Abstract
Objective:
Technological advances in vascular surgery have changed the field dramatically over the past 10 years. Herein, we evaluate the impact of endovascular procedures on general surgery training.
Methods:
National operative data from the Residency Review Committee for Surgery were examined from 1997 through 2006. Total major vascular operations, traditional open vascular operations and endovascular procedures were evaluated for mean number of cases per graduating chief general surgery resident (GSR) and vascular surgery fellow (VSF).
Results:
As endovascular surgical therapies became widespread, GSR vascular case volume decreased 34% over 10 years, but VSF total cases increased 78%. GSR experience in open vascular operations decreased significantly, as evidenced by a 52% decrease (P < 0.0001) in elective open AAA repair. VSFs have also seen significant decreases in open vascular procedures. Experience in endovascular procedures has increased for both general surgery and vascular residents, but the increase has been much larger in absolute number for VSFs.
Conclusions:
GSR experience in open vascular procedures has significantly decreased as technology has advanced within the field. Unlike VSFs, this loss has not been replaced by direct experience with endovascular training. These data demonstrate the impact technology can have on how we currently train general surgeons. New educational paradigms may be necessary in which either vascular surgery as an essential component is abandoned or training in catheter-based interventions becomes required.
General surgery resident experience in open vascular procedures has significantly decreased as endovascular advances have changed the field of vascular surgery. Unfortunately, residents have only made small strides in learning endovascular skills. If these trends continue, new training paradigms may be necessary to maintain quality general surgery residency education.
Vascular surgery has long been recognized as important in general surgery training. The Residency Review Committee (RRC) for Surgery has specific requirements for general surgery residents (GSR) to obtain adequate knowledge in and experience with vascular surgery.1 In addition to specific educational goals and objectives, the RRC requires that GSRs perform 44 cases as surgeon throughout their entire 5-year clinical residency in the “Defined Categories” of vascular surgery. Although the American Board of Surgery (ABS) does not require a certain minimum number of procedures within a content area, it does broadly require competency in the field of vascular surgery.2
More so than in most fields, technologic advances in vascular surgery have changed the specialty dramatically over the past 10 years. Since the Food and Drug Administration approval of the endostent in 1999 for the treatment of abdominal aortic aneurysm (AAA), there has been an increase in endovascular abdominal aortic aneurysm repair (EVAR) nationwide. According to Dillavou et al, from 2000 to 2003, the total number of elective AAA repairs, which included both open procedures and endovascular repairs, did not change significantly across the United States.3 The number of endovascular AAA repairs, however, did increase significantly, whereas the number of open AAA repairs declined sharply. The introduction of endovascular programs at teaching hospitals across the nation helped to effect this change, as the specialty became more endovascularly based.
Reports from a select group of leading academic surgical centers across the United States indicate that a change has occurred at least at the institutional level, whereby GSR experience in vascular surgery has diminished because of the increasing number of endovascular procedures being performed, mostly by vascular surgery fellows (VSFs).4–7 Individually, these institutional reports have addressed this topic from unique perspectives. For example, Sternbergh et al reported that over a 5-year period (1997–2001), elective open AAA repair experience decreased for GSRs but did not change significantly for VSFs at the Ochsner Clinic in New Orleans.5 Citing these same trends, the vascular surgery group at Baylor College of Medicine in Houston called for the evaluation of the residency system to improve upon the training paradigm for vascular fellowship and general surgery residency.6 In addition, directed allocation of the precious dwindling resource of open AAA repair to those who would ultimately perform the procedure, namely, vascular fellowship-trained surgeons, has even been suggested.7 In the only national study to date, Cronenwett examined the RRC database for GSRs and VSFs from 1994 to 2003.8 He drew conclusions that were similar to the previously mentioned institutional reports, and in addition, stated that GSRs were still far exceeding the minimum number of vascular cases required by the RRC. He went on further to describe the need for more vascular surgery fellowship positions to meet the demand for increased interventional volume and to compete with other specialties.
The purpose of this study is to examine the effects of changing rates of open and endovascular procedures on GSR vascular experience at the national level over the past 10 years (1997–2006). Our goal is not only to identify the areas in which GSR education in vascular surgery may be feeling the effects of technologic advances, but to recommend changes that can be made to ensure that future generations of general surgeons will continue to receive quality training in vascular surgery.
METHODS
To test the hypothesis that the increasing rate of endovascular procedures is having a negative impact on GSR experience with vascular surgery, operative log data for GSRs and VSFs were reviewed. The RRC for Surgery compiles these data for all GSRs and VSFs in the United States. These reports are distributed annually to general and vascular surgery program directors and are also made available on the internet at www.acgme.org. “National Resident Report C” or “Resident Statistic Summary” was reviewed for cases logged in vascular surgery by GSRs and for all cases logged by VSFs for the academic years 1996–1997 through 2005–2006.9
The total number of graduating chief GSRs or VSFs completing their programs per year was evaluated. The mean number of cases logged by GSRs as “Total Surgeon” and by VSFs as “Surgeon Fellow” (“Total Surgeon” before 2000–2001) throughout their entire training program was examined in several categories. First, overall vascular experience was determined by examining total vascular procedures for GSRs and VSFs. Second, open vascular operations were evaluated. The major areas of aneurysms, cerebrovascular, and peripheral-obstructive were examined to evaluate trends in these broader categories. Then, individual procedures: open, elective infra-renal AAA repair, carotid endarterectomy (CEA), and lower-extremity bypass were examined to evaluate trends in specific operations. Third, therapeutic endovascular procedures were evaluated using the same approach. The major area of therapeutic endovascular was examined for overall trend, and the individual procedures: EVAR and balloon angioplasty were examined for specific changes.
Only cases for which the GSR or VSF was the operating surgeon were considered. For all graduating chief GSRs the mean number of cases reported as total surgeon, which includes surgeon chief and surgeon junior, was evaluated. For VSFs, cases reported for total surgeon (1997–2000) and cases logged as surgeon fellow (2001–2006) were evaluated. Cases logged as teaching assistant and first assistant, while valuable educational opportunities were not included in the data set because they do not count for credit towards requirements for program completion. Only primary procedures were included in the data set, as secondary procedures are only tracked for VSFs and not for GSRs. During the time period from which data were collected, the RRC modified the coding procedures for many of the vascular areas and procedures included in this study. Changes in the coding system were as follows.
Before 2001 VSFs used the codes surgeon chief or surgeon junior for cases in which they were the operating surgeon. After 2001 the RRC changed this to surgeon fellow.
In 2001 the RRC added the major area endovascular therapeutic to the VSF case log code, as well as the specific procedure code for EVAR and balloon angioplasty.
In 2002 endovascular was added to the major areas of vascular surgery for GSRs, and EVAR and balloon angioplasty became specific case log options.
Statistical Analysis
Analysis of variance, where case volume was the outcome and year was the main effect, were performed using SAS Release 9.1 software. Data are reported as mean values for each year. Given missing data on standard deviations for 1 or more years, we followed a conservative approach of imputing the highest nonmissing standard deviation in each series to all years where the standard deviation was missing. This approach was followed for only 1 analysis for VSFs (lower extremity bypass) but for 2 analyses for GSRs (total vascular procedures and lower extremity bypass). Statistical significance was accepted at the P < 0.05 level.
RESULTS
Total Major Vascular Case Volume Has Increased for VSFs and Decreased for GSRs
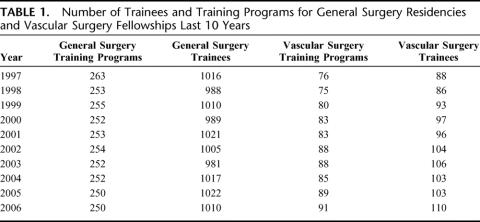
Vascular surgery operative experience can be evaluated by overall total number of major vascular cases logged by GSRs and VSFs; trends depicted in Figure 1. Chief GSRs graduating in 2006 averaged significantly fewer major vascular cases logged, 130 compared with 197 cases logged per chief resident who graduated in 1997 (34% decrease, P < 0.0001). This downward trend accelerated dramatically between the 2001 and the 2002 academic years from 186 to 141. VSFs, however, have shown increasing mean numbers of total major vascular case experience. VSFs finishing programs in 1997 logged an average of 290 major vascular cases per year, while this number increased to 516 per fellow finishing programs in the 2006 academic year (78% increase, P < 0.0001).
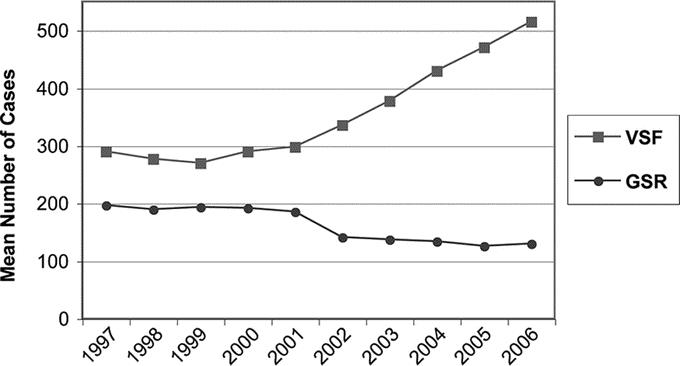
FIGURE 1. Mean numbers of cases logged for vascular surgery fellows and general surgery residents for total major vascular procedures over a 10-year period. Trends were significant at P < 0.0001. VSF, vascular surgery fellow; GSR, general surgery resident.
Both VSFs and GSRs Have Experienced Decreases in Open Vascular Operations
Major Open Areas
Operative case log data for vascular surgery is reported by the RRC according to major vascular area, such as peripheral-obstructive, cerebrovascular, and aneurysms. Evaluation of these data showed decreasing operative experience for VSFs and for GSRs (Figs. 2 and 3). Over the past 10 years, VSFs experienced decreasing case volume in peripheral-obstructive from 75 to 70 (6%, P = not significant), in cerebrovascular from 61 to 50 (19%, P < 0.0001), and in aneurysms from 41 to 33 (19%, P < 0.0001). Over the same time period GSRs showed significant decreases in the major areas of peripheral- obstructive from 29 to 23 (22%, P < 0.0001), cerebrovascular from 23 to 17 (23%, P < 0.0001), and aneurysms from 14 to 7 (47%, P < 0.0001).
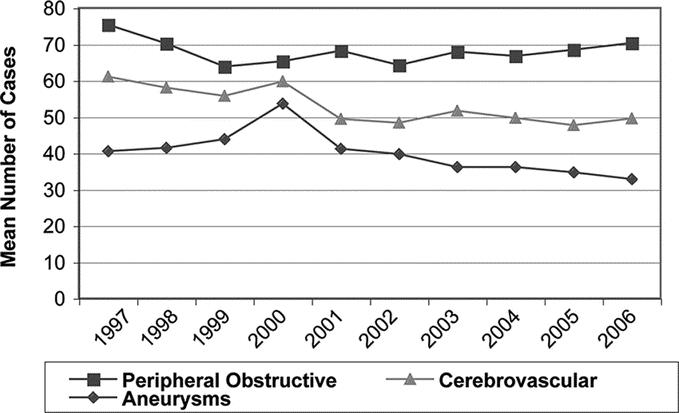
FIGURE 2. Mean numbers of cases over the last 10 years by vascular surgery fellows for open procedures in selected major areas of vascular surgery: peripheral obstructive, cerebrovascular, and aneurysms. Trends were significant at P < 0.0001, except for peripheral obstructive, which was not significant.
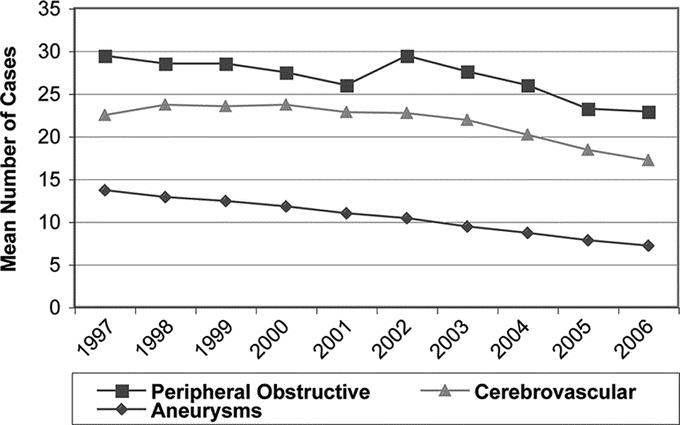
FIGURE 3. Mean numbers of cases over the last 10 years by general surgery residents in open procedures in selected major areas of vascular surgery: peripheral obstructive, cerebrovascular, and aneurysms. Trends were significant at P < 0.0001.
Specific Open Procedures
Specific index vascular surgery procedures, which were once used to judge the adequacy of vascular surgery training, were examined. VSFs who completed their training over the last 10 years, saw significant decreases in these index procedures (Fig. 4): CEA decreased from 56 to 43 (23%, P < 0.0001), lower-extremity bypass from 58 to 36 (37%, P < 0.0001), and open, elective infra-renal AAA repair from 22 to 15 (31%, P < 0.0001). Graduating chief GSRs have also shown significant decreases in all 3 of these index procedures (Fig. 5). Over the past 10 years, GSRs experienced decreases in CEA from 22 to 16 (26%, P < 0.0001), in lower-extremity bypass from 23 to 13 (45%, P < 0.0001), and in open, elective infra-renal AAA repair from 8 to 4 (52%, P < 0.0001).
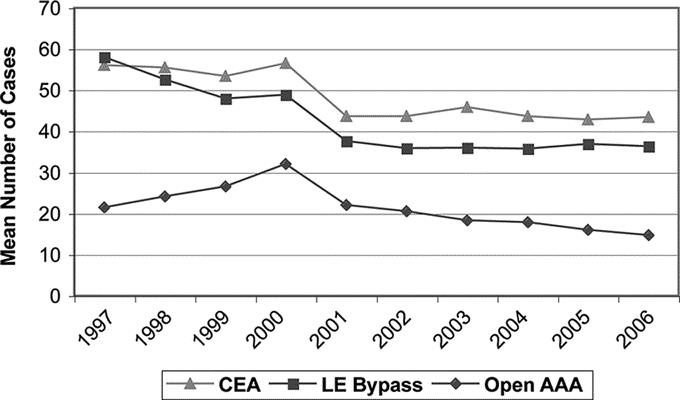
FIGURE 4. Mean numbers of cases reported by vascular surgery fellows over a 10-year period for specific open vascular cases. CEA, carotid endarterectomy; LE Bypass, lower extremity bypass; Open AAA, open elective infrarenal AAA repair. All trends were significant at P < 0.0001.
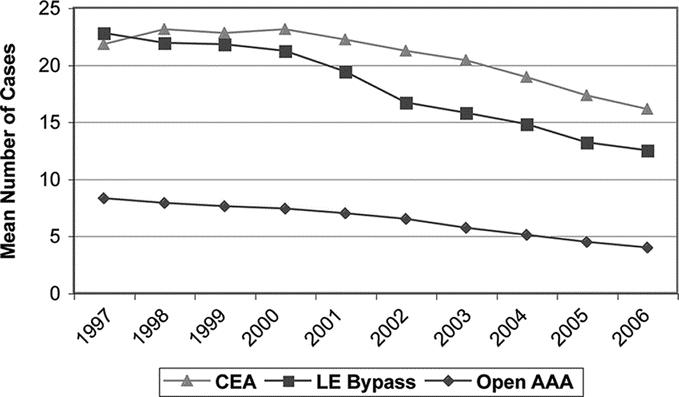
FIGURE 5. Mean numbers of cases reported by graduating chief general surgery residents over a 10-year period for specific open vascular cases. CEA, carotid endarterectomy; LE Bypass, lower extremity bypass; Open AAA, open elective infrarenal AAA repair. All trends were significant at P < 0.0001.
Both VSFs and GSRs Have Experienced Increases in Endovascular Cases
Major Endovascular Therapeutic Procedures
VSFs have experienced significant increases in therapeutic endovascular procedures. Since 2001, VSFs have seen a 3-fold increase in their mean number of therapeutic endovascular cases from 42 to 150 (260%, P < 0.0001). Endovascular experience also increased for GSRs: mean numbers of endovascular cases logged doubled from 5 in 2002 to 10 in 2006 (100%, P < 0.0001). The data are shown in Figure 6. Only therapeutic endovascular procedures were included in this analysis as GSRs do not have the option to code for diagnostic procedures, while VSFs do.
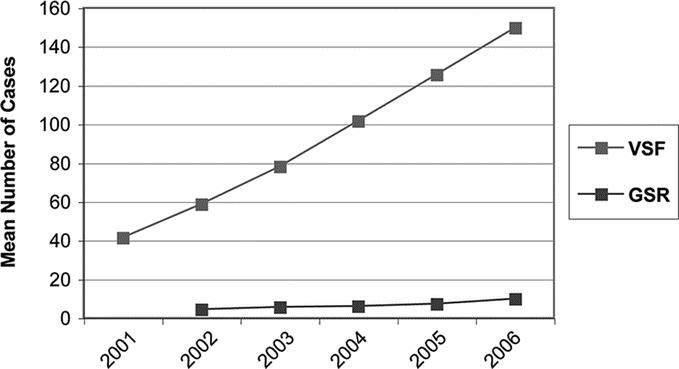
FIGURE 6. Mean numbers of cases by vascular surgery fellows and general surgery residents in the major area of endovascular procedures. All trends were significant at P < 0.0001. VSF, vascular surgery fellows; GSR, general surgery resident. Endovascular cases were not recorded for GSRs until the 2002 academic year.
Specific Endovascular Procedures
VSFs, not only saw a significant increase in EVAR in relative terms but also performed nearly 3 times as many EVARs in absolute terms, as the mean number of cases logged per fellow increased from 17 in 2001 to 45 in 2006 (163%, P < 0.0001). GSRs have shown increasing numbers of mean EVARs logged per graduating chief from 1 in 2002 to 2 in 2006 (100%, P < 0.0001). These are both significant increases, but the absolute increase in volume is much larger for the VSFs (Figs. 7 and 8). VSFs saw a significant increase in balloon angioplasty cases from 11 to 50 per fellow over 6 years (350%, P < 0.0001), and GSRs also had a significant increase in balloon angioplasties from 1 to 2 over a 5-year period (100%, P < 0.0001). Again, the increase in balloon angioplasty cases logged is much larger for VSFs when described in absolute number.
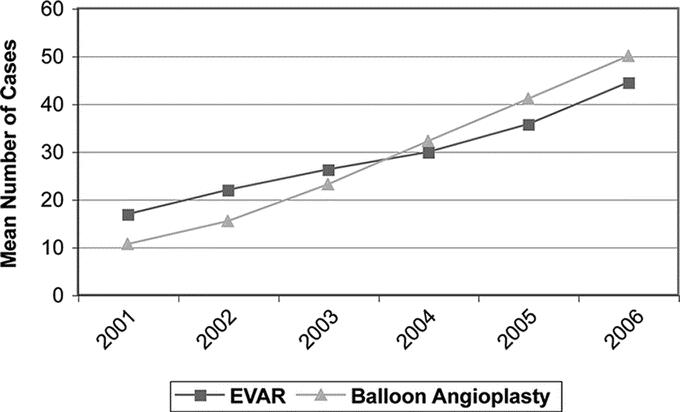
FIGURE 7. Mean numbers of cases by vascular surgery fellows in specific endovascular cases over the past 6 years: EVAR and balloon angioplasty. Trends were significant at P < 0.0001. EVAR, endovascular AAA repair. Note that the RRC began tracking endovascular cases for VSFs after 2000.
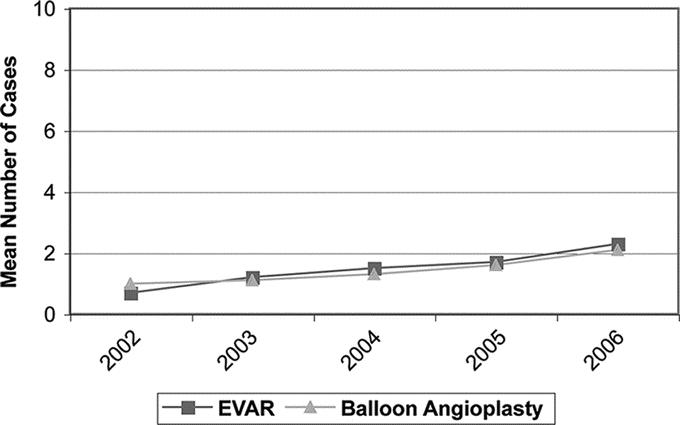
FIGURE 8. Mean numbers of cases by graduating chief general surgery residents in specific endovascular cases over the past 5 years: EVAR and balloon angioplasty. Trends were significant at P < 0.0001. EVAR, endovascular AAA repair. Note that the RRC began tracking endovascular cases for GSRs after 2001.
The Number of Vascular Surgery Trainees and Training Programs Has Increased
From the academic year 1997 through 2006 the number of general surgery residency programs decreased from 263 to 250 nationwide. The total number of graduating chief GSRs only declined slightly from 1016 in 1997 to 1010 in 2006. Vascular surgery training programs showed the opposite trend, however, with increasing number of programs and fellows trained. The total number of vascular surgery training programs increased from 76 in 1997 to 91 in 2006. These programs also showed an increase in the number of VSFs that graduated from 88 in 1997 to 110 in 2006, an increase of 25% (Table 1).
TABLE 1. Number of Trainees and Training Programs for General Surgery Residencies and Vascular Surgery Fellowships Last 10 Years
DISCUSSION
Our review of national operative log data in vascular surgery for GSRs for the past 10 years demonstrates decreases in overall vascular experience and open vascular procedures, such as open AAA repair, CEA, and lower extremity bypass. For GSRs this decrease in vascular case volume is not being reciprocated by an absolute increase in endovascular procedures. Thus, the shift from traditional open operations to endovascular procedures is having a significant impact on the education of GSRs in vascular surgery as depicted by case volume analysis. VSFs, however, are enjoying the benefits of increases in overall vascular experience, endovascular case volume, and fellowship positions available. Unfortunately, VSFs are also feeling the effect of decreases in open vascular procedures on their training experience.
Competency in any area of general surgery is more than can be measured simply by the tracking of operative cases. Technical skills, the ability to collect and process information and make diagnoses, and managing patients as well as complications are all essential in evaluating competency within any or all of the content areas. Current GSRs are evaluated in the Accreditation Council for Graduate Medical Education (ACGME) Competencies throughout their residencies.1 The tracking of cases and the evaluation of operative skills, however, are traditionally used in determining competency. In fact, the RRC requires that GSRs each have a minimum of 44 cases as surgeon in the “Defined Categories” of vascular surgery over their 5-year clinical residency to fulfill their requirements for graduation. GSRs, who finished in 2006, have on average 100 cases in the “Defined Categories” of vascular surgery and as such still have sufficient case volume to exceed the minimum vascular requirements for graduation. Significant decreases in open procedures such as open AAA, however, may leave them without proficiency in critical operative vascular techniques. Although the RRC does not require minimum numbers of specific operative procedures, like open AAA repair, there is evidence for the importance of case volume and training in outcomes for specific vascular surgical procedures, such as AAA repair and CEA.10 The current field of GSRs are graduating training programs with far less experience in open vascular surgery, a small increase in volume of endovascular procedures, and likely a diminished overall vascular surgery education raising questions as to their competency level in vascular surgery.
Current GSRs have significantly fewer opportunities to learn and reinforce the operative skills of open vascular procedures than their predecessors. Although, endovascular surgery is replacing many of the traditional open vascular procedures, GSRs have not shown a marked movement towards performing these endovascular procedures and learning the new skill sets required. In fact GSRs only show increases in mean number of EVAR and balloon angioplasty from 1 to 2 over the last 5 to 6 years, accounting for very little endovascular experience. As the field of vascular surgery becomes more endovascular, GSRs will not be able to receive quality training in vascular surgery if these trends continue. It is in the face of a diminished training experience for GSRs in both open vascular and endovascular procedures that the general surgery educational paradigm needs to be critically evaluated. One possible choice is to eliminate vascular surgery as an essential component of general surgery training.
Although VSFs show significant increases in overall vascular case volume as well as endovascular experience, they are also experiencing significant decreases in open vascular operative training. Increasingly, open interventions are becoming more complex in nature. Thus, vascular training programs are facing the challenges of adequately training fellows in open techniques while continuing to build endovascular skills. According to Brevetti et al, those who specialize in vascular surgery will need the benefit of training in open procedures, especially open AAA repair.7 By eliminating vascular surgery from the core of general surgery training, the precious resource of open vascular operations could be allocated to vascular fellows. In addition, the ABS is offering a Primary Certification in Vascular Surgery that does not require prior general surgery certification.2 Trends like these, that are intended to ensure adequately trained vascular fellows may serve ultimately to separate vascular surgery from general surgery altogether and cause further decreases in GSR exposure to vascular surgery.
The other choice is to maintain vascular surgery as a core of general surgery training. The ABS states that vascular surgery is an “essential component” of general surgery.2 The RRC has minimum requirements for GSRs to attain operative experience in the “defined categories” of vascular surgery.1 While on a vascular surgery rotation, GSRs, more so than on any other surgical service, learn valuable operative techniques of proximal and distal control of blood vessels, creation of vascular anastamoses, and working around major blood vessels. These surgical skills can carry over to other fields of general surgery and serve the surgeon for many years in practice. In addition, GSRs gain experience in managing patients with vascular diseases. To maintain the goal of training GSRs who are competent in the field of vascular surgery not only must the technical skills learned from open procedures be preserved, but also the new skill set of endovascular techniques must be embraced. GSRs need to be trained in the state-of-the-art of vascular surgery, which is largely becoming endovascular procedures.
The application of some simple and innovative methods may help to maintain the quality of resident education. First, the operating room is still the best classroom. Increasing residents’ exposure to the limited source of traditional open vascular procedures must be a priority. Encouraging GSRs to “double-scrub” may be a way to help accomplish this end. This has traditionally occurred in the setting of a senior resident or fellow acting as a “teaching assistant” and taking a junior resident through a case. Because only 1 resident or fellow can claim responsibility as “surgeon” for the case, tracking of the true educational experience by roles can be difficult. Second, RRC recognition of secondary procedures, which are currently not tracked for GSRs, would serve to increase the experience for residents from 1 operative case. The tracking of secondary procedures for VSFs is well established since 2000 after the emergence of multiple component endovascular procedures. Next, new technologies are already being employed for GSR education. GSRs can learn and employ endovascular skill sets, through new teaching techniques such as surgical simulation.11 Model patients and scenarios, computer-based operative simulation, and animal operative labs are all valuable training experiences in vascular training as well other areas of general surgery. Fourth, endovascular procedures have valuable skill sets, and the participation of GSRs must be encouraged. Finally, in the face of technologic advances within surgical fields, the RRC must be vigilant in monitoring resident operative volume trends to identify deficiencies where interventions may be needed to preserve the quality of training.
In conclusion, the technologic advances in endovascular procedures, which have dramatically improved our care of the vascular patient, are also changing the educational environment for general surgeons. GSRs today have significant decreases in open vascular operative experience without any substantial increase in endovascular training. In the face of diminished vascular experience for GSRs, changes in the surgical education paradigm might be necessary to ensure adequate vascular training. An important part of this change, if vascular surgery is to remain under the umbrella of general surgery, is to emphasize modern (ie, endovascular) treatment strategies, and not solely open procedures. In addition, continued vigilance in monitoring these changes is imperative to maintain quality in GSR education.
Discussions
Dr. K. Craig Kent (New York, New York): If one sums the data the only real conclusion that one can make is that the specialty of vascular surgery has changed. It is just different than it was a few years ago. The percutaneous first data that my group presented yesterday and Ron Fairman's data on carotid stenting are indicative of the fact that vascular surgery is changing and that we are heading in a different direction.
The consequence of this, of course, is that traditional open vascular surgery cases are becoming an endangered species, a rare commodity. And if we think this is a problem now, fast forward 5 years. For those of us who have expertise in catheter- intervention, there are no secrets about what the future will hold. So the question at hand appears to be, what to do with these scarce cases? Should we use them to train general surgical residents or should we use them to train vascular fellows?
The answer, at least to me, seems relatively straightforward. If there are enough to go around and this may be the case in a number of programs at least today then let's train everyone. If there are not enough cases to go around, and this will increasingly be the issue as endovascular surgery becomes more prominent in our specialty, we need to concentrate these resources in the hands of surgeons who will become the experts, ie, our vascular fellows.
These thoughts lead to a number of different questions.
First, do the authors believe that a finishing general surgical resident in current times, with no experience with endovascular techniques, should practice vascular surgery in the community? If the answer is yes, how will such an individual, if they do not offer endovascular techniques, compete with cardiologists or other specialists who do provide these minimally invasive approaches? As many of you know, even vascular surgeons that are catheter trained are struggling to maintain their market share.
I found the concept of double scrubbing interesting. There clearly still is benefit to general surgical residents being involved in open vascular procedures. These residents can learn exposure, arterial control, and suturing techniques. Can you think of other mechanisms that would allow residents and fellows to simultaneously benefit from the limited number of open cases that are available?
And the last question, and perhaps the most provocative is, what do you think about general surgical residents learning endovascular skills? I am a proponent of this. When residents rotate on my service, I want them to behave like vascular surgeons. And catheter intervention is what we do. But how do we convince our general surgical residents of the added value? Would it not be worthwhile as an incentive for the RRC to establish minimum requirements for general surgical residents in catheter intervention?
New technology is wonderful for our patients, but it brings up many issues regarding training, as the authors so eloquently highlighted. I appreciate the group at Jefferson being so thoughtful as to bring these to our attention.
Dr. Paul D. Dimuzio (Philadelphia, Pennsylvania): Thank you, Dr. Kent, for you comments and insight. Your group has certainly been instrumental in bringing out many of these changes in our field.
Should the general surgery resident of today go out and practice vascular surgery? If you look at the data specifically, I think you have to conclude that for carotid endarterectomy, open aneurysm repair, and peripheral bypass, the answer is no. The average graduating general surgery resident does not have the experience to practice vascular surgery. However, I do want to emphasize that the data that we put forth represents the mean numbers of cases, and that there are programs that are providing general surgery residents plenty of open and endovascular experience. With that in mind, if an interested general surgery resident at a high-volume program wants to go into practice and perform vascular procedures, I believe this still may be reasonable. For the average resident, I believe we should emphasize competency in the state-of-the-art of vascular surgery as it is today, and not hold on to the past. The state of the art right now is endovascular surgery.
The genesis of this investigation was my observation that as more and more of my cases were being performed by endovascular means, I was seeing fewer and fewer general surgery residents with me in the operating room. This was worrisome to me. Therefore, there was no stimulus for our general surgery residents to read about vascular surgery patients. Even worse, given that many of the patients were discharged the same or the next day after surgery, the residents had no clue as to what vascular surgery disease was about.
So, how can we stimulate their interest? We mentioned patient simulators, as you have alluded to and pioneered. Additionally, we need to be creative. For example, in my basic science laboratory, I use a large animal model. I have IACUC approval for the residents to come in after the animal is sacrificed, divide the aorta, and suture it back together.
Finally, I agree that it would be helpful for the RRC to provide a stimulus for general surgery resident to forge ahead and learn these procedures. For example, making balloon angioplasty and stent procedures count as defined category procedures. This small step would be very valuable in enticing residents to learn modern day vascular surgery.
Dr. Marc K. Wallack (New York, New York): I think Dr. Kent is on the money as far as the issue of the RRC. And there are now 3 vascular surgeons on the RRC beginning to look at the issue. Linda Riley and Pat Claggett would be the individuals that you could lobby to make sure general surgery residents are allowed to count these kinds of patients and give them more incentive to get involved.
However, what I would also like to make sure is that this august body understands that general surgery is being raided, and every year we perform fewer and fewer cases. The Advisory Council of General Surgery understands that right now, and Dr. Valentine, who is essentially president of the Association of Program Directors of Surgery, gave his keynote address on that topic.
Jefferson has a great surgical training program—and I want to quote your last comment here—which “underscores the need to preserve general surgery residencies,” because all of us are general surgeons, and the Early Specialization Program (ESP), the zero and 5 paradigms should only be for a few, not for all. How are we going to continue to train general surgeons, and how are we going to outline what a general surgery residency is if we continue to allow this invasion from within?
Dr. Paul J. Dimuzio (Philadelphia, Pennsylvania): I believe that with any part of general surgery, if you want to place a premium on what is important, the leaders of general surgery need to emphasis and keep pace with state-of-the-art practice. The state-of-the-art in vascular surgery is no longer open repair; it is endovascular repair. Therefore, if we wish to keep vascular surgery a significant part of general surgery, we need to emphasize endovascular procedures. We cannot say to the general surgery resident “Okay, open vascular surgery is disappearing, so you don't need to scrub on my stent-graft case.” On the contrary, we need to say, “This is how we fix an AAA in 2007. I hope you read the films.”
And I think that will have another effect. If the general surgery residents are going to start to see an emphasis on endovascular, they will learn modern care. So even though the majority of them will not practice endovascular surgery, they will be able to sit down with their patient and know in a very professional sense what is right for the person's care.
So we need to emphasize to the general surgery training community that residents need to be trained in state-of-the-art care. There should be much less emphasis on the open surgical cases. Leave these for the fellows who are actually going to be caring for your and my aneurysm in 20 to 30 years.
Dr. Richard H. Bell, Jr. (Philadelphia, Pennsylvania): Education experts would tell us that if we are thinking about modifying your curriculum as you propose that we modify the general surgery curriculum, that you should do a “needs” assessment. In other words, you should try to decide what the finishing general surgery resident needs to know about vascular surgery and not just sort of redefine or modify the curriculum in a vacuum. And I think I have some data that might be instructive in this regard.
A couple of years ago, I reviewed the reported experience of general surgeons taking the re-certifying exam. I think they must send in a 1-year case list before they re-certify. And at that time, people with no Boards other than the basic Board in surgery, who I guess we could call general surgeons, were reporting an average of about 50 vascular cases per year, of which about 30 were vascular access. And if you took away amputations and portal hypertension operations, you found that they were doing fewer than 10 what we would call traditional or high-end vascular procedures.
I guess 1 comment that I would make is that that time frame 1995 to 2001 preceded the widespread use of endovascular surgery. And so, I think that some of the changes you are describing may not be due to endovascular surgery, but to the maturation of vascular surgery as a specialty of surgery.
The second comment I would make is that I looked at the re-certifying experience of the 2005 re-certifiers who were out 10, 20, or 30 years. And again, about 10% of their practice is vascular, about 50 cases a year, still 30 cases are vascular access and fewer than 10 cases are carotids, lower extremity bypass, aorta and so forth. They reported an average of 2 endovascular procedures.
I would suggest that maybe an interesting thing for us to do, if someone in the vascular community would like to work with us on this, is to take a closer look at that. That is, do we have a lot of general surgeons performing 1 carotid a year and 1 or 2 endovascular procedures a year? And is that good? Or, do we have a few general surgeons doing a lot of vascular procedures and a great many of them doing none, which I suspect is the case. In which case, then I think you have to ask yourself, what is the point of including endovascular techniques in general surgery residency if 90% of the graduates will never do that?
I think that the conversation thus far today is interesting but is limited and needs to be considered in the larger context of what the public needs from its surgeons and what role general surgery plays in meeting that need.
Dr. Paul J. Dimuzio (Philadelphia, Pennsylvania): So you pose the question, “What is the point?” That is a great question. Why should residents learn all these endovascular procedures if they will not do it anyway?
One could argue that if we are going to train and keep vascular surgery as part of general surgery, residents need to understand vascular disease and participate actively in its treatment. And even though they may not necessarily practice vascular surgery, they will still encounter their own patients or those referred to them with vascular disease. As such, it is very reasonable to expect them to understand modern day treatment of these problems, even if they will subsequently refer them to a vascular specialist.
You speak about the practicality, or perhaps impracticality, of this approach. As you know, case volume in training and in practice typically translates into good clinical outcome. If the leaders of general surgery no longer feel vascular surgery is an important part of general surgery, training paradigms should change.
Dr. Gregorio A. Sicard (St. Louis, Missouri): As a vascular general surgeon, and I still practice a little general surgery, and head of a vascular program, I would like to point out that you go back 10 years in your numbers assessment. During that period, there have been a significant amount of changes in the categories assigned that the resident fills out to apply for their Boards. And let me give you an example.
Carotid stenting was not in the form for vascular fellowships as residents completed their fellowships to apply for their Boards in vascular surgery as early as 12 months ago. So number 1, are you comparing apples to apples throughout that period?
And number 2, was the number of months that the residents rotated at senior levels the same throughout that period? Obviously interns and second-year residents will not be doing aneurysms, open or endovascular, or carotid procedures.
What happens in a lot of programs, as they establish fellowships, which you showed very nicely, is that senior residents or the resident complement that rotates through the vascular program, decreases. Therefore, what you may be seeing is just that the time they are actually spending in vascular surgery has shrunk, and therefore, that may explain the decrease in numbers.
Dr. Paul J. Dimuzio (Philadelphia, Pennsylvania): Your group was one of the first to recognize this in 2001 in terms of the changes with aneurysms.
Regarding your first question, as far as the number of months, that is something quite frankly we did not think of tracking. We looked solely at Schedule C in terms of the number of cases. So that is something that we can go back and look at to see if this really is a mean effect.
As far as the changing categories, we were very cognizant of trying to compare apples to apples. As you probably know, vascular surgery fellows can record and review secondary procedures. If they do a femoral- popliteal bypass plus an iliac balloon angioplasty at the same time, the fellow records and tracks both cases. That is not even being done by the RRC at this time for general surgery residents. And perhaps allowing this will encourage residents to scrub on these types of cases. We were very careful in comparing apples to apples. That is a very good point.
Footnotes
Reprints will not be available from the corresponding author.
Correspondence: Paul J. DiMuzio, MD, Department of Surgery, Thomas Jefferson University, 111 South 11th Street, Suite 6350 Gibbon Bldg., Philadelphia, PA 19107. E-mail: paul.dimuzio@jefferson.edu.
REFERENCES
- 1.Accreditation Council for Graduate Medical Education, Residency Review Committee for Surgery. Program requirements for residency education in surgery. November, 2005. Available at: www.acgme.org.
- 2.The American Board of Surgery. Booklet of Information-Surgery 2006–2007. Available at: www.absurgery.org.
- 3.Dillavou ED, Muluk SC, Makaroun MS. Improving aneurysm-related outcomes: nationwide benefits of endovascular repair. J Vasc Surg. 2006;43:446–452. [DOI] [PubMed] [Google Scholar]
- 4.Choi ET, Wyble CW, Rubin BG, et al. Evolution of vascular fellowship training in the new era of endovascular techniques. J Vasc Surg. 2001;33:S106–S110. [DOI] [PubMed] [Google Scholar]
- 5.Sternbergh WC, York JW, Conners MS, et al. Trends in aortic aneurysm surgical training for general and vascular surgery fellows in the era of endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2002;36:685–689. [DOI] [PubMed] [Google Scholar]
- 6.Lin PH, Bush RL, Milas M, et al. Impact of an endovascular program on the operative experience of abdominal aortic aneurysm in vascular fellowship and general surgery residency. Am J Surg. 2003;186:189–193. [DOI] [PubMed] [Google Scholar]
- 7.Brevetti LS, Nackman GB, Shindelman LE, et al. Influence of endovascular training on fellowship and general surgical training. J Surg Res. 2003;115:100–105. [DOI] [PubMed] [Google Scholar]
- 8.Cronenwett JL. Vascular surgery training in the United States, 1994 to 2003. J Vasc Surg. 2004;40:660–669. [DOI] [PubMed] [Google Scholar]
- 9.Data Collections System. National Resident Report C or Resident Statistic Summary. [database online] Chicago, IL. Accreditation Council for Graduate Medical Education; 2007. Updated February 21, 2007.
- 10.Pearce WH, Parker MA, Feinglass J, et al. The importance of surgeon volume and training in outcomes for vascular surgical procedures. J Vasc Surg. 1999;29:768–776. [DOI] [PubMed] [Google Scholar]
- 11.Chaer RA, DeRubertis BG, Lin SG, et al. Simulation improves resident performance in catheter-based intervention. Ann Surg. 2006;244:343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]