing interests: None declared.
References
- 1.Tombran‐Tink J, Chader C G, Johnson L V. PEDF: pigment epithelium‐derived factor with potent neuronal differentiative activity. Exp Eye Res 199153411–414. [DOI] [PubMed] [Google Scholar]
- 2.Duh E J, Yang H S, Suzuma I.et al Pigment epithelium‐derived factor suppresses ischemia‐induced retinal neovascularization and VEGF‐induced migration and growth. Invest Ophthalmol Vis Sci 200243821–829. [PubMed] [Google Scholar]
- 3.Zhang S X, Wang J J, Gao G.et al Pigment epithelium‐derived factor (PEDF) is an endogenous anti‐inflammatory factor. FASEB J 200620323–325. [DOI] [PubMed] [Google Scholar]
- 4.Spranger J, Osterhoff M, Reimann M.et al Loss of the antiangiogenic pigment epithelium‐derived factor in patients with angiogenic eye disease. Diabetes 2002502641–2645. [DOI] [PubMed] [Google Scholar]
- 5.Verma M J, Lloyd A, Rager H.et al Chemokines in acute anterior uveitis. Curr Eye Res 1997161202–1208. [DOI] [PubMed] [Google Scholar]
- 6.Yamagishi S, Adachi H, Abe A.et al Elevated serum levels of pigment epithelium‐derived factor (PEDF) in the metabolic syndrome. J Clin Endocrinol Metab 2006912447–2450. [DOI] [PubMed] [Google Scholar]
- 7.Inagaki Y, Yamagishi S, Okamoto T.et al Pigment epithelium‐derived factor prevents advanced glycation end products‐induced monocyte chemoattractant protein‐1 production in microvascular endothelial cells by suppressing intracellular reactive oxygen species generation. Diabetologia 200346284–287. [DOI] [PubMed] [Google Scholar]