Uncorrected refractive error barely features when it comes to reports of global visual impairment.1 The reason is simple—the World Health Organization (WHO) definition2 classifies visual impairment and blindness according to visual acuity with “best possible correction”. Recent population‐based surveys have reported visual acuity in its many guises as uncorrected, presenting with habitual correction and best corrected. This work has exposed the enormous burden of uncorrected refractive error among industrialised3,4 and developing nations.5,6
The survey from Timor‐Leste reported by Ramke et al7(see page 860) in this issue of the BJO represents an important addition to the literature. This population‐based survey reports on uncorrected refractive error and presbyopia in adults (aged ⩾40 years) of Timor‐Leste. This country is poverty stricken and has recently emerged as an independent democracy from a period of great upheaval. What is it about this survey that is of particular interest?
First, this is one of the few population‐based surveys of refractive error that have reported on spectacle coverage for distance vision. We defined this term when reporting on spectacle coverage in the Bangladesh National Low Vision and Blindness Survey8 as Met refractive error need/(Met refractive error need+Unmet refractive error need)×100. The authors of the Timor‐Leste study have used this definition and have explored the assumptions involved with it, for distance and near vision— a useful exercise for further studies that intend to assess coverage. Unsurprisingly, distance spectacle coverage was higher among the urban and literate and those in paid employment, compared with rural, illiterate and those adults involved in subsistence farming.
Second, this survey is unusual in that it looked at the burden of presbyopia. The scale of this problem remains largely unknown in non‐European‐derived populations, with remarkably few population‐based studies having addressed this issue.9,10,11 There is a perception that presbyopia is of less importance in locations where reading is uncommon; however, the Timor‐Leste study7 and others9,11 have demonstrated a considerable unmet presbyopic need in largely rural locations. A recent study by Patel et al12 in rural Tanzania also demonstrated that uncorrected refractive error has a significant impact on vision‐related quality of life. There is a pressing need for more studies of presbyopia at a population level, as near vision, particularly the ability to read, is of great importance in socioeconomic development.
Third, the method used in this survey may not be familiar to readers. The rapid assessment for cataract surgical services method was used.13 This was developed to simplify the examination process by limiting the medical examination to cataract, and involves a torch, a visual acuity measuring device, a pinhole and a direct ophthalmoscope. This method has advantages of speed, simplicity, low cost and the involvement of local less experienced staff, but it is likely to underestimate the prevalence of coexistent ocular disease, in particular that of the posterior segment of the eye. Other studies of spectacle coverage8 have used a much more comprehensive examination method using best‐corrected visual acuity rather than pinhole‐corrected acuity to judge the effect of the refractive error. The limitations of using a pinhole to judge the presence or absence of refractive error were not discussed in the Timor‐Leste paper. A study comparing the results of rapid and more comprehensive methods would be useful, but until then caution should be exercised when comparing results from surveys using the two approaches. It would be interesting to know just how “rapid” the study was or the nature of the logistics involved, both of which would be of use to others planning such surveys. However, despite this, the survey was successful in obtaining a great deal of information that provides an overview of the areas of need, which could be explored later in more detail with a more comprehensive approach.
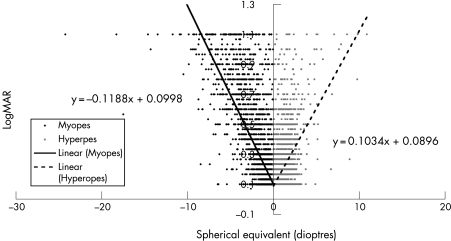
Fourth, the study used a cut‐off of 6/18 on account of the choice of sampling method. As an overview this is fine, but there is also likely to be a need among those with uncorrected refractive error but with better visual acuity. Most of the population‐based studies on refractive error so far have classified myopia or hyperopia as ±0.5 dioptres (D). Just how visually impaired does one become at a given refractive error? We modelled the effect of refractive error on visual acuity in the Bangladesh National Low Vision and Blindness Survey8 using refractive error data from the right eyes of 11 750 subjects (fig 1). Myopia (spherical equivalent) of –1.68 DS or more, or hyperopia of 2.04 DS or more, equated to a distance visual acuity of 6/12. Although these figures are admittedly pertinent to one particular population, such an analysis gives a more realistic approach to deciding on which cut‐off of refractive error to target. It is important for population‐based surveys to categorise the severity of refractive errors, rather than simply choose a cut‐off of 0.5 D on which to report.
Figure 1 Distance visual acuity logarithmic minimal angle resolution and refractive error (spherical equivalent) for 11 750 right eyes. Linear regression lines are given for myopia (solid line) and hypermetropia (dashed line). Data from the Bangladesh National Low Vision and Blindness Survey.8
Finally, this study yielded some interesting information on usage, cost and availability of spectacles. Remarkably little information exists on this issue in the literature.14 Gender differences were evident, with women less likely to have a presbyopic correction than men, yet this gender difference was not found for distance vision. Adults aged >70 years were seven times more likely to be uncorrected for distance than those aged 40–49 years. Clearly, there are important age and gender differences, which may reflect differences in cultural attitudes, perceptions and needs between these groups. It would have been interesting to explore the willingness to wear spectacles among these subgroups and among those who had a need rather than questioning all participants. “Need” is a complex issue—an illiterate farmer may not think that he or she needs a presbyopic correction, whereas an urban literate office worker may have quite a different view. Discontinued use has been shown to be a significant problem in some studies—for example, the Andhra Pradesh Eye Disease Study (APEDS)14—in which reasons included loss of spectacles, discomfort and a perception that they were unnecessary. A total of 13% of spectacle wearers in the APEDS Study and 81% in the Bangladesh National Blindness and Low Vision Survey8 were wearing incorrectly prescribed spectacles at the time of these studies. The prescribing pattern needs to be appropriate to the needs and perceptions of the population involved, so as not to introduce barriers to more widespread uptake or lack of continued uptake if the need persists. It was interesting to read in this Timor‐Leste paper that the main reasons underlying unwillingness to wear a correction were cosmesis and embarrassment. Inability to pay was of lesser importance. Distributing spectacles to everyone with a visually significant refractive error would be costly and probably wasteful. Perhaps it would be more appropriate to heighten awareness of uncorrected refractive error and demonstrate the benefits of correction. The individual could then make up his or her mind whether to wear a refractive correction in an environment where spectacles were available and accessible.
Many countries have insufficient numbers of personnel trained in refraction and a general lack of mid‐level ophthalmic personnel. Quality of refractive services, as well as quantity, is also critical in ensuring that the barriers to uptake are minimised. The Timor‐Leste paper provides an interesting overview of the issues of availability and accessibility for spectacle‐dispensing networks in this country, which, like many countries, is currently tipped in favour of the urban population.
If the burden of ocular disease is defined in terms of person‐years affected, the refractive error burden may exceed that of cataract.15 This paper by Ramke et al7 is an impressive attempt to gather a wealth of practical information using a rapid assessment technique. The information gathered provides the basis for action to reduce the impact of uncorrected refractive error in this population. Further research in this area is much needed.
Footnotes
Competing interests: None.
References
- 1.Resnikoff S, Pascolini D, Etya'ale D.et al Global data on visual impairment in the year 2002. Bull World Health Organ 200482844–851. [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization International statistical classification of diseases, injuries and causes of death, tenth revision. Geneva: WHO, 1993
- 3.McCarty C A. Uncorrected refractive error. Br J Ophthalmol 200690521–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor H R, Livingston P M, Stanislavsky Y L.et al Visual impairment in Australia: distance visual acuity, near vision and visual field findings of the Melbourne Visual Impairment Unit. Am J Ophthalmol 1997123328–337. [DOI] [PubMed] [Google Scholar]
- 5.Dandona L, Dandona R, Srinivas M.et al Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci 200142908–916. [PubMed] [Google Scholar]
- 6.Jadoon M Z, Dineen B, Bourne R R.et al Prevalence of blindness and visual impairment in Pakistan: the Pakistan National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci 2006474749–4755. [DOI] [PubMed] [Google Scholar]
- 7.Ramke J, du Toil R, Palagyi A.et al Correction of refractive error and presbyopia in Timor‐Leste. Br J Opthalmol 200791860–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourne R R A, Dineen B P, Noorul Huq D M.et al Correction of refractive error in the adult population of Bangladesh: meeting the unmet need. Invest Ophthalmol Vis Sci 200445410–417. [DOI] [PubMed] [Google Scholar]
- 9.Burke A G, Patel I, Munoz B.et al Population‐based study of presbyopia in rural Tanzania. Ophthalmology 2006113723–727. [DOI] [PubMed] [Google Scholar]
- 10.Nwosu S N. Ocular problems of young adults in rural Nigeria. Int Ophthalmol 199822259–263. [DOI] [PubMed] [Google Scholar]
- 11.Nirmalan P K, Krishnaiah S, Shamanna B R.et al A population‐based assessment of presbyopia in the state of Andhra Pradesh, South India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci 2006472324–2328. [DOI] [PubMed] [Google Scholar]
- 12.Patel I, Munoz B, Burke A G.et al Impact of presbyopia on quality of life in a rural African setting. Ophthalmology 2006113728–734. [DOI] [PubMed] [Google Scholar]
- 13.Limburg H, Kumar R, Indrayan A.et al Rapid assessment of prevalence of cataract blindness at district level. Int J Epidemiol 1997261049–1054. [DOI] [PubMed] [Google Scholar]
- 14.Dandona R, Dandona L, Kovai V.et al Population‐based study of spectacles use in Southern India. Indian J Ophthalmol 200250145–155. [PubMed] [Google Scholar]
- 15.Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ 200179237–243. [PMC free article] [PubMed] [Google Scholar]