Abstract
Objective:
We sought to identify factors contributing to wrong-site surgery (wrong patient, procedure, side, or part).
Methods:
We examined all reports from all hospitals and ambulatory surgical centers—in a state that requires reporting of wrong-site surgery—from the initiation of the reporting requirement in June 2004 through December 2006.
Results:
Over 30 months, there were 427 reports of near misses (253) or surgical interventions started (174) involving the wrong patient (34), wrong procedure (39), wrong side (298), and/or wrong part (60); 83 patients had incorrect procedures done to completion. Procedures on the lower extremities were the most common (30%).
Common contributions to errors resulting in the initiation of wrong-site surgery involved patient positioning (20) and anesthesia interventions (29) before any planned time-out process, not verifying consents (22) or site markings (16), and not doing a proper time-out process (17). Actions involving operating surgeons contributed to 92.
Common sources of successful recovery to prevent wrong-site surgery were patients (57), circulating nurses (30), and verifying consents (43). Interestingly, 31 formal time-out processes were unsuccessful in preventing “wrong” surgery.
Conclusions:
Wrong-site surgery continues to occur regularly, especially wrong-side surgery, even with formal site verification. Many errors occur before the time-out; some persist despite the verification protocol. Patients and nurses are the surgeons’ best allies. Verification, starting with verification of the consent, needs to occur at multiple points before the incision.
All 427 experiences with wrong-site surgery reported to a statewide system over 30 months were analyzed: 174 reached patients, often before formal site verification. Wrong-side surgery dominated, primarily involving extremities and eyes. Surgeons and anesthesia providers were most often implicated; patients and nurses were most likely to correct errors.
We sought to identify factors contributing to the problem of surgery done in error, specifically doing surgery on the wrong patient, doing the wrong procedure (one other than the one indicated and intended), or doing the procedure on the wrong side, when the structures are symmetrical, or at the wrong location or body part otherwise, such as the wrong digit, the wrong spinal level, or the wrong location within a structure (medial vs. lateral, anterior vs. posterior, proximal vs. distal, etc). With the lack of a conventional shorthand for all the above concepts, we will refer to surgery that is done on the wrong patient, the wrong procedure, the wrong side of the body, or the wrong part of an anatomic structure under a general heading of wrong-site surgery. We recognize that for some, wrong-site surgery has meant an incorrect site within an anatomic structure, such as the hand or spine, and for others, it has meant both specific wrong-site surgery within the intended anatomic structure and the wrong side of a symmetrical structure.
Wrong-site surgery is perceived as a medical error that should never happen, not a medical risk that the patient must accept, and therefore a core patient safety problem. Legally, it qualifies under the principle of res ipsa loquitur. The National Quality Forum (NQF) includes wrong-site surgery events on its list of Serious Reportable Events, commonly referred to as “never events.”1 Several states use that list as the basis for reporting patient safety problems. In some states (eg, Minnesota), these reports are made public. Florida imposes fines and disciplinary actions against surgeons for doing wrong-site surgery. As of July 2006, they had disciplined 45 physicians; 3 had been fined $20,000 each.2
Even without the threat of public disclosure or fines, the cost of wrong-site surgery may be high to more than the patient. There is the potential loss of trust in the provider by the patient. A malpractice claim may result in a settlement or award on verdict in the 6- to 7-figure range in 2005 US dollars.3,4
Kwaan et al5 evaluated wrong-site surgeries reported to a large medical malpractice insurer between 1985 and 2004 and determined that the incidence, based on claims and excluding spinal surgery, was 1 in 112,994 procedures. Put another way, wrong-site surgery was reported to insurance companies or a lawsuit was filed once every 5 to 10 years at any 1 hospital.5
From 1995 to the end of December 2006, the Joint Commission received 532 Sentinel Events that were wrong-site surgeries.6 The Physician’s Insurance Association of America reviewed claims of 22 malpractice carriers insuring 110,000 physicians from 1985 to 1995.7 The study revealed 331 wrong-site surgery cases and 1000 closed malpractice claims involving wrong-site surgery. Minnesota reported 26 wrong-site surgeries during their first year of public reporting and 31 their second year.8,9
In Virginia, a wrong-site surgery was reported in 1 of every 30,000 surgeries, or about 1 wrong-site surgery per month.10 In the State of New York in 2001, a wrong-site surgery was reported in 1 of every 15,500 surgeries.10 Page quotes information from Washington University in St. Louis claiming 4000 wrong-site surgeries annually in the United States, or 1 in 17,000 surgeries, the third most frequent life-threatening medical error.11
Canale has estimated that an orthopedic surgeon has a 25% chance of doing wrong-site surgery during a 35-year career.12,13 A survey mailed to hand surgeons revealed that 21% reported performing at least 1 wrong-site surgery during their careers, 63% of which were wrong-finger surgeries.14 Wrong-site surgery for hand procedures was estimated to be 1 in 27,686 in this study.14
In June 1994, the Canadian Orthopedic Association published a position paper on wrong-side surgery in orthopedics.15 From 1994 to 1996, they conducted a major education campaign to eliminate wrong-site surgery in this specialty.16 In 1998, the American Academy of Orthopedic Surgeons endorsed a similar program.13,16 The North American Spine Society followed in 2001.17 The American Academy of Ophthalmology and affiliated societies issued a joint statement on eliminating wrong-site surgery of the eye in the same year.18 The Association of Perioperative Registered Nurses issued their first position statement on correct-site surgery in 2001,19 followed by the American College of Surgeons in 2002.20 The Joint Commission published a review of wrong-site surgery in their Sentinel Event Alert in 1998,21 made the elimination of wrong-site surgery one of their first National Patient Safety Goals in 2003,22 and required compliance with a Universal Protocol for the elimination of wrong-site surgery in 2004.22,23 The NQF endorsed the Universal Protocol in 2006.24 The Veterans Health Administration developed a comprehensive policy in 2004.25 Several states require or recommend specific wrong-site surgery protocols.22,26,27
The Canadian Orthopedic Association and American Academy of Orthopedic Surgeons have both emphasized marking the operative site.15,16 The Joint Commission requires, as part of its Universal Protocol, doing a preoperative verification involving the patient, marking the operative site, and doing a time-out just before starting the procedure.22,23 The United Kingdom’s National Patient Safety Agency (NPSA) and the Royal College of Surgeons of England have a checklist with similar elements.28,29 The North American Spine Society has a similar protocol with the additional of confirming vertebral levels with intraoperative radiographs.30,31 The Veterans Health Administration has 2 members of the OR team review pertinent radiographs before starting the procedure.25
To date, no definitive scientific studies have been published on the efficacy of these recommendations and no one has reported a significant decrease in the incidence or number of wrong-site surgery events. It is difficult to determine a true incidence, not only because of the lack of a standard threshold for what constitutes wrong-site surgery and documented under-reporting by healthcare providers,32 but also because the denominator of potential opportunities for each of the distinct wrong-site errors is unknown. In addition, the number of surgical procedures needed to show a statistically significant difference between 2 incidences of rare events is enormous.33 However, any reduction of this relatively rare adverse outcome other than a prolonged period without any events is not an improvement, in our opinion.
The number of sentinel events reported to the Joint Commission has not changed significantly, despite the required use of the Universal Protocol,6,22 nor has the number of reports changed in New York, despite their efforts,34 or Florida, despite fining errant providers,2 or in Minnesota, despite mandatory public reporting.8,9
Since June 28, 2004, the Pennsylvania Patient Safety Authority has been collecting and analyzing reports of events involving the clinical care of a patient in a medical facility that either results in an unanticipated injury or could have injured the patient (near misses), under the mandate of state law. The law requires reporting of these events from all hospitals and ambulatory surgical facilities across the state, among other medical facilities, with the protection of confidentiality, for the purpose of shared learning.35 Pennsylvania is the only state requiring reporting of “near miss” events that do not harm patients. The reporting is done using a statewide electronic reporting system called the Pennsylvania Patient Safety Reporting System (PA-PSRS). As analysts under contract with the Patient Safety Authority, we chose to analyze reasons for the failure of the existing solutions to eliminate wrong-site surgery.
PATIENTS AND METHODS
We reviewed all reports from all hospitals and ambulatory surgical centers in Pennsylvania to PA-PSRS. Reports involving wrong-part, wrong-side, wrong-procedure, and wrong-person surgery from the initiation of the statewide reporting requirement on June 28, 2004 until December 31, 2006 were identified, reviewed, and analyzed. We excluded surgery done outside an operating room (OR) or ambulatory surgical center, changes to a planned procedure as a result of pathology revealed by the operation, surgery involving wrong prostheses (such as an incorrect-size intraocular lens or a wrong-side artificial knee), intended procedures with improper techniques, cancellations or delays because of wrong test results, events outside the OR arena that led up to the problem in the OR (eg, the cause of a mislabeled biopsy report), inadequate preparations of patients for surgery, and medication errors or allergic reactions.
Each report was reviewed when submitted and assigned a wrong-site category. Reports with novel aspects were discussed and analyzed at a weekly meeting. If a report contained puzzling information, clarification was sought from the reporter. To ensure capture of all reports of wrong-site surgery, we searched the entire PA-PSRS database using keywords associated with descriptions of wrong-site surgery in report narratives.
Wrong-site surgery reports were classified by type of wrong-site error, the body part involved, and the extent to which it affected the patient. Based on all the information reported about each event, assessments were made about the initial source of the error, contributing factors, cues to recovery if any, and methods of verification during the recovery process, if any.
The ways in which wrong-site errors affected the patient were classified into 4 groups: errors not reaching the patient (near misses, documentation errors, or management of specimens), errors touching the patient, but not violating the informed consent (eye drops, surgical preparation involving the wrong site, or preliminary imaging), errors that resulted in initiating procedures covered by consents and belated recovery (regional anesthesia, skin incisions, or incomplete operations), and errors resulting in completion of wrong-site definitive procedures in an OR (both open and closed).
We listed each step of an operation mentioned in any report of wrong-site surgery from the diagnostic test result that triggered the consultation to the postoperative documentation of the procedure. If a step was implicated as the source of an error or contributing factor for an error, the implication was noted, along with whether the error at that step was associated with an event that did not reach the patient, an event that did touch the patient or initiate a procedure with belated recovery, or an event that resulted in a complete wrong-site procedure. Likewise, if a step was implicated as the cue for recovery, successful or not, or as a source of verification enabling recovery, a notation was added to the appropriate consolidated outcome group. We calculated a net contribution to prevention or presence of wrong-site surgery by subtracting all the factors contributing to events that, at minimum, led to wrong-site patient contact from the factors associated with recovery and no patient contact.
RESULTS
During the 30-month period, 433,528 reports to PA-PSRS were reviewed, included in the database, and mined for reports of wrong-site surgery. We identified 427 reports involving wrong-site surgery in an operating venue. Of these reports, 253 described events that did not touch the patient and 174 that did touch the patient. Of the 379 acute-care facilities reporting to PA-PSRS, 129 submitted wrong-site surgery reports, 97 submitted reports describing events that touched the patient. Using a high threshold of an incision at a wrong site, 18 institutions had >1 wrong-site surgery within a 12-month span.
Of the 427 reports, 239 (56.0%) were near misses, where the error was caught before any care was rendered. Then, in rough chronological order, the error was identified following a preliminary radiograph on the wrong patient according to 1 report (0.2%), following topical medication instilled in the wrong eye according to 9 reports (2.1%), following insertion of intravenous or arterial catheters in inappropriate locations for the operations by anesthesia providers according to 4 reports (0.9%), following initiation of anesthesia at a wrong site according to 39 reports (9.1%), following initiation of general anesthesia according to 1 report (0.2%), following injection of an isotope in a wrong site according to 1 report (0.2%), and during “shaving” (sic) of the wrong operative site according to 2 reports (0.5%). Although these 57 wrong-site errors (13.3% of all reports) were corrected before the incision was made, another 33 (7.7%) were corrected only after the initial skin incision was made, according to 19 reports (4.4%), or in midprocedure, according to 14 reports (3.3%). Wrong-site errors were never corrected according to 83 reports (19.4%); 9 (2.1%) reported completion of wrong-site procedures involving puncture wounds only and 74 (17.3%) reported completion of wrong-site procedures involving an incision. Wrong-site errors did not stop with the end of the surgical procedure. Another 13 wrong-site errors were reported involving mislabeled specimens (3.0%): 6 indicated the wrong side; 5 the wrong patient; 1 the wrong site; and 1 was not specific about the labeling error. Finally, 2 errors were reported involving postoperative documentation of the surgical procedure (0.5%): 1 indicated that the wrong side was documented and 1 incorrectly documented a principle procedure that was not done. This last report described 2 errors, the other being a preliminary radiograph on the wrong side that erroneously led to the cancellation of the principle procedure—an error that was not identified until after the patient left the OR (with the procedure erroneously documented as having been done).
Wrong-side surgery was the dominant form of wrong-site surgery, described in 298 reports (70%). Next were other wrong-part reports involving wrong locations (spinal level, digit, medial vs. lateral, anterior vs. posterior, proximal vs. distal, etc.), described 60 times (14%). The wrong procedure was described in 39 reports (9%). The wrong patient was reported 34 times (8%). The numbers and percentages are >427 and 100% because 4 reports described 2 errors each. Two reports involved both wrong side and wrong part (eg, right knee vs. left hip). One patient received a wrong procedure as a result of being misidentified as another patient and was counted in both categories. One report, mentioned in the preceding paragraph, described 2 separate types of errors during 1 encounter: wrong side and wrong procedure.
There were significant differences in the extent to which wrong-site surgery errors were perpetuated according to type of error. Wrong-side errors were significantly more likely to be caught as near misses or during the injection of anesthesia in the wrong location and less likely to go on to complete wrong-side operations. Wrong-part surgery, typically surgery at the wrong vertebral level, was significantly less likely to be caught before starting and more likely to result in a complete operation, probably because of the reliance on intraoperative imaging to verify the vertebral level. Wrong procedures were also significantly more likely to be continued to completion. On review, the most common theme for wrong procedures was that the actions were based on faulty documented information and/or reliance on memory. Wrong-patient errors were also significantly more likely to be caught as near misses at the beginning of the case and less likely to be caught after patient contact, specifically during anesthetic blocks. Wrong-patient errors were significantly more likely than wrong-side or wrong-part errors to be involved in incorrect labeling of specimens. (A tabulation of these results is available from the authors upon request.)
Most wrong-site surgeries involved symmetrical anatomic structures. Of the 334 reports in which 361 anatomic structures were mentioned, 100 (30%) involved the legs, 48 (14%) involved the arms, 80 (24%) involved head or neck structures, 69 (21%) involved the genital, urinary, pelvic or groin structures, 22 (7%) involved the lumbar structures, 20 (6%) involved the chest, and 10 (3%) involved the breast. The colon was involved in 5 reports, including 3 wrong-side surgeries, 1 to completion. One report involved the proper identification of fetal twins for a selective abortion. No reports involved the heart, although 2 involved the harvesting of saphenous veins for coronary artery bypass grafts from the wrong leg (included above). No reports involved the liver, biliary system, pancreas or spleen. No correlations were done with the type of error or extent of error because of the large amount of missing information in this category. (A complete, detailed list is available from the authors upon request.)
We noted 46 steps described in the reports. The step most commonly implicated as an initial source or a contributing factor for wrong-site error with patient contact was the one describing the actions of the surgeon in the OR, occurring in 92 reports (53% of patients touched). Failures of the formal time-out process, described in 59 reports (34%), included doing the time-out before positioning the patient (1), starting the operation before or during the time-out (8 and 2 respectively), and otherwise not following the time-out procedure correctly (17). The time-out process failed to prevent contact with the wrong-site in 31 reports. In 17 reports, the wrong-site contact occurred before the time-out, usually with anesthetic interventions, but 14 complete wrong-site procedures were done despite time-outs described without shortcomings. Related to the failures of the formal time-out process were the failure to do a separate time-out for a distinct second procedure on a patient (1), the failures to include multiple procedures in the formal time-out process (4), and the failures to include information about the site of secondary parts of a procedure (such as vein harvesting) in the formal time-out process (5).
The actions of the anesthesia provider in the OR were described in 29 reports (17%). In all but one, these anesthetic interventions at the wrong site were corrected and did not result in completed wrong-site surgery. Fourteen steps—involving documentation, review, or verification of patient information, such as diagnostic tests, office records, consents, patient records, operative schedules, and patient identification—were implicated a total of 145 times in the reports, with some reports mentioning problems with more than 1 such step. Problems with the diagnostic test motivating the surgery were implicated a total of 49 times and included both inaccurate information in the report (16) and the failure to review the study (18), inaccuracies included the patient’s name (5), the side of the pathology (2), and the interpretation of the test (8). Incorrect consents were implicated in 12 reports (7%) and incorrect information in the surgeons’ office records was implicated in 11 (6%). Office records not being available as a source of verification in the OR area contributed to 4 complete wrong-site procedures according to reports.
Errors in positioning the patient and preparing the operative site were implicated in 20 reports (11%) and a related step, application of a surgical tourniquet, was implicated by 2 reports (1%). Patient and/or family provided incorrect information, a factor in 17 reported events (10%) including 11 complete wrong-site procedures. Failures to verify using site markings were implicated in 16 reports (9%) and problems with marking the operative site were implicated in 6 reports (3%). The problems consisted of 2 failures to mark the site, 2 incorrect markings, and 2 obliterations of the marks.
The most common error mentioned in the reports was incorrectly scheduling the procedure. Errors in scheduling were mentioned in 111 of 427 reports, but were only implicated in 7 of the events with patient contact (4%).
Although incorrect information from patients and/or families was a factor in 17 reports of wrong-site contact, correct information from patients and/or families was most commonly implied as a cue or resource for complete recovery from an impending wrong-site surgery, with 57 reports (23% of the reports that never involved patient contact). Although the actions of surgeons in the OR were the most common factor implicated in reports of wrong-site contact, surgeon involvement in the reconciliation and verification process in the preoperative holding area was ascribed as a resource for preventing wrong-site surgery in 49 reports (19%). Although incorrect consents were implicated in 12 reports of wrong-site contact, verification against proper consents aided full recovery according to 43 reports (17%) and belated recovery after contact in another 5. Similar experiences were cited for 41 reports of verification against information from the patient’s medical record for the encounter (16%) and 33 reports of verification against the surgeons’ office records (13%).
The nurses doing reconciliation and verification in the preoperative holding area were consistently effective in catching errors before they reached the patient. They were involved in the successful correction of the 30 impending errors they identified (12% of all reports without patient contact). Although surgeons were also effective in preventing wrong-site surgery in the preoperative holding area, as noted above, they were less effective in preventing wrong-site errors once in the OR. They were involved in 23 recoveries overall, but only 11 before the patient being touched (4% of such reports). The other 12 included 3 reports of needle punctures, 4 reports of skin incisions, and 2 reports of partial operations before the surgeons recognized the wrong-site errors in addition to 3 caught before the invasive parts of the procedures were started. The circulating nurses in the OR were less successful than their preoperative counterparts. They noticed 21 wrong-site errors, but only 7 reports indicated recovery before patient contact (3% of such reports). Although 12 reports described recoveries occurring after patient contact, 2 additional reports indicated unsuccessful attempts at recovery with completion of wrong-site surgery nevertheless. Both surgeons were questioned about what they were doing and replied that they would proceed.
Some recovery efforts may be less effective than others. For example, the formal time-out process was mentioned as a recovery effort in 16 reports, but only prevented initial wrong-site contact in 9. It was done but was ineffective in preventing wrong-site surgery according to 1 report, was done and caught the error after the surgeon began the operation in 2, and was done after the initial anesthetic block and/or preparation of the operative site in 4.
We looked at the net contribution of each step in the operative experience to the development or prevention of wrong-site contact. We estimated this by calculating the net positive contribution of each step to preventing the occurrence of wrong-site contact (recovery with no contact minus development with no contact), then calculating the net negative contribution of the step to the development of wrong-site contact (development with any contact minus recovery efforts when contact occurred), then calculating the difference between the net positive contribution preventing contact and the net negative contribution when contact occurred. The actions of surgeons verifying the reconciliation process in the preoperative holding area had the greatest net contribution (+42) to the prevention of wrong-site errors. Information provided by the patient or family was next (+38), followed by verification against the surgeons’ office records (+29), verification against a proper consent (+25), and verification against information from the patient’s medical record for the encounter (+22). The nurses in the preoperative holding area and the circulating nurses in the OR were equally effective at identifying errors (+17), although as mentioned above, the nurse in the preoperative setting was able to have more impact earlier in the process.
The most commonly implicated factor reported in the development of wrong-site errors was scheduling of the procedure with the OR (a net −99), but it was only implicated in 7 events that touched the patient, as noted above, with 2 contributions to recovery for a net −5. The actions of the surgeon in the OR was the predominant factor implicated as contributing to, rather than preventing, complete wrong-site procedures (a net −62 complete wrong-site procedures and a net −71 overall). Patient information that was inaccurate contributed to a net −47, with inaccurate consents contributing to an additional net −28 and inaccurate reports of definitive diagnostic tests contributing to an additional net −23.
Failures in the formal time-out process contributed to a net −45, including a net −24 complete wrong-site procedures and a net −28 additional wrong-site errors that reached the patient, offset by only 7 recoveries before patient contact. Failures in marking the operative site contributed to a net −30, although only a net −6 contributed to patient contact. Positioning the patient and/or preparing the operative site contributed to a net −26, including a net −8 complete wrong-site procedures, a net −12 other wrong-site patient contacts, and a net −6 errors completely corrected by other mechanisms. Actions of the anesthesia providers in the OR contributed to a net −26, all involving anesthetic interventions at a wrong site. Improper labeling of specimens contributed to a net −13 wrong-site reports, none of which resulted in direct patient contact.
Looking just at how often factors were cited in reports, consents were most commonly included (n = 124), followed by scheduling (n = 123), actions of surgeons in the OR (n = 117), verification by patients and/or families (n = 86), and the formal time-out process (n = 77). The factors mentioned the least included multitasking (n = 1), emergencies (n = 2), wristband identification (n = 3) and transport to the OR (n = 9).
(A complete tabulation of all these results is available from the authors upon request.)
DISCUSSION
In contrast to Kwaan’s threshold of professional liability,5 we used a much more inclusive threshold of any wrong-site error that reached the patient physically, on the premise that a wrong-site error resulting in a claim was the tip of an iceberg and that a lesser error was both a bellwether and a potential loss of trust by the patient. Of the 188 wrong-site errors that got past the original preoperative screening process, 30% were corrected after preliminary imaging studies or isotope studies were done, topical eye medications were given, intravascular catheters were inserted, anesthetic blocks were done at incorrect locations, general anesthesia was started, or preparation of the surgical site was started; 18% were corrected sometime after the surgical procedures were started; and 44% were never corrected. The remaining 8% occurred after the procedures were finished.
Although the devastating outcome of a wrong-site surgery serious enough to result in a professional liability claim is rare and we do not know the number of opportunities for wrong-site surgery in the OR to calculate a true incidence, we can currently anticipate a report of a wrong-site surgery event reaching a patient in an operating room an average of once each year in a 300-bed hospital. Given the preponderance of wrong-side errors relative to the others, it is not surprising that surgeons who work on symmetrical structures may have a 1 in 4 chance to be involved in a wrong-site error during their careers.12,13 Based on the anatomic structures involved in the reports, virtually all surgical specialties are vulnerable to wrong-site surgery.
Our analysis was based on interpretations of written reports, primarily of narratives by people who were involved with or investigated a wrong-site event in their institution. Many reports described events from the nurse’s perspective. None were obviously from the perspective of the surgeon or anesthesia provider. The authors did not do any independent analyses of the events on-site.
Although reporting of near-miss as well as actual wrong-site surgery events is mandatory and compliance is checked by Pennsylvania Department of Health inspectors, the ratio of near-miss reports to complete wrong-site surgeries varied from 0:1 for 31 facilities to 28:1, with an average of 5:1 among the 33 reporting near misses. We inferred that not all facilities report successful recovery using established processes, such as time-outs and marking of the operative site. Nevertheless, the authors believe that the information about recoveries obtained as a result of the requirement in Pennsylvania to report near-miss medical errors provided invaluable insights not available from information of complete wrong-site events, such as those reported to the Joint Commission sentinel event database or other patient safety databases using the NQF Serious Reportable (“never”) Events as the criterion.
The reporting of events associated with wrong-site surgery obviously implies breakdowns in the steps in place to prevent such occurrences, especially those steps critical to preventing such errors. Our interest was noting the relative strength of these steps by comparing the near-miss events with and the other events without successful recovery. The current emphasis is on asking the patient to indicate the site, marking the site, and following a formal time-out process just before the incision. Although one might presume that all errors were due to failures of human performance in these and other tasks, we noted some errors that would not be caught by conventional procedures in the OR. For example, 1 patient had an operation based on a pathologic diagnosis that was dictated under his or her name, but belonged to another patient. The error was perpetuated throughout the operative experience and was not discovered until examination of the removed organ showed no evidence of disease. One patient was given incorrect information, which she then forwarded to the operating team. Another report involved a selective abortion of an abnormal twin fetus, where identification could not be done by standard means.
In the opinion of the authors, a single time-out just before the incision is an inadequate strategy that fails the safety principles of redundant checks of critical steps dependent on human behavior and ignores the potential impact of predictable human biases. Focusing just on 1 type of error, the predominant wrong-side surgeries, 8 patients in our 30-month experience had wrong-side errors corrected by time-out processes, 21 wrong-side errors occurred despite time-out processes that were described without any apparent inadequacies, with 12 of them resulting in complete wrong-side procedures.
In particular, 26 local anesthetics or nerve blocks were done with no mention of or explicitly before a formal time-out process. Another 15 wrong-side reports implicated incorrect positioning. In 3, the confusion resulted from turning the patient from supine to prone. Five reports described the wrong knee being put in a leg holder, with subsequent skin preparation, draping, and unremarkable formal time-out process, followed by an incision or complete procedure on the wrong leg. In the opinion of the authors, these 5 errors were examples of confirmation bias (the psychologic tendency to confirm an impression despite the facts) that over-rode the formal time-out process.36
Information about the site of secondary parts of a procedure (such as vein harvesting) was not always included. This problem might be rectified by adopting Makary’s recommendation of a full time-out briefing.37
Markings of the operative site were not always accurate. Again, among the reports of wrong-side events, 17 incorrect markings were corrected as a result of the preoperative reconciliation and verification process. Although 10 reports indicated wrong-side errors were caught as a result of correct markings, correct-side markings failed to prevent another 16 wrong-side surgeries, of which 6 were not recognized until after the procedure was over.
Also just looking at wrong-side events, patients and family were not totally reliable in identifying the correct side. Although they helped correct wrong-side errors according to at least 55 reports, another 13 patients and/or families indicated the incorrect side; wrong-side contact then occurred in 7 of those reports.
In the traditional preoperative reconciliation and verification process, an OR nurse reviews the operation as scheduled, the patient’s identity and verbal understanding, the consent and the information in the medical record, such as the surgeon’s notes and the results of definitive diagnostic tests. This step appeared effective in catching wrong-site errors, especially when the surgeon became involved in this preoperative reconciliation and verification phase. The reconciliation and verification were compromised by incorrect information and by the absence of surgeons’ office records. The information most commonly incorrect was the information given to the person receiving information for the upcoming OR schedule. This misinformation affects not only the schedule, but the room setup and equipment as well. In addition, some operating rooms batch patients by side to reduce wrong-side errors; scheduling errors may negate that effort.
Although labeling of specimens had no immediate impact on any patients, the implications described in the downstream confusion with the wrong patient undergoing removal of a normal organ, described above, sets up future opportunities for wrong-site surgery.
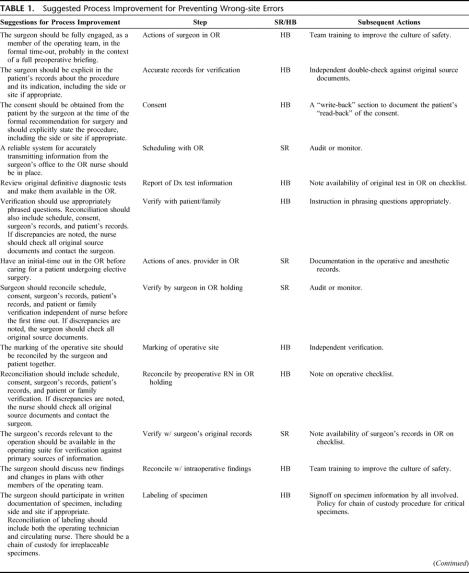
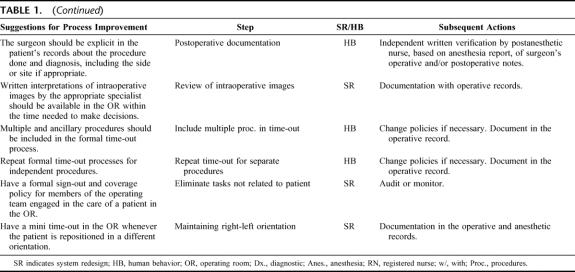
Considering the number of wrong-site surgery protocols published and used, the literature is largely silent concerning the effectiveness of surgical site verification interventions analyzed in a controlled observational design or a clinical trial.7 We do not wish to add to the problem of solutions based on logic, but not effectiveness. We also wish to adhere to the philosophy of the Institute for Healthcare Improvement to keep the process as simple as possible.10 The following suggested process improvements for preventing wrong-site surgery are made with the understanding that they should be monitored for effectiveness. These suggestions for improvement in the site verification process are hypothesized as ways to strengthen the system’s reliability by improving the system design and ensuring redundancy in steps dependent on human behavior (Table 1).38,39 They are prioritized according to how many reports they address. Each suggestion carries a follow-up action for implementation or monitoring.
TABLE 1. Suggested Process Improvement for Preventing Wrong-site Errors
TABLE 1. (Continued)
The suggested process improvements for preventing wrong-site surgery are based on the following conclusions from our analysis of contributing and recovery factors implicated in reports submitted from across a state over 2.5 years.
The accurate collection and transmission of information from the surgeon’s initial preoperative encounter with the patient is critical to preventing downstream errors, starting with the accuracy and completeness of the information conveyed when scheduling the procedure with the OR. The accuracy of the documents used in the preoperative reconciliation is essential to successful verification. These documents include the operative consent, the schedule, and the surgeon’s records of the patient’s history and physical examination, definitive diagnostic test results, plus an exact description of the proposed procedure and the side or site as appropriate. This information should be readily available at the time of preoperative reconciliation and verification. It should be fully reassessed independently by 2 providers whenever inconsistencies are identified.
Currently, the patient, family, and preoperative nurse provide the most protection against wrong-site surgery. The authors believe that more early involvement is needed by anesthesia providers and surgeons. In particular, we hypothesize that wrong-site surgery events would be reduced by the participation of the surgeon preoperatively in the reconciliation and verification process, involving the documents and the patient’s understanding, and by the participation of those providing anesthesia in a preliminary time-out in the OR before the patient is touched. Currently, many more errors are instigated providing local or regional anesthesia, albeit not all by anesthesia specialists, than detected by those providers.
The authors hypothesize that time-out failures are often due to wrong-site errors initiated by positioning the patient, providing the anesthesia, or preparing the operative site and perpetuated by confirmation bias; they may be decreased by a preliminary time-out in the OR before the patient is touched.
In general, wrong-site surgery does not “just happen” to surgeons and surgical facilities. It is a monitor of the accuracy and completeness of the information brought to the point of care, the quality of professional communication, and the degree of teamwork among the members of the operating team. The patient’s surgeon is key to all of these factors contributing to, and preventing, wrong-site surgery.
The opportunities for wrong-site surgery occur regularly, given high-risk patient situations and the realities of human behavior, such as confirmation bias. Neither the knowledge of the patient, marking the operative site, nor a formal time-out process just before incision are sufficient barriers to prevent wrong-site surgery. Site verification needs to start with the initial patient encounter with the surgeon, continue through the initial reconciliation and verification process during the preoperative nurse and patient encounter, occur at multiple critical points in the OR, and actively engage the members of the patient’s operating team, especially the surgeon and anesthesia provider.
ACKNOWLEDGMENTS
The authors thank Caprice Christian Greenberg, MD, MPH, Jesse Munn, BA, Stanton N. Smullens, MD, and Miriam Solomon, PhD, for their comments and suggestions.
Discussions
Dr. Julie Ann Freischlag (Baltimore, Maryland): Wrong-side surgery, no matter how it is defined, has multifactorial causes, and many variables, mainly human in the surgeon, patient, anesthesiologist, and nurse.
Our approach at Johns Hopkins has been to expand the time-out to what we call briefing, which utilizes a checklist in order to prompt a conversation prior to incision. Marking is done by a member of the OR surgical team in the pre-op area. The briefing is orchestrated in the OR room by the attending surgeon. A debriefing is also done at the end of the procedure and is recorded by the nurse, again a conversation about what issues went on with the case, instruments, and checking the specimen by the surgeon for proper labeling. We presented our briefing and debriefing last October at the College and have made a video to teach others.
So instead of your multiple times-out that you are requesting, what are your thoughts on using a meaningful conversation before and after an operation to create an environment of communication and feedback for all members of the surgical team?
What value have you gained from near misses? Is that information fed back to the hospital and the surgical team to learn from their mistakes?
Have you been successful in getting other health care deliverers such as emergency room physicians, interventional radiologists, and cardiologists, to do time-outs, briefings, and debriefings? We are just beginning that at Hopkins, and it has been a little difficult.
Lastly, do you think that surgeons are now accepting of the need for briefings and debriefings? It has been a 4-year journey at Hopkins, and I know everyone else has struggled, too, to get a buy-in to have such a conversation when someone might actually say it is the left leg, not the right. Why are some so resistant to this kind of formal process to enhance patient safety?
Dr. John R. Clarke (Philadelphia, Pennsylvania): First of all, I would like to say that in our manuscript we do talk about the Hopkins expanded time-out, so I think this is a benefit. But we do feel that there needs to be some collective bringing together of all the information and all the people, and that this should be done before the patient is touched, not at the last second before making the incision.
I would also like to emphasize that the debriefing at the end of the case gives you the opportunity to look at specimen management problems. Thirteen of our problems were mislabeling the specimen, and that sets you up for an error with the next case down the line, such as some other patients getting an operation for your patient’s pathology.
As far as feedback goes, we feed back to the institutions through the Patient Safety Reporting System Patient Safety Advisory, so that all the institutions benefit from the lessons learned. The near-miss information tells us where errors are caught and, therefore, where the protective mechanisms are strongest.
Regarding other venues, we noticed in particular that wrong-side events occur when someone is doing a procedure alone. We published suggestions in our Patient Safety Advisory that people should bring another provider in for a time-out process.
As far as resistance goes, we experienced a couple of cases where the physician was clearly uncooperative. I think this is only going to change when you do as Hopkins has done, change the culture.
Dr. Allen Livingstone (Miami, Florida): This is a remarkably intractable problem, including in the State of Florida where we have an extremely high awareness of potential malpractice situations and their financial consequences. In 2005 in Florida, there were 31 wrong-site operations, 5 wrong patient surgeries (the ultimate in wrong side!), and 86 instances where the wrong procedure was done. It is clear that current safeguards are insufficient.
We also have an extended time-out at Jackson Memorial Hospital, and a policy, just like airline pilots do, that anybody can stop the operation at any time. The nurses are even allowed to stop the patient from going into the operating room if they are uncertain which side is to be marked. In spite of this, there are still cases of wrong side surgery.
The impact on the patient and the malpractice consequences are obvious and very significant. But in many states including Florida, wrong-side surgery also has significant implications on one’s medical license. In Florida, all such instances are reported to the State as a Code 15 and the rule of res ipsa loquitur applies. In each case, the physician is fined a minimum of 10 to 20 thousand dollars, community service is mandated, and if the instance is egregious, the medical license is suspended or revoked. As a consequence, surgeons are very conscious of this problem, including in teaching institutions, but still episodes occur.
Just a final anecdote; in spite of our current policies, we recently had a case of wrong-side surgery. The patient identified the extremity, it was marked in the intake area by the surgeon while the patient was awake, it was checked in the operating room, and everybody agreed that it was the right thigh. The patient was then turned prone, and the operation proceeded on the wrong thigh. It is hard to believe that wrong-side surgery cannot be stopped. But it better be, because if we do not solve this problem, the public and legislators will.
Dr. John R. Clarke (Philadelphia, Pennsylvania): It is fortunate that nurses can stop the procedure if they are not satisfied. We had several reports in which the physician started to operate while the nurse was still doing the time-out. Some hospitals in Pennsylvania have solved that problem by having a policy of not allowing the surgeon to have a sharp instrument until the time-out is completed.
We have also seen some prone-supine problems as well. In 1 case, the anesthesiologist blocked the sciatic nerve, then rolled the patient back to block the femoral nerve but didn’t switch sides of the table. People do get confused by the positioning of the patient. Perhaps, people need to go through some formal mini-time-out when they change the position of the patient.
Dr. Michael M. Abecassis (Chicago, Illinois): I think these processes are all very important, including the time-out. Twenty years ago when I was a resident, I was on call 1 night and was called because a patient identified that the pneumonectomy had been done on the wrong side. And he was on a ventilator and subsequently required a lung transplant.
The reason that mistake happened, when it was analyzed, was that the x-rays, the images, had been done at an outside hospital. The surgeon had booked it as the wrong side. He had been consented as the wrong side. And if there had been a time-out, everybody would have been convinced that the wrong side was the right side.
So my question is, do you see a role for appending diagnostic testing and images to the process of evaluating whether you are operating on the right side or not?
Dr. John R. Clarke (Philadelphia, Pennsylvania): Absolutely. We have seen a number of instances similar to what you described, including 1 case where a patient had a thyroidectomy for somebody else’s cancer because it was dictated and transcribed under her name.
The problem of the imaging study or the pathology report being mislabeled is a problem of a similar nature to wrong-site surgery that occurs prior to the operating room in pathology or radiology. It obviously can lead to the problem of wrong-site surgery. I think people would be wise to verify diagnostics by looking at the images themselves.
Dr. Michael E. Zenilman (Brooklyn, New York): Just a quick comment and then a question. New York State already mandates an expand time-out process to include site verification when scheduling of a case for surgery, verification of relevant pathology and radiology reports as part of a checklist before surgery, and that the surgeon mark the site with their own initials—nobody else’s. For quality assurance purposes, we have encouraged incident reporting of any events that do not comply.
The question I have is regarding reporting of the near misses. I am very supportive of reporting and analyzing them, but what do we do about patient disclosure once we know about them.
Dr. John R. Clarke (Philadelphia, Pennsylvania): We operate under rules of strict confidentiality. There are no names of patients or providers allowed in the reports submitted to us. Our confidentiality is mandated by state law. So, we have no problem. What we do with our information is disseminate it to everybody. So everyone benefits.
If I could go back to your first comment, the V.A. requires 2 people to look at the original pathology or imaging study in order to confirm. Nevertheless, they experienced a case recently of someone removing the wrong testicle for cancer.
Dr. Hiram C. Polk, Jr. (Louisville, Kentucky): This report on surgical time-out is meant to be a report of a process. We have done a little with it. All of you can do better!
There are 2 points that have come to our attention recently that are really important. Number 1, the more often you have the patient awake adds another level of safety and is a huge improvement.
It would be smart if surgeons learn to dictate the surgical time-out into their preliminary op note “why the patient had the operation.” Use 8 or 10 words, describe the time-out process going on. This is really good work, like Dr. Grosfeld’s talk this morning. It is not happy news, but it is something we really need to do better.
Dr. John R. Clarke (Philadelphia, Pennsylvania): I agree wholeheartedly with your suggestion of putting the time-out in the notes. We certainly concur that the longer the patient is awake, or at least if you do this interaction when the patient is awake, the better. We have had more than 1 patient in the reports described as saying, “Do you have to shave the left leg in order to operate on the right leg?” or words to that effect.
Footnotes
Supported by a contract from the Pennsylvania Patient Safety Authority to the ECRI Institute.
Reprints: John R. Clarke, MD, Clinical Director of the Pennsylvania Patient Safety Reporting System, 5200 Butler Pike, Plymouth Meeting, PA 19462. E-mail: jclarke@ecri.org.
REFERENCES
- 1.National Quality Forum. Serious Reportable Events in Healthcare: A Consensus Report. Washington: National Quality Forum; 2002. [Google Scholar]
- 2.Fort Lauderdale Sun-Sentinel Broward Metro Edition. Preventing Surgical Mistakes: State Licensing Board Opts for a System of Checks Over an increase in Penalties. Fort Lauderdale: Sun-Sentinel; July 29, 2006.
- 3.Associated Press. Big payout in wrong knee surgery lawsuit. Choreographer awarded $450,000 from hospital, doctor. [MSNBC Web site]. January 21, 2005. Available at: www.msnbc.msn.com/id/6852479/. Accessed April 24, 2007.
- 4.Baldwin C. Jury awards $1.2 M in lawsuit. [Casper Star Tribune Web site]. May 13, 2005. Available at: www.casperstartribune.net/articles/2005/05/13/news/b30aab17c9f31d398725700000063b2f.txt. Accessed April 24, 2007.
- 5.Kwaan MR, Studdert DM, Zinner MJ, et al. Incidence, patterns, and prevention of wrong-site surgery. Arch Surg. 2006;141:353–357. [DOI] [PubMed] [Google Scholar]
- 6.Joint Commission. Sentinel event statistics. [Joint Commission Web site]. December 31, 2006. Available at: www.jointcommission.org/NR/Rdonlyres/74540565-400F-4992-863E-8F9E94EB56/0/SE_state_12_06.pdf. Accessed April 24, 2007.
- 7.Shojania KG, Duncan BW, McDonald KM, et al, eds. Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Subchapter 43. 2. Strategies to avoid wrong-site surgery. Evidence Report/Technology Assessment No. 43, AHRQ Publication No. 01-E058. Rockville, MD: Agency for Healthcare Research and Quality; 2001:498–503. [Google Scholar]
- 8.Minnesota Department of Health. Adverse health events in Minnesota: second annual public report. [Minnesota Department of Health Web site]. February 2006. Available at www.health.state.mn.us/patientsafety/ae/aereport0206.pdf. Accessed April 24, 2007.
- 9.Minnesota Department of Health. Adverse health events in Minnesota: third annual public report. [Minnesota Department of Health Web site]. January 2007. Available at www.health.state.mn.us/patientsafety/ae/aereport0107.pdf. Accessed April 24, 2007.
- 10.Dunn D. Surgical site verification: A through Z. J Perianesth Nurs. 2006;21:317–331. [DOI] [PubMed] [Google Scholar]
- 11.Page L. System marks new method of preventing wrong-site surgery. Mater Manag Health Care. 2006;15:55–56. [PubMed] [Google Scholar]
- 12.Canale ST. Wrong-site surgery: a preventable complication. Clin Orthop Relat Res. 2005;433:26–29. [PubMed] [Google Scholar]
- 13.American Academy of Orthopaedic Surgeons. Wrong site surgery. [American Academy of Orthopaedic Surgeons Web site]. 1998. Available at: www5.aaos.org/wrong/viewscrp.cfm. Accessed April 24, 2007.
- 14.Meinberg EG, Stern PJ. Incidence of wrong-site surgery among hand surgeons. J Bone Joint Surg Am. 2003;85:193–197. [DOI] [PubMed] [Google Scholar]
- 15.Wright PH, Burnaby BC. Committee on orthopaedic practice and economics (COPE) position paper on wrong sided surgery in orthopaedics: prepared for the Canadian Orthopaedic Association. [Canadian Orthopaedic Association Web site]. Available at: www.coa-aco.org/library_NEW/Wrong_Sided_Surgery.asp. Accessed April 24, 2007.
- 16.American Academy of Orthopaedic Surgeons. Advisory statement: wrong-site surgery. [American Academy of Orthopaedic Surgeons Web site]. October 2003. Available at: www.aaos.org/about/papers/advistmt/1015.asp. Accessed April 24, 2007.
- 17.North American Spine Society. Prevention of wrong-site surgery. Sign, mark and x-ray (SMaX). [North American Spine Society Web site]. 2001. Available at: www.spine.org/SMaX.cfm. Accessed April 24, 2007.
- 18.American Society of Ophthalmic Registered Nurses. Eliminating wrong-site surgery. A joint statement of the American Academy of Ophthalmology, the American Society of Ophthalmic Registered Nurses and the American Association of Eye and Ear Hospitals. [American Society of Ophthalmic Registered Nurses Web site]. 2001. Available at: webeye.ophth.uiowa.edu/asorn/Safety/SafetyBulletin1.htm. Accessed April 24, 2007.
- 19.Association of Perioperative Registered Nurses. AORN position statement on correct site surgery. [Association of Perioperative Registered Nurses Web site]. 2003. Available at: www.aorn.org/about/positions/correctsite.htm. Accessed April 24, 2007.
- 20.American College of Surgeons. Statement on ensuring correct patient, correct site, and correct procedure surgery. Bull Am Coll Surg. 2002;87:26. [PubMed] [Google Scholar]
- 21.Joint Commission. Lessons learned: wrong site surgery. Sentinel event alert. [Joint Commission Web site]. August 6, 1998. Available at: www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_6.htm. Accessed April 24, 2007. [PubMed]
- 22.Carney BL. Evolution of wrong site surgery prevention strategies. AORN J. 2006;83:1115–1118, 1121–1122. [DOI] [PubMed] [Google Scholar]
- 23.Joint Commission. Universal protocol for preventing wrong site, wrong procedure, wrong person surgery. [Joint Commission Web site]. Available at: www.jointcommission.org/NR/rdonlyres/E3C600EB-043B-4E86-B04E-CA4A89AD5433/0/universal_protocol.pdf. Accessed April 24, 2007.
- 24.National Quality Forum. National Quality Forum updates endorsement of safe practices for better healthcare. [National Quality Forum Web site]. 2006. Available at: www.qualityforum.org/pdf/news/prSafePractices10-15-06.pdf. Accessed April 24, 2007.
- 25.Department of Veterans Affairs. Veterans Health Administration. Ensuring correct surgery and invasive procedures. VHA directive 2004-028 [Department of Veterans Affairs Web site]. 2005. Available at: www.va.gov/NCPS/SafetyTopics/CorrectSurg/CorrectSurgDir.DOC. Accessed April 24, 2007.
- 26.Partnership for Health & Accountability in Georgia. PHA correct site surgery [Georgia Hospital Association Web site]. January 11, 2006. Available at: http://gha.org/pha/keyissues/correctsitesurgery/index.asp. Accessed April 24, 2007.
- 27.State of New York Department of Health. New York State surgical and invasive procedure protocol for hospitals, diagnostic and treatment centers, ambulatory surgical centers, individual practitioners. [New York State Department of Health Web site]. 2006. Available at: http://w2.health.state.ny.us/query.html?qt=INVASIVE+procedure+protocol&Submit=Search. Accessed April 24, 2007.
- 28.Edwards P. Promoting correct site surgery: a national approach. J Perioper Pract. 2006;16:80–86. [DOI] [PubMed] [Google Scholar]
- 29.National Patient Safety Agency. Patient safety alert 06. Correct site surgery [National Patient Safety Agency Web site]. 2005. Available at: www.npsa.nhs.uk/site/media/documents/883_CSS%20PSA%20FINAL.pdf. Accessed April 24, 2007.
- 30.North American Spine Society. Sign, mark and x-ray checklist for safety [North American Spine Society Web site]. 2001. Available at: www.spine.org/forms/smaxchecklist.pdf. Accessed April 24, 2007. Accessed April 24, 2007.
- 31.Wong DA. Spinal surgery and patient safety: a systems approach. J Am Acad Orthop Surg. 2006;14:226–232. [DOI] [PubMed] [Google Scholar]
- 32.Seiden SC, Barach P. Wrong-side/wrong-site, wrong-procedure, and wrong-patient adverse events: are they preventable? Arch Surg. 2006;141:931–939. [DOI] [PubMed] [Google Scholar]
- 33.Clarke JR. How a system for reporting medical errors can and cannot improve patient safety. Am Surg. 2006;72:1088–1091. [DOI] [PubMed] [Google Scholar]
- 34.State of New York Department of Health Office of Health Systems. Management division of primary and acute care services. New York patient occurrence reporting and tracking system report. [New York State Department of Health Web site]. 2004. Available at: www.health.state.ny.us/nysdoh/hospital/nyports/annual_report/2002–2004/docs/2002–2004_nyports_annual_report.pdf. Accessed April 24, 2007.
- 35.Medical Care Availability and reduction of error (Mcare) act. [Patient Safety Authority Web site]. 2002. Available at: www.psa.state.pa.us/psa/lib/psa/act_13/act_13.pdf. Accessed April 24, 2007.
- 36.Reason J. Safety in the operating theatre, Part 2: Human error and organisational failure. Qual Saf Health Care. 2005;14:56–60. [PMC free article] [PubMed] [Google Scholar]
- 37.Makary MA, Mukherjee A, Sexton JB, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg. 2007;204:236–243. [DOI] [PubMed] [Google Scholar]
- 38.Grout JR. Preventing medical errors by designing benign failures. Jt Comm J Qual Saf. 2003;29:354–362. [DOI] [PubMed] [Google Scholar]
- 39.Grout JR. Mistake proofing: changing designs to reduce error. Qual Saf Health Care. 2006;15(suppl 1):i44–i49. [DOI] [PMC free article] [PubMed] [Google Scholar]