Abstract
Cytochrome P450s (CYPs) represent a large class of heme-containing enzymes that catalyze the metabolism of multitudes of substrates both endogenous and exogenous. Until recently, however, CYPs have been largely overlooked in cancer drug development, acknowledged only for their role in Phase I metabolism of chemotherapeutics. The first successful strategy targeting CYP enzymes in cancer therapy was the development of potent inhibitors of CYP19 (aromatase) for the treatment of breast cancer. Aromatase inhibitors ushered in a new era in hormone ablation therapy for estrogen dependent cancers, and have paved the way for similar strategies (i.e. inhibition of CYP17) that combat androgen dependent prostate cancer. Identification of CYPs involved in the inactivation of anti-cancer metabolites of Vitamin D3 and Vitamin A has triggered development of agents that target these enzymes as well. The discovery of the over-expression of exogenous metabolizing CYPs, such as CYP1B1, in cancer cells has roused interest in the development of inhibitors for chemoprevention and of prodrugs designed to be activated by CYPs only in cancer cells. Finally, the expression of CYPs within tumors has been utilized in the development of bioreductive molecules that are activated by CYPs only under hypoxic conditions. This review offers the first comprehensive analysis of strategies in drug development that either inhibit or exploit CYP enzymes for the treatment of cancer.
Keywords: Cytochrome P450s, cancer, drug development, chemotherapy
Introduction
Cyotochrome P450s (CYPs) are a large ubiquitous family of proteins containing a single iron protoporphyrin IX prosthetic heme group. The majority of CYPs (designated Class I and II) act as versatile monooxygenases. These enzymes catalyze a multitude of reactions, including the hydroxylation of alkanes to alcohols, conversion of alkenes to epoxides, arenes to phenols, sulfides to sulfoxides and sulfones, and the oxidative split of C-N, C-O, C-C or C-S bonds.
Functionally, CYPs can be classified into two groups: those with specific roles in the metabolism of endogenous molecules such as hormones, and those that non-specifically process exogenous molecules (drugs, chemicals, natural products etc.). Both classes of CYPs offer potential targets in chemotherapeutic and chemopreventative strategies.
Most CYPs were once considered liver specific enzymes, but now their extrahepatic expression has been well established. It has long been known that CYP17 and CYP19--the enzymes responsible for the production of androgens and estrogens, respectively--are expressed in the testes, ovaries and adrenals. However, CYP19 has subsequently been found expressed locally in the adipose tissue of the breast, and indirect evidence suggests CYP17 may also be expressed in adipose tissue as well.1, 2 It is also now well established that expression of CYPs responsible for the metabolism of anti-cancer metabolites of vitamin A (all-trans-retinoic acid; ATRA) and vitamin D (1α, 25-dihydroxyvitamin D3; 1,25-D3) are induced by their substrates in target cells (including cancer).3–11 Members of CYP families 1, 2 and 3 have also been identified in both healthy and cancerous extrahepatic tissue.12–19 The enzymes in these families are involved in the metabolism of xenobiotic substances such as carcinogens, pro-carcinogens and chemotherapeutics.20–23 Of note, CYP1B1 and, more recently, CYP2W1 have been identified as having tumor-specific expression.15, 17, 18, 24, 25
These observations have lead to a greater appreciation for the role of CYPs in tumor formation and development. Targeting of these enzymes with natural or synthetic small molecules offers potential benefits in cancer prevention and therapy. Because crystal structures for nearly all CYPs are yet to be determined, drug design strategies rely on the knowledge of substrate structure and the enzyme’s mechanism of action. Strategies to target these enzymes include: i. designing molecules that inhibit the enzymes; ii. designing prodrugs that are activated by the enzymes; iii. immuno-based therapies that target immune responses towards the enzymes; iv. genetic therapy strategies to express specific CYPs in cancer cells.26 This review will focus on the small molecule based approaches (i. and ii.) being employed to target CYPs involved in hormone, vitamin, and xenobiotic metabolism for the treatment and prevention of cancer (Fig 1).
Figure 1.
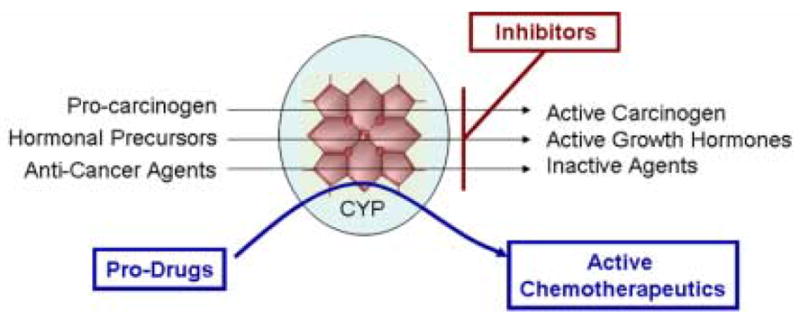
Potential strategies targeting CYPs for cancer therapy and prevention
CYPs and Hormone Dependent Cancer
Aromatase (CYP19)
The development of aromatase inhibitors for the treatment of breast cancer (BCa) represents the paradigm of success of CYP inhibition in cancer therapy. For years, the standard pharmacological treatment for hormone dependent BCa in post-menopausal women was blocking estrogen (E) binding to the estrogen receptor (ER) with tamoxifen. ER is a nuclear hormone receptor that is normally activated by E to recruit co-activators and induce transcription of target genes. By blocking E binding to the ER, tamoxifen prevents E-induced proliferation. Unfortunately, tamoxifen, although an important advance in BCa therapy, has many drawbacks. First, it is a partial ER agonist in many tissue types,27 which has been correlated with a 3-fold increase in the incidences of endometrial cancer in patients receiving the drug.28 Furthermore, resistance to tamoxifen therapy inevitably results.27 An alternative approach to tamoxifen treatment is inhibition of estrogen synthesis. The target for such therapy is the enzyme aromatase, which catalyzes the rate limiting step in the conversion (aromatization) of androgens to estrogens (Fig 2). Aromatase is expressed in many tissues throughout the body, including adipose and muscle, which are the main sites of estrogen synthesis in post-menopausal woman.1 Therefore, surgery to remove endocrine glands is ineffective, and inhibition of estrogen production requires a systemic pharmacological approach.
Figure 2.
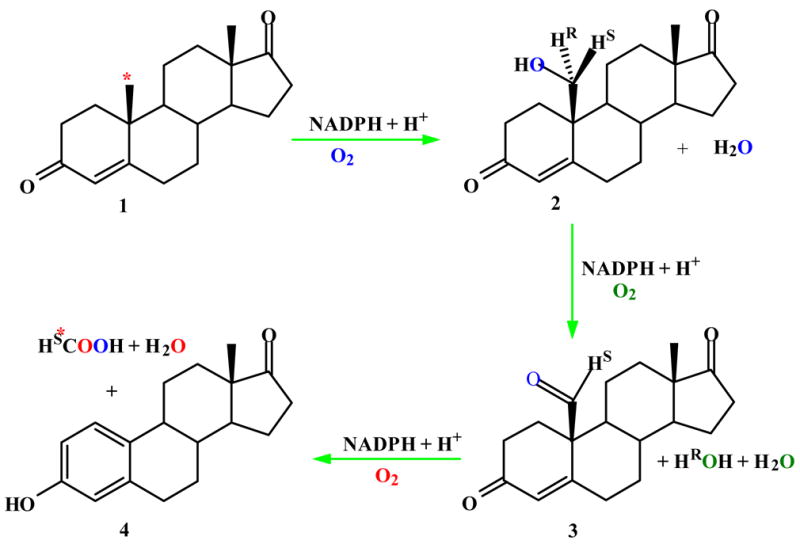
Biosynthesis of estrogens from androgens catalyzed by CYP19 (aromatase).
The first successful aromatase inhibitor, 4-hydroxyandrostenedione (4-OHA, Formestane) was demonstrated by Angela Brodie and colleagues to have efficacy against breast cancer tumors in 1977.29 Since then, several selective inhibitors of aromatase have been developed (Fig 3). These include fellow steroidal inhibitor 6-methylenandrosta-1,4-diene-3,17-dione (exemestane) as well as two non-steroidal triazoles, letrozole (femara) and anastrozole (arimidex). All four of these inhibitors are approved for the treatment of BCa, and have been shown in clinical trials to be more effective as a first line therapy than tamoxifen for post-menopausal women with hormone-sensitive BCa.30 A great deal of work is still being done in this field to optimize the efficacy of aromatase inhibitors both alone and in combination with other treatments, but these studies are beyond the scope of discussion here. Despite the obstacles that lay ahead, it seems clear that aromatase inhibitors represent the first successful class of cancer therapeutics specifically designed to target a CYP enzyme.
Figure 3.
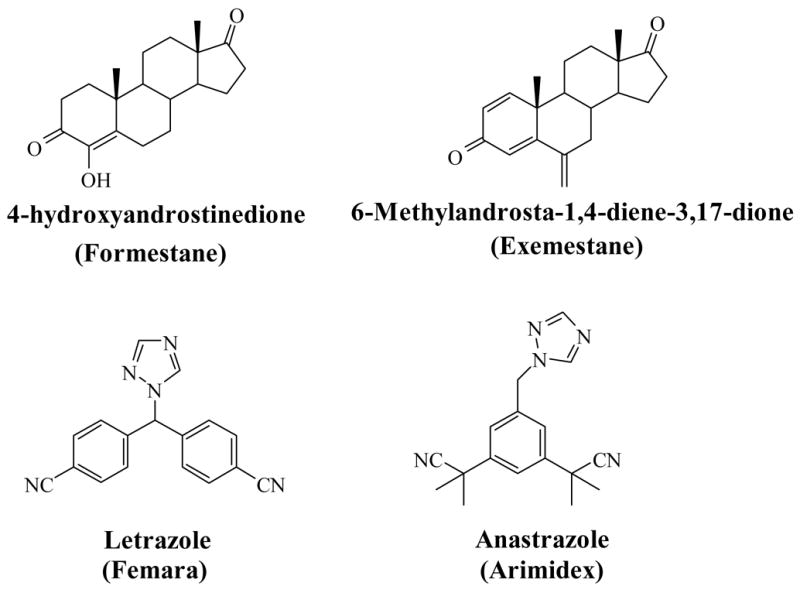
Chemical Structures of Aromatase Inhibitors
17α-Hydroxylase,C17,20-Lyase (CYP17)
The clinical success of aromatase inhibitors raises the question of whether a similar strategy could be employed for the treatment of androgen dependent cancers such as Prostate Cancer (PCa). In 1941, Charles Huggins and colleagues first demonstrated the benefits of hormone deprivation therapy in prostate cancer.31, 32 To this day, androgen ablation remains the standard treatment for advanced PCa.
At the molecular level, androgens, mainly testosterone (T) and dihydrotestosterone (DHT), bind to the androgen receptor (AR) in target cells and initiate transcription of genes involved in cell proliferation and survival.33, 34 Generally, androgen withdrawal therapy is carried out via treatment with LHRH or GnRH agonists and anti-androgens (AR antagonists, e.g. bicalutamide, flutamide). Unfortunately, LHRH and GnRH agonists fail to prevent synthesis of testosterone by the adrenal glands (site of about 10% of total androgen production) and anti-androgens can act as weak agonists in prostate cancer cells expressing mutated and/or over-expressed AR.35 In addition, combination therapy with anti-androgens seems to fail to extend survival rates in patients with advanced PCa, with response times ranging for only 12–33 months.36 It has been shown that patients developing resistance to anti-androgen therapy maintain levels of T and DHT in their cancerous tissue at levels sufficient to activate the AR, and that an increase in AR mRNA was the only change consistently associated with anti-androgen resistance.35, 37 Taken together, these results suggest that androgens play a role even in so called hormone-refractory PCa. Furthermore, recent experiments suggest the possibility of androgen production in adipose tissue.2 Thus, compounds that can systemically inhibit the production of androgens, similar to the systemic inhibition of estrogen production in BCa, may prove to be more effective in the treatment of PCa.
The last step in the production of T requires two sequential reactions both catalyzed by the same enzyme, 17α-hydroxlase/17,20-lyase (CYP17; Fig 4).38 Therefore, CYP17 has become the target of interest for systemic inhibition of androgen production. Ketoconazole (Fig 5), an anti-fungal agent that non-specifically inhibits a broad range of CYP enzymes, has been used clinically as a second line therapy for advanced hormone refractory PCa39 and showed efficacy in patients no longer responding to treatment with the anti-androgen flutamide.40 Owing to its lack of specificity for CYP17, ketoconazole treatment is, unfortunately, limited by toxicity. Clinical trials using low dose ketoconazole (LDK) co-treated with glucocorticoids and chemotherapeutics or androgen withdrawal therapies have shown similar efficacy to high dose ketoconazole (HDK) with reduced toxicity.41–43
Figure 4.
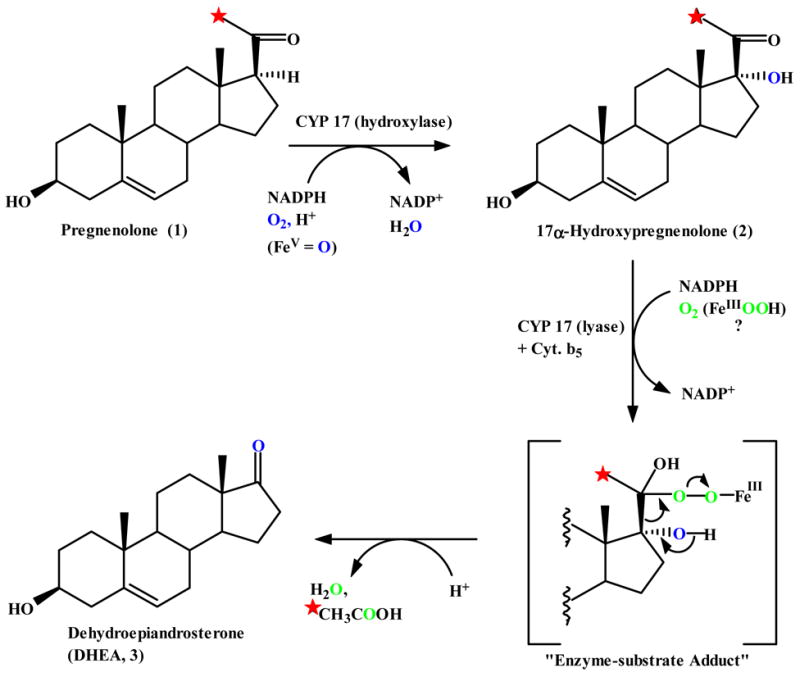
Biosynthesis of Androgens
Figure 5.
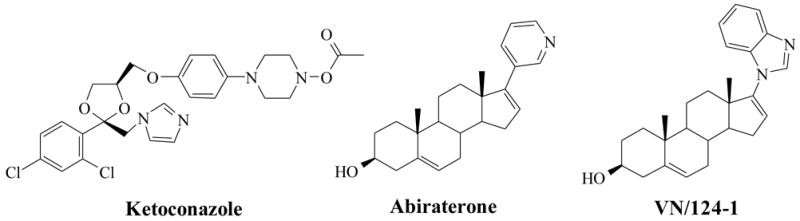
Inhibitors of CYP17. Ketoconazole is a broad range CYP inhibitor while abiraterone and VN/124-1 are designed as specific CYP17 inhibitors.
Despite the potential therapeutic benefits of LDK, development of more potent and selective inhibitors of CYP17 would clearly offer a therapeutic advantage over ketoconazole. One such molecule, abiraterone (Fig 5), has already entered Phase II clinical trials. At the 2007 American Association for Cancer Research Annual Meeting, Attard et al. reported exciting Phase II results for abiraterone acetate (pro-drug of abiraterone) showing PSA responses (≥50%) in 11/18 hormone-refractory patients and a drop in circulating T levels from castrate levels (<50ng/dl) to undetectable levels (<1ng/dl)44. Our laboratory has done extensive research in this field as well, and has developed several molecules that inhibit both CYP17 and the AR directly. One of these compounds, a 17-benzoimidazole called VN/124-1 (Fig 5), has shown superb anticancer properties both in-vitro and in-vivo.45 In fact, VN/124-1 is the only CYP17 inhibitor/antiandrogen to date that has been shown to inhibit prostate cancer tumor growth in-vivo more effectively than castration.45 VN/124-1 has recently been licensed to Tokai Pharmaceuticals Inc., Boston, MA, USA with hopes of following abiraterone into the clinic within a few years. A more comprehensive review of this subject can be found in the several reviews written by our group and others regarding the development of CYP17 inhibitors.46–49
Inhibiting Vitamin Metabolism
25-Hydroxyvitamin D3-24-hydroxylase (CYP24)
Vitamin D is synthesized in the skin upon exposure to UVB radiation. One of Vitamin D’s active metabolites, 1,25-D3 (clinical formulation is known as calcitriol), acts as hormone, and like E and T, it binds to a nuclear receptor, the vitamin D receptor (VDR), and initiates transcription. Unlike T and E, however, 1,25-D3 has gained attention as an anticancer agent because of its ability to inhibit proliferation, promote differentiation, and induce apoptosis in many cancer cell types including colon and prostate.50–53 The role of 1,25-D3 in cancer prevention is also supported by epidemiological studies that reveal a negative correlation between occurrence of certain cancers and sunlight exposure.54–56 This connection has been particularly well documented in colon cancer where it has recently been suggested by Grant and Garland that as much as 20–30% of colorectal cancer incidences are due to insufficient exposure to sunlight.57 Deactivation of 1,25-D3 occurs via hydroxylation at C-24 catalyzed by CYP24 (Fig 6).58 CYP24 is mainly expressed in the kidney, however, its expression has been demonstrated in other tissue types both healthy and cancerous 3, 59–63 and has been identified as a possible oncogene.64 CYP24’s role in tumor development and initiation is further supported by its apparent over-expression in lung and colon cancer compared to the corresponding healthy tissue.62, 63 Importantly, CYP24’s expression is inducible by treatment with 1,25-D3.3 This negative feedback mechanism limits the amount of 1,25-D3 present in tumor cells, and consequently the effectiveness of 1,25-D3 therapy. Therefore, regulation of CYP24 enzymatic activity may potentiate the anti-cancer benefits of 1,25-D3. In addition, clinical benefits of 1,25-D3 have been limited do to hypercalciuric and/or hypercalcemic side effects at therapeutically necessary concentrations.51 Targeting CYP24 provides the opportunity to increase endogenous levels of 1,25-D3, or reduce the effective dose of exogenous 1,25-D3, a therapeutic strategy that may help overcome the deleterious side effects associated with 1,25-D3 treatment.
Figure 6.
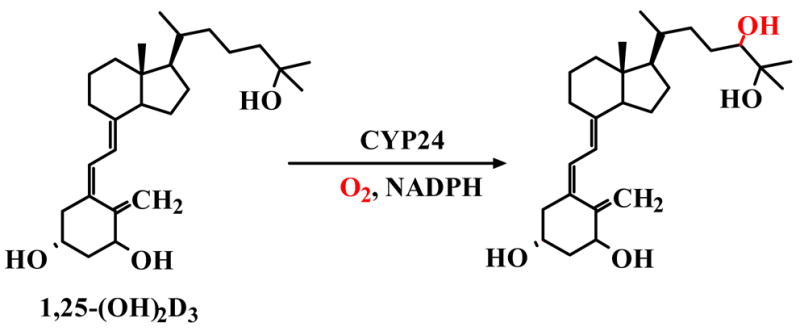
Metabolism of 1,25-D3 via C-24 hydroxylation catalyzed by CYP24.
Strategies to limit CYP24 action include down-regulation of the enzyme’s expression, as well as inhibition of the enzyme itself. Genestein (Fig 7A), a naturally occurring isoflavonoid with anticancer properties65, has been shown to inhibit the transcription of CYP24 as well as CYP27B1 (25-hydroxyvitamin D-1α-hydroxylase),61, 66 which catalyzes the hydroxylation at C-1 of 25-hydroxyvitamin D3 to 1,25-D3.67 Interestingly, co-treatment with the histone deacetylase inhibitor trichostatin A increased inhibition of CYP24 expression while restoring expression of CYP27B1.66 Because CYP27B1 has been shown to be expressed in cancer cells,68, 69 this co-treatment offers a unique strategy to maximize the amount of 1,25-D3 present in tumors by suppressing its metabolism while leaving its synthesis unhindered. Genestein, and various synthetic derivatives, have been evaluated extensively in pre-clinical studies and have shown promising results as chemopreventative and adjuvant chemotherapies65, 70 prompting the need for evaluation of these compounds in clinical trials.
Figure 7.
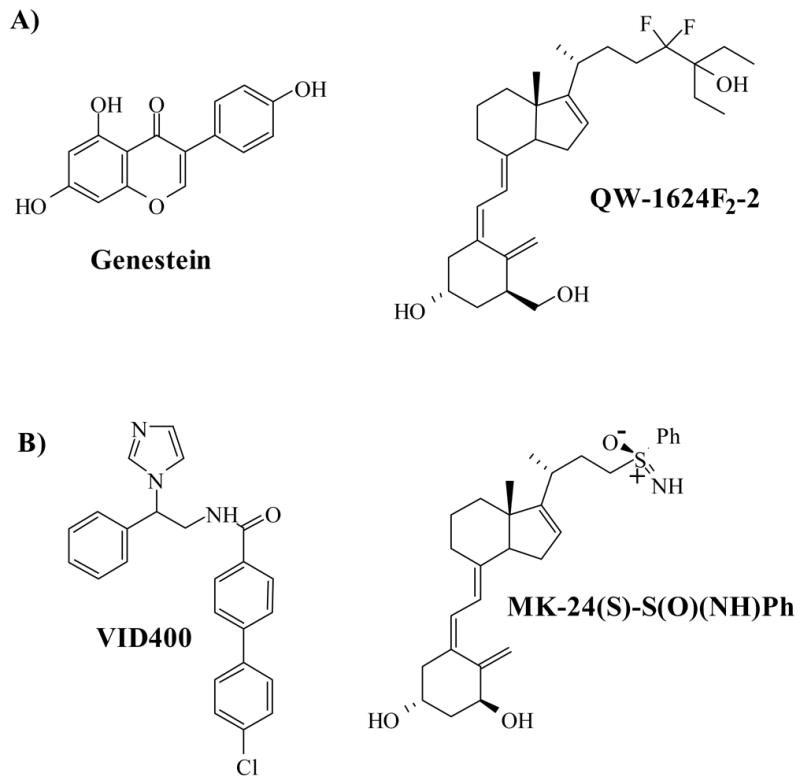
CYP24 Inhibitors. A: Genestein and QW1624F2-2 inhibit CYP24 expression B) VID400 and MK-24(S)-S(O)(NH)Ph inhibit CYP24 enzyme activity
Recently, Sundaram et al. described the ability of the synthetic 1,25-D3 analogue, QW-1624F2-2 (Fig 7A), to inhibit the expression of CYP24.71 QW-1624F2-2 was originally described by Posner et al. to mimic the actions of 1,25-D3 through binding of the VDR and activation of transcription.72 Importantly, however, it lacks the calcemic side effects of 1,25-D3. QW-162F2-2 seems to be as effective as 1,25-D3 in inhibiting cell growth, inducing its effect through modulation of cell cycle and apoptotic proteins.73 The molecule has also been shown to inhibit neuroblastoma xenografts in nude mice more effectively than the 1,25-D3 analogue, EB1089 (1α, 25-dihydroxy-22, 24-diene-24, 26,27-trishomovitamin D3).74 Furthermore, QW-1624F2-2 can inhibit the expression of CYP24 even in the presence of 1,25-D3, and has been shown to act synergistically with 1,25-D3 to inhibit cell proliferation.71 These pre-clinical results are compelling, and demonstrate a need to develop QW-1624F2-2 as a chemotherapeutic agent.
Obviously, small molecules that can bind to CYP24 and inhibit the enzyme’s activity directly may also prove to be effective treatments for some forms of cancer. Currently, the non-selective CYP inhibitor ketoconazole (Fig 5) is being used as an adjuvant therapy for hormone refractory prostate cancer, mainly for its inhibition of CYP17 (discussed earlier). However, the compound has also been shown to inhibit CYP24 and act synergistically with Vitamin D3 analogues in cell culture75, 76 and is being tried in combination with calcitriol in a phase I clinical trial.77 Liarozole (Fig 9), a CYP inhibitor initial designed to inhibit CYP26, has also been shown to inhibit 1,25-D3 hydroxylation and act synergistically with 1,25-D3 in androgen independent DU-145 prostate cancer cells.78 Unfortunately, both liarozole and ketoconazole are more potent inhibitors of CYP27B1 than they are of CYP24, greatly limiting their potential efficacy.
Figure 9.
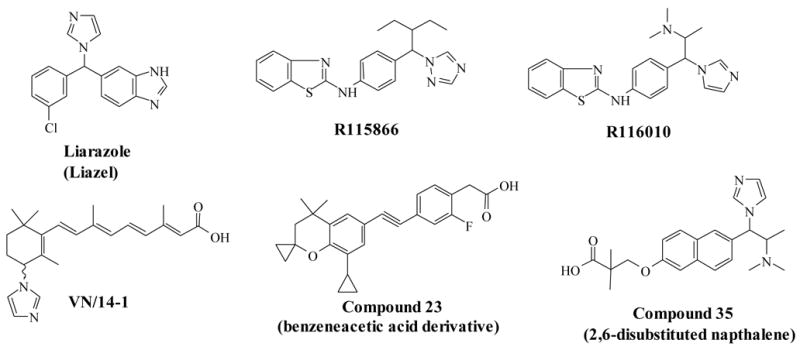
Retinoic Acid Metabolism Blocking Agents
Due to these limitations, selective CYP24 inhibitors offer a therapeutic advantage, and several groups have developed compounds to this end.76, 79–81 Schuster and colleagues have developed potent azol containing inhibitors of CYP24, and their lead compound, VID400 (Fig 7B), is highly selective for CYP24 over CYP27B1 (IC50’s of 15nM and 616nM respectively).82 VID400 is currently undergoing pre-clinical development as an anti-proliferation agent.79, 82, 83 A different class of CYP24 inhibitors, sulfone analogues of 1,25-D3, have recently been developed by Posner and colleagues.81, 84 Their lead compound, a NH phenyl sulfoximine called MK-24(S)-S(O)(NH)Ph (MK; Fig 7B), has shown great specificity for CYP24 with an IC50 of 7.4nM, compared to CYP27B1 (IC50 = 554nM) and CYP27A1 (IC50 > 1000nM). MK was recently shown to be effective in pre-clinical models of lung cancer, working synergistically with 1,25-D3 to inhibit growth of the nonsmall cell lung cancer cell line 128-88T.63
ATRA Hydroxylase (CYP26)
All-trans-retinoic-acid (ATRA) is the most active biological metabolite of vitamin A. Through its interaction with nuclear retinoic acid receptors (RAR), ATRA induces cellular differentiation of epithelial cells,85 and is being used for the treatment and prevention of several types of cancer.86–89 However, despite ATRA’s pre-clinical efficacy and its clinical success in the treatment of acute promyelocytic leukemia,90 the overall clinical efficacy of ATRA against human cancer has been disappointing.91, 92 ATRA’s success seems limited by the development resistance in patients..93 Like 1,25-D3, this resistance seems to be due, in part, by the rapid metabolism of ATRA in-vivo via C-4 hydroxylation (Fig 8). 94, 95 This realization has inspired researches to develop new classes of drugs designed to inhibit the metabolism of ATRA. Such drugs are often termed retinoic acid metabolism blocking agents (RAMBAs).
Figure 8.
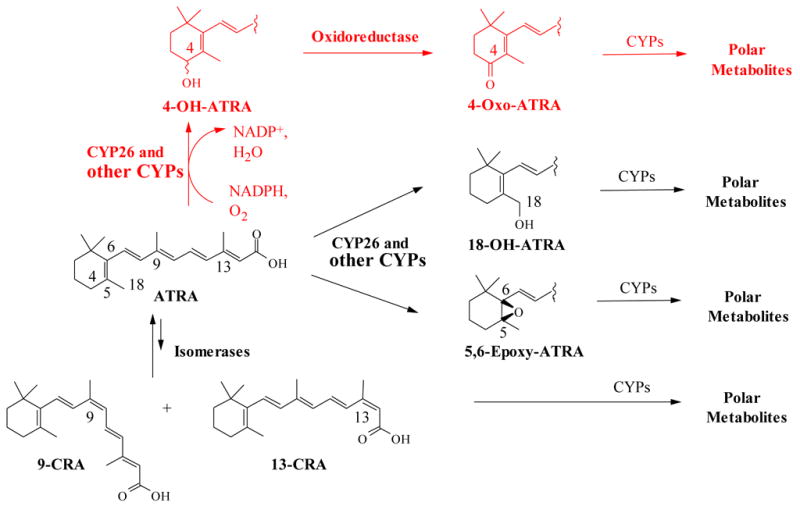
Metabolism of ATRA by CYP26.
Many CYPs have been identified that show the ability to metabolize ATRA via 4-hydroxylation including CYP2C8, CYP3A4, and CYP2C9.96–99 However, the specificity of these enzymes for ATRA is quite low.96–98 CYP26A1 and CYP26B1 have recently been identified as members of a new family of P450 enzymes that seem dedicated to ATRA metabolism.10, 11 Furthermore, CYP26A1 expression has been shown to be induced upon treatment with ATRA in cancer cells,4–9 and expression of the enzyme limits induction of apoptosis by ATRA.5 This phenomenon appears to be implicated in clinically acquire resistance to ATRA. In addition, certain cancers including acute promyelocytic leukemia, prostate, breast and non-small lung carcinomas express CYP26A at constitutively high levels5–7, 100–102 This has lead to a great deal of interest in the specific targeting of RAMBAs towards CYP26. However, non-specific inhibition of all enzymes involved in ATRA metabolism is an alternative strategy that hinges on the idea that non-specific metabolism of ATRA would prevent accumulation of the hormone to levels sufficient enough to induce the expression of CYP26.
Liarazole (LiazelTM; Johnson and Johnson Pharmaceutical Research and Development; Fig 9) is the first and only RAMBA to be evaluated clinically in patients with cancer. Interestingly, liarazole is a relatively weak inhibitor of CYP26 (IC50 ~ 2.2–6.0μM).103–107 Liarazole showed promise in pre-clinical models of prostate cancer 106, 108 and clinically as a second line therapy following failure of androgen deprivation.109 However, liarazole’s usefulness as a cancer therapy is unfortunately limited by its lack of specificity for CYP isozymes responsible for ATRA metabolism, as well as its moderate potency against CYP26 and is no longer being developed as an anti-cancer agent.10 Follow-up compounds R115866 and R116010 (Fig 9) are far more potent and selective inhibitors of CYP26 and have shown efficacy in pre-clinical cancer models.10 Work by our group, researchers at Allergan Sales Inc, and OSI Pharmaceuticals Inc have yielded novel compounds classified as azolyl retinoids, benzeneacetic acid derivatives, and 2,6-disubstituted napthalenes, respectively (Fig 9). All of these compounds have shown strong inhibition of CYP26. Additionally, the azolyl retinoids and the 2,6 disubstituted napthalenes have shown anti-cancer properties in pre-clinical models.10, 110, 111 In fact, one of our RAMBAs, VN/14-1, inhibits the growth of letrozole resistant breast cancer cells more potently than parental letrozole sensitive cells.112 These results indicate the potential usefulness of RAMBAs for hormone refractory cancers. Despite promising published pre-clinical results, no clinical trials have been undertaken to date with any RAMBA other than liarazole. However, plans are underway to advance our novel RAMBAs alone and in combination with histone deacetylase inhibitors for clinical trials in breast and prostate cancer patients. For more information on the development and utility of RAMBAs, please consult our group’s recent review on the subject (Njar et al., ref 10).
Exogenous Metabolizing CYP’s and Cancer
CYP1
Humans express three types of CYP1 enzymes: CYP1A1, CYP1A2, and CYP1B1. Members of this family are under the transcriptional regulation of the aryl hydrocarbon receptor (AhR), and are known to activate pro-carcinogens such as polycyclic aromatic hydrocarbons (PAHs). All members of the CYP1 family are expressed in extrahepatic tissues,113 but CYP1B1 is unique in that it is over-expressed in many tumor types relative to normal tissues.15, 17, 18 This insight has peaked a great deal of interest into CYP1B1.
Evidence for the role of CYP1B1 in tumorgenesis is supported not only by its increased expression, but also by its ability to activate several carcinogens in the chemical classes of PAHs, heterocyclic amines, aromatic amines, and nitropolycyclic hydrocarbons.114, 115 Furthermore, recent epidemiological studies have linked CYP1B1 polymorphisms to increased or decreased risk of certain cancers.116–119 It is also likely that CYP1B1, along with CYP1A1, plays a role in advanced carcinoma, as well, as the ability of these enzymes to metabolize chemotherapeutic agents may help tumors avoid chemotherapeutic induced cytotoxicity.120–122
Of most importance, however, is CYP1B1’s role in estradiol metabolism. It catalyzes the hydroxylation of estradiol primarily at the C-4 position. C-2 hydroxylation can also occur primarily through CYP1A2 and CYP3A4. However, C-4 hydroxylation seems to be the preferred pathway outside of the liver, and may play an important role in estrogen-related tumorgenesis.123 The reasons for this are two-fold. First, 4-hydroxyestradiol is a strong ER agonist, with a binding affinity for the estrogen receptor 1.5 fold greater than estradiol.124 Secondly, and more importantly, 4-hydroxyestradiol is subsequently converted to estradiol 3,4-quinone, which has been shown to bind DNA and form unstable adducts leading to mutations.123, 125
An obvious strategy for chemoprevention would therefore be the inhibition of CYP1B1. Studies with CYP1A1, CYP1A2, and CYP1B1 knockout mice demonstrated that animals lacking any one of these genes developed normally, and showed no noticeable deficiencies. Furthermore, CYP1B1 knockout mice showed strong resistance to 7,12-Dimethylbenz[a]anthracene (DMBA) induced tumor formation.126 These studies provide evidence for the potential efficacy and safety of a chemopreventative agent that blocks CYP1B1 expression or activity.
As previously mentioned, members of the CYP1 family are under the transcriptional control of AhR. AhR binds a diverse set of exogenous molecules, including carcinogens such as PAH’s and polyhalogenated hydrocarbons which are present in air pollution and cigarette smoke.127, 128 Upon binding, AhR translocates to the nucleus where it binds aryl hydrocarbon nuclear translocator (ARNT). The AhR/ARNT dimer regulates transcription of target genes.127 The ability of PAH’s and other carcinogens to induce CYP1 family expression is illustrated by experiments demonstrating elevated CYP1A1 and CYP1B1 expression in lung and urothelial tissue of smokers compared to non-smokers.129, 130 Because CYP1A1 and CYP1B1 are necessary for the activation of many carcinogens that induce CYP1 expression via AhR, treatment with antagonists of AhR seems to be a practical chemopreventative strategy.
Many natural products have shown promise for this indication. Recently, the flavonoid kaempferol (Fig 10A) was shown to inhibit agonist binding to AhR, as well as agonist induced AhR/ARNT/DNA complex formation and induction of CYP1A1 expression.131 Kaempferol also inhibited cigarette smoke condensate induced growth of immortalized lung epithelia cells (BEAS-2B) in a soft agar colony assay. In these studies, kaempferol inhibited the AhR with an IC50 of 28nM and cellular responses were seen at 10μM (~IC90). Other natural inhibitors of CYP1 family expression include 5,7-dimethoxyflavone, which inhibits both expression and activity of CYP1A1,132 and the stilbene phytoestrogen resveratrol (Fig 10A).133
Figure 10.
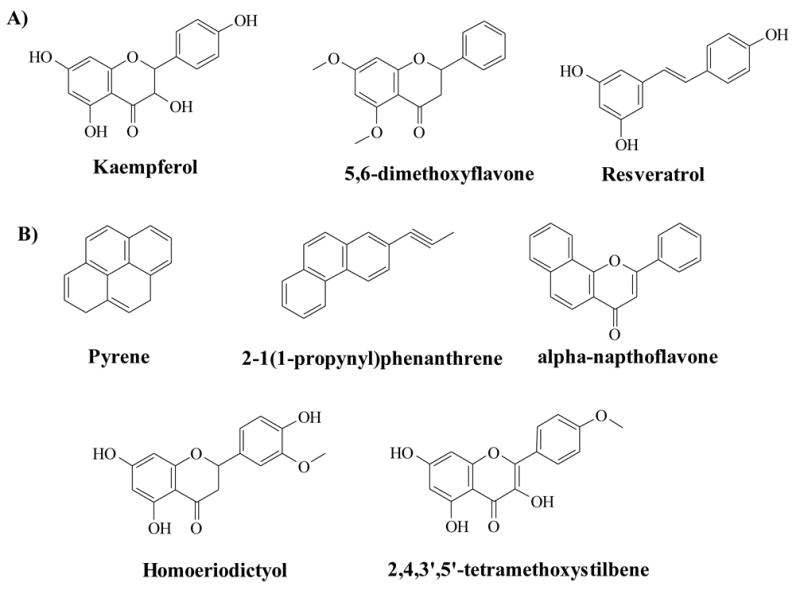
CYP 1 Inhibitors. A) Inhibitors of CYP1 family transcription (Ahr antagonists) B) Inhibitors of CYP1 family enzyme activity.
In addition to AhR inhibitors, a vast array of compounds, both natural and synthetic, have been evaluated for their ability to directly inhibit CYP1B1 enzymatic activity.115, 123, 134–137 Molecules that have been identified as potent inhibitors come from diverse chemical families including synthetic aromatics, coumarins, flavonoids, and stillbenes. Table 1 shows the IC50 values of various compounds shown to inhibit members of the CYP1 family, and Figure 10B shows the structures of representative compounds. Unfortunately, it remains unclear whether the inhibition of CYP1 family members by these compounds translates into chemoprevention in-vivo.
Table 1.
Inhibitors of the CYP1 family
| Compound | CYP1B1 IC50 (nM) | CYP1A1 IC50 (nM) | CYP1A2 IC50 (nM) | Reference |
|---|---|---|---|---|
| Pyrene | 2 | 41 | 7 | 134 |
| 2-(1-propynyl) phenanthrene | 30 | 150 | 60 | 134 |
| 3,3’,4,4’,5’-pentachlorobiphenyl | 11 | ND | ND | 135 |
| α-Napthoflavone | 5 | 60 | 6 | 134 |
| Acacetin | 7 | 80 | 80 | 136 |
| Homoeriodictyol | 240 | >4000 | >4000 | 136 |
| 2,4,3’,5’-tetramethoxystilbene | 6 | 300 | 3000 | 137 |
| 2-[2-(3,5-Dimethoxy-phenyl)- vinyl]-thiopene | 2 | 61 | 11 | 137 |
An alternative strategy for CYP1 based chemotherapies involves the activation of an inactive prodrug to a cytotoxic compound. It has been reported that resveratrol can be activated to an active anticancer agent, piceatannol, by CYP1B1 within cancer cells.138 Unfortunately, resveratrol has recently been shown to have limited anti-cancer activity in-vivo in an athymic mouse cancer model.139 New synthetic prodrugs specifically designed to be activated by CYP1A1 and CYP1B1 have been developed and have shown promise as novel approaches to cancer therapy.
One such compound, phortress, is a benzothiazole prodrug that has entered phase I clinical trials(Fig 11A).140 In the absence of cells, phortress, a hydrophilic lysil-amide, does not undergo hydrolysis, but is rapidly hydrolyzed in the presence of cells to its lipophilic amide parent compound 5F203. 5F203 is then taken up by sensitive cells where it acts as a potent AhR agonist, leading to the induction of AhR target genes (i.e. CYP1A1 and CYP1B1). It is believed that CYP1A1 then metabolizes 5F203 to generate reactive electrophillic species, which ultimately leads to DNA damage and cell death. The drug has shown tremendous pre-clinical results both in-vitro and in-vivo against sensitive tumors.140 Obviously, only AhR expressing cancer cells are susceptible to phortress, so patients will require screening to select those who might benefit from the drug.
Figure 11. Prodrugs activated by CYPs.
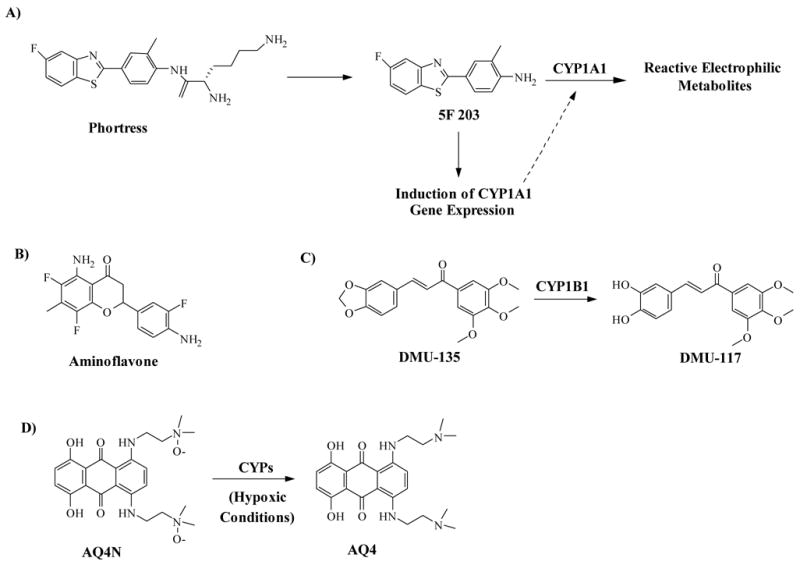
A) Phortress and its metabolite 5F203. 5F203 activates Ahr inducing transcription of CYP1A1, which activates the drug to a reactive electrophilic species. B) Aminoflavone is activated by CYP1A1 in a similar fashion as 5F203 C) DUM-135 and its active metabolite DMU-117. DUM-135 is activated by CYP1B1 to form its active metabolite, DMU-117 (a tyrosine kinase inhibitor). D) AQ4N and AQ4. AQ4N is activated by CYPs only under hypoxic conditions to form the active topoisomerase inhibitor AQ4
Aminoflavone (5-amino-2,3-fluorophenyl-6,8-difluoro-7-methyl-4H-1-benzopyran-4-one; Fig 11B) has recently followed phortress into phase I clinical trials. The compound is believed to function through a similar mechanism as 5F203.141 Interestingly, however, it has recently been shown that aminoflavone requires the expression of sulfotransferase A1 (SULTA1) to elicit a cellular response,142 suggesting aminoflavone activation may be more complex than previously thought.
It remains unclear what the long term effects of treatment with phortress or aminoflavone will have on patients. As discussed earlier, activation of AhR and induction of CYP1 family proteins is believed to be involved in the development of some cancers. Inducing CYP1 expression may induce more harm then benefit in the long run. Still, the developers of phortress have pointed out that the drug’s cell specific activation of AhR differs greatly from that of carcinogens, such as PAHs, and pre-clinical safety results demonstrated relatively low toxicity.140 Only time will tell if the exciting pre-clinical results of phortress and aminoflavone can translate to clinical efficacy.
Alternatively, prodrugs designed to be explicitly activated by the tumor specific CYP1B1 would offer the added safety advantage of not having to induce CYP1 enzymes. One such molecule, DMU-135 (3,4-Methylenedioxy-3’,4’,5’-trimethoxy chalcone; Fig 11C) has recently been described.143 DMU-135 is converted by CYP1B1 within tumors to form its active metabolite, DMU-117, a potent non-selective tyrosine kinase inhibitor (and potentially a COX inhibitor as well). DMU-135 is being developed as a chemopreventative agent, and has shown the ability to prevent tumor gastrointestinal tumor formation in the ApcMin+ mouse model without any sign of toxicity. DMU-135 represents the first prodrug specifically targeted for activation by CYP1B1.
CYP2
Many members of the CYP2 family have been identified in extrahepatic tissue.12, 14, 113 Of note, four are novel CYPs discovered by the Human Genome Project: CYP2S1, CYP2R1, CYP2U1 and CYP2W1.144 These enzymes play an important role in xenobiotic metabolism, but are also important in endogenous metabolism as well. For example, CYP2S1 can metabolize ATRA, and CYP2R1 is a vitamin D hydroxylase.144 The potential role of these enzymes in tumor development and progression remains unclear.
CYP2W1 is of particular interest, however, because it has recently been demonstrated as a tumor-specific CYP24, 25, especially in gastric and adrenal cancers. Little is known about CYP2W1, but arachidonic acid and indole have recently been identified as potential substrates.144, 145 Despite our limited knowledge of the enzyme’s function, its apparent tumor-specific expression is intriguing. Further research is needed to determine if this enzyme may be a potential target (either through inhibition or activation of prodrugs) for the prevention or treatment of gastric and adrenal cancers.
Bioreductive Prodrug AQ4N
The topoisomerase inhibitor prodrug AQ4N (1,4-bisan5,8-dihydroxyanthracene-9,10-dione; Novacea®, Fig 11D) exploits the expression of exogenous metabolizing CYP’s in tumor cells in a unique manner. Though it does not target a specific CYP enzyme, the local of expression of CYPs is required for its activation making it a notable strategy in CYP targeting for cancer therapy.
It is well established that hypoxic conditions often exist within the tumor microenvironment.146 AQ4N is activated to its basic amine, AQ4, only in the hypoxic tumor microenvironment by CYP3A4, CYP1A1, and CYP1B1.147 AQ4N is a weak DNA binder, but AQ4 interacts tightly with DNA and can penetrate surrounding cells increasing its efficacy within a tumor.147, 148 The bioreduction of AQ4N is strongly inhibited by oxygen, ensuring its activation only occurs under hypoxic conditions. Because hypoxic cells are resistant to chemo and radiotherapies, AQ4N is being developed mainly as an adjuvant treatment option.149–151 AQ4N is entering Phase Ib/IIa clinical trials.152
Conclusions
Great progress has already been made in the targeting of CYP enzymes in cancer therapy. For example, aromatase inhibitors have changed the way estrogen dependent cancers such as BCa are treated. This success has paved the way for similar strategies in inhibiting androgen production to combat AD prostate cancer. Molecules designed to block the CYPs responsible for 1,25-D3 and ATRA metabolism (i.e., RAMBAs) offer advantages in vitamin therapy to fight several forms of cancer. The potential role of xenobiotic metabolizers CYP1A1 and CYP1B1 in the activation of carcinogens and inactivation of chemotherapeutics suggests therapeutic benefits in inhibiting these enzymes. Furthermore, CYP expression in tumor cells is being exploited with prodrugs such as phortress, aminoflavone, DMU-135, and AQ4N that are activated by these enzymes within the tumor. Of these, Phortress, aminoflavone, and AQ4N have already reached clinical trials.
Of the drugs discussed, only aromatase inhibitors have achieved clinical success. It remains to be seen whether or not the pre-clinical excitement surrounding other CYP directed therapeutics will resonate in the clinic. Still, CYP directed drugs offer a desperately needed new approach in cancer chemotherapy.
Acknowledgments
Research in Dr. Njar’s laboratory is supported by grants from US National Institutes of Health (NIH) and the National Cancer Institute (NCI), grant number R21 CA117991-01/02 and also from US Department of Defense (DOD), grant number WX1XWH-04–1–0101. Robert D. Bruno is supported by a training grant from the National Institute of Environmental Health Sciences (2T32ES007263–16A1). We thank all these agencies for their generous support.
Biographies
Vincent C. O. Njar completed his B. Sc. (Hons) in chemistry at University of Ibadan (Nigeria) in 1976 and went on to obtain a Ph.D. in organic chemistry in 1980 from University College London (UK) under the supervision of Derek V. Banthorpe. Following two years of postdoctoral research with the late Eliahu Caspi at Worcester Foundation for Experimental Biology, Shrewsbury, Mass. (USA), he joined the Department of Chemistry at the University of Ibadan (Nigeria) as Lecturer II. He was promoted through the ranks and became Professor of Organic Chemistry in 1996. He is currently Associate Professor of Pharmacology & Experimental Therapeutics at University of Maryland School of Medicine, Baltimore, MD USA. His research focus is on medicinal chemistry, pharmacology and development of inhibitors of androgen synthesis (CYP17 inhibitors), anti-androgens, androgen receptor down-regulating agents (ARDAs) and retinoic acid metabolism blocking agents (RAMBAs) as potential anti-cancer agents. Research on the combination of retinoids and/or RAMBAs with histone deacetylase inhibitors (HDACIs) and DNA methylation inhibitors (DMIs) is also being pursued. Our Technology on “CYP17 inhibitors/antiandrogens for prostate cancer” has recently been licensed by our University to Tokai Pharmaceuticals Inc., Boston, MA, USA. His research is interdisciplinary and has strong therapeutics translational potentials. Overall, his research is at the interface of medicinal chemistry and pharmacology/oncology aimed at discovery and development of new drugs for treatments of breast and prostate cancers.

Robert D. Bruno received a B.S. degree in Biology from James Madison University (Virginia, U.S.A.) in 2004. He is currently a Ph.D. student in the Molecular Medicine graduate program at the University of Maryland, Baltimore where he works with Dr. Vincent Njar. His research relates to the development of new therapeutic strategies for advanced prostate cancer using novel CYP17 (lyase) inhibitors/anti-androgens in combination with androgen receptor down-regulating agents.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Longcope C. Steroids. 1987;50:253. doi: 10.1016/0039-128x(83)90076-4. [DOI] [PubMed] [Google Scholar]
- 2.Puche C, Jose M, Cabero A, Meseguer A. Eur J Endocrinol. 2002;146:223. doi: 10.1530/eje.0.1460223. [DOI] [PubMed] [Google Scholar]
- 3.Haussler MR, Whitfield GK, Haussler CA, Hsieh JC, Thompson PD, Selznick SH, Dominguez CE, Jurutka PW. Journal of Bone and Mineral Research. 1998;13:325. doi: 10.1359/jbmr.1998.13.3.325. [DOI] [PubMed] [Google Scholar]
- 4.Kim SY, Yoo SJ, Kwon HJ, Kim SH, Byun Y, Lee KS. Metabolism. 2002;51:477. doi: 10.1053/meta.2002.31335. [DOI] [PubMed] [Google Scholar]
- 5.Osanai M, Petkovich M. Mol Pharmacol. 2005;67:1808. doi: 10.1124/mol.104.005769. [DOI] [PubMed] [Google Scholar]
- 6.Downie D, McFadyen MC, Rooney PH, Cruickshank ME, Parkin DE, Miller ID, Telfer C, Melvin WT, Murray GI. Clin Cancer Res. 2005;11:7369. doi: 10.1158/1078-0432.CCR-05-0466. [DOI] [PubMed] [Google Scholar]
- 7.Ozpolat B, Mehta K, Tari AM, Lopez-Berestein G. Am J Hematol. 2002;70:39. doi: 10.1002/ajh.10099. [DOI] [PubMed] [Google Scholar]
- 8.Sonneveld E, van den Brink CE, van der Leede BM, Schulkes RK, Petkovich M, van der Burg B, van der Saag PT. Cell Growth Differ. 1998;9:629. [PubMed] [Google Scholar]
- 9.Ray WJ, Bain G, Yao M, Gottlieb DI. J Biol Chem. 1997;272:18702. doi: 10.1074/jbc.272.30.18702. [DOI] [PubMed] [Google Scholar]
- 10.Njar VC, Gediya L, Purushottamachar P, Chopra P, Vasaitis TS, Khandelwal A, Mehta J, Huynh C, Belosay A, Patel J. Bioorg Med Chem. 2006;14:4323. doi: 10.1016/j.bmc.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 11.Njar VC. Mini Rev Med Chem. 2002;2:261. doi: 10.2174/1389557023406223. [DOI] [PubMed] [Google Scholar]
- 12.Mace K, Bowman ED, Vautravers P, Shields PG, Harris CC, Pfeifer AM. Eur J Cancer. 1998;34:914. doi: 10.1016/s0959-8049(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 13.Murray GI, McFadyen MC, Mitchell RT, Cheung YL, Kerr AC, Melvin WT. Br J Cancer. 1999;79:1836. doi: 10.1038/sj.bjc.6690292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashizume T, Imaoka S, Mise M, Terauchi Y, Fujii T, Miyazaki H, Kamataki T, Funae Y. J Pharmacol Exp Ther. 2002;300:298. doi: 10.1124/jpet.300.1.298. [DOI] [PubMed] [Google Scholar]
- 15.Murray GI, Taylor MC, McFadyen MC, McKay JA, Greenlee WF, Burke MD, Melvin WT. Cancer Res. 1997;57:3026. [PubMed] [Google Scholar]
- 16.Murray GI. J Pathol. 2000;192:419. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH750>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 17.Gibson P, Gill JH, Khan PA, Seargent JM, Martin SW, Batman PA, Griffith J, Bradley C, Double JA, Bibby MC, Loadman PM. Mol Cancer Ther. 2003;2:527. [PubMed] [Google Scholar]
- 18.Tokizane T, Shiina H, Igawa M, Enokida H, Urakami S, Kawakami T, Ogishima T, Okino ST, Li LC, Tanaka Y, Nonomura N, Okuyama A, Dahiya R. Clin Cancer Res. 2005;11:5793. doi: 10.1158/1078-0432.CCR-04-2545. [DOI] [PubMed] [Google Scholar]
- 19.Murray GI, Weaver RJ, Paterson PJ, Ewen SW, Melvin WT, Burke MD. J Pathol. 1993;169:347. doi: 10.1002/path.1711690312. [DOI] [PubMed] [Google Scholar]
- 20.Gut I, Danielova V, Holubova J, Soucek P, Kluckova H. Arch Toxicol. 2000;74:437. doi: 10.1007/s002040000141. [DOI] [PubMed] [Google Scholar]
- 21.Huang Z, Roy P, Waxman DJ. Biochem Pharmacol. 2000;59:961. doi: 10.1016/s0006-2952(99)00410-4. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez FJ, Gelboin HV. Drug Metab Rev. 1994;26:165. doi: 10.3109/03602539409029789. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez FJ. Toxicol Lett. 2001;120:199. doi: 10.1016/s0378-4274(01)00296-x. [DOI] [PubMed] [Google Scholar]
- 24.Karlgren M, Gomez A, Stark K, Svard J, Rodriguez-Antona C, Oliw E, Bernal ML, Ramon y Cajal S, Johansson I, Ingelman-Sundberg M. Biochem Biophys Res Commun. 2006;341:451. doi: 10.1016/j.bbrc.2005.12.200. [DOI] [PubMed] [Google Scholar]
- 25.Aung PP, Oue N, Mitani Y, Nakayama H, Yoshida K, Noguchi T, Bosserhoff AK, Yasui W. Oncogene. 2006;25:2546. doi: 10.1038/sj.onc.1209279. [DOI] [PubMed] [Google Scholar]
- 26.McFadyen MCE, Melvin WT, Murray GI. Mol Cancer Ther. 2004;3:363. [PubMed] [Google Scholar]
- 27.Jordan VC. Annu Rev Pharmacol Toxicol. 1995;35:195. doi: 10.1146/annurev.pa.35.040195.001211. [DOI] [PubMed] [Google Scholar]
- 28.Fornander T, Hellstrom AC, Moberger B. J Natl Cancer Inst. 1993;85:1850. doi: 10.1093/jnci/85.22.1850. [DOI] [PubMed] [Google Scholar]
- 29.Brodie AM, Schwarzel WC, Shaikh AA, Brodie HJ. Endocrinology. 1977;100:1684. doi: 10.1210/endo-100-6-1684. [DOI] [PubMed] [Google Scholar]
- 30.Brodie AM, Njar VC. Steroids. 2000;65:171. doi: 10.1016/s0039-128x(99)00104-x. [DOI] [PubMed] [Google Scholar]
- 31.Huggins CCVH. Cancer Res. 1941;1:293. [Google Scholar]
- 32.Huggins C, Jr, RE S, Hodges CV. Arch Surgery. 1941;43:209. [Google Scholar]
- 33.Edwards J, Bartlett JM. BJU Int. 2005;95:1320. doi: 10.1111/j.1464-410X.2005.05526.x. [DOI] [PubMed] [Google Scholar]
- 34.Heinlein CA, Chang C. Endocr Rev. 2002;23:175. doi: 10.1210/edrv.23.2.0460. [DOI] [PubMed] [Google Scholar]
- 35.Chen CD, Welsbie DS, Tran C, Baek SH, Chen R, Vessella R, Rosenfeld MG, Sawyers CL. Nat Med. 2004;10:33. doi: 10.1038/nm972. [DOI] [PubMed] [Google Scholar]
- 36.Hellerstedt BA, Pienta KJ. CA Cancer J Clin. 2002;52:154. doi: 10.3322/canjclin.52.3.154. [DOI] [PubMed] [Google Scholar]
- 37.Mohler JL, Gregory CW, Ford OH, 3rd, Kim D, Weaver CM, Petrusz P, Wilson EM, French FS. Clin Cancer Res. 2004;10:440. doi: 10.1158/1078-0432.ccr-1146-03. [DOI] [PubMed] [Google Scholar]
- 38.Hall PF. J Steroid Biochem Mol Biol. 1991;40:527. doi: 10.1016/0960-0760(91)90272-7. [DOI] [PubMed] [Google Scholar]
- 39.Trachtenberg J, Halpern N, Pont A. J Urol. 1983;130:152. doi: 10.1016/s0022-5347(17)51007-1. [DOI] [PubMed] [Google Scholar]
- 40.Small EJ, Baron AD, Fippin L, Apodaca D. J Urol. 1997;157:1204. [PubMed] [Google Scholar]
- 41.Harris KA, Weinberg V, Bok RA, Kakefuda M, Small EJ. J Urol. 2002;168:542. [PubMed] [Google Scholar]
- 42.Nakabayashi M, Xie W, Regan MM, Jackman DM, Kantoff PW, Oh WK. Cancer. 2006;107:975. doi: 10.1002/cncr.22085. [DOI] [PubMed] [Google Scholar]
- 43.Eklund J, Kozloff M, Vlamakis J, Starr A, Mariott M, Gallot L, Jovanovic B, Schilder L, Robin E, Pins M, Bergan RC. Cancer. 2006;106:2459. doi: 10.1002/cncr.21880. [DOI] [PubMed] [Google Scholar]
- 44.Attard G, Reid AHM, Barrett M, Karavasilis V, Molife R, Thompson E, Parker C, Dearnaley D, Lee G, Bono JSD. LB-180. American Association for Cancer Research Annual Meeting 2007; Los Angeles, CA. [Google Scholar]
- 45.Handratta VD, Vasaitis TS, Njar VC, Gediya LK, Kataria R, Chopra P, Newman D, Jr, Farquhar R, Guo Z, Qiu Y, Brodie AM. J Med Chem. 2005;48:2972. doi: 10.1021/jm040202w. [DOI] [PubMed] [Google Scholar]
- 46.Attard G, Belldegrun AS, de Bono JS. BJU Int. 2005;96:1241. doi: 10.1111/j.1464-410X.2005.05821.x. [DOI] [PubMed] [Google Scholar]
- 47.Njar VC, Brodie AM. Curr Pharm Des. 1999;5:163. [PubMed] [Google Scholar]
- 48.Hakki T, Bernhardt R. Pharmacol Ther. 2006;111:27. doi: 10.1016/j.pharmthera.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 49.Leroux F. Curr Med Chem. 2005;12:1623. doi: 10.2174/0929867054367185. [DOI] [PubMed] [Google Scholar]
- 50.Gonzalez-Sancho JM, Larriba MJ, Ordonez-Moran P, Palmer HG, Munoz A. Anticancer Res. 2006;26:2669. [PubMed] [Google Scholar]
- 51.Beer TM, Myrthue A. Anticancer Res. 2006;26:2647. [PubMed] [Google Scholar]
- 52.Moreno J, Krishnan AV, Feldman D. The Journal of Steroid Biochemistry and Molecular Biology. 2005;97:31. doi: 10.1016/j.jsbmb.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 53.Studzinski GP, McLane JA, Uskokovic MR. Critical Reviews in Eukaryotic Gene Expression. 1993;3:279. [PubMed] [Google Scholar]
- 54.Zhou W, Suk R, Liu G, Park S, Neuberg DS, Wain JC, Lynch TJ, Giovannucci E, Christiani DC. Cancer Epidemiol Biomarkers Prev. 2005;14:2303. doi: 10.1158/1055-9965.EPI-05-0335. [DOI] [PubMed] [Google Scholar]
- 55.Grant WB. Prog Biophys Mol Biol. 2006;92:65. doi: 10.1016/j.pbiomolbio.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Grant WB. Cancer. 2002;94:1867. doi: 10.1002/cncr.10427. [DOI] [PubMed] [Google Scholar]
- 57.Grant WB, Garland CF. American Family Physician. 2003;67:465. [PubMed] [Google Scholar]
- 58.Ohyama Y, Okuda K. J Biol Chem. 1991;266:8690. [PubMed] [Google Scholar]
- 59.Ohyama Y, Noshiro M, Okuda K. FEBS Letters. 1991;278:195. doi: 10.1016/0014-5793(91)80115-j. [DOI] [PubMed] [Google Scholar]
- 60.Diesing D, Cordes T, Fischer D, Diedrich K, Friedrich M. Anticancer Res. 2006;26:2755. [PubMed] [Google Scholar]
- 61.Cross HS, Kallay E, Farhan H, Weiland T, Manhardt T. Recent Results Cancer Res. 2003;164:413. doi: 10.1007/978-3-642-55580-0_30. [DOI] [PubMed] [Google Scholar]
- 62.Bareis P, Bises G, Bischof MG, Cross HS, Peterlik M. Biochemical and Biophysical Research Communications. 2001;285:1012. doi: 10.1006/bbrc.2001.5289. [DOI] [PubMed] [Google Scholar]
- 63.Parise RA, Egorin MJ, Kanterewicz B, Taimi M, Petkovich M, Lew AM, Chuang SS, Nichols M, El-Hefnawy T, Hershberger PA. Int J Cancer. 2006;119:1819. doi: 10.1002/ijc.22058. [DOI] [PubMed] [Google Scholar]
- 64.Albertson DG, Ylstra B, Segraves R, Collins C, Dairkee SH, Kowbel D, Kuo WL, Gray JW, Pinkel D. Nature Genetics. 2000;25:144. doi: 10.1038/75985. [DOI] [PubMed] [Google Scholar]
- 65.Sarkar FH, Adsule S, Padhye S, Kulkarni S, Li Y. Mini Rev Med Chem. 2006;6:401. doi: 10.2174/138955706776361439. [DOI] [PubMed] [Google Scholar]
- 66.Farhan H, Wahala K, Cross HS. Journal of Steroid Biochemistry and Molecular Biology. 2003;84:423. doi: 10.1016/s0960-0760(03)00063-3. [DOI] [PubMed] [Google Scholar]
- 67.Townsend K, Evans KN, Campbell MJ, Colston KW, Adams JS, Hewison M. J Steroid Biochem Mol Biol. 2005;97:103. doi: 10.1016/j.jsbmb.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 68.Diesel B, Fischer U, Meese E. Recent Results Cancer Res. 2003;164:151. doi: 10.1007/978-3-642-55580-0_11. [DOI] [PubMed] [Google Scholar]
- 69.Radermacher J, Diesel B, Seifert M, Tilgen W, Reichrath J, Fischer U, Meese E. Anticancer Res. 2006;26:2683. [PubMed] [Google Scholar]
- 70.Sarkar FH, Li Y. Cancer Res. 2006;66:3347. doi: 10.1158/0008-5472.CAN-05-4526. [DOI] [PubMed] [Google Scholar]
- 71.Sundaram S, Beckman MJ, Bajwa A, Wei J, Smith KM, Posner GH, Gewirtz DA. Mol Cancer Ther. 2006;5:2806. doi: 10.1158/1535-7163.MCT-06-0092. [DOI] [PubMed] [Google Scholar]
- 72.Posner GH, Lee JK, Wang Q, Peleg S, Burke M, Brem H, Dolan P, Kensler TW. J Med Chem. 1998;41:3008. doi: 10.1021/jm980031t. [DOI] [PubMed] [Google Scholar]
- 73.Alagbala AA, Johnson CS, Trump DL, Posner GH, Foster BA. Oncology. 2006;70:483. doi: 10.1159/000098813. [DOI] [PubMed] [Google Scholar]
- 74.Reddy C, Patti R, Guttapalli A, Maris J, Yanamandra N, Rachamallu A, Sutton L, Phillips P, Posner GH. Journal of Cellular Biochemistry. 2006;97:198. doi: 10.1002/jcb.20629. [DOI] [PubMed] [Google Scholar]
- 75.Peehl DM, Seto E, Hsu JY, Feldman D. J Urol. 2002;168:1583. doi: 10.1097/01.ju.0000030158.18335.84. [DOI] [PubMed] [Google Scholar]
- 76.Yee SW, Campbell MJ, Simons C. J Steroid Biochem Mol Biol. 2006;98:228. doi: 10.1016/j.jsbmb.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 77.Trump DL, Muindi J, Fakih M, Yu WD, Johnson CS. Anticancer Res. 2006;26:2551. [PubMed] [Google Scholar]
- 78.Ly LH, Zhao XY, Holloway L, Feldman D. Endocrinology. 1999;140:2071. doi: 10.1210/endo.140.5.6698. [DOI] [PubMed] [Google Scholar]
- 79.Schuster I, Egger H, Astecker N, Herzig G, Schussler M, Vorisek G. Steroids. 2001;66:451. doi: 10.1016/s0039-128x(00)00166-5. [DOI] [PubMed] [Google Scholar]
- 80.Schuster I, Egger H, Bikle D, Herzig G, Reddy GS, Stuetz A, Stuetz P, Vorisek G. Steroids. 2001;66:409. doi: 10.1016/s0039-128x(00)00159-8. [DOI] [PubMed] [Google Scholar]
- 81.Kahraman M, Sinishtaj S, Dolan PM, Kensler TW, Peleg S, Saha U, Chuang SS, Bernstein G, Korczak B, Posner GH. J Med Chem. 2004;47:6854. doi: 10.1021/jm040129+. [DOI] [PubMed] [Google Scholar]
- 82.Schuster I, Egger H, Herzig G, Reddy GS, Schmid JA, Schussler M, Vorisek G. Anticancer Res. 2006;26:2653. [PubMed] [Google Scholar]
- 83.Schuster I, Egger H, Reddy GS, Vorisek G. Recent Results Cancer Res. 2003;164:169. doi: 10.1007/978-3-642-55580-0_13. [DOI] [PubMed] [Google Scholar]
- 84.Posner GH, Crawford KR, Yang HW, Kahraman M, Jeon HB, Li H, Lee JK, Suh BC, Hatcher MA, Labonte T, Usera A, Dolan PM, Kensler TW, Peleg S, Jones G, Zhang A, Korczak B, Saha U, Chuang SS. J Steroid Biochem Mol Biol. 2004;89–90:5. doi: 10.1016/j.jsbmb.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 85.Chambon P. Faseb J. 1996;10:940. [PubMed] [Google Scholar]
- 86.Miller WH., Jr Cancer. 1998;83:1471. doi: 10.1002/(sici)1097-0142(19981015)83:8<1471::aid-cncr1>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 87.Altucci L, Gronemeyer H. Nat Rev Cancer. 2001;1:181. doi: 10.1038/35106036. [DOI] [PubMed] [Google Scholar]
- 88.Fontana JA, Rishi AK. Leukemia. 2002;16:463. doi: 10.1038/sj.leu.2402414. [DOI] [PubMed] [Google Scholar]
- 89.Njar VC, Gediya L, Purushottamachar P, Chopra P, Belosay A, Patel JB. Med Chem. 2006;2:431. doi: 10.2174/157340606777724022. [DOI] [PubMed] [Google Scholar]
- 90.Warrell RP, Jr, Frankel SR, Miller WH, Jr, Scheinberg DA, Itri LM, Hittelman WN, Vyas R, Andreeff M, Tafuri A, Jakubowski A, et al. N Engl J Med. 1991;324:1385. doi: 10.1056/NEJM199105163242002. [DOI] [PubMed] [Google Scholar]
- 91.Trump DL. Leukemia. 1994;8(Suppl 3):S50. [PubMed] [Google Scholar]
- 92.Trump DL, Smith DC, Stiff D, Adedoyin A, Day R, Bahnson RR, Hofacker J, Branch RA. Cancer Chemother Pharmacol. 1997;39:349. doi: 10.1007/s002800050582. [DOI] [PubMed] [Google Scholar]
- 93.Freemantle SJ, Spinella MJ, Dmitrovsky E. Oncogene. 2003;22:7305. doi: 10.1038/sj.onc.1206936. [DOI] [PubMed] [Google Scholar]
- 94.Muindi J, Frankel SR, Miller WH, Jr, Jakubowski A, Scheinberg DA, Young CW, Dmitrovsky E, Warrell RP., Jr Blood. 1992;79:299. [PubMed] [Google Scholar]
- 95.Muindi JR, Frankel SR, Huselton C, DeGrazia F, Garland WA, Young CW, Warrell RP., Jr Cancer Res. 1992;52:2138. [PubMed] [Google Scholar]
- 96.Leo MA, Lasker JM, Raucy JL, Kim CI, Black M, Lieber CS. Arch Biochem Biophys. 1989;269:305. doi: 10.1016/0003-9861(89)90112-4. [DOI] [PubMed] [Google Scholar]
- 97.Nadin L, Murray M. Biochem Pharmacol. 1999;58:1201. doi: 10.1016/s0006-2952(99)00192-6. [DOI] [PubMed] [Google Scholar]
- 98.McSorley LC, Daly AK. Biochem Pharmacol. 2000;60:517. doi: 10.1016/s0006-2952(00)00356-7. [DOI] [PubMed] [Google Scholar]
- 99.Marill J, Cresteil T, Lanotte M, Chabot GG. Mol Pharmacol. 2000;58:1341. doi: 10.1124/mol.58.6.1341. [DOI] [PubMed] [Google Scholar]
- 100.Van heusden J, Wouters W, Ramaekers FC, Krekels MD, Dillen L, Borgers M, Smets G. Br J Cancer. 1998;77:1229. doi: 10.1038/bjc.1998.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Klaassen I, Brakenhoff RH, Smeets SJ, Snow GB, Braakhuis BJ. Br J Cancer. 2001;85:630. doi: 10.1054/bjoc.2001.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ozpolat B, Mehta K, Lopez-Berestein G. Leuk Lymphoma. 2005;46:1497. doi: 10.1080/10428190500174737. [DOI] [PubMed] [Google Scholar]
- 103.Van Wauwe J, Van Nyen G, Coene MC, Stoppie P, Cools W, Goossens J, Borghgraef P, Janssen PA. J Pharmacol Exp Ther. 1992;261:773. [PubMed] [Google Scholar]
- 104.Van Wauwe JP, Coene MC, Goossens J, Cools W, Monbaliu J. J Pharmacol Exp Ther. 1990;252:365. [PubMed] [Google Scholar]
- 105.Bruynseels J, De Coster R, Van Rooy P, Wouters W, Coene MC, Snoeck E, Raeymaekers A, Freyne E, Sanz G, Vanden Bussche G, et al. Prostate. 1990;16:345. doi: 10.1002/pros.2990160409. [DOI] [PubMed] [Google Scholar]
- 106.Van Ginckel R, De Coster R, Wouters W, Vanherck W, van der Veer R, Goeminne N, Jagers E, Van Cauteren H, Wouters L, Distelmans W, et al. Prostate. 1990;16:313. doi: 10.1002/pros.2990160406. [DOI] [PubMed] [Google Scholar]
- 107.De Coster R, Wouters W, Van Ginckel R, End D, Krekels M, Coene MC, Bowden C. J Steroid Biochem Mol Biol. 1992;43:197. doi: 10.1016/0960-0760(92)90208-z. [DOI] [PubMed] [Google Scholar]
- 108.Smets G, Van Ginckel R, Daneels G, Moeremans M, Van Wauwe J, Coene MC, Ramaekers FC, Schalken JA, Borgers M, De Coster R. Prostate. 1995;27:129. doi: 10.1002/pros.2990270303. [DOI] [PubMed] [Google Scholar]
- 109.Debruyne FJ, Murray R, Fradet Y, Johansson JE, Tyrrell C, Boccardo F, Denis L, Marberger JM, Brune D, Rassweiler J, Vangeneugden T, Bruynseels J, Janssens M, De Porre P. Urology. 1998;52:72. doi: 10.1016/s0090-4295(98)00129-0. [DOI] [PubMed] [Google Scholar]
- 110.Patel JB, Huynh CK, Handratta VD, Gediya LK, Brodie AM, Goloubeva OG, Clement OO, Nanne IP, Soprano DR, Njar VC. J Med Chem. 2004;47:6716. doi: 10.1021/jm0401457. [DOI] [PubMed] [Google Scholar]
- 111.Njar VC, Nnane IP, Brodie AM. Bioorg Med Chem Lett. 2000;10:1905. doi: 10.1016/s0960-894x(00)00391-7. [DOI] [PubMed] [Google Scholar]
- 112.Belosay A, Brodie AM, Njar VC. Cancer Res. 2006;66:11485. doi: 10.1158/0008-5472.CAN-06-2168. [DOI] [PubMed] [Google Scholar]
- 113.Ding X, Kaminsky LS. Annu Rev Pharmacol Toxicol. 2003;43:149. doi: 10.1146/annurev.pharmtox.43.100901.140251. [DOI] [PubMed] [Google Scholar]
- 114.Shimada T, Hayes CL, Yamazaki H, Amin S, Hecht SS, Guengerich FP, Sutter TR. Cancer Res. 1996;56:2979. [PubMed] [Google Scholar]
- 115.Peter Guengerich F, Chun YJ, Kim D, Gillam EM, Shimada T. Mutat Res. 2003;523–524:173. doi: 10.1016/s0027-5107(02)00333-0. [DOI] [PubMed] [Google Scholar]
- 116.Sissung TM, Price DK, Sparreboom A, Figg WD. Mol Cancer Res. 2006;4:135. doi: 10.1158/1541-7786.MCR-05-0101. [DOI] [PubMed] [Google Scholar]
- 117.Wenzlaff AS, Cote ML, Bock CH, Land SJ, Santer SK, Schwartz DR, Schwartz AG. Carcinogenesis. 2005;26:2207. doi: 10.1093/carcin/bgi191. [DOI] [PubMed] [Google Scholar]
- 118.Sasaki M, Tanaka Y, Okino ST, Nomoto M, Yonezawa S, Nakagawa M, Fujimoto S, Sakuragi N, Dahiya R. Clin Cancer Res. 2004;10:2015. doi: 10.1158/1078-0432.ccr-03-0166. [DOI] [PubMed] [Google Scholar]
- 119.McGrath M, Hankinson SE, Arbeitman L, Colditz GA, Hunter DJ, De Vivo I. Carcinogenesis. 2004;25:559. doi: 10.1093/carcin/bgh039. [DOI] [PubMed] [Google Scholar]
- 120.McFadyen MC, McLeod HL, Jackson FC, Melvin WT, Doehmer J, Murray GI. Biochem Pharmacol. 2001;62:207. doi: 10.1016/s0006-2952(01)00643-8. [DOI] [PubMed] [Google Scholar]
- 121.Patterson LH, Murray GI. Curr Pharm Des. 2002;8:1335. doi: 10.2174/1381612023394502. [DOI] [PubMed] [Google Scholar]
- 122.Stiborova M, Bieler CA, Wiessler M, Frei E. Biochem Pharmacol. 2001;62:1675. doi: 10.1016/s0006-2952(01)00806-1. [DOI] [PubMed] [Google Scholar]
- 123.Chun YJ, Kim S. Med Res Rev. 2003;23:657. doi: 10.1002/med.10050. [DOI] [PubMed] [Google Scholar]
- 124.Van Aswegen CH, Purdy RH, Wittliff JL. J Steroid Biochem. 1989;32:485. doi: 10.1016/0022-4731(89)90380-4. [DOI] [PubMed] [Google Scholar]
- 125.Cavalieri EL, Stack DE, Devanesan PD, Todorovic R, Dwivedy I, Higginbotham S, Johansson SL, Patil KD, Gross ML, Gooden JK, Ramanathan R, Cerny RL, Rogan EG. Proc Natl Acad Sci U S A. 1997;94:10937. doi: 10.1073/pnas.94.20.10937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gonzalez FJ. Toxicology. 2002;181–182:237. doi: 10.1016/s0300-483x(02)00288-3. [DOI] [PubMed] [Google Scholar]
- 127.Denison MS, Nagy SR. Annu Rev Pharmacol Toxicol. 2003;43:309. doi: 10.1146/annurev.pharmtox.43.100901.135828. [DOI] [PubMed] [Google Scholar]
- 128.Song Z, Pollenz RS. Mol Pharmacol. 2002;62:806. doi: 10.1124/mol.62.4.806. [DOI] [PubMed] [Google Scholar]
- 129.Kim JH, Sherman ME, Curriero FC, Guengerich FP, Strickland PT, Sutter TR. Toxicol Appl Pharmacol. 2004;199:210. doi: 10.1016/j.taap.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 130.Dorrenhaus A, Muller T, Roos PH. Arch Toxicol. 2006 doi: 10.1007/s00204-006-0134-9. [DOI] [PubMed] [Google Scholar]
- 131.Puppala D, Gairola CG, Swanson HI. Carcinogenesis. 2006 doi: 10.1093/carcin/bgl169. [DOI] [PubMed] [Google Scholar]
- 132.Wen X, Walle UK, Walle T. Carcinogenesis. 2005;26:803. doi: 10.1093/carcin/bgi015. [DOI] [PubMed] [Google Scholar]
- 133.Chen ZH, Hurh YJ, Na HK, Kim JH, Chun YJ, Kim DH, Kang KS, Cho MH, Surh YJ. Carcinogenesis. 2004;25:2005. doi: 10.1093/carcin/bgh183. [DOI] [PubMed] [Google Scholar]
- 134.Shimada T, Yamazaki H, Foroozesh M, Hopkins NE, Alworth WL, Guengerich FP. Chem Res Toxicol. 1998;11:1048. doi: 10.1021/tx980090+. [DOI] [PubMed] [Google Scholar]
- 135.Pang S, Cao JQ, Katz BH, Hayes CL, Sutter TR, Spink DC. Biochem Pharmacol. 1999;58:29. doi: 10.1016/s0006-2952(99)00070-2. [DOI] [PubMed] [Google Scholar]
- 136.Doostdar H, Burke MD, Mayer RT. Toxicology. 2000;144:31. doi: 10.1016/s0300-483x(99)00215-2. [DOI] [PubMed] [Google Scholar]
- 137.Kim S, Ko H, Park JE, Jung S, Lee SK, Chun YJ. J Med Chem. 2002;45:160. doi: 10.1021/jm010298j. [DOI] [PubMed] [Google Scholar]
- 138.Potter GA, Patterson LH, Wanogho E, Perry PJ, Butler PC, Ijaz T, Ruparelia KC, Lamb JH, Farmer PB, Stanley LA, Burke MD. Br J Cancer. 2002;86:774. doi: 10.1038/sj.bjc.6600197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Niles RM, Cook CP, Meadows GG, Fu YM, McLaughlin JL, Rankin GO. J Nutr. 2006;136:2542. doi: 10.1093/jn/136.10.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bradshaw TD, Westwell AD. Curr Med Chem. 2004;11:1009. doi: 10.2174/0929867043455530. [DOI] [PubMed] [Google Scholar]
- 141.Kuffel MJ, Schroeder JC, Pobst LJ, Naylor S, Reid JM, Kaufmann SH, Ames MM. Mol Pharmacol. 2002;62:143. doi: 10.1124/mol.62.1.143. [DOI] [PubMed] [Google Scholar]
- 142.Meng LH, Shankavaram U, Chen C, Agama K, Fu HQ, Gonzalez FJ, Weinstein J, Pommier Y. Cancer Res. 2006;66:9656. doi: 10.1158/0008-5472.CAN-06-0796. [DOI] [PubMed] [Google Scholar]
- 143.Sale S, Tunstall RG, Ruparelia KC, Butler PC, Potter GA, Steward WP, Gescher AJ. Invest New Drugs. 2006;24:459. doi: 10.1007/s10637-006-5947-0. [DOI] [PubMed] [Google Scholar]
- 144.Karlgren M, Miura S-i, Ingelman-Sundberg M. Toxicology and Applied Pharmacology. 2005;207:57. doi: 10.1016/j.taap.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 145.Yoshioka H, Kasai N, Ikushiro S, Shinkyo R, Kamakura M, Ohta M, Inouye K, Sakaki T. Biochem Biophys Res Commun. 2006;345:169. doi: 10.1016/j.bbrc.2006.04.080. [DOI] [PubMed] [Google Scholar]
- 146.Boyle RG, Travers S. Anticancer Agents Med Chem. 2006;6:281. doi: 10.2174/187152006777698169. [DOI] [PubMed] [Google Scholar]
- 147.Patterson LH, McKeown SR. Br J Cancer. 2000;83:1589. doi: 10.1054/bjoc.2000.1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ali MM, Symons MC, Taiwo FA, Patterson LH. Chem Biol Interact. 1999;123:1. doi: 10.1016/s0009-2797(99)00097-6. [DOI] [PubMed] [Google Scholar]
- 149.McKeown SR, Hejmadi MV, McIntyre IA, McAleer JJ, Patterson LH. Br J Cancer. 1995;72:76. doi: 10.1038/bjc.1995.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.McKeown SR, Friery OP, McIntyre IA, Hejmadi MV, Patterson LH, Hirst DG. Br J Cancer Suppl. 1996;27:S39. [PMC free article] [PubMed] [Google Scholar]
- 151.Hejmadi MV, McKeown SR, Friery OP, McIntyre IA, Patterson LH, Hirst DG. Br J Cancer. 1996;73:499. doi: 10.1038/bjc.1996.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.United States: Food and Drug Administration. [Accessed: 03/23/07];2006 : NCT00394628. http://www.clinicaltrials.gov/ct/show/NCT00394628?order=1.


