Acute hydrops occurs in approximately 3% of eyes with keratoconus.1 The incidence increases dramatically in eyes with associated vernal keratoconjunctivitis.2,3 Neovascularisation rarely develops after resolution of acute hydrops although it has been reported with large area of involvement with hydrops associated with either close proximity to the limbal vascular arcades4 or intrastromal clefts.5 The association between patient age and area of involvement of hydrops, with the subsequent risk of development of neovascularisation, has not been adequately addressed in a prospective clinical trial.
In Saudi Arabia, patients present with severe keratoconus at a much younger age than in Western populations and have a higher incidence of associated atopic eye disease.2,3 The average age at the time of penetrating keratoplasty in our patient population is 19 years, with nearly one quarter of all cases performed in children 15 years of age or younger.3 Approximately one fifth of cases have severe vernal keratoconjunctivitis or seasonal allergic conjunctivitis, 30% have a history of hydrops prior to corneal transplantation,3 and one quarter of the cases have penetrating keratoplasty at 5 years of age or younger.3 In this study we evaluate the influence of early age on the severity and sequelae of acute hydrops.
Methods
After obtaining approval of the Institutional Review Board of the King Khaled Eye Specialist Hospital, all patients with keratoconus who presented to the emergency room with acute hydrops between February 1, 2004 and July 31, 2004 were enrolled in a prospective, observational clinical trial. A comprehensive ocular examination was performed at the time of presentation and after resolution of the hydrops. The location of acute hydrops was identified and measured using slit lamp examination of the hydrops and its relation to the distance from the limbus. Also, the presence or absence of vascularisation was noted at the time of hydrops. All patients were treated with a tapering regimen of topical fluoromethalone 0.1% and lubrication.
Results
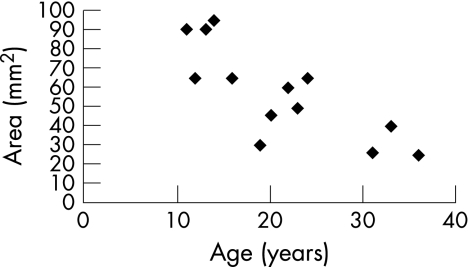
Thirteen patients (eight males, five females) were enrolled in the study (table 1). The median age was 20 years (range, 11–36). Complete resolution of hydrops occurred after a mean of 10.2 weeks (range, 6–13). Seasonal or vernal keratoconjunctivitis was present in nine (69.2%) eyes. There was an inverse correlation between age and area of involvement of corneal hydrops and the likelihood of developing neovascularisation after resolution (table 1, fig 1). Based on the Fischer exact test, patients 16 years of age or younger (5 out of 13) were significantly more likely to have an area of involvement of more than 90 mm2 (p = 0.03), to have involvement less than 1.0 mm of the limbal vascular arcades (p = 0.02), and to develop neovascularisation after resolution of the hydrops (p = 0.03) than older patients. Proximity of the hydrops of less than 1.0 mm from the vascular arcades was significantly correlated with the risk of development of neovascularisation (p = 0.03). Although atopic disease was present in all 3 eyes that developed neovascularisation, there was no significant correlation between the presence of atopic disease and the likelihood of development of neovascularisation.
Table 1 Case Summaries.
| Case | Age, gender | Hydrops size Max., Min. (mm) | Area (mm2) | Limbal Vascular arcade proximity (mm) | Duration of hydrops resolution (weeks) | Vascularisation after resolution | VKC/SAC |
|---|---|---|---|---|---|---|---|
| 1 | 11, F | 10, 9 | 90 | 0.2 | 13 | Yes | Yes |
| 2 | 12, M | 8, 8 | 64 | 1.0 | 11 | No | Yes |
| 3 | 13, M | 10, 9 | 90 | 0.2 | 12 | No | Yes |
| 4 | 14, F | 10, 10 | 100 | 0.1 | 12 | Yes | Yes |
| 5 | 16, M | 8, 8 | 64 | 0.1 | 12 | Yes | Yes |
| 6 | 19, F | 6, 5 | 30 | 1.5 | 8 | No | Yes |
| 7 | 20, M | 7, 7 | 49 | 1.5 | 9 | No | No |
| 8 | 22, M | 9, 7 | 63 | 0.2 | 9 | No | Yes |
| 9 | 23, M | 7, 7 | 49 | 1.7 | 6 | No | No |
| 10 | 24, M | 8, 8 | 64 | 1.0 | 11 | No | Yes |
| 11 | 31, F | 5, 5 | 25 | 2.0 | 10 | No | No |
| 12 | 33, F | 7, 6 | 42 | 1.5 | 9 | No | Yes |
| 13 | 36, M | 6, 4 | 24 | 1.3 | 11 | No | No |
VKC, vernal keratoconjunctivitis; SAC, seasonal allergic conjunctivitis; Max, maximum; Min, minimum
Figure 1 Relationship between patient age and area of involvement of acute hydrops
Discussion
The present study demonstrates a clear inverse correlation between age and the severity of acute hydrops, as well as the likelihood of developing neovascularisation after its resolution. This correlation could be explained on the basis of severity of allergy and rubbing or other reasons related to structural differences in developing corneas such as variations in the distribution and orientation of proteoglycan glycosaminoglycans complexes with time.6 Like previous reports of neovascularisation following involvement of hydrops near the limbal arcades,4 the use of topical steroids was ineffective in preventing neovascularisation in our three cases. Topical cyclosporine A may play a role in suppressing the development of corneal neovascularisation7 and should be evaluated prospectively, along with a more aggressive regimen of intensive topical corticosteroids, in a clinical trial of treatment of severe hydrops that extends within 1 mm of the limbal vascular arcades.
Footnotes
Competing interests: None.
References
- 1.Tuft S J, Gregory W M, Buckley R J. Acute corneal hydrops in keratoconus. Ophthalmology 19941011738–1744. [DOI] [PubMed] [Google Scholar]
- 2.Mahmood M, Wagoner M D. Penetrating keratoplasty in eyes with keratoconus and vernal keratoconjunctivitis. Cornea 200019468–470. [DOI] [PubMed] [Google Scholar]
- 3.Cameron J A, Al‐Rajhi A A, Badr I A. Corneal ectasia in vernal keratoconjunctivitis. Ophthalmology 1989961615–1623. [DOI] [PubMed] [Google Scholar]
- 4.Rowson N J, Dart J K G, Buckley R J. Corneal neovascularisation in acute hydrops. Eye 19926404–406. [DOI] [PubMed] [Google Scholar]
- 5.Feder R S, Wilhelmus W R, Vold S D.et al Intrastromal clefts in keratoconus patients with hydrops. Am J Ophthalmol 19981269–16. [DOI] [PubMed] [Google Scholar]
- 6.Smolek M K, Klyse S D. Cornea. In: Duane's Foundation of Clinical Ophthalmology. Volume 1. In: Tasman W, Jaeger EA, eds. Philadelphia: Lippincott, 1994;chapter, 813 [Google Scholar]
- 7.Lipman R M, Epstein R J, Hendricks R L. Suppression of corneal neovascularisation with cyclosporine. Arch Ophthalmol 1992110405–407. [DOI] [PubMed] [Google Scholar]