Abstract
Purpose
Clinical outcomes for phacoemulsification surgery are still compared with the almost 10‐year‐old benchmark of the 1997–98 National Cataract Surgery Survey (NCSS) published in this journal. Extraneous to the peer‐reviewed research literature, more recent databases suggest much better results may be being obtained. This offered the rare opportunity to perform an audit as research investigating if this was indeed the case and a new benchmark is needed, with the additional standard of rigorous study peer review by independent senior ophthalmologists. At this pilot centre for Patient Choice provision, all cataract surgery was performed on Consultant‐supervised training lists, a novel extension in‐sourcing care using public resources rather than to an independent sector that may not be supervised by NHS Consultants. Patient satisfaction was also surveyed. We asked whether the NCSS is out‐of‐date, and whether good outcomes on Choice schemes are compatible with Consultant‐led training within the National Health Service?
Methods
An audit of 1000 consecutive patients undergoing cataract surgery on Patient Choice at the Western Eye Hospital between October 2002 and September 2004. All subjects were scheduled for phacoemulsification. A novel policy was extending “choice” onto training list slots for this period. A validated questionnaire assessed patient satisfaction.
Results
A best corrected visual acuity of 6/12 or better was obtained in 93% of cases. Over 80% of cases were ±1 D of target refraction (65.7% within 0.5 D). The total incidence of complications was 8.7%. Overall incidence of major complications was 2.4%. Incidence of vitreous loss was 1.1% and that of endophthalmitis 0.1%. Complications rates were lowest for consultants (less than 1%). User satisfaction with having cataract surgery on “patient choice” was high.
Conclusions
Cataract surgery under patient choice on supervised training lists is associated with a visual outcome and an incidence of complications at least as good as the published national average. User satisfaction is high. Cataract surgery under patient choice is compatible with training activity in receiving hospitals. The improvement in outcomes since the 1997–98 NCSS suggest that the accepted standards for complication rates should be updated to reflect the fact that phacoemulsification has become an established procedure.
Keywords: cataract surgery, outcomes, training, patient choice, independent treatment centres
Clinical outcomes for phacoemulsification surgery are still compared with the almost 10‐year‐old benchmark of the 1997–98 National Cataract Surgery Survey (NCSS).1 Cataract surgery also continues to be recurrently targeted by successive government drives to push down waiting list times. Present and future policy is committed to extending citizen “Choice” to healthcare. In October 2002 the UK government initiated the “patient choice” scheme, the pilot for which would offer choice to patients waiting for cataract surgery.2 Under the scheme patients waiting for longer than six months for routine cataract surgery were given the option of choosing to have the operation performed locally or at a different hospital with a shorter waiting list.2 The scheme has subsequently been extended to routine surgery in other surgical specialties in addition to ophthalmology—plastic surgery, ENT, general surgery, obstetrics and gynaecology. The UK Department of Health plans to expand the Patient Choice scheme within the National Health Service (NHS).3 Bookings are being made electronically using “choose and book” software even before patients leave the GP surgery. By the start of 2006, already the vast majority of Primary Care Trusts were offering patients a choice of at least four providers in 14 specialties.3 The operating framework for 2006/7 is committed to extending choice to any NHS Foundation Trust, nationally procured independent treatment centre or other nationally approved independent sector treatment centre provider (IS‐TC).4
Cataract was the flagship of the patient choice scheme. Given demand for this operation, an ageing population, and official government commitment to patient choice, it will continue to receive attention under the choice scheme when waiting lists increase again above waiting time targets, which are being continually shortened. Surgery on choice schemes is provided by a variety of high throughput models in both the NHS and independent sectors. Most of these models reduce opportunities for training. One exception to this is when surgery is performed in slots on training lists supervised by NHS Consultants. However there are no studies published in the peer‐reviewed literature comparing results with nationally accepted standards. Questionnaires suggest favourable public and patient perceptions on patient choice, as well as out‐of‐hours clinics, but there is little information on user satisfaction with choice in the independent peer‐reviewed literature.5,6,7,8,9
The Western Eye Hospital (WEH), in the West End of London, performed the first operation on this scheme in October 2002, with patients travelling from a variety of referring units in South, North and East London, and further afield from Essex and Surrey. The WEH is a busy teaching hospital where training is a high priority, and where cataract surgery on patient choice is performed on consultant‐supervised training lists. We asked whether the existing benchmark of the NCSS is out‐of‐date in the context of whether good outcomes on patient choice are compatible with surgical training.
Methods
Three main outcome measures were used: standard clinical outcomes on visual improvement, complications and patient satisfaction. Pre‐operative, operative and post‐operative data on the first 1000 consecutive patients undergoing cataract surgery on patient choice between October 2002 and September 2004 were entered onto an ongoing electronic database (customised by Medisoft®). All operations were performed on a consultant‐supervised operating list, with the consultant performing and/or supervising trainees (Senior House Officer (SHO), Specialist Registrar(SpR), Fellow) in one, two or three operating theatres.
Data was collected and entered by a trainee ophthalmologist (FHZ). The data was extracted with the assistance of Medisoft® by one of the authors (FHZ), and analysed (FHZ, MCC, PAB). As in the NCSS of 1997–98,1 data was collected and inputted both prospectively and retrospectively. The first data entry began at surgical pre‐assessment, and the last on the last visit to outpatients, or casualty in the case of complications, whichever was latest. No post‐operative details were inputted less than two weeks from the date of surgery.
Consecutive subgroups of 150 and 100 patients, respectively before and after surgery, were questioned specifically about their level of satisfaction with having their operation performed on patient choice. This used a modified validated patient satisfaction questionnaire based on PSQ‐III (long‐form) applied at surgical pre‐assessment and two weeks after surgery (FHZ, BJB, PAB).10,11 The questionnaire stresses delivery, courtesy, accessibility and confidence in the provision of healthcare; irrelevant questions pertaining to cost effectiveness (questions 4, 10, 14, 24, 27,32,44), accident and emergency [28] and questions concerning political issues in healthcare [28] were eliminated.
Results
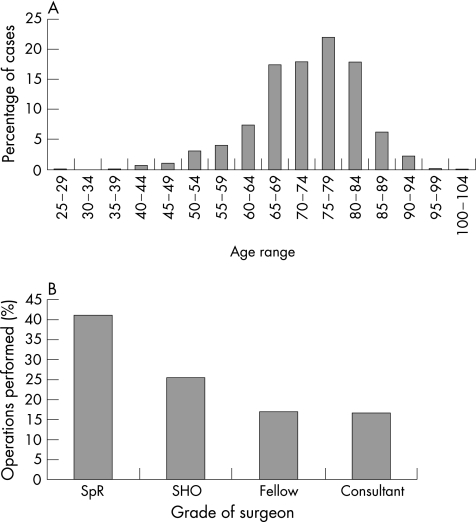
Patients had a mean age of 75–79 and 53% were female (fig 1A).
Figure 1 (A) Age distribution of patients undergoing surgery; (B) Percentage of operations performed by grade of surgeon. Specialist Registrar (SpR); Senior House Officer (SHO).
Ancillary data
Day cases accounted for 96% of operations.12 Mean length of admission for inpatients was one night. In total 92% of all operations were performed under local anaesthetic with a senior anaesthetist present on‐site; the remainder of operations were done under general anaesthetic. Overall, 63% of cases were performed under regional orbital blocks, 27% regional sub‐Tenon's blocks, 2% topical and 8% under general anaesthesia; ophthalmologists were much more likely to administer a sub‐Tenon's or topical block compared with anaesthetists.
Mean follow‐up was 48 days following surgery (7 days to 9 months), most commonly 2 weeks (mode). Some patients had follow‐up for their first eye while being assessed for their second eye. Grade of first surgeon was Specialist Registrar (SpR) (41%), Senior House Officer (SHO) (25.5%), Fellow (17.0%) and Consultant (16.5%) (fig 1B).
Visual outcomes
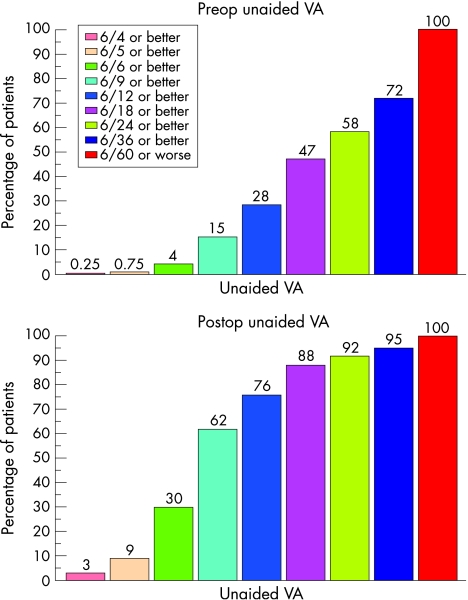
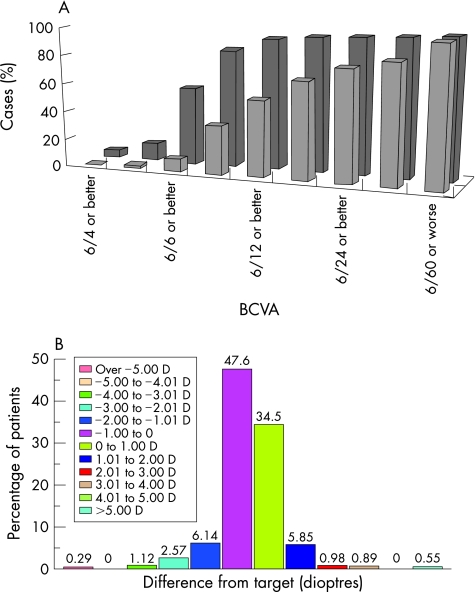
Uncorrected visual acuity was improved by cataract surgery for all levels of visual acuity (fig 2). Pre‐operative uncorrected visual acuity was 6/36 (mode) and post‐operatively this was 6/9. Overall 76% of patients had an improvement in uncorrected visual acuity to 6/12 or better. Best corrected visual acuity (BCVA) also showed an improvement for all levels of visual acuity (fig 3A). Pre‐operative BCVA was 6/12 (mode) and post‐operatively this was 6/9. Overall 93% of patients had an improvement in BCVA to 6/12 or better.
Figure 2 Cumulative bar charts showing uncorrected visual acuity before (above) and after (below) surgery.
Figure 3 (A) Cumulative bar chart showing improvement in best corrected visual acuity; (B) Deviation of post‐op refraction from target refraction
In 2% of patients BCVA was 6/60 or worse before and after cataract surgery, out of which only two had no improvement in Snellen vision following surgery. One had a chronic macula‐off retinal detachment detected at surgical pre‐assessment and the other had age‐related macular degeneration and hazy ocular media. Both cases were informed pre‐operatively of their very guarded prognosis, but still wished to proceed. The patient with AMD had a subjective improvement in vision following surgery.
Mean pre‐operative K readings were 43.00–43.99 D ( mean of K1 and K2). Deviation of post‐operative refraction from target refraction is shown in fig 3B and in table 1.
Table 1 Deviation of post‐operative refraction from target refraction.
| Change from predicted refraction | Cumulative % of cataract operations |
|---|---|
| +/− 1 D (+/−0.5 D) | 82.1 (65.7) |
| +/− 2 D (+/−1.5 D) | 94.1 (91.3) |
| +/− 3 D | 97.6 |
| +/− 4 D | 99.7 |
| +/− 5 D | 99.7 |
| +/− 6 D | 100 |
Over 80% of cases were within +/− 1 D of target refraction, and 65.7% within +/−0.5 D of target refraction.
Complications
The total incidence of complications was 8.7% (table 2).
Table 2 List of complications.
| Event | Associated events | Frequency % (no) |
|---|---|---|
| Vitreous loss | Posterior capsule tears progressed to dropped nucleas in one case (0.1%) and to retinal detachment in two cases (0.2%) | 1.1% (11) |
| Endophthalmitis | 0.1% (1) | |
| Iris trauma | 1.2% (12) | |
| Clinical cystoid macular oedema | 1.2% (12) | |
| Wound leaks | One progressed to re‐operation with formal wound revision | 11% (11) |
| Posterior capsule opacity or plaque | 0.8% (8) | |
| Posterior capsule tear without vitreous loss | 0.4% (4) | |
| Progression of diabetic retinopathy | 0.3% (3) | |
| Hyphaema | 0.1% (1) | |
| Scleritis | 0.1% (1) | |
| Persistent post‐operative uveitis | 11% (11) | |
| Persistent corneal oedema | 0.7% (7) | |
| Persistent raised intraocular pressure | 0.3% (3) | |
| Retrobulbar haemorrhage | 0.1% (1) | |
| Ptosis | 0.1% (1) | |
| Any of the above events | Any of the above events | 8.7% (87) |
Overall there were 87 distinct complications occurring in 69 patients. The risk of any given patient listed for phacoemulsification developing a complication is therefore 6.9%.
So as to enable comparison with previous large studies, the following were counted as “major” complications (table 3): vitreous loss, endophthalmitis, iris trauma (significant and noted during surgery or post‐operatively for example prolapse).
Table 3 Incidence of major complications compared to similarly large studies (see text).
| Complication | WEH | MEH13 | NCSS1 |
|---|---|---|---|
| 2004 | 2003 | 1997–98 | |
| Overall | 2.4% | 2.4% | 5.3% |
| Vitreous loss | 1.1% | 0.7% | 4.4% |
| Endophthalmitis | 0.1% | 0 | 0.1% |
| Iris Trauma | 1.2% | 1.7% | 0.77% |
aPersonal communication: audit of 2000 cases by Mr V Maurino, Clinical Lead, Moorfields St Ann's DTC13
Overall incidence of major complications is 2.4%
Posterior capsule tears associated with vitreous loss accounted for 1.1% of all complications: one case progressed to dropped nucleus (0.1%), and two to retinal detachment (0.2%), both in high myopes which were detected post‐operatively. There were no cases of retinal detachment without posterior capsule tear. Incidence of endophthalmitis was 0.1%, and of iris trauma 1.2%, including three cases of iris prolapse, of which one occurred post‐operatively requiring further surgery. There were no cases of suprachoroidal haemorrhage.
Complications of intermediate severity included 12 cases of clinical cystoid macular oedema (CMO), 11 wound leaks, of which one was associated with post‐operative hypotony and one required formal would revision, eight cases of early posterior capsule opacification or plaques, of which three needed Nd‐YAG laser capsulotomy within six months of surgery, four posterior capsule tears with no vitreous loss, three cases of progression of diabetic retinopathy one requiring argon laser, one hyphaema, and one case of post‐operative scleritis.
Anaesthetic complications were one case of retrobulbar haemorrhage and one ptosis. There were no complications due to general anaesthesia. There were 21 minor complications: 11 cases of persistent uveitis (beyond 1 month), seven cases of persistent corneal oedema and three of persistently raised IOP (> 21 mm Hg).
Complications rates by grade of surgeon were highest in SpRs (6.5%), then Fellows (4.5%), followed by SHOs (2%) and then Consultants (0.1%).
Patient satisfaction
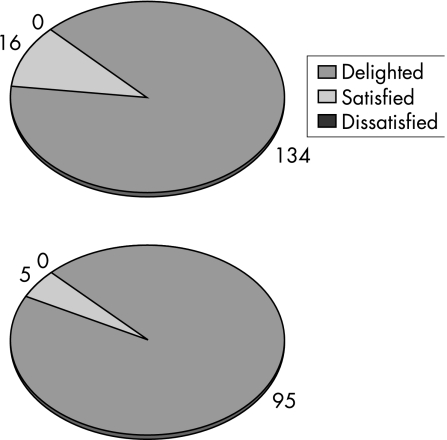
All patients were satisfied with their pre‐operative management on patient choice: 89% were delighted and 11% simply satisfied; no patients were dissatisfied (fig 6). Post‐operatively, patient satisfaction with had their cataract surgery performed under patient choice was also 100%, of which 95% were delighted and 5% simply satisfied; no patients were dissatisfied (fig 4). Travelling time, travel delays, and lack of notes from the referring trust were the most frequently cited concerns of patients.
Figure 4 User satisfaction with “patient choice” before surgery (top) and after surgery (bottom).
Discussion
Cataract surgery under “patient choice” on supervised training lists is associated with a visual outcome and an incidence of complications generally better than the published national average in the NCSS (1997–98),1 and user satisfaction is high. A best visual acuity of 6/12 or better was obtained in 93% of cases, compared with a quoted range of 77 to 92% in the centres participating in the NCSS.
Comparison of complications with previous large studies is complicated by a lack of uniformity in categorisation of complications between the previous large surveys and audits. The NCSS categorised complications according to pre‐operative, operative and post‐operative course to produce a comprehensive incidence of all complications. A similarly large study of 2000 patients did not include all minor complications which can be expected such as persistent uveitis.13 In the current study both these approaches were utilised to categorise all complications into major, intermediate and minor. Some complications in the NCSS were listed in a manner that while providing epidemiological data was out of the context of the risk to an individual patient clinically, for example iris emulsification was listed separately to an iris tear, though most or all cases of iris tear were likely due to iris phacoemulsification. Therefore, to obtain a more meaningful estimate of complication rates in a given patient undergoing surgery, we avoided counting associated complications separately, which can be misleading in establishing an accurate incidence of complications for practical purposes. This is relevant to calculating surgical risk pre‐operatively, which has subsequently become a topical area.12,14 Only distinctly separate events were counted as a distinct complication for example posterior capsule tear progressing to vitreous loss progressing to nucleas drop was counted as one complication, with the detailed events in this sequence noted as an “associated event”. This follows from the concept of risk assessment for an individual patient undergoing surgery, which while nothing new, is nonetheless of especial relevance at present with the new NHS consent forms, allocation of cases for training purposes and to assessment of hospital units' complication rates.12,13,14,15,16,17
It is routine practice for patients undergoing cataract surgery at the WEH to be told to return to the 24‐hour Eye Casualty at the Western Eye Hospital if they had problems, or to telephone at any time for advice. However there is still likely to be some under‐estimation of late complications such as posterior capsule opacification that come on late and present with insidious symptoms, although this does not greatly deter comparison with previous studies because this is a problem shared with them. In common with the other studies there will also have been some under‐reporting of complications that are known to be under‐diagnosed, for example post‐operative scleritis (of which we found only one case reported).18 Under‐diagnosis of complications is unlikely to be the cause of lower complication rates between this audit and the NCSS, since readily diagnosed complications were also much less frequent, for example hyphaema occurred in 0.1% of cases in this study yet in 0.5% of cases in the NCSS.
It is thus likely that the fall in the overall incidence of complications in this study compared to the NCSS is a direct consequence of greater surgical experience with phacoemulsification in the United Kingdom over the past 8 or 9 years and not to any methodological difference in data collection. Of note, this difference is particularly marked for major complications. This is further supported by the finding in this study of low complication rates for NHS Consultant Ophthalmologists (less than 1% as compared to 32% in the NCSS). In the current study, the incidence of major complications was similar to two other very large database searches which the Royal College of Ophthalmologists and the United Kingdom Society of Cataract and Refractive Surgeons had been bringing to attention in 2003–4. The first was an audit performed at Moorfields St Ann's Diagnosis and Treatment Centre (MEH) where surgery was performed mainly by NHS Consultants and the senior‐most trainees, and the other the UK Electronic Patient Record (EPR) cataract audit, which in common with the current study utilised the Medisoft® data collection and retrieval system.19 The incidence of major complications quoted in the NCSS of 1997–98 is thus very dissimilar with both the present study and two other large database searches previously presented to large UK audiences. The current study was peer‐reviewed for publication and went so far as to note even minor and intermediate complications. The incidence of major complications in this study was 2.4% compared to 5.3% in the NCSS. The overall incidence of complications in this study (8.7%) was lower than the NCSS of 1997–98 (32%).
The “improvement” in results compared to the previous standard of the 1997–98 cataract survey, and which was also published in this journal, is worth noting. Experience in countries like Sweden, where there is a national cataract database, suggest that in the future there are unlikely to be further improvements in overall complication rates from phacoemulsification in the UK, which is likely to have plateaued. Even very large studies of overall complication rates from cataract surgery such as the current study may not be published in the peer‐reviewed research literature again as they may not be perceived to be contributing new research data. Yet a useful up to date benchmark on endophthalmitis rates in particular will still be needed,20 for which the ongoing EPR figures may be accessed till a national UK cataract database becomes a reality.
Most other results in this study reflect only changes to local constraints and preferences since the 1990s. Only 96% of cases underwent day case surgery. Overall 92% of cases were performed under local anaesthesia, while this was 99% in the Pilot Electronic Cataract Survey.19 Only 2% of operations were performed under topical anaesthesia, a technique that is increasingly used for high throughput cataract lists and for teaching lists, and it is likely this technique may be much more prevalent in some other units, for example 99% of cases in Norwich.21 Complications from sharp needle techniques were very rare in this study, and none life‐threatening. The fact that only 27% of patients underwent sub‐Tenon's anaesthesia simply reflects the individual preferences of the large number of operating surgeons (almost 40) whose results were audited. Sub‐Tenon's technique is recognised as having lower complication rates compared to sharp needle techniques, and can safely be given using the surgeons' operating microscope. Unlike the vogue of much of the 1990s, it can reasonably be argued that technical advances and greater experience render it now neither cost‐effective nor indeed necessary anymore to employ a “senior anaesthetist” for every list.21
This study also shows that adequate consultant‐supervision of cataract surgery performed predominantly by trainees can be associated with outcomes at least as good (and usually much better) than those of the NCSS,1 and similar to a recent audit of work conducted at MEH St Ann's DTC,13 in both of which studies most surgery was performed predominantly by consultants and/or the senior‐most trainees as opposed to this study where over two‐thirds of operations were performed by closely supervised junior or middle‐grade trainees. The somewhat counter‐intuitive result of finding the highest complication rates amongst SpRs, followed by Fellows, and fewer in more inexperienced trainees (SHOs), may be explained by case selection bias. SpRs and Fellows are likely to perform more challenging cases under supervision, and might start using more advanced phacoemulsification techniques, whereas SHOs usually perform only the most straightforward operations. Moreover those in the SHO training grade (equivalent to junior and middle residents) are likely to have a higher level of supervision so it may be the case that complications are averted.
The current study found user satisfaction to be very high with cataract surgery performed under patient choice. This is not altogether surprising bearing in mind positive feedback from a survey by the Picker Institute of Europe.6 However questionnaire studies in general, including even the validated format used in the current study, must be interpreted with great caution, especially with cataract surgery. This is also important as healthcare policy now leans much more on subjective perceptions of patient satisfaction outcomes, as opposed to hard data on complication rates. An extensive literature review during the period of this study for the independent regulator of NHS performance suggests very high satisfaction rates exist following cataract surgery for obvious reasons.22 This review, by Kings College London, made it clear that questionnaires assessing patient satisfaction in any comparative manner need to fine‐probe patients' perceptions, and for this reason the validated format that we independently used was devised. This interjects a note of caution into currently quoted and extremely high patient satisfaction levels reported from the Netcare cataract IS‐TC as trumpeted by government. Furthermore, with regard to hard clinical outcomes from cataract surgery, these too have not been published in the peer‐reviewed research literature by the latter IS‐TC. To rebut this suggestion it may be argued that audit activity is generally not research—but exceptions do exist and a large audit scrutinised by senior peer reviewers in which outcomes considerably exceed the literature benchmark achieves publication status in a research journal as clinical science for obvious reasons, as indeed the current study proves. The lack of such an audit may be due to improper clinical risk management by IS‐TCs, which a recent review has flagged up as a problem of these mobile cataract teams who in the UK fail to make adequate provision or plan for the management of postoperative complications, leaving local NHS Consultant Ophthalmologists to diagnose and treat complications for operations performed by IS‐TC surgeons.23 This might skew any audit figures as may be forthcoming from IS‐TCs. The intention from government now is that many, if not all, NHS (in the English NHS System) referrals will be made via “choose and book”. But before “choosing” patients might also be expected to have the opportunity to see audit results for operations performed outside the supervision of NHS Consultants, especially since the latter have published such figures for care under their supervision herein.
Opinion and summary
There have been great advances in the practice and provision of modern phacoemulsification cataract surgery in the seven years since the NCSS in 1997–98, and yet this study is still quoted as the UK benchmark for acceptable rates of success and complications. We suggest that the findings of this and other studies should help to redefine what should now be expected of cataract surgery and to “set the bar higher” than the out of date standards for visual results and complication rates still widely accepted and cited. Initial rates of complications for cataract surgery are being challenged with much better results. Recently Kelly et al have reported a very low postoperative endophthalmitis rate of 0.55 cases per 1000 cataract extractions at a UK district general hospital, which is 50% lower than the NCSS.20
Cataract surgery under patient choice can clearly be compatible with training activity in receiving hospitals. However, it nevertheless has the potential to impact negatively on training in referring hospitals, especially if uncomplicated cases are selected for referral, a practice sometimes referred to as “cherry picking”. This study gives no information on the effect on referring hospital case mix and the effect that this may have on service and training in these units. This consideration is of not inconsiderable relevance to the quality of services that can and will be provided within the National Health Service at a time when outsourcing of cataract surgery to the independent sector is set to increase. At this time of radical change within how the NHS treats patients it should be reassuring for patients to learn that cataract surgery supervised by NHS Consultants is associated with results that set the benchmark.
Supplementary Material
Acknowledgements
We are grateful to Mr. V Maurino, Lead Consultant Surgeon, Moorfields St Ann's DTC, for granting us access to the cataract surgery audit presented at UKISCRS 2003.
Abbreviations
BCVA - best corrected visual acuity
IS‐TC - independent sector treatment centre
NCSS - National Cataract Surgery Survey
SHO - Senior House Officer
SpR - Specialist Registrar
WEH - Western Eye Hospital
Footnotes
We are grateful to St Mary's NHS Trust providing additional funds to facilitate the large volume of data collection and retrieval.
Competing interests: None.
This work was presented at the podium of the United Kingdom and Ireland Society of Cataract and Refractive Surgeons (UKISCRS) Annual Meeting, Chester, England, September 2004 and at the podium of the Royal Society of Medicine, London, June 2005
References
- 1.Desai P, Minassian D C, Reidy A. National cataract surgery survey 1997–8: a report of the results of the clinical outcomes. British Journal of Ophthalmology 1999831336–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Building on the best: Choice, responsiveness and equity in the NHS HMSO. 2003; CM 6079010160792X
- 3.Choice at Referral—Guidance Framework (www.dh.gov.uk)
- 4. The NHS in England: the operating framework for 2006/7 ( www.dh.gov.uk )
- 5.Magee H, Davis L, Coulter A. Public views on healthcare performance indicators and patient choice. Journal of the Royal Society of Medicine 200396338–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Questionnaire Surveys, Picker Institure‐ Europe http://www.pickereurope.org/
- 7.Churchill A J, Gibbon C, Anand S.et al Public opinion on weekend and evening outpatient clinics. Br J Ophthalmol. 2003;87: 257–8, doi: 10. 1136/bjo. 87. 3. 257. [DOI] [PMC free article] [PubMed]
- 8.Zaidi F H, Lee N. Public opinion favours out‐of‐hours clinics. Interviews challenge multi‐centre questionnaire (electronic response to Churchill et al. Public opinion of weekend and evening outpatient clinics. BJO 200387257–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feeney C L, Roberts N J, Partridge M R. Do medical outpatients want “out of hours” clinics? BMC Health Serv Res 2005547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haynes R, Gale S, Mugford M.et al Cataract surgery in a community hospital outreach clinic: patients' costs and satisfaction. Social Science and Medicine 2001531631–1640. [DOI] [PubMed] [Google Scholar]
- 11.RAND Health http://www.rand.org/health/surveys/PSQIII.html
- 12.Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol. 2004 Oct 881242–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maurino V. Moorfields St Anns DTC; United United Kingdom and Ireland Society of Cataract and Refractive Surgeons (UKISCRS), Chester, September 2003
- 14.Liu C. Risk stratification for the humble cataract. Br J Ophthalmol. 2004 Oct 881231–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aylward G, Larkin D, Cooling R. Audit of cost and clinical outcome of cataract surgery. Health Trends 199325126–129. [PubMed] [Google Scholar]
- 16.Ibrahim T, Ong S M, Taylor G J. The new consent form: is it any better? Ann R Coll Surg Engl. 2004 May 86206–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tuft S J, Minassian D, Sullivan P. Risk factors for retinal detachment after cataract surgery: a case‐control study. Ophthalmology. 2006 Apr 113650–656. [DOI] [PubMed] [Google Scholar]
- 18.Scott J A, Clearkin L G. Surgically induced scleritis following cataract extraction. Eye 19948292–297. [DOI] [PubMed] [Google Scholar]
- 19.The Royal College of Ophthalmologists Cataract surgery guidelines 2004
- 20.Kelly S P, Mathews D, Mathews J.et al Reflective consideration of postoperative endophthalmitis as a quality marker. Eye. 2005 Jul 13; (Epub ahead of print) [DOI] [PubMed]
- 21.Astbury N J. Personal communication.
- 22.Smith E, Ross F. Patient Experiences of Care Pathways: Cataract, Hip Replacement and Knee Arthroscopy. A Review of the Literature for the Commission for Health Improvement. Kings's College London. http://www.kcl.ac.uk/schools/nursing/nru/pdf/chi/PatientExperiences.pdf
- 23.Kelly S P, Astbury N J. Patient safety in cataract surgery. Eye 200620275–282. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.