Choroidal osteoma usually occurs in 20–30 year old, healthy, white women as a well‐defined, unilateral (75%), solitary, yellow orange, slow‐growing juxtapapillary lesion.1 This is the first time that a choroidal osteoma has been associated with Stargardt's dystrophy.
Case report
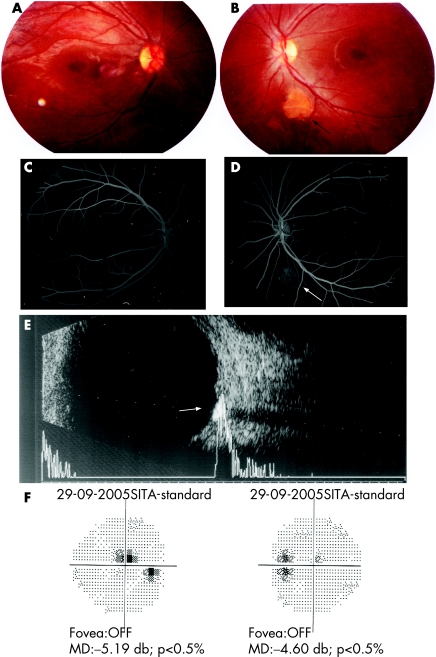
A 16‐year‐old girl presented with bilateral reduction of distance visual acuity (6/24) since 2 years. Near vision, colour vision, stereoacuity and anterior segments of both eyes were normal. Amsler grid testing in the left eye revealed a blur of the grid superotemporal to the foveal fixation point. Stereoscopic funduscopy revealed bilateral Stargardt's maculopathy (foveolar pigment epithelial changes with parafoveal orange‐coloured flecks; figs 1A,B), with an approximately 2.5 mm yellowish subretinal lesion situated 2‐disc diameters below the left optic disc (fig 1B). Fundus fluorescein angiography (FFA) revealed macular and perimacular hypofluorescence (dark choroid) with hyperfluorescence and late staining of the lesion inferior to the left optic disc (figs 1C,D). A/B ultrasound echography demonstrated a corresponding 0.9 mm thick, 2.5 mm diameter lesion with high, homogeneous internal reflectivity and marked shadowing of tissue signals posterior to the lesion (fig 1E), characteristic of choroidal osteoma. Serum calcium phosphate and parathyroid hormone levels, electroretinogram, electro‐oculogram and visual evoked potential tests were normal. Goldman's perimetry revealed bilateral central scotomas (fig 1F). FFA and B ultrasound scan were used to monitor the patient for subretinal choroidal neovascular membranes (CNVM) or haemorrhage.
Figure 1 (A,B) Fundus photographs of right and left eyes revealing bilateral bull's eye maculopathy and left juxta papillary calcific lesion (arrow). (C,D) Fundus fluorescein angiography of right and left eyes. Bilateral dark choroids and hyperfluorescent juxtapapillary lesion in left eye. (E) B ultrasound scan reveals shadowing posterior to the highly dense lesion (A ultrasound scan: sound attenuation posterior to the lesion). (F) Perimetric central field defects. MD, mean deviation.
Comment
This is the first report of a choroidal osteoma occurring in a patient with Stargardt's maculopathy. The clinical and ultrasound features were characteristic for a choroidal osteoma as described above.
Choroidal osteomas present as unilateral yellow–white to orange–red juxtapapillary choroidal lesions, which can occasionally extend into the macula or involve both choroids.1 The main differential diagnosis of choroidal osteoma is idiopathic sclerochoroidal calcification.
Sclerochoroidal calcification, common in 50–80 year old men, presents with bilateral (47% are unifocal), geographic, plaque‐like or mildly elevated yellow–white fundal lesions along the retinal vascular arcades,2,3 with rare multiple grey scleral lesions that resemble the choroidal lesion.3
Choroidal osteomas, common in women, increase in size in 41% of cases, and can cause a reported secondary poor visual acuity (⩽6/60) in 45% and 56% of eyes at the 5 and 10 years follow‐up, respectively.4 Spontaneous resorption of the lesion can occur. CNVM, subretinal fluid and haemorrhages complicate 33% of cases. Quantitative CT scans have demonstrated occult lesions in 90% of fellow eyes of clinically unilateral cases.1 Oval or round choroidal osetoma lesions with scalloped margins range from 2 to 22 mm in basal breadth and 0.5 to 2 mm in height, with pseudopoidal extensions, surface telangiectases and altered pigmentation.1 Central serous retinopathy has been associated with choroidal osteomas.1,5 FFA reveals an early patchy hyperfluorescence and diffuse late staining with vascular tufts on the vitreal surface of the tumour that fill in the early phases.1 CT scan demonstrates a radiopaque “bone‐like” density of the lesion. Osteomas seem hyperintense on T1‐weighted and hypointense on the T2‐weighted MRI images.1
Choroidal osteomas must be distinguished by ultrasound/CT scan from adult vitelliform macular dystrophy, serpiginous chorioretinitis, central serous chorioretinopathy, calcified granulomas, trauma, Cogan's plaques and chorioretinal scarring.1,2
Idiopathic choroidal calcification has been associated with Rieger anomaly, limbal dermoids, retinitis pigmentosa, spontaneous choroidal haemorrhage, organoid nevus, epidermal nevus, Bartter and Gitelman's syndromes.
The pathogenesis in choroidal osteoma is unknown. Although an association of choroidal osteoma with Stargardt's maculopathy may be coincidental, the association could be related to a dysfunction of the retinal pigment epithelium or choriocapillaries. Complicated extrafoveolar CNVM are treated with photocoagulation/photodynamic/transpupillary thermo therapy. Submacular surgery is indicated in subfoveolar CNVM or haemorrhage.1
Footnotes
Competing interests: None declared.
References
- 1.Kadrmas E F, Weiter J J. Choroidal osteoma. Int Ophthalmol Clin 199737171–182. [DOI] [PubMed] [Google Scholar]
- 2.Shields J A, Shields C L. CME review: sclerochoroidal calcification: the 2001 Harold Gifford Lecture. Retina 200222251–261. [DOI] [PubMed] [Google Scholar]
- 3.Honavar S G, Shields C L, Demirci H.et al Sclerochoroidal calcification: clinical manifestations and systemic associations. Arch Ophthalmol 2001119833–840. [DOI] [PubMed] [Google Scholar]
- 4.Shields C L, Sun H, Demicri H.et al Factors predictive of tumor growth, tumor decalcification, related choroidal neovascularisation, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol 20051231658–1666. [DOI] [PubMed] [Google Scholar]
- 5.Grand M G, Burgess D B, Singerman L J.et al Choroidal osteoma. Treatment of associated subretinal neovascular membranes. Retina 1984484–89. [PubMed] [Google Scholar]