Abstract
Objectives:
The timing of definitive fixation for major fractures in patients with multiple injuries is controversial. To address this gap, we randomized patients with blunt multiple injuries to either initial definitive stabilization of the femur shaft with an intramedullary nail or an external fixateur with later conversion to an intermedullary nail and documented the postoperative clinical condition.
Methods:
Multiply injured patients with femoral shaft fractures were randomized to either initial (<24 hours) intramedullary femoral nailing or external fixation and later conversion to an intramedullary nail. Inclusion: New Injury Severity Score >16 points, or 3 fractures and Abbreviated Injury Scale score ≥2 points and another injury (Abbreviated Injury Scale score ≥2 points), and age 18 to 65 years. Exclusion: patients in unstable or critical condition. Patients were graded as stable or borderline (increased risk of systemic complications).
Outcomes:
Incidence of acute lung injuries.
Results:
Ten European Centers, 165 patients, mean age 32.7 ± 11.7 years. Group intramedullary nailing, n = 94; group external fixation, n = 71. Preoperatively, 121 patients were stable and 44 patients were in borderline condition. After adjusting for differences in initial injury severity between the 2 treatment groups, the odds of developing acute lung injury were 6.69 times greater in borderline patients who underwent intramedullary nailing in comparison with those who underwent external fixation, P < 0.05.
Conclusion:
Intramedullary stabilization of the femur fracture can affect the outcome in patients with multiple injuries. In stable patients, primary femoral nailing is associated with shorter ventilation time. In borderline patients, it is associated with a higher incidence of lung dysfunctions when compared with those who underwent external fixation and later conversion to intermedullary nail. Therefore, the preoperative condition should be when deciding on the type of initial fixation to perform in patients with multiple blunt injuries.
Patients with multiple injuries were randomized to initial external fixation or nailing of their femoral shaft fracture. Stable patients experienced shorter ventilation times: patients in uncertain (borderline) condition developed more acute lung injuries after intramedullary nailing. Therefore, the surgical management of the femur fracture should be adapted to the clinical condition.
It is accepted that primary definitive stabilization of major fractures in patients with blunt multiple injuries is advantageous in terms of reduced ventilation time, shorter hospital stay, and improved early mobilization of the patient.1
However, there is controversy in the orthopedic literature as to whether all patients benefit from this approach. A certain subset of patients, specifically those in severe shock or those who have additional severe head or chest injuries may be at increased risk for complications after primary definitive stabilization of major fractures.2–5 It is still unclear whether initial temporary stabilization of fractures by external fixation (damage control orthopedics [DCO]4), or definitive stabilization of all major fractures should be performed in all cases.6–12
To date, any recommendations and guidelines described above have been based only on level II to III evidence. Currently, there are several prospective randomized studies dealing with fracture management in general,10,13,14 but no level I studies have investigated whether temporary fracture fixation should be recommended for certain patient populations.15 This prospective, randomized, controlled analysis therefore tests the hypothesis that initial temporary fracture stabilization is more advantageous than initial definitive stabilization for femoral shaft fractures in patients with more severe injuries with regard to the development of systemic complications.
PATIENTS AND METHODS
Setting
This investigation was designed as a prospective, randomized intervention trial in 10 level I trauma centers. The study was carried out from January 1, 2000 to February28, 2006.
Subjects
The inclusion criteria consisted of multiple injuries with a New Injury Severity Score (NISS) exceeding 16 points. Alternatively, 3 extremity injuries with an Abbreviated Injury Scale (AIS) score of 2 or more points in association with an injury of another body region with an AIS score of 2 or more points had to be present. Patients were required to have a long bone midshaft fracture of the lower extremity eligible for antegrade intramedullary (IM) fixation and be between 18 and 65 years old. In addition, the thoracic AIS value had to be less than 4 points. The exclusion criteria included previous polytrauma, body weight >250 lbs, open epiphyseal plates, and multiple premorbid conditions. Among these conditions were cardiac insufficiency, coronary insufficiency, cardiac transplantation, pulmonary hypertension, emphysema, pulmonary disease requiring medical treatment, lung transplantation, previous acute respiratory distress syndrome (ARDS), and previous malignancy. In addition, patients were excluded if a critical clinical condition was observed during their emergency room treatment (patients in unstable or extremis condition,12 chest trauma AIS score >2 points), a systolic blood pressure <90 mm Hg despite fluid therapy, requirement of vasopressors, anuria, severe head trauma requiring craniotomy or medication to lower intracranial pressure, intracranial pressure >25 mm Hg, core body temperature <32°C, and a platelet count <80,000/μL blood.
Operational Definitions
The severity of injury was graded on the basis of the NISS.16 To facilitate comparison with other studies, the degree of total severity of injury was also categorized by the Injury Severity Score (ISS), calculated based on the AIS.17
The Revised Trauma Score (RTS) was calculated based on the data obtained on arrival of the patient.18
Severe head injury was defined as morphologic evidence of cranial injury based on an initial computer tomography head scan. The initial neurologic state was evaluated according to the Glasgow Coma Scale.19
Acute lung injury (ALI) was diagnosed when bilateral diffuse infiltrates were present on the chest roentgenogram, pulmonary capillary wedge pressure was less than or equal to18 cm H2O, and the oxygenation ratio (PaO2/FiO2) was lower than 300.20
The severity of thoracic injuries was graded according to the admission chest roentgenogram, the chest roentgenogram at 1 day after admission, and the chest computed tomography, if available. Based on this information, the number of rib fractures was documented. Also, the incidences of pneumothorax, hemothorax, pressure pneumothorax, and lung contusion were assessed.21,22
Systemic inflammatory response syndrome (SIRS) was defined as the presence of the following criteria: body temperature >38°C, heart rate greater than 90 bpm, respiratory rate greater than 20/min or PaCO2 <32 mm Hg, and neutrophil count greater than 12,000/mL or less than 4000/mL. Sepsis was diagnosed by a scoring system.23 Pneumonia was diagnosed if the body temperature was at least 38.5°C and if, in addition, 1 of the following criteria was met: infiltrate on chest roentgenogram in the absence of ARDS or positive culture in bronchoalveolar lavage fluid. Multiple organ failure (MOF) was diagnosed according to a scoring system,24 when at least 3 organs demonstrated a grade II dysfunction. The diagnosis of a fat embolism syndrome was made according to a scoring system.25
Standardization of Study Protocol
Before the start of the study, all participating centers met on several occasions to review the study criteria and procedures, including the methods for randomization and feasibility of the data collection techniques. A steering committee was created for the overall organization of the study (H.C.P., K.G., and H.T.). An adjudication committee (K.G. and S.N.), reviewed patient eligibility. Data safety and monitoring was performed by means of regular meetings of the key investigators (H.C.P., P.G., D.R., E.E.H., and M.M.). All participating centers took part in biannual meetings during which concerns regarding data collection, safety issues, and the accuracy of the data were addressed. All participating centers were included in the authorship. Internal review board approval (no. 2019) was obtained by the coordinating center and each local facility. Informed consent was obtained from the patient or the patient's closest relative.
Subject Recruitment and Randomization
Consecutive patients with blunt multiple injuries in 10 centers were randomized to 2 treatment arms regarding the management of their femur fracture, as outlined below.
Planned Interventions and Their Timing
Patients were randomly treated by either primary (<24 hours) intramedullary femoral nailing or by initial external fixation, followed by secondary intramedullary nailing (damage control orthopedic surgery), as soon as the patient was deemed stable enough for surgery.
Distribution of Subgroups and Determination of the Clinical Status
Further differentiation was made according to the patient's status. Four clinical categories for patient grading were distinguished, as previously proposed (stable, borderline, unstable, or in extremis).12,26 The clinical grading of the patient's status was performed in the emergency room by the attending physician. Treatment group differences were examined separately in the stable and borderline patient groups. Patients in unstable and extremis condition were eliminated from the study.
Endpoints of the study included the incidence of pulmonary complications (ALI).
Assignment and Blinding Procedures
A randomization list was generated by a computerized system provided by the Department of Statistics. Randomization was performed on an individual patient basis. The sequence was numbered by a technical assistant uninvolved in the study, and then printed and inserted into a sealed envelope. Each center was provided with sequential envelopes containing 1 of the 2 treatment strategies. For all patients who met the inclusion criteria, the sealed envelope that contained the type of treatment was opened after completion of the diagnostics and grading of the patient's status to account for the exclusion criteria. The sealed envelope was opened by a physician in the emergency room who was not involved in the surgical care of the patient. The fracture stabilization was subsequently performed by the orthopedic surgeon on call. All patients were assigned after completion of the primary survey according to 1 of the 2 treatment arms described above, after all injuries had been categorized and the inclusion criteria were met.
Stopping Rules
The treating attending physician was permitted to stop the study and proceed with the fixation of the femoral fracture if the patient's status was deemed inadequate to allow randomization. Causes included in the study protocol were unexpected deterioration of the clinical status (hemorrhagic shock, development of uncontrollable bleeding etc) or unexpectedly increased surgical time for fixation of the fracture (eg, diagnosis of vascular injury and limb ischemia).
Fracture classification was graded according to Orthopedic Trauma Organization of North America's classification system,27 and open fractures by a score.28
Primary surgery was defined as an operative intervention within 24 hours after trauma.
Technique of Surgery and Perioperative Documentation
Intramedullary instrumentation was performed in a standardized fashion, using an antegrade technique and usually a piriformis fossa starting point. In some patients, unreamed nailing was performed, based on the preference of the facility and of the surgeon. External fixation was performed as a standardized procedure. There were no limitations regarding the choice of implants. The perioperative assessment included documentation of clinical and laboratory data to assess blood loss, coagulopathy, wound infection, and pneumonia. Local (wound infection, compartment syndrome etc) and systemic complications (ALI, MOF, sepsis) were documented. Pin tract infection was assessed using a scoring system.29
General Treatment
Multiple trauma patients were regularly submitted to intubation and artificial ventilation. For patients included in the study, lost volume was replaced with crystalloid or colloid solutions; hypertonic solutions were not used. Patients underwent repeated arterial blood gas measurements and measurements of central venous pressures by insertion of a central venous catheter.
Data Management and Analysis
All data were collected in a data base designed for the purpose of this study, based on Microsoft Office Access software.
Estimation of Required Sample Size
A power analysis was undertaken before the study. According to this analysis, 150 patients were required to detect a significant difference in the primary outcome variables (ALI and systemic complications) with a power of 80% at an a priori alpha level of 0.05.
Data Analysis
First, analyses were conducted to examine the relation between treatment group (ie, external fixation vs. intramedullary nailing) and variables indexing patient demographic characteristics and initial injury severity. This was done to determine whether the random assignment resulted in similar patient characteristics across the 2 treatment groups. Independent sample t-tests were used to examine treatment group differences for variables that approximated a Gaussian distribution. For nonnormal indicators of injury severity Mann-Whitney U tests were performed. Pearson χ2 tests were performed for binary indicators of injury severity, except when expected cell counts did not exceed 5 participants. When this occurred, Fisher exact test tests were used. A similar set of analyses were used to document that patients classified as being in stable condition exhibited more severe initial injuries, a poorer clinical course, and more clinical complications than patients in borderline condition.
Treatment group differences on postoperative course and complications were examined using regression models. For postoperative course outcomes associated with the number of hours patients spent in the intensive care unit (ICU) and on a ventilator, Cox regressions were used. Specifically, the difference between treatment groups was examined after controlling for differences between the groups on initial injury severity. A Cox regression is appropriate for predicting the time until an event, such as release from the ICU or removal from a ventilator, using 1 or more independent variables. Group differences were quantified using the hazard ratio (HR). For binary outcomes assessing complications during the postoperative course (ie, pneumonia, ALI, ARDS, SIRS, SEPSIS MOF), logistic regressions were used. Again, the association between treatment group status and risk of complications were examined after controlling for differences between the groups on initial injury severity. Group differences were quantified using the odds ratio (OR) in these analyses. For all regression models, robust standard errors were used and P values <0.05 were considered statistically significant. After analyzing treatment group differences on these postoperative course outcomes for the entire sample, these regression models were rerun separately for patients in stable condition and patients in borderline condition.
RESULTS
Nineteen patients were excluded after enrollment, 10 from the external fixation group and 9 from the intramedullary nailing group. All patients were excluded due to detection of additional injuries in the emergency room. The patients excluded from the external fixation and intramedullary nailing groups exhibited comparable injury severity. Therefore the analysis was considered to be by intention to treat. A total of 165 patients were included in the study. The stopping rule was not used in any of these patients.
Overall, the mean age of the patients was 32.6 ± 11.7 years. There were 132 (80.0%) men and 33 women (20.0%). The mean ISS was 25.8 ± 9.6 points, the mean NISS was 29.0 ± 9.7 points, and the mean RTS was 0.88 ± 0.43 points. The mechanism of injury was a car accident in 116 (70.3%) cases, a motorcycle accident in 31 (18.8%), a fall in 4 (2.4%), suicide attempt in 4 (2.4%) and a pedestrian accident in 10 cases (6.1%). Nineteen patients demonstrated bilateral femoral shaft fractures. There were 42 (25.5%) open fractures. Among these, 16 (9.6%) were grade 1 open fractures; 16 (9.6%) were grade 2 open fractures and 10 (6.1%) were grade 3 open fractures. Bilateral fractures were present in 9 patients (12.7%) in external fixation group, and in 10 patients (10.6%) in the intramedullary nailing group. The amount of blood units administered within the first 24 hours was 366.8 ± 695.4 mL.
In terms of postoperative outcomes, the duration of the intensive care unit stay was 239.8 ± 269.9 hours and the duration of ventilation 163.4 ± 216.1 hour. Overall, 21% of patients developed pneumonia, 24% developed ALI, 36% were diagnosed with SIRS, 5% had MOF, and 13% experienced sepsis. There were no diagnoses of intraoperative fat embolism in patients undergoing a femoral nail, and no fat embolism syndrome diagnosed postoperatively. One patient died 1 week after trauma from secondary cerebral herniation.
None of the patients who presented with open fractures required coverage with a muscle flap, free flap or skin graft for the femoral injury. One patient required a skin graft and 1 patient required a muscle flap after an open tibia fracture. No osteomyelitis was observed. In the group submitted to external fixation, a crust was present in 19 (26.7%) patients, serous secretion in 5 (7.04%), inflammation and reddening around the screws in 17 (23.9%) and infection requiring local debridement in 2 (2.8%) patients.
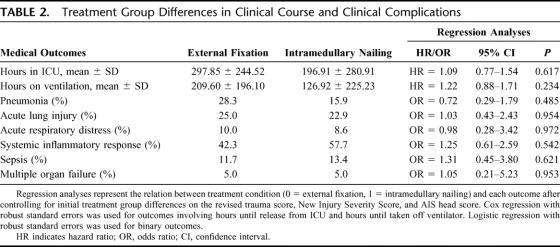
Of the 165 patients in the study, 71 (43.0%) were randomized to the external fixation treatment group and 94 (56.9%) were randomized to the intramedullary nailing treatment group. Comparisons between the 2 groups on demographic characteristics and initial injury severity are presented in Table 1. Analyses indicated that patients in the external fixation group exhibited significantly higher RTSs, ISSs, and head trauma scores than patients undergoing initial intramedullary nailing of the femur. No other statistically significant differences between the 2 groups in terms of demographic characteristics or initial injury severity were found. For example, there was no difference in the number of open versus closed fractures across the 2 treatment groups, with 16 (22.5%) open fractures in the external fixation group and 26 (27.7%) in the intramedullary nailing group. There were 6 (8.5%) grade 1 open fractures in the external fixation group and 10 (10.6%) in the intramedullary nailing group; 7 (9.8%) grade 2 open fractures in the external fixation group and 9 (9.6%) in intramedullary nailing group; 3 (4.2%) grade 3 open fractures in the internal fixation group, and 7 (7.4%) in the intramedullary nailing group. Bilateral fractures were also similar across the 2 groups, with 9 patients (12.7%) from external fixation group and 10 patients (10.6%) from intramedullary nailing group experiencing bilateral fractures.
TABLE 1. Treatment Group Differences on Demographic Characteristics and Initial Injury Severity
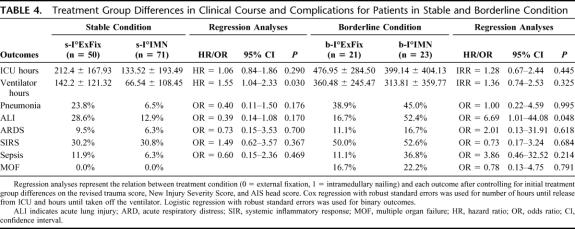
Comparisons between the 2 treatment groups on indices of postoperative course and complications are present in Table 2. Because patients in the external fixation group exhibited more severe injuries than patients the intramedullary nailing group as indicated by their higher RTS, NISS, and head trauma scores, these indices of injury severity were statistically controlled for in regressions examining treatment group differences on postoperative outcomes. Results indicated that there were no significant differences between the 2 treatment groups in terms of postoperative course and complications after accounting for group differences in initial injury severity.
TABLE 2. Treatment Group Differences in Clinical Course and Clinical Complications
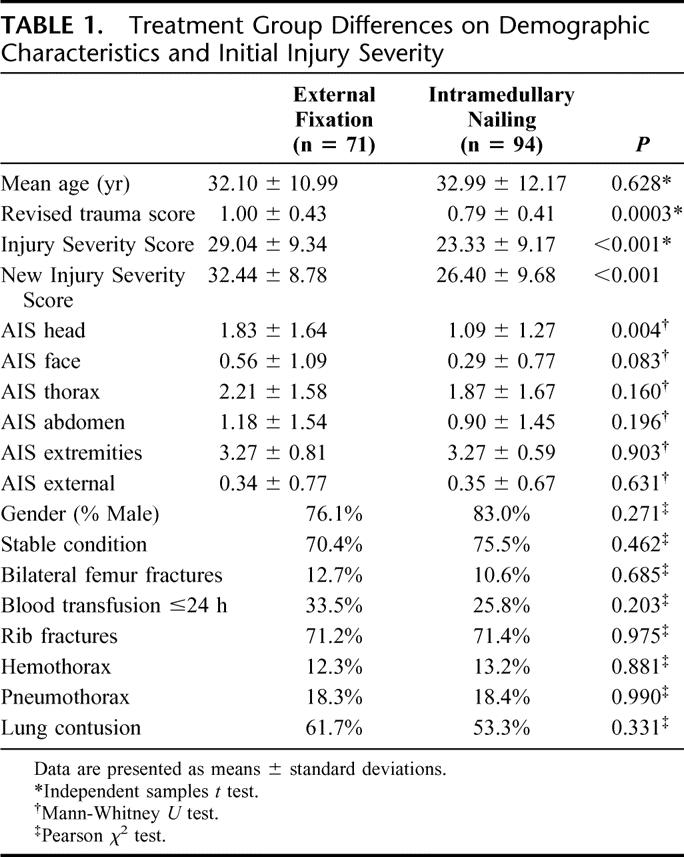
Analyses documenting differences between stable (n = 121, 72.7%) and borderline (n = 44, 27.3%) patient groups in terms of initial injury severity and postoperative outcomes are presented in Table 3. These analyses validated the notion that borderline patients have significantly worse injuries and postoperative outcomes than stable patients. In terms of initial injury, borderline patients demonstrated higher scores on the revised trauma index, injury severity index, and head and thorax injury indices in comparison with stable patients. Borderline patients were also more likely to have a bilateral femoral fracture, a hemothorax, and require a blood transfusion within 24 hours of admission in comparison with stable patients. In terms of postoperative outcomes, borderline patients spent more hours in the ICU and more hours on ventilation in comparison stable patients. Borderline patients were also more likely than stable patients to experience clinical complications such as ALI, SIRS, sepsis, and MOF.
TABLE 3. Differences Between Stable and Borderline Patients on Initial Injury Severity, Clinical Course, and Clinical Complications
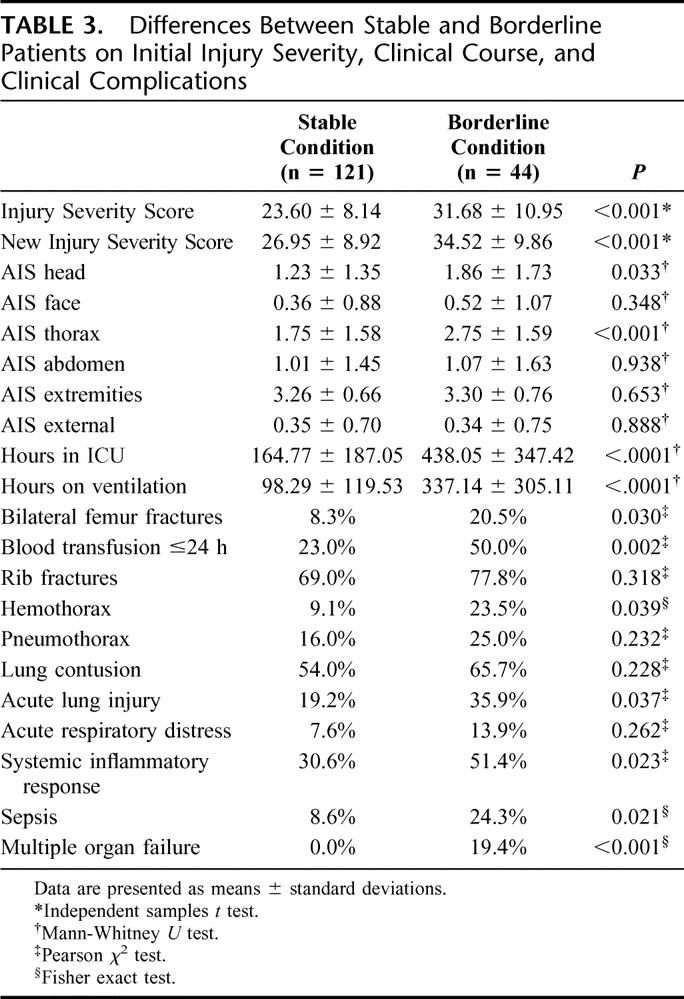
The final set of analyses examined the influence of treatment group status on postoperative clinical course and complications separately for stable and borderline patients (Table 4). Again, regression analyses statistically controlled for differences between the 2 treatment groups in terms of initial injury severity (ie, RTS, new injury severity index, head injury score) when examining group differences. For patients who presented in stable condition, those who underwent intramedullary nailing experienced a shorter duration on a ventilator in comparison with those in the external fixation condition. In contrast, borderline patients that underwent initial nailing of the femur had a higher incidence of ALI in comparison with those who underwent external fixation. After adjusting for initial injury severity, the odds of developing ALI were 6.69 times greater in borderline patients who underwent intramedullary nailing in comparison with those who underwent external fixation.
TABLE 4. Treatment Group Differences in Clinical Course and Complications for Patients in Stable and Borderline Condition
DISCUSSION
For patients with severe injuries and those in uncertain or critical condition, general surgeons modified their surgical treatment strategy for multiply injured patients more than a decade ago. A temporizing approach (damage control) was developed to focus on initial hemorrhage control only, followed by definitive care of the lesion once the patient had been stabilized. The clinical course of patients undergoing the temporizing approach has been so convincing that a prospective randomized study has not been required to achieve these management changes.30–36 In contrast, in the orthopedic literature a longstanding controversy continues regarding whether or not initial surgical stabilization of major extremity fractures should be definitive in all cases, or if in certain subgroups, the surgical procedure creates a secondary insult and should be avoided.10,37 The available retrospective studies have been criticized because of the long study period,38 the inclusion criteria, the injury severity, the inclusion of isolated fractures,9,10,39 the distribution of additional injuries (chest trauma)40,41 or the fixation method.42 So far 3 prospective randomized studies have investigated the effect of fracture fixation on the postoperative clinical course. These studies examined the timing of fracture stabilization (traction vs. surgery within or after 24 hours after injury),10 or the effects of the operative procedure (reaming vs. nonreaming of the femoral canal) on the clinical course.13,14 To our knowledge, the present study is the first prospective randomized trial that investigates whether temporary or definitive initial fixation (external fixation vs. nailing) of the femoral shaft fracture is advantageous, in regard to the clinical condition. Despite the prospective randomized protocol, several limitations have to be considered in the current study.
First, because of the differences in injury severities between the 2 intervention groups (external fixation vs. intramedullary nailing), one may wonder whether selection bias has occurred. However, to minimize this risk, group assignment was determined by a numbered and sealed envelope, which was sent to the participating centers. Therefore, all investigators were unaware of which group a patient would be assigned until consent was obtained and the patient was found appropriate for inclusion in the study. We therefore feel that selection bias can be ruled out as a cause for the differences in injury severity described above. In this line, it is of note that uneven distributions are unavoidable despite use of a prospective randomized study design.43–45 In addition, this concern has been addressed by using a multivariate analysis, which corrected for the differences in injury severity and distribution (eg, head injuries).
Second, most studies performed in single institutions1,6,9,10 have used ventilation time as an end point. We chose not to do so because the protocols for weaning patients off the ventilator may have differed between the participating institutions and standardization was not possible. In line with this, none of the 3 previous prospective randomized studies10,13,14 has included a protocol for weaning. Their main groups demonstrated a similar variation in ventilation times as the current investigation. In addition, ventilation time is well known to be influenced by the presence of severe head trauma.46,47 Although patients in the external fixation group exhibited higher levels of head trauma than those who underwent intramedullary nailing, patients in stable condition who received external fixation had a longer duration on a ventilator than those who received intramedullary nailing, even after controlling for differences in initial injury severity. As a result, external fixation should not be recommended for patients in stable condition as it produced no added benefits in terms of clinical complications, and seemed to delay clinical recovery. This finding confirms previous studies, namely Bone's hallmark publication in that early fracture fixation in stable patients is beneficial.10
Third, criticism may arise because ALI was the main end point and no further significant group differences in life threatening complications were detected apart from ALI. However, similar trends occurred in the other parameters and these were associated with sustained changes in the ORs. Moreover, ALI is known as a distinct clinical complication48,49 and has been used as a relevant and reliable end point in numerous previous prospective investigations, and may have sustained clinical sequelae.50,51
Fourth, the sample size may be viewed as being too small. However, the current study overlooks 165 patients with multiple injuries, among whom 44 were in uncertain condition. In comparison, the previous largest prospective randomized publication summarized 83 patients with multiple injuries.10 Other prospective randomized studies had a smaller sample of patients with multiple injuries.13,14 Among the retrospective studies, Reynolds et al52 looked at the influence of chest trauma and summarized the data of 105 multiply injured patients from a single institution over a 10 year period. Among these, they compared 35 patients undergoing early (<24 hours) nailing versus 13 patients undergoing nailing 24 to 48 hours after injury. They describe that the incidence of pulmonary complications was slightly higher in patients who received an intramedullary nail <24 hours, but no significant difference was measured and the data were not controlled for injury severity or other variables, such as the presence of head trauma.52 Most recently, the effect of failure to perform a damage control approach on mortality was reported from a large data base. There were 64 patients who had recognized errors in care that contributed to their death. In 5 of them (7%), these were associated with unduly long initial operative procedures.53 Thus, in view of significant differences based on our multivariate analysis, we feel that the data set is solid despite a limited number of patients in the borderline subgroup.
Also, there is ample evidence that patients in uncertain and critical condition are at high risk for complications and death if they are submitted to inappropriate initial surgical strategies.6,7,9,14 Based on meetings with the participating centers and suggestions by the Institutional Review Board committees, it was deemed unethical to randomize patients with high ISSs and those at high risk of developing complications due to their injury distribution. Finally, had the inclusion of patients with very severe injuries been performed, we would most likely have found more life threatening complications, but differentiating these complications induced by the injuries and the effects of the initial surgery might not have been possible.3,5,9,35,37,38
In contrast to the potential drawbacks discussed above, we have tried to control for several other variables that might interfere with the reliability of our data. Chest trauma is a major risk factor for the development of pulmonary dysfunction4,21 and was documented in detail, especially in regard to pulmonary contusions.22,54 Bilateral pulmonary contusions were documented separately, because they carry the highest risk for the development of lung failure.55,56 The parameters that were used in this study to quantify the degree of thoracic injuries have previously been demonstrated to differentiate different degrees of chest trauma appropriately.21,22
Only midshaft femoral fractures were studied, because it is well described that the pattern of the femoral fracture has an influence on the clinical course by determining the pressure effects observed during intramedullary fixation.57–59 Previous authors excluded proximal fractures and fracture patterns where an ipsilateral femoral neck or subtrochanteric fracture was present,13 or provided even more specific inclusion criteria.14
Finally, the grading system12,26 for differentiating between stable and borderline patients seems to have provided a reliable differentiation between a borderline and a stable condition. Patients graded as borderline had a higher injury severity and other parameters indicative that their status was significantly worse. These parameters were obtained before and independent of the surgical procedure (eg, hemoglobin value on admission, RTS). We therefore feel that the results of this study are more valid than the retrospective studies cited above that tried to determine the influence of fracture fixation of the femur and the degree of trauma on the clinical outcome. Our results demonstrate an association between a surgical intervention and the postoperative clinical course in patients with multiple injuries. This seems to be related to the distribution of injuries and severity of certain injury patterns. Specifically, the following key observations were made:
When the 2 treatment groups are compared, patients who underwent initial external fixation were more severely injured and had a higher degree of head trauma. After correction for these differences in initial injury severity, the incidence of general complications was comparable across the 2 treatment groups for the sample as a whole.
For stable patients, there was a longer duration of ventilator care required for patients who underwent external fixation in comparison with those who underwent intramedullary nailing, even after controlling for group differences in initial injury severity.
In patients whose condition was borderline, a higher incidence of ALI occurred in those patients who underwent initial fixation of the femur with an intramedullary nail. In comparison with patients in borderline condition who underwent external fixation, the odds of developing ALI was over 6 times greater in borderline patients who underwent intramedullary nailing.
Regarding the finding that overall there was a similar rate of complications when comparing the 2 methods of treatment, one would expect that the higher injury severity in the subjects that underwent external fixation is relevant for the hospital course, and a higher incidence of complications in this group would be expected. In fact, a trend toward a higher rate of pneumonia was observed. Because all other AIS values were comparable, the higher ISS value is best explained by the higher degree of head trauma in the patients that underwent external fixation. The external fixation group demonstrated a trend toward longer duration of ventilation and of intensive care, which may also be related to the degree of head injuries, which was sustained in 3 patients. The relationship between head injury and an increased duration of ventilation and intensive care therapy has been extensively described and is outlined above.60 In addition, a higher degree of hemorrhagic shock may have altered the clinical course of head injured patients, because the effect of hemorrhagic episodes on the clinical course of head injured patients has been well reported.61,62
The second finding demonstrates that patients with an uncertain (borderline) condition have an increased incidence of pulmonary complications if they undergo early definitive fixation of a femur fracture. The relevance of fracture fixation in regard to the pulmonary changes is supported by a comparable incidence of bilateral lung contusions and other parameters of chest trauma, including the AIS of the chest between the 2 treatment groups. It is noteworthy that a trend toward higher injury severity and a worse trauma score on admission was present in the group that underwent external fixation, indicating that these patients were in potentially worse condition before having their femur stabilized with an external fixateur. In addition, the severity of head injuries was higher in the group randomized to external fixation. These parameters clearly put patients in the external fixateur group at a higher risk of complications. Nevertheless, patients stabilized with an external fixateur developed a significantly lower incidence of ALI than patients that underwent intramedullary nail fixation and there was no difference in the intensive care stay. After correction by multivariate analysis, the index groups differed again regarding their complication rate. Given these considerations, it is very likely that in this subgroup the impact of surgery has had an influence on the hospital course.
This finding is in agreement with data on the inflammatory response, determined from a subset of these patients.63 It is also supported by the results obtained from a trauma registry that proved the importance of the surgical impact on the posttraumatic course.38 Furthermore, a large prospective cohort study has documented clinical benefits for patients who undergo early external fixation followed by conversion to an intramedullary nail.9
One potential drawback to the DCO approach is the development of local infections due to prolonged external fixation, deriving from the pin sites of Schanz screws.64,65 We have previously monitored patients in which the conversion from an external fixateur to an intramedullary device was performed. Patients had an increased risk for an infection if the application of the external fixateur was prolonged, ie, longer than 2 weeks after injury.66 In the current study, the time to conversion from external fixation to intramedullary fixation was 6 (range, 1–20) days. As in other studies,4,6 in selected patients the clinical condition did not improve enough to allow us to perform a timely conversion, but in general this was achieved within the 2 week interval.
In summary, this study confirms that for multiply injured patients in a clinically stable condition, early intramedullary nailing of the femoral shaft fracture continues to be the gold standard for treatment. In contrast, a higher incidence of systemic complications is seen if intramedullary nail fixation is performed for immediate stabilization of the femur fracture in patients who present in a borderline clinical condition. Given this, we believe that the following recommendation is justified: In patients who present with an unclear status, the type of surgical procedure for fixation of a femoral shaft fracture should be carefully selected, according to the initial assessment of the clinical condition. In borderline patients, an external fixateur should be applied for temporizing purposes.
Discussions
Dr. Lewis M. Flint, Jr. (Tampa, Florida): My interest in the role of fracture management in the total care of the injured patient became sharply focused when I had the honor of working with the late Dr. John Border and the recently deceased Dr. Roger Seibel at the trauma center in Buffalo, New York.
The report that Dr. Pape lists as reference number 1 in the bibliography of his paper is the published manuscript Border presented to the meeting of this Association in 1985. The 1985 report recounted the results achieved by Dr. Border's team with the use of early definitive fixation of femur fractures as a means of reducing the risk of post-injury sepsis and pulmonary failure in the injured patient.
John Border felt that early control of all surgically repairable injuries, including femur fractures, combined with aggressive protein based nutrition and early mobilization of the patient were keys to reducing the risk of these complications. The elimination of prolonged femur traction and the mobilization of the patient out of what John termed the “supine crucifixion position” were, he felt, critical components leading to the success of this approach. He restricted this approach to patients who would be able to get out of bed after fracture repair and his patients were clinically more like those in your “stable” group.
Over time, trauma surgeons and trauma orthopedic surgeons have extended this approach of early placement of intramedullary nails in femur fractures to aggressively treat more severely injured patients and complication rates have increased possibly due to the added inflammatory stimulus of the operation to fix the fracture to a patient whose inflammatory response is already primed. It is also possible that John's emphasis on nutrition and mobilization have not been applied as he originally suggested.
These deteriorating outcomes led to the concept of “damage control orthopedics”, which is the concept under study in this report. Using the damage control approach, patients receive fixation of the fracture using an external frame followed by aggressive critical care to stabilize the patient for a later definitive repair of the fracture with an intramedullary nail.
You have shown an increase in acute lung injury and sepsis as defined by the critical care community when femur fracture fixation with an intramedullary nail is used in severely injured high-risk patients. In my view, however, a major contribution that this report makes is that a series of bedside assessments done early in the resuscitative phase can identify those high-risk patients, and the patients best identified can be assigned to internal fixation. By whatever means the fracture is dealt with, these high-risk patients consume large amounts of resources and are critically ill.
You have also shown, by identifying good risk patients, that there is a group of patients where intramedullary nailing gives better results than internal fixation. Because of the skill of your surgeons and excellent critical care, there were no deaths in the high-risk patients. There were fewer days of critical care support required in the patients assigned to internal fixation. These are important observations. I have several questions.
I have some methodologic concerns. Did all centers contribute patients equally? Your study involved 10 centers over 74 months. This would mean the center would, on average, enroll a patient about every 4 to 5 months. At my center, there are, on average, 5 early femur fracture repairs with an intramedullary nail and 7 external fixation procedures for femur fractures per month. Because of the volume outcome relationship that exists in trauma units, it would be useful to know the contribution from each center and the distribution of complications among centers. Could you please address these issues?
Second, was the protocol for nutrition and mobilization standardized for the enrolled patients? Were these the same for patients treated with intramedullary nails as well as external fixators? How many of each group reached nutritional and mobilization goals?
Finally, I believe most trauma surgeons would agree that damage control is a concept that seems to work and makes clinical sense. Does your study prove its value for high-risk patients with femur fractures or is more data needed from other centers in other countries to confirm this approach?
Dr. Hans C. Pape (Pittsburgh, Pennsylvania): First of all, there is quite a difference in the organization of trauma care between Europe and the United States. First, there is no general versus orthopedic surgeon in the European system. Second, recently orthopedic centers in Europe have been obliged for financial reasons to treat fair numbers of elective trauma cases due to the integration of the DRG system in the German reimbursement. Ever since I came to work in Pittsburgh, my practice has changed and I am taking care of acute fractures only. In the wintertime when things get slower, I do a little bit more elective work in terms of non-unions and corrective surgery of extremities. Also, I have learned that the caseload and the general volume are higher in the United States than in Europe, which is due to the size of the capture area. This may explain the higher patient numbers that you mentioned.
As far as the patient numbers in the centers are concerned, there were differences, of course. We looked specifically at whether variances of the complications depended on specific centers. First of all, we investigated the complication rate in the city hospitals versus the academic centers. There was no difference. We also looked at those who enrolled fewer versus more than 10 patients. And again, there was no difference. The 2 centers who included the largest volume were Hanover and Leeds. And these two did have a slightly higher complication rate, which was unexpected, but then again these 2 centers included patients with the highest injury severity scores. In summary, I do believe that there was no center specific complication rate that could have flawed our results.
As far as the ICU treatment is concerned regarding external fixation versus IM nailing, the same protocol was used and the patients were weaned off the ventilator whenever possible. I am not aware of substantial differences in nutritional status, but I have to admit that we did not focus on that specifically.
As far as further study is concerned, there is a group of 16 centers within the United States that is planning to perform a study with larger patient numbers and which, to my mind, will hopefully add even more to our knowledge.
Dr. Carl E. Bredenberg (Cape Elizabeth, Maine): I have 2 questions. The first is, in the group that initially underwent external fixation, how long was it before they underwent definitive internal fixation? Historically, external fixation was used as a prolonged and often the only treatment, and it is against that standard that early internal fixation was shown to be preferable. Is this an example of what others have described as comparing early fixation versus very early fixation or perhaps early fixation versus too early fixation? My second question, was there evidence of fat embolization consequent to intramedullary nailing?
Dr. Hans C. Pape (Pittsburgh, Pennsylvania): As far as the conversion time is concerned, it certainly is an issue. Orthopedic surgeons are always concerned about intramedullary infection, so it is something that must be kept in mind. The conversion time in the stable patient group was 48 hours and in the borderline patient group was about 5 days. Last year my group published a cohort study in the Journal of Orthopaedic Trauma that looks at the infection rate after external fixation in more than 150 patients. It appeared that the conversion must be performed within a week. Superficial infection mainly occurred in patients in whom the conversion took place after more than 14 days. But even in that subgroup there were no deep infections. Nevertheless, I think we have to look closely at this issue.
Also, another important issue to stress is to try and stabilize the patient as early as possible. The bottom line should be to avoid traction. To my mind it is better to have a patient with a relatively stable leg with an external fixator in the ICU because you never know what will happen during the upcoming posttraumatic days. Even Dr. Border points out that it is better to have a patient stabilized right away with whatever method is available rather than not fixing him with an external fixator and leaving him in traction.
As far as the second question is concerned, we did look specifically at fat embolism. There was no identifiable patient in whom the deterioration was due solely to fat embolism in that borderline group.
Dr. H. Gill Cryer (Los Angeles, California): I have a couple of questions.
First of all, the definition of acute lung injury as you defined it was not clear to me. But the question I have for you is, what was the effect of that? If you developed acute lung injury, how long did they require ventilator support?
The second question I have relates to the group in the external fixator group that developed acute lung injury. Were there any of those that did not ever get definitive fixation as a result of developing ARDS and acute lung injury? Did any of the patients in the external fixator group never get fixed; never get an intermedullary rod, because they developed acute lung injury or ARDS?
Dr. Hans C. Pape (Pittsburgh, Pennsylvania): We looked at the issue of how the acute lung injury affects the general course, and it appeared there was an increase in the ventilation time of about 5 days. Three of the patients with acute lung injury or who developed ARDS in the ex fix group had acute lung injuries in the first place, and there was no case of pulmonary worsening after external fixation.
All patients who had an external fixator were converted to an intramedullary nail. For the stable patients the mean conversion time was 5 days, mainly due to chest trauma; for the borderline group it was 16 days, mainly due to chest and head trauma. I do believe that there may be an issue with patients who are never converted from an external fixateur to an IM nail, but I believe that would be in the patient groups who are more severely injured and in worse condition.
Dr. Jonathan R. Hiatt (Los Angeles, California): My question relates to one of your first answers. In Europe, the orthopedic surgeon is often the traumatologist, and in the United States the general surgeon. Here in the United States we have something of a crisis in specialty support of our trauma centers. In the past our group and others have proposed training for a general trauma surgeon who could perform not only general surgical procedures but also some of the orthopedic and neurosurgical procedures for which we lack support. Could you envision a day when the general surgeon might be able to do early fixation of these fractures?
Dr. Hans C. Pape (Pittsburgh, Pennsylvania): I think that is a very political question. I personally find it helpful to have a general surgeon who is in charge of the general management. In many European centers, the visceral surgery is no longer done by the trauma surgeon. Instead, general surgeons open the abdomen and thoracic surgeons open the chest. When I was the senior attending in Hannover, Germany, we would meet in the emergency room with the general surgeons if there was an abdominal trauma. We would also go to the CT scanner together, and then decide who would do his or her procedures and in which sequence.
Since I came here [to the United States], the situation is very different. I am in the operating room fixing fractures all the time. The general surgeon is the one who takes care of the management, so if I wanted to, I could stop thinking about the general condition of the patient because someone else performs this function for me. Of course, I do think that it is helpful to have somebody who has the whole picture and thinks about the stabilization of the extremity as well as hemorrhage control. After all, it is all about good communication between the Departments.
Footnotes
Members of the European Polytrauma Study on the Management of Femur Fractures (EPOFF) study group: A. Gruner, MD, Braunschweig, Germany; M. Wittke, MD, Celle, Germany; C. Dumont, Göttingen, Germany; K. Grimme, Hannover, Germany; M. Mueller, MD, Kiel, Germany; D. Rixen, MD, Cologne, Germany; J. Morley, MD, Leeds, United Kingdom; R. Stiletto, MD, Marburg, Germany; E. Ellingsen Husbye, MD, Oslo, Norway; and R. Bayeff-Filoff, MD, Rosenheim, Germany.
Supported by AO/ASIF (Grant No. AO/ASIF. 99 P65 and 03 P2).
Reprints: Hans-Christoph Pape, MD, FACS, Director, Division of Trauma, Department of Orthopaedic Surgery, University of Pittsburgh Medical Center 3471 Fifth Avenue Suite 1010, Pittsburgh, PA 15213. E-mail: papehc@upmc.edu.
REFERENCES
- 1.Seibel R, LaDuca J, Hassett JM, et al. Blunt multiple trauma (ISS 36), femur traction, and the pulmonary failure-septic state. Ann Surg. 1985;202:283–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pape H-C, Regel G, Dwenger A, et al. Influence of thoracic trauma and prim. femoral nailing on the incidence of ARDS in multiple trauma patients. Injury. 1993;24:82–103. [DOI] [PubMed] [Google Scholar]
- 3.Wudel JH, Morris JA, Yates K, et al. Massive transfusion: outcome in blunt trauma patients. J Trauma. 1991;31:1–7. [PubMed] [Google Scholar]
- 4.Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopaedics. J Trauma. 2000;48:613–623. [DOI] [PubMed] [Google Scholar]
- 5.Freedland M, Wilson RF, Bender JS, et al. The management of flail chest injury: Factors affecting outcome. J Trauma. 1990;30:1460–1468. [DOI] [PubMed] [Google Scholar]
- 6.Nowotarski PJ, Turen CH, Brumback RJ, et al. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg Am. 2000;82:781–788. [PubMed] [Google Scholar]
- 7.Giannoudis PV. Surgical priorities in damage control in polytrauma. J Bone Joint Surg Br. 2003;85:478–483. [DOI] [PubMed] [Google Scholar]
- 8.Roberts CS, Pape HC, Jones AL, et al. Damage control orthopaedics: evolving concepts in the treatment of patients who have sustained orthopaedic trauma. Instr Course Lect. 2005;54:447–462. [PubMed] [Google Scholar]
- 9.Taeger G, Ruchholtz S, Waydhas C, et al. Damage control orthopedics in patients with multiple injuries is effective, time saving, and safe. J Trauma. 2005;59:409–417. [DOI] [PubMed] [Google Scholar]
- 10.Bone LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of fractures. J Bone Joint Surg. 1989;71:336–339. [PubMed] [Google Scholar]
- 11.Bosse MJ, MacKenzie EJ, Riemer BL, et al. Adult respiratory distress syndrome, pneumonia, and mortality following thoracic injury and a femoral fracture treated either with intramedullary nailing with reaming or with a plate. A comparative study. J Bone Joint Surg Am. 1997;79:799–809. [DOI] [PubMed] [Google Scholar]
- 12.Pape H-C, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients—relevance of damage control orthopaedic surgery. Am J Surg. 2002;183:622–629. [DOI] [PubMed] [Google Scholar]
- 13.Anwar IA, Battistella F, Neimann R, et al. Femur fractures and lung complications—a prospective randomized study of reaming. Clin Orth Rel Res. 2004;422:71–76. [PubMed] [Google Scholar]
- 14.Canadian Orthopaedic Trauma Society. Reamed versus unreamed intramedullary nailing of the femur: comparison of the rate of ARDS in multiply injured patients. J Orthop Trauma. 2006;20:384–387. [DOI] [PubMed] [Google Scholar]
- 15.Bhandari M, Giannoudis PV. Evidence-based medicine: what it is and what it is not. Injury. 2006;37:302–306. [DOI] [PubMed] [Google Scholar]
- 16.Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–926. [DOI] [PubMed] [Google Scholar]
- 17.Baker SP, O'Neill B, Haddon W, et al. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 18.Champion HR, Copes WS, Sacco WJ, et al. A revision of the Trauma Score. J Trauma. 1989;29:623–629. [DOI] [PubMed] [Google Scholar]
- 19.Teasdale G, Jennett B. Assessment of coma and impaired consciousness, a practical scale. Lancet. 1974;13:81–84. [DOI] [PubMed] [Google Scholar]
- 20.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. [DOI] [PubMed] [Google Scholar]
- 21.Tyburski JG, Collinge JD, Wilson RF, Eachempati R. Pulmonary contusions: Quantifying the lesions on chest x-ray films and the factors affecting prognosis. J Trauma. 1999;46:833–838. [DOI] [PubMed] [Google Scholar]
- 22.Pape H-C, Remmers D, Rice J, et al. Appraisal of early evaluation of blunt chest trauma: Development of a standardized score for clinical decision making. J Trauma. 2000;49:496–504. [DOI] [PubMed] [Google Scholar]
- 23.Stevens LE. Gauging the severity of surgical sepsis. Arch Surg. 1983;118:1190–1192. [DOI] [PubMed] [Google Scholar]
- 24.Moore FA, Moore EE, Pogetti R, et al. Gut bacterial translocation via the portal vein: a clinical perspective with major torso trauma. J Trauma. 1991;31:629–638. [DOI] [PubMed] [Google Scholar]
- 25.Gurd AR. Fat embolism: an aid to diagnosis. J Bone Joint Surg Br. 1970;52:732–736. [PubMed] [Google Scholar]
- 26.Pape HC, Giannoudis PV, Krettek C, et al. Timing of fixation of major fractures in blunt polytrauma: role of conventional indicators in clinical decision making. J Orthop Trauma. 2005;19:551–562. [DOI] [PubMed] [Google Scholar]
- 27.Swiontkowski MF, Agel J, McAndrew MP, et al. Outcome validation of the AO/OTA fracture classification system. J Orthop Trauma. 2000;14:534–541. [DOI] [PubMed] [Google Scholar]
- 28.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of Type III open fractures. J Trauma. 1984;24:742–746. [DOI] [PubMed] [Google Scholar]
- 29.Green SA. Complications of external skeletal fixation. Clin Orthop Relat Res. 1983;180:109–116. [PubMed] [Google Scholar]
- 30.Rotondo MF, Schwab CW, McGonigal MD, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–382. [PubMed] [Google Scholar]
- 31.Burch JM, Ortiz VB, Richardson RJ, et al. Abbreviated laparotomy and planned reoperation for critically injured patients. Ann Surg. 1992;21:476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Talbert S, Trooskin SZ, Scalea T, et al. Packing and reexploration for patients with nonhepatic injuries. J Trauma. 1992;33:121–126. [DOI] [PubMed] [Google Scholar]
- 33.Johnson JW, Gracias VH, Schwab CW, et al. Evolution in damage control for exsanguinating penetrating abdominal injury. J Trauma. 2001;51:261–271. [DOI] [PubMed] [Google Scholar]
- 34.Shapiro MB, Jenkins DH, Schwab CW, et al. Damage control: collective review. J Trauma. 2000;49:969–978. [DOI] [PubMed] [Google Scholar]
- 35.Moore EE, Burch JM, Franciose RJ, et al. Staged physiologic restoration and damage control surgery. World J Surg. 1998;22:1184–1191. [DOI] [PubMed] [Google Scholar]
- 36.Hirshberg A, Walden R. Damage control for abdominal trauma. Surg Clin North Am. 1997;77:813–820. [DOI] [PubMed] [Google Scholar]
- 37.Rixen D, Grass G, Sauerland S, et al. Polytrauma Study Group of the German Trauma Society. Evaluation of criteria for temporary external fixation in risk-adapted damage control orthopedic surgery of femur shaft fractures in multiple trauma patients. J Trauma. 2005;59:1375–1395. [DOI] [PubMed] [Google Scholar]
- 38.Pape H-C, Hildebrand F, Pertschy S, et al. Changes in the management of femoral shaft fractures in polytrauma patients: From early total care to damage control orthopaedic surgery. J Trauma. 2002;53:452–462. [DOI] [PubMed] [Google Scholar]
- 39.Buckley R, De Groote R, Powell JP. A prospective randomized trial comparing reamed versus unreamed intramedullary nailing of femoral shaft fractures: assessment of pulmonary dysfunction. In: Proceedings of the Annual Meeting of the Orthopaedic Trauma Association, Vancouver; 1998:111–112.
- 40.Bone LB, Anders MJ, Rohrbacher BJ. Treatment of femoral fractures in the multiply injured patient with thoracic injury. Clin Orthop Relat Res. 1998;347:57–61. [PubMed] [Google Scholar]
- 41.Pape H-C, Auf'M'Kolck M, Paffrath T, et al. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion—a cause of posttraumatic ARDS? J Trauma. 1993;34:540–548. [DOI] [PubMed] [Google Scholar]
- 42.Carlson DW. Femur fractures in chest-injured patients: is reaming contraindicated? J Orthop Trauma. 1998;12:164–168. [DOI] [PubMed] [Google Scholar]
- 43.Bono CM, Tornetta P. Errors in the design of orthopaedic studies. Injury. 2006;37:355–360. [DOI] [PubMed] [Google Scholar]
- 44.Ehrlich PF, Newman KD, Haase GM. Lessons learned from a failed multiinstitutional randomized controlled study. J Pediatric Surg. 2002;37:431–436. [DOI] [PubMed] [Google Scholar]
- 45.Bhandari M, Pape HC, Giannoudis PV. Issues in the planning and conduct of randomised trials. Injury. 2006;37:349–354. [DOI] [PubMed] [Google Scholar]
- 46.Bakay L. Brain injuries in polytrauma. World J Surg. 1983;7:42–48. [DOI] [PubMed] [Google Scholar]
- 47.Siegel JH, Gens DR, Manatov T, et al. Effect of associated injuries and blood volume replacement on death, rehabilitation needs, and disability in blunt traumatic brain injury. Crit Care Med. 1991;19:1252–1265. [DOI] [PubMed] [Google Scholar]
- 48.Kou YR, Bien MY. Ventilatory management of acute lung injury by neurally adjusted ventilatory assist and positive end-expiratory pressure. Crit Care Med. 2006;34:3055–3056. [DOI] [PubMed] [Google Scholar]
- 49.Vincent JL, Zambon M. Why do patients who have acute lung injury/acute respiratory distress syndrome die from multiple organ dysfunction syndrome? Implications for management. Clin Chest Med. 2006;27:725–731. [DOI] [PubMed] [Google Scholar]
- 50.Avecillas JF, Freire AX, Arroliga AC. Clinical epidemiology of acute lung injury and acute respiratory distress syndrome: incidence, diagnosis, and outcomes. Clin Chest Med. 2006;27:549–557. [DOI] [PubMed] [Google Scholar]
- 51.Hough CL. Neuromuscular sequelae in survivors of acute lung injury. Clin Chest Med. 2006;27:691–703. [DOI] [PubMed] [Google Scholar]
- 52.Reynolds MA, Richardson JD, Spain DA, et al. Is the timing of fracture fixation important for the patient with multiple trauma? Ann Surg. 1995;222:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gruen RL, Jurkovich GJ, McIntyre L, et al. Patterns of errors contributing to trauma mortality: lessons learned from 2594 deaths. Ann Surg. 2006;244:371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: Flail chest vs pulmonary contusion. J Trauma. 1988;28:298–304. [DOI] [PubMed] [Google Scholar]
- 55.Cohn SM. Pulmonary contusion: Review of the clinical entity. J Trauma. 1997;42:973–979. [DOI] [PubMed] [Google Scholar]
- 56.Johnson JA, Cogbill TH, Winga ER. Determinations of outcome after pulmonary contusion. J Trauma. 1986;26:695–697. [DOI] [PubMed] [Google Scholar]
- 57.Stürmer KM, Schuchardt W. Neue Aspekte der gedeckten Marknagelung und des Aufbohrens der Markhöhle im Tierexperiment. Teil II: Der intramedulläre Druck beim Aufbohren der Markhöhle. Unfallheilkunde. 1980;83:346–352. [PubMed] [Google Scholar]
- 58.Stürmer KM. Measurement of intramedullary pressure in an animal experiment and propositions to reduce the pressure increase. Injury. 1993;24(3):7–21. [DOI] [PubMed] [Google Scholar]
- 59.Wenda K, Runkel M, Rudig L, et al. The effect of bone marrow embolization on the choice of procedure in the stabilization of femoral fractures. Orthopaede. 1995;24:151–163. [PubMed] [Google Scholar]
- 60.Giannoudis P, Veysi V, Pape H-C, et al. When should we operate on major fractures in patients with severe head injuries? Am J Surgery. 2002;183:261–267. [DOI] [PubMed] [Google Scholar]
- 61.Pietropaoli JA, Rodgers FB, Shackford SM, et al. The deleterious effect of intraoperative hypotension on outcome in patients with severe head injuries. J Trauma. 1992;33:403–407. [DOI] [PubMed] [Google Scholar]
- 62.Jaicks RR, Cohn SM, Moller BA. Early fixation may be deleterious after head injury. J Trauma. 1997;42:1–5. [DOI] [PubMed] [Google Scholar]
- 63.Pape H-C, Grimme K, van Griensven M, et al. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters in a prospective randomized analysis. J Trauma. 2003;55:1–7. [DOI] [PubMed] [Google Scholar]
- 64.Tornetta P, DeMarco C. Intramedullary nailing after external fixator of the tibia. Bull Hosp Jt Dis. 1995;54:5–13. [PubMed] [Google Scholar]
- 65.Blachut PA, Meek RN, O'Brien PJ. External fixation and delayed intramedullary nailing of open fractures of the tibial shaft. A sequential protocol. J Bone Joint Surg Am. 1990;72:729–735. [PubMed] [Google Scholar]
- 66.Harwood PJ, Giannoudis PV, Probst C, et al. The risk of local infective complications after damage control procedures for femoral shaft fracture. J Orthop Trauma. 2006;20:181–189. [DOI] [PubMed] [Google Scholar]