Abstract
Objectives
To determine the content and extent, design, and relative importance of patient assessment courses in the professional pharmacy curriculum.
Methods
A 20-item questionnaire was developed to gather information pertaining to patient assessment. Pharmacy practice department chairs were mailed a letter with an Internet link to an online survey instrument.
Results
Ninety-six percent of the programs indicated that patient assessment skills were taught. Forty-five percent of respondents indicated their course was a standalone course. The most common topics covered in assessment courses were pulmonary examination, vital signs, and cardiovascular assessment.
Conclusion
There is significant variability in the topics covered, depth of content, types of instruction, and evaluation methods used in patient assessment courses in US colleges of pharmacy. This survey was an initial assessment of what is being done regarding education of student pharmacists on patient assessment.
Keywords: curriculum design, laboratory instruction, patient assessment, physical assessment
INTRODUCTION
Since patient assessment skills are part of the everyday practice of pharmacists, it is important that pharmacy students are properly trained with these skills. Pharmacists are using these skills daily as they continue the transition from pharmacotherapy advisors to managers of medication therapy. Thus, the purpose of our study was to determine what is currently being taught to students within the doctor of pharmacy curriculum. For the purpose of this study, the terms patient assessment and physical assessment are used interchangeably.
As defined by Jones et al, “physical assessment is the process through which pharmacists evaluate patient information (both subjective and objective) that was gathered from the patient and other sources and make decisions regarding: (1) the health status of the patient, (2) drug therapy needs and problems, (3) interventions that will resolve identified drug problems and prevent future problems; and (4) follow-up to ensure that patient outcomes are being met. The primary focus of patient assessment is to identify, resolve, and prevent drug therapy problems.”1 Pharmaceutical care is one of the educational outcomes from the Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes. Pharmacists will need the ability to provide patient-centered care through providing care plans and communication with patients and other health care providers.2 The Joint Commission of Pharmacy Practitioners states that pharmacists should strive to be responsible for the measurement and assurance of medication therapy outcomes.3 Responses to a 1981-1982 survey of American pharmacy programs regarding a definition of physical assessment included: “the skill necessary to assess changes in a patients' status, especially when drug therapy is involved,” “to evaluate a patient's basic disease process and subsequent response to drug therapy,” and “to judge whether the therapeutic intervention is effective, less than effective or toxic for a particular patient.”4
Since pharmacists are recognized under the Medication Modernization Act of 2003 as providers of medication therapy management, pharmacy programs need to continue to teach and reevaluate the role of the pharmacist in providing patient assessment to properly educate future pharmacists.5 Part of this reevaluation is recognizing and enhancing opportunities for the provision of patient assessment skills to their patients. The goal of Medication Therapy Management is to optimize therapeutic outcomes and the improvement of quality of life for patients. In order to achieve this, it will be necessary for pharmacists to perform patient assessment skills related to medication therapy to determine efficacy and tolerability, and interpret the findings of other providers.6,7 As the role of the pharmacist becomes increasingly patient-care oriented, pharmacists must be able to gather essential information in order to properly monitor drug therapies. Pharmacists in diverse clinical settings assess patients using a variety of patient assessment skills.3
The Accreditation Council for Pharmacy Education (ACPE) lists patient assessment laboratory as an essential subject for the development of pharmacists that should be included as part of a curriculum's science foundation.8 Some of the skills the patient assessment laboratory should teach include how to obtain a comprehensive patient history, basic assessment techniques, interpretation of common laboratory tests and diagnostic test values, and use of nonprescription point-of-care testing devices.8 As a result of a patient assessment course, students should be able to integrate essential elements of clinical care, including conducting the patient assessment, establishing patient relationships, and performing critical thinking.
Two national reviews of patient assessment instruction in US colleges and schools of pharmacy were identified. In a 1981-1982 investigation, Closson found that approximately half of US colleges offered instruction in patient assessment and concluded that this number might need to increase in order to meet the growing need for patient assessment skills in community pharmacy.4 A survey of patient assessment course offerings in US colleges of pharmacy9 demonstrated that pharmacists of the future will have to have the necessary skills required to assess therapeutic outcomes.9 To do this, pharmacists will need to have a more direct patient care role. Since this study was published, the ACPE has revised their standards and guidelines for pharmaceutical education.8
This study will (1) compile data on the content and extent of patient assessment within pharmacy curriculum, (2) review design of patient assessment courses, and (3) determine the relative importance that respondents place on patient assessment courses in their curriculum.
METHODS
A 20-item questionnaire was developed to gather information pertaining to patient assessment within a pharmacy curriculum. The survey instrument included items addressing the following: timing of patient assessment course, overall course design, topics covered, equipment used, instructional and assessment techniques used, education of instructors, collaboration with other healthcare professionals, and the use of integrated teaching techniques. These questions were adapted from items from the survey instruments by da Camara and Closson as well as from the authors' personal experience and informal discussions with other faculty members teaching similar courses at other institutions.4,9 The survey instrument consisted of multiple-choice and short-answer questions. Both the electronic and hard copy versions of the survey instrument were reviewed by faculty members at the Bernard J. Dunn School of Pharmacy who had previously been involved with the instruction of patient assessment. Based on the feedback from these internal reviewers, adjustments were made to both versions of the instrument to allow for optimal data collection. Pharmacy practice department chairs were selected as the recipients of the survey instrument based on the approach used by the previous study by da Camara.9 All pharmacy practice department chairs at US colleges and schools of pharmacy were sent both a printed copy of the survey instrument via US mail and an Internet link via e-mail to an electronic version of the survey instrument on SurveyMonkey.com (Survey Monkey Corporation, Portland, Oregon). Department chairs were identified through the American Association of Colleges 2005/2006 Roster of Faculty and Professional Staff10 or by review of respective college's web sites. Included with the survey instrument was an explanation of the survey and the objectives for performing the data collection. A reminder was sent electronically to non-respondents 2 weeks after the initial mailing. Since department chairs were provided with both electronic and paper versions of the study, the survey instruments were randomly assigned a number that was entered in the unique identifier field of the survey instrument to help identify duplicate responses from the same college or school. If multiple responses were received, only the most complete survey instrument was included in the data analysis. Survey recipients were given 1 month to complete the survey instrument. Several survey instruments were returned after the 1 month deadline had expired and these surveys were incorporated into the final tabulation of the results.
Data from electronic survey instruments were downloaded to a Microsoft Excel spreadsheet, and responses from paper survey instruments were entered manually into the database. Response means and percentage of respondents were calculated.
RESULTS
Seventy-four percent of the survey instruments were returned: 60% (43) via the online survey instrument and 40% (29) via postal mail. Ninety-six percent of the 72 responding programs indicated that patient assessment skills are taught within their pharmacy curriculum. Some of the department chairs passed the survey instrument on to a course or laboratory coordinator to complete. When asked why patient assessment skills were taught in the curriculum, the most common response was for the advancement of the profession of pharmacy (60 out of 67 respondents or 90%). Thirty-one (46%) respondents indicated that they taught patient assessment skills because it was a requirement of the program; 30 (44.7%), because it was an ACPE requirement; and 33 (49%), because it was an interest of the faculty member. Forty-five percent (30 of out 66 respondents) indicated that their course was a standalone course within their curriculum. Of the remaining 36 pharmacy programs, 15 indicated that patient assessment was part of their therapeutics course; 9, part of a skills laboratory; 6, part of a pharmaceutical care course; 2, part of pharmacology; 1, part of pathophysiology; and 3, part of other courses. Sixty-five percent of responding programs indicated that patient assessment skills were covered in their third-professional year, 49% indicated it was covered during the second-professional year, 19% in the first-professional year, and 16% in the fourth-professional year. Twenty percent of respondents indicated that patient assessment skills were covered in more than 1 year of the curriculum. The majority (91%) of respondents indicated that they felt the course was well timed in the curriculum. Those that felt that it was not well timed indicated that their patient assessment material was more spread throughout the curriculum (n = 3), during the second-professional year (n = 1) and the third-professional year (n = 3). A mean of 2.3 (range 1-4) credit hours were assigned to the patient assessment course.
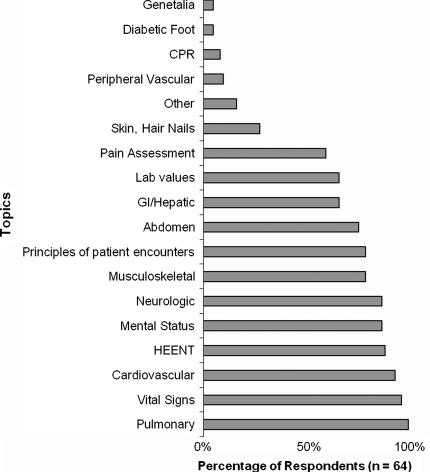
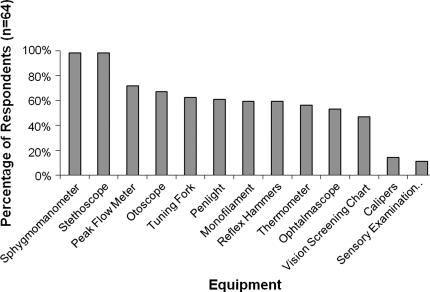
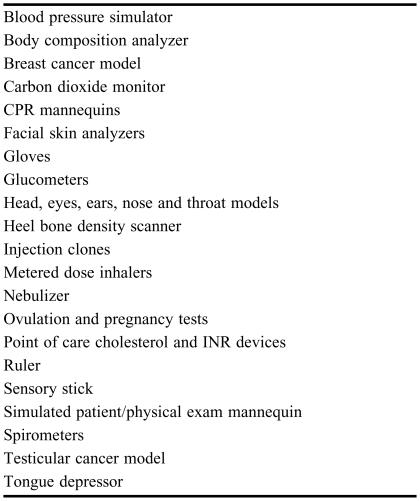
The most common topics that programs covered in the course were pulmonary examination, followed by vital signs and cardiovascular assessment. A review of the frequency with which various topics were covered can be found in Figure 1. Skin, hair, and nails; genitalia; diabetic foot examinations; cardiopulmonary resuscitation; and peripheral vascular assessment were not provided as responses on the survey instrument but were frequent write-in responses. Some of the other topics listed by respondents included nephrology, diabetes, immunizations, basic imaging techniques, health and wellness screenings, nutritional assessment, breast examinations, medication errors, billing, consult note writing, pregnancy, and infant assessment. Figure 2 illustrates the equipment that the responding programs indicated they were using in the instruction of patient assessment. Table 1 lists other equipment used by the students during their physical assessment course.
Figure 1.
Topics Covered in Patient Assessment Instruction.
Figure 2.
Equipment Used by Pharmacy Students during Patient Assessment Course.
Table 1.
Other Equipment Used For Physical Assessment Instruction
CPR = Cardiopulmonary Resuscitation; INR = International Normalized Ratio
Forty-three percent of respondents (22 out of 51) indicated that they used a textbook in their course; the most commonly used text was Bickely's Bates Guide to Physical Examination and History Taking with followed by Jones's Patient Assessment in Pharmacy Practice. Some other responses included instructor-prepared notes, Bate's Visual Guide to Physical Examination, and Tietze's Clinical Skills for Pharmacists: A Patient-Focused Approach. Eighty-six percent (n = 57) of responding programs indicated that they used a laboratory approach for instruction, 70% used lectures, 11% used self-study, and 8% used an accelerated course over 3-7 days. Nineteen of the programs indicated they only used laboratory instruction, 12 only used lecture, and 1 only used simulated patient settings. Some of the programs that indicated they used an abbreviated course further indicated that instruction was provided over a period of time (2.5 days to 1 week). One program indicated that they provided instruction on patient assessment through advanced pharmacy practice experiences. Seventy-six percent (n = 67) of the responding programs indicated that their course is taught in a pharmacy program laboratory setting, 27% in a simulated clinical setting, and 63% in a classroom. Other programs indicated that they used nursing and medical school laboratories and clinical practice sites.
Eighty-two percent (65) of responding programs taught patient assessment independent of other health science and medical programs. Eighteen percent of the respondents indicated their course was affiliated with the following: physician assistant program, 4; nursing and nurse practitioner program, 5; osteopathic program, 1; dentistry program, 1; and physical therapy program, 1. Fifty-four of 66 responding programs (82%) indicated that the course was taught by pharmacy practice faculty members, 8 programs used nurses, 12 programs used non-faculty pharmacists, 8 programs used physician assistants, and 10 programs utilized physicians. Some programs also indicated that they used emergency medical technicians, pharmacy residents, and/or senior pharmacy students, and one program had an individual who was trained both as a pharmacist and a nurse. Seventy-seven percent (66) of the programs indicated that their course instructors received training through postgraduate experiences. Thirty-seven programs indicated that the instructors received on-the-job training and formal physical assessment coursework. Two programs indicated that their faculty members had attended certificate and training programs.
Eighty-five percent (66) of the programs indicated that they used hands-on or practical type examinations to assess students' proficiency and understanding of the material, while 72% used written examinations. Programs indicated that they used the following techniques exclusively or in conjunction with the other examination techniques: verbal examinations, proficiency examinations (pass/fail), laboratory write-ups, case study presentations, and progress notes.
DISCUSSION
The majority of US pharmacy programs incorporate patient assessment into other courses. This is in contrast to the results of the 1995 study by da Camara which found that 75% of programs offered the patient assessment course as a standalone course.9 While integration of patient assessment into other courses offers students the opportunity to combine the therapeutics and pathophysiologic changes associated with the covered disease states, it could limit students' hands on experience and in-depth instruction in patient assessment. Schön argues in his book Educating the Reflective Practitioner that professional schools need to allow students time to practice the skills that they are taught through a reflective coaching experience.11 Relying on experiential education could lead to high variability between PharmD programs in terms of instructional depth, topics covered, and instructional methods. If a course is integrated into another course, time may not be sufficient to perform and critique students' skills. Assessment skills should be repeated throughout a course, eg, the students are taught how to assess a patient's blood pressure and should perform this skill through the semester or year in order to achieve mastery.
We also found there is variability between responding pharmacy programs in the patient assessment topics covered. Da Camara reported the most common topics included in 1996 were the assessment of chest lungs, and heart. Similarly our study found that pulmonary examination, vital signs, and cardiovascular assessment as the most common topics offered currently.9 Pharmacy educators should determine the essential skills that pharmacists need in order to provide patient care in all settings. This could include pharmacists being able to monitor the efficacy of the medication therapy as well as provide wellness services. The American College of Physicians cites that there is a shortage of primary care practitioners; therefore, pharmacists may be called up to help provide more basic wellness services.12 Pharmacists need to become respected as health care providers who can provide the assessment necessary to monitor medication therapy, through demonstration of proficiency. Beyond mere exposure to various examination and diagnostic techniques, pharmacy students need to develop skills to provide proficient patient assessment services in order to achieve the goals set forth in the CAPE outcomes.
Seventy-two percent of programs indicated that written examinations were a part of their assessment of students' understanding of the skills taught, with 15% indicating that this is the only type of assessment conducted. Given the hands-on nature of these skills, assessment should occur by direct observation of these skills during practical or hands-on examinations. As part of this competency, student pharmacists should be expected to achieve a certain level of proficiency with patient assessment skills.
A majority of the course instructors for patient assessment skills obtained these skills through postgraduate education. In contrast, da Camara et al found that a majority of their respondents (14) received most of their training on physical assessment through on-the-job training. This apparent change may be due to the increasing role of postgraduate education in preparing individuals for faculty appointments.9 The use of postgraduate training for instruction on patient assessment skills speaks to the advanced clinical nature of postgraduate education. It also suggests a lack of sufficient training as part of professional degree programs. This could also lead to significant variability in the aptitude and proficiency of pharmacy instructors and thus the information that is provided to pharmacy students.
Sixty-five percent of the pharmacy programs that responded to our survey included patient assessment skills as part of the third-professional year curriculum; however, 35% included the training in other years. This was consistent with da Camara's findings that the majority of programs offered instruction in patient assessment skills during the fourth and fifth years of a 6-year doctor of pharmacy program.9 Longitudinal exposure and instruction on patient assessment skills can offer a better understanding and repeated practice through the curriculum. However, offering a patient assessment course too early in the curriculum can prevent students from connecting these skills with real patients and clinical experiences that they will be exposed to during advanced pharmacy practice experiences. However, relying on the clerkship experience alone for the majority of this instruction could be problematic due to a lack of formalized instruction and standardization across practice sites.
In 1984, Adamcik and Stimmel investigated the most commonly used physical assessments to monitor drug therapy.13 They evaluated members of the American College of Clinical Pharmacy (ACCP) and Southern California Adjunct Practice Faculty and found that one third of the ACCP members and 20% of the adjunct faculty regularly used physical assessment in the monitoring of patients.13 They also cited lack of training as the major barrier that prevented those surveyed from using patient assessment.13
By using a systematic approach, pharmacists are able to obtain the proper data, which ultimately results in improved patient care. Exposure to patient assessment in the pharmacy curriculum will better prepare pharmacy students for experiential learning, postgraduate training, and pharmacy practice.
Our study was able to provide an overview of patient assessment instruction in pharmacy programs in the United States due to the high response rate representing a majority of pharmacy programs. Potential limitations of our study include variability in who the responder to the survey was. While we tried to direct the survey to the pharmacy practice chair, the survey instrument was sometimes further directed to the coordinator of the course in order to answer some of the more detailed questions. This could have led to variability in the responses that we received. Also some programs did not complete the entire survey instrument, which limited the data that we were able to collect. The electronic survey instrument was not formatted to allow for multiple responses to the question regarding course design (ie, lecture, laboratory, self-study, abbreviated course, or other). This could have caused differences in responses between users of the Web-based survey instrument and the paper survey instrument, as well as a limited number of respondents who felt more than one response was appropriate.
This survey was an initial assessment of what is being done regarding education of pharmacy students in patient assessment. The next step will be an evaluation of the skills that pharmacists currently need to be proficient in practice for a variety of settings, which can then be used to set a national standard that all pharmacy programs should achieve.
CONCLUSION
As the role of the pharmacist continues to evolve, pharmacy education must also evolve to meet the needs of the changing field. Patient assessment is an area where a minimum standard for patient assessment that all graduating student pharmacists should meet is needed in order to prepare pharmacy students for practice. Currently, the amount of variability in the topics covered, the depth of content, and the types of instruction and evaluation prevent the pharmacy profession from being able to set this standard to advance the practice of pharmacy within the eyes of the public and other health care providers.
ACKNOWLEDGMENTS
The authors thank Scott Stolte, PharmD, and Renee Ahrens Thomas, PharmD, MBA, for assisting in manuscript preparation and completion. Funding for this project was received from Shenandoah University through an internal school of pharmacy research fund.
REFERENCES
- 1.Jones RA. Patient Assessment and the Pharmaceutical Care Process. In: Jones RM, Rospond RM, editors. Patient Assessment for Pharmacy Practice. Baltimore, Md: Lippincott Williams & Wilkins; 2003. pp. 2–8. [Google Scholar]
- 2. American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education (CAPE), Advisory Panel on Educational Outcomes. Educational outcomes. Revised version 1998. Available from http://www.aacp.org/Docs/MainNavigation/ForDeans/5763_CAPEoutcomes.pdf. Accessed July 20, 2006.
- 3. Joint Commission of Pharmacy Practitioners. JCPP Future Vision of Pharmacy Practice. November 10, 2004. Available at: http://www.aacp.org/Docs/MainNavigation/Resources/6725_JCPPFutureVisionofPharmacyPracticeFINAL.pdf. Accessed September 6, 2006.
- 4.Closson RG. Physical assessment instruction, 1981-1982: A survey of american colleges of pharmacy. Am J Pharm Educ. 1984;48:25. [Google Scholar]
- 5. United States Centers for Medicare and Medicaid Services. Medicare Prescription Drug Benefit Final Rule; 42 CFR Parts 400, 403, 411, 417, and 423 Medicare Program. January 28, 2005. Available at http://www.cms.hhs.gov/PhysicianSelfReferral/Downloads/CMS4068F.pdf. Accessed October 12, 2006.
- 6.American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication Therapy Management in Community Pharmacy Practice. Core elements of an MTM Service (Version 1.0) J Am Pharm Assoc. 2005;45:573–9. doi: 10.1331/1544345055001256. [DOI] [PubMed] [Google Scholar]
- 7. The Lewin Group. Medication Therapy Management Services: A Critical Review. May 15, 2005. Available at: http://www.aphanet.org/AM/Template.cfm?Section=Search§ion=MTM_Services&template=/CM/ContentDisplay.cfm&ContentFileID=1036. Accessed October 12, 2006.
- 8. Accreditation Council for Pharmaceutical Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. February 2006. Available at: http://www.acpeaccredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed September 6, 2006.
- 9.da Camara CC, D'Elia RP, Swanson LN. Survey of physical assessment course offerings in American Colleges of pharmacy. Am J Pharm Educ. 1996;60:343–7. [Google Scholar]
- 10. Roster of Faculty and Professional Staff, 2005/2006. Alexandria, Va: American Association of Colleges of Pharmacy; 2005.
- 11.Schön DA. Educating the Reflective Practicioner. San Francisco, Calif: Jossey-Bass; 1987. [Google Scholar]
- 12. The Impending Collapse of Primary Care Medicine and Its Implications for the State of the Nation's Health Care. Washington, DC: American College of Physicians. January 30, 2006. Available at: http://www.acponline.org/hpp/statehc06_1.pdf. Accessed December 14, 2006.
- 13.Adamcik BA, Stimmel GL. Use of physical assessment skills by clinical pharmacists in monitoring drug therapy response: attitudes and frequency. Am J Pharm Educ. 1989;53:127–33. [Google Scholar]