Abstract
In early-onset myasthenia gravis, the thymus contains lymph node-type infiltrates with frequent acetylcholine receptor (AChR)-specific germinal centers. Our recent evidence/two-step hypothesis implicates hyperplastic medullary thymic epithelial cells (expressing isolated AChR subunits) in provoking infiltration and thymic myoid cells (with intact AChR) in germinal center formation. To test this, we screened for complement attack in a wide range of typical generalized myasthenia patients. Regardless of the exact serology, thymi with sizeable infiltrates unexpectedly showed patchy up-regulation of both C5a receptor and terminal complement regulator CD59 on hyperplastic epithelial cells. These latter also showed deposits of activated C3b complement component, which appeared even heavier on infiltrating B cells, macrophages, and especially follicular dendritic cells. Myoid cells appeared particularly vulnerable to complement; few expressed the early complement regulators CD55, CD46, or CR1, and none were detectably CD59+. Indeed, when exposed to infiltrates, and especially to germinal centers, myoid cells frequently labeled for C1q, C3b (25 to 48%), or even the terminal C9, with some showing obvious damage. This early/persistent complement attack on both epithelial and myoid cells strongly supports our hypothesis, especially implicating exposed myoid cells in germinal center formation/autoantibody diversification. Remarkably, the similar changes place many apparent AChR-seronegative patients in the same spectrum as the AChR-seropositive patients.
More than 80% of patients with typical generalized myasthenia gravis (MG) have IgG autoantibodies (IgG1 and IgG3) against the muscle acetylcholine receptor (AChR) in its native conformation (and are designated AChRAb+).1,2 These antibodies cause receptor loss, and thus weakness, by accelerating AChR degradation1,3 and especially by activating complement.1,4 Another 5 to 10% of cases instead have (predominantly IgG4) autoantibodies against the muscle-specific kinase (MuSK).5,6,7,8 These MuSKAb+ patients’ MG tends to be more severe, more bulbar,6,7 and apparently harder to control with corticosteroids and azathioprine. It is extremely rare to find anti-AChR and anti-MuSK antibodies in the same patient.5,6,7,8,9,10,11 The remaining 10 to 15% of MG patients seem to have neither antibody in standard radioimmunoprecipitation tests5,6,7,8,9,10,12 and are usually termed seronegative (“SNMG”). Their MG nevertheless improves after plasma exchange, implying that they too have autoantibodies. Identifying their target(s) and developing an equally clear antibody test should save many delays in diagnosis.
In patients with early-onset anti-AChRAb+ MG (EOMG), the myasthenia often ameliorates after thymectomy, and characteristic thymic changes are found in >80% of cases.13,14,15,16,17,18,19 These include epithelial hyperplasia16 and extra-parenchymal infiltration by lymph node-like tissue with T-cell areas and germinal centers (GCs).13,14,15,16,17,19 We have hypothesized that autosensitization is a two-step process15,17: First, helper T cells are primed by unfolded AChR subunits that are expressed in medullary thymic epithelial cells (mTECs).20,21 Next, early antibodies against these subunits then attack rare muscle-like myoid cells nearby. These express intact AChR22 and have long been implicated in autoimmunization.15,23 The ensuing immune complex formation, activation of antigen-presenting cells, and consequent inflammation and complement-mediated damage together provoke formation of GC, leading to autoantibody diversification.17 Myoid cells are the only cells known to express whole AChR outside muscle, where lymphoid infiltrates are minimal in MG.24 By contrast, in the thymus, myoid cells colocalize significantly with these GCs, especially in cases of recent MG onset,15 which clearly incriminates them still further in pathogenesis. Attack on them and/or destruction by complement could explain their very uneven distribution and/or their occasional rarity in EOMG.15 In MuSKAb+ MG, the thymus is typically normal-for-age, and such hyperplasia is rare,25,26 but some infiltrates are seen in 30%26 to 50%25 of SNMG cases.
Seeking more direct evidence to implicate thymic myoid and/or epithelial cells in the response, we have now looked for signs of complement attack on them and for expression of the complement-regulatory proteins CD46, CD55, and CD59. The ability to label these markers in routine paraffin sections25 has enabled us to study a large series of these uncommon cases collected over ∼25 years. Our findings further implicate myoid cells and mTECs in the pathogenesis not only of EOMG but also of SNMG.
Materials and Methods
Clinical Material
With informed consent and ethical committee approval, we studied thymic tissue from the same 11 adult age-matched controls (mostly undergoing thyroid or parathyroid surgery in Würzburg25) and the same 67 patients with generalized MG as in Leite and colleagues25 (detailed in Supplemental Table at http://ajp.amjpathol.org). Their MG was diagnosed by clinical and electromyographic criteria in several centers25; these patients comprised 23 with AChRAb+ MG (=EOMG), 14 with MuSKAb+ MG, and 30 with SNMG (clearly seronegative for both antibodies). We also included another eight generalized MG cases with previously borderline antibodies that now proved low-positive (0.5 to 2 nmol/L) with the higher AChR concentrations currently available27 (and negative against MuSK); these are designated AChRAblo here.
Thymic Sections and Antibodies
Thymic sections (5 μm) from routine formalin-fixed, paraffin-embedded blocks were mounted on 3-amino-propyl-triethoxy-silane-coated slides.25 The sections were dewaxed and rehydrated through graded ethanol solutions and then either microwaved in Target Retrieval Solution (DakoCytomation, Glostrup, Denmark) for 10 minutes at 900 W (for most antibodies) or pretreated with protease type XXIV [0.0125% solution (w/v) in phosphate-buffered saline (PBS; Sigma, Gillingham, Dorset, UK)] at 37°C for 30 minutes for the antibodies asterisked in Table 1, which lists all of the antibodies used.28,29,30,31,32
Table 1.
Primary Antibodies Used for Labeling of Thymic Tissue Sections
| Antibody to | Species, isotype | Clone | Source |
|---|---|---|---|
| Thymocytes and T cells | |||
| CD1a | Mouse, IgG1 | O10 | Immunotech |
| CD3 | Rabbit | DakoCytomation | |
| CD4 | Mouse, IgG1 | 1F6 | Novocastra |
| CD8 | Mouse, IgG1 | C8/144B | DakoCytomation |
| B cells and germinal center cells | |||
| CD20 | Mouse, IgG2a | L26 | DakoCytomation |
| CD21 (CR2) | Mouse, IgG1 | 1F8 | DakoCytomation |
| CD35 (CR1) | Mouse, IgG1 | Ber-MAC-DRC | DakoCytomation |
| Epithelial cells and myoid cells | |||
| Cytokeratin | Rabbit | Abcam | |
| Cytokeratin | Mouse, IgG1 | LP34 | DakoCytomation |
| Desmin | Mouse, IgG1 | D33 | DakoCytomation |
| Desmin* | Mouse, IgG1 | DE-R-11 | DakoCytomation |
| Complement components, receptors, and regulators, and IgG | |||
| C1q | Mouse | G10 | (B.P. Morgan, unpublished) |
| C3c,* NB also detects C3b | Rabbit | DakoCytomation | |
| C9* | Rabbit | Reference 28 | |
| C3aR | Mouse, IgG2a | BIIG1 | Reference 29 |
| C5aR | Rabbit | Reference 29 | |
| CD46 | Mouse | GB24 | References 30, 31 |
| CD55 | Mouse, IgG1 | BRIC 216 | IBGRL, Bristol, UK |
| CD59 | Rabbit | Reference 32 | |
| D68 | Mouse, IgG3 | PG–M1 | DakoCytomation |
| gG* | Rabbit | DakoCytomation |
Tissue pretreated with protease as in Materials and Methods.
Immunohistochemistry
Microwaved sections were incubated at 20°C in a peroxidase-blocking reagent for 10 minutes (DakoCytomation) and for 30 minutes with monoclonal antibodies to human CD3, CD1a, or cytokeratin at optimized dilutions in PBS. After two washes in PBS, binding was detected with the peroxidase-based Envision+ (DakoCytomation) method, before washing and counterstaining with hematoxylin, washing in tap water, and mounting.
Double-Immunofluorescence Labeling
Pretreated sections were incubated for 30 minutes at 20°C with a mixture of two primary antibody dilutions. After two 5-minute washes in PBS, the sections were then incubated with isotype-specific secondary antibodies conjugated to Alexa Fluor 488 or Alexa Fluor 568 (Molecular Probes, Leiden, The Netherlands) at 1:200, for 45 minutes at 20°C. After two further washes, slides were mounted, and nuclei counterstained with 4,6-diamidino-2-phenylindole in fluorescence mounting medium (DakoCytomation).
We used paraffin sections of tonsils or biopsies from rejecting or IgA-nephropathic kidneys as positive controls. Negative controls included either irrelevant primary antibodies matched for species/isotype or none at all. The slides were stored at 4°C for 24 hours and then analyzed on a Zeiss fluorescence microscope (Welwyn Garden City, UK). All of the images were captured via a cooled digital camera, using MacProbe V3.4 software (Applied Imaging, Newcastle-upon-Tyne, UK).
Immunofluorescence Analysis
All slides were coded and analyzed systematically by a single blinded observer (M.I.L.). Entire sections labeled for CD3, CD1a, or cytokeratin (CK) were used to measure areas of total thymic tissue and its compartments25; GCs were counted throughout entire anti-CD20/CD21+CD35-labeled sections to calculate their frequencies/mm2 of thymic tissue.25
Myoid cells were counted throughout two entire sections from each case (one double-stained for desmin/CD20 and the other for desmin/cytokeratin); counts were averaged when we calculated the percentage of exposed myoid cells, ie, those in direct contact with, or wholly within, any infiltrates (see Figure 6). We assessed their disposition in different compartments in all of the sections stained for desmin/cytokeratin. Optimal staining for desmin (in myoid cells) required different retrieval conditions from C3b and C9 (but not from CD59). Double labeling therefore demanded compromises; these were made at the expense of desmin, which normally stains strongly. We might thus have overlooked some small/weakly desmin+ cells.
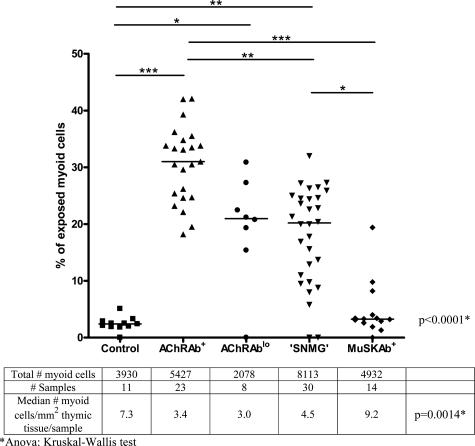
Figure 6.
Percentages of myoid cells exposed to the infiltrates in non-MG controls and MG patient subgroups. Their rarity in the control and MuSKAb+ samples reflects the paucity of infiltrates. There were significantly fewer myoid cells/mm2 in the AChRAb+ group than in the controls (see mini-table below; *P < 0.05, **P < 0.01, ***P < 0.001). *Analysis of variance: Kruskal-Wallis test indicating intergroup heterogeneity.
In every staining combination for complement regulators, components, or receptors, the overall distribution of the labeling was noted (diffuse versus patchy, blood vessels versus parenchyma), and each main feature was graded in each entire section from − to ++++ according to its extent and intensity (−, no staining; +/−, very weak or very rare; +, weak or sporadic; ++, moderate or frequent; +++, strong or extensive; and ++++, very strong staining throughout the section). We recorded labeling on myoid cells according to the thymic compartments in which they were found. Most staining combinations were studied systematically in every thymus, but CD46, CD55, and C1q only in two representative samples from each subgroup (including one MuSKAb+ thymus with infiltrates and one without).
Statistical Analysis
We used the Kruskal-Wallis one-way analysis of variance test followed by Dunn’s post test (for heterogeneity), linear regression, and χ2 with Yates’ correction.
Results
Overview of Distinct Thymic Compartments
In all of the MG thymi, the cortex was essentially normal, as expected,13,14,15,16,17,18 apart from some evidence of atrophy/fatty replacement. This was more evident after steroid treatment in some cases (Supplemental Table at http://ajp.amjpathol.org), which thus enriched the medulla and infiltrates, but had very few other obvious effects. Nearly all MG samples also included areas of relatively normal medullary parenchyma (nMed) with abundant CD4+ and CD8+ T cells, dendritic cells, macrophages, and thymic epithelial cells (TECs), as well as numerous CD20+ B cells mainly around the Hassall’s corpuscles.
In many of the MG thymi, other parenchymal areas were compressed into characteristic medullary epithelial bands (MEBs) by expanding perivascular infiltrates, which were negative for cytokeratin. These infiltrates consisted primarily of lymph node-type T-cell areas, including many antigen-presenting cells, high endothelial venules, and some B cells, as well as GCs varying in number and size. Infiltrates are quantitated (in the same samples) in Leite and colleagues.25 In brief, they were rare/small in the controls, although they were age-matched adults. However, they were seen in nearly all of the AChRAb+ MG thymi (including the AChRAblo) and also in >50% of the SNMG samples but in only 3 of the 14 with MuSKAb+ MG.25 The distribution of myoid cells is detailed in the final section. The changes in MG are described below in order of increasing abnormality.
Expression of Complement Receptors [C5aR, C3aR, and CR1 (=CD35)]
Numerous cell types (T, B, and dendritic cells and macrophages) normally express receptors for activated complement components. In both MG and normal thymi, some TECs stained for C5aR, mainly in subcapsular and medullary areas (especially around the Hassall’s corpuscles) rather than in the cortex (Figure 1A). Surprisingly, in the MG samples with infiltrates, we saw increased staining on many of the mTECs in the MEBs as well as in the nMed, but it was minimal in the infiltrates (Figure 1C; summarized in Table 2).
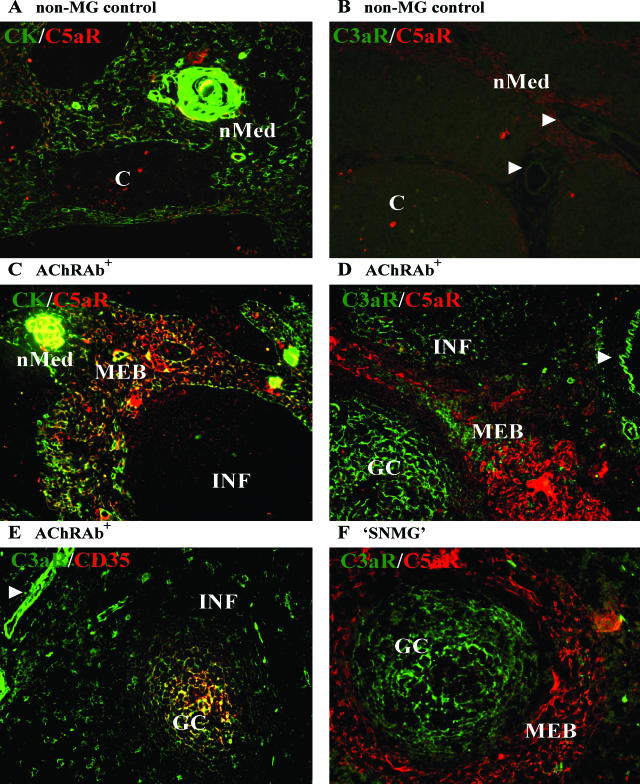
Figure 1.
Distribution of complement receptors C3aR, C5aR, and CR1 (receptor for C3b and C4b) (all in red) in epithelial areas and/or infiltrates in thymi from non-MG controls (A and B), AChRAb+ (C–E), or SNMG (F) MG patients. A and B: In control thymi, occasional mTECs are weakly C5aR+, as in some areas in MG thymi, but labeling for C3aR is almost absent, even in blood vessels (arrowheads) (female donor 29 years of age). C–F: In MG, both C3aR and C5aR are expressed strongly in most samples with infiltrates (INF) ± GCs. C5aR is mainly on epithelial cells (cytokeratin+ in C; green), whether in the relatively normal medulla (nMed) or MEBs (C, D, and F), whereas most C3aR labeling is seen in the infiltrates and particularly in the GC (D–F), and in blood vessels (white arrowheads) (D and E). [MG donors all female: C, 17 years of age; D, 20 years of age, E, 29 years of age; and F, 38 years of age (only F was taking steroids)]. Original magnifications, ×200.
Table 2.
Summary of the Range and Intensity of Labeling in the Main Thymic Compartments in MG Samples with Infiltrates
| Complement receptors:
|
Complement regulators:
|
Activated complement components:
|
|||||
|---|---|---|---|---|---|---|---|
| C5aR | C3aR | CD46/CD55 | CD59 | C1q | C3b | C9 | |
| Cortex | |||||||
| MG | +/− | − | +/− | ++/− | − | − | − |
| (Con) | (−) | (−) | (+) | (+) | (−) | (−) | (−) |
| nMed | |||||||
| MG | +++/+ | +/− | ++/+ | +++/+ | ++/+ | ++/+ | − |
| (Con) | (++) | (−) | (+) | (+) | (±) | (+/−) | (−) |
| MEBs | |||||||
| MG | ++++/+ | ++/− | +++/+ | ++++/+ | ++++/+ | ++++/+ | ±/− |
| Infiltrates | |||||||
| MG | +/− | ++++/+ | +++/+ | ++++/+ | +++/+ | ++++/+ | +/− |
| Myoid cells | |||||||
| MG | +/− | +/− | +/− | − | ++/− | +++/− | +/− |
| (Con) | (−) | (−) | (+) | (−) | (−) | (−) | (−) |
| Blood vessels | |||||||
| MG | ++/− | ++++/+/− | ++/− | ++++/+ | ++/+ | ++ | − |
| (Con) | (+) | (±) | (+) | (+++) | (+) | (++) | (−) |
Maximal levels for controls (Con) are shown in parentheses where applicable. Each staining was graded in each entire section from − to ++++ according to its extent and intensity (−, no staining; +/−, very weak or very rare; +, weak or sporadic; ++, moderate or frequent; +++, strong or extensive; and ++++, very strong staining throughout the section). The controls had virtually no MEBs or infiltrates and MG samples without infiltrates (eg, in MuSKAb+ MG) were broadly similar. Labeling in septa and surrounding connective tissue was similar to that in blood vessels, but generally weaker, especially for C3aR and CD59. Distributions were very similar for CD46 and CD55. nMed, relatively normal medullary areas; MEBs, medullary epithelial bands.
In general, C3aR showed an inverse distribution to that of C5aR (Figure 1, D and F; Table 2). It was seen in only two of the controls, where it was largely confined to blood vessels (Figure 1B, arrowheads). In most MG samples, it was seen also on occasional patches of mTECs (Figure 1D). Although many extraparenchymal T and B cells were C3aR+ too, it was strongest/most abundant on the follicular dendritic cells in the GC (Figure 1, D–F) and also in blood vessels (Figure 1, D and E). The receptor for C3b, CR1 (CD35), was essentially confined to GCs (Figure 1E) and was not detected in the controls.
In the various MG subgroups, the above changes occurred in any thymi with sizeable infiltrates (summarized in Table 2), correlating with their frequency and extent. Therefore, they were somewhat more prominent in the AChRAb+ than the AChRAblo and apparently SNMG samples but were rare in MuSKAb+ thymi. The C3aR and C5aR expression implies the potential to respond to any available activated complement component, subject to complement regulation.
Expression of Complement Regulators [CR1 (=CD35), CD46, CD55, and CD59]
On binding their targets, antibodies may initiate the classical complement cascade by activating C1, leading to formation of the C3 convertase (C4b2a) and activation (conversion) of C3, so generating both active C3b fragments and the C5 convertase (C4b2a3b). This leads to cleavage of C5 and assembly of pore-forming membrane-attack complexes (MAC; C5b-C9) in target cell membranes.33
The major cell-bound complement regulators are CD55 (DAF), which accelerates decay of the C3 convertase, CD46, which enhances enzymatic degradation of C3b and C4b, and CD59, which blocks assembly of C9 into the MAC.34 CR1 (=CD35) can also regulate the C3 convertase but is primarily a receptor for activated C3. We screened all thymi for CD59 and CR1 and two representative samples from each patient subgroup for CD46 and CD55. We detected CR1 in all GCs (Figure 1E), but not elsewhere.
In control thymi, labeling for CD46 (Figure 2A) and CD55 (not shown) was minimal and primarily restricted to blood vessels in the medulla and septa (Table 2). By contrast, CD59 was more widespread, being found, in addition, on scattered macrophages and dendritic cells, as well as on some subcapsular and medullary TECs (especially around Hassall’s corpuscles; Figure 2D), like C5aR, but more variable in extent and intensity.
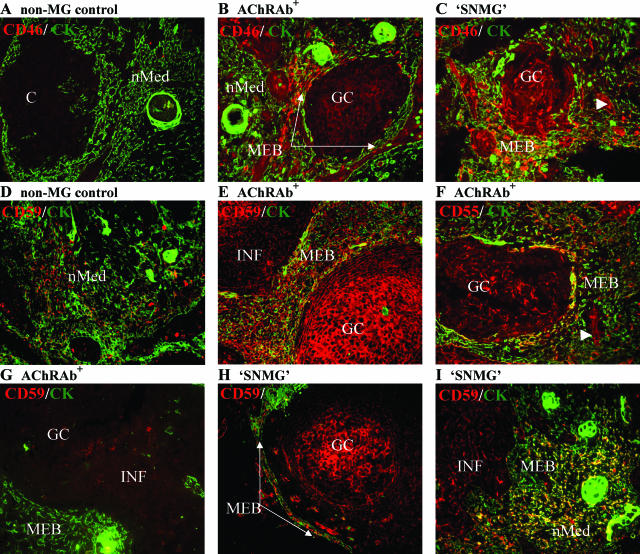
Figure 2.
Distribution of complement regulators CD46, CD55, and CD59 (all in red) in epithelial areas and infiltrates in control (A and D) and MG thymi (B, C, and E–I). Cytokeratin (CK, green). A: In controls, CD46 (A) and CD55 (not shown) expression is minimal; in MG, both are much stronger in the MEBs than in the nMed in both AChRAb+ (B and F) and SNMG (C) MG. They are also seen on blood vessels, some mTECs, and other cells (eg, macrophages), and especially in the GC; CD55 sometimes shows a linear distribution at MEB borders (F, bottom left) like that of laminin. D: In controls, CD59 is expressed by numerous medullary TECs and some septal macrophages. In MG, CD59 labeling is variable: it is extensive in nMed (I) and in many MEBs, infiltrates, and GC in both AChRAb+ (E) and SNMG (H) MG, but not universally, even where there are nearby infiltrates (G). White arrowheads mark blood vessels. (Donors all female: A, 17 years of age; B, 16 years of age; C, 40 years of age; D, 21 years of age; E, 20 years of age; F, 16 years of age; G, 20 years of age; *H, 38 years of age; and *I, 33 years of age; *taking steroids). Original magnifications, ×200.
In MG, CD46 and CD55 were again patchily up-regulated in the nMed, and especially in the MEBs (Figure 2, B, C, and F), and so was CD59 (Figure 2, E, H, and I; summarized in Table 2); they were frequently also seen in blood vessels (Figure 2, C and F; arrowheads). Clear double-labeling of cytokeratin+ cells was more obvious for CD59 and CD55 than CD46 (Figure 2, E, F, and I than B). As expected,35 all three complement regulators were more prominent in the infiltrates, on macrophages, B cells, and dendritic cells and especially in most GCs (Figure 2, B, C, E, F, H, and I; Table 2), although not in every infiltrated area (Figure 2G). With rare exceptions, all these findings were broadly similar in the infiltrated areas in all of the MG subgroups, although CD55 was less evident in an unusual MuSKAb+ sample with infiltrates (not shown).
Deposition of C1q, C3b, and C9 Components
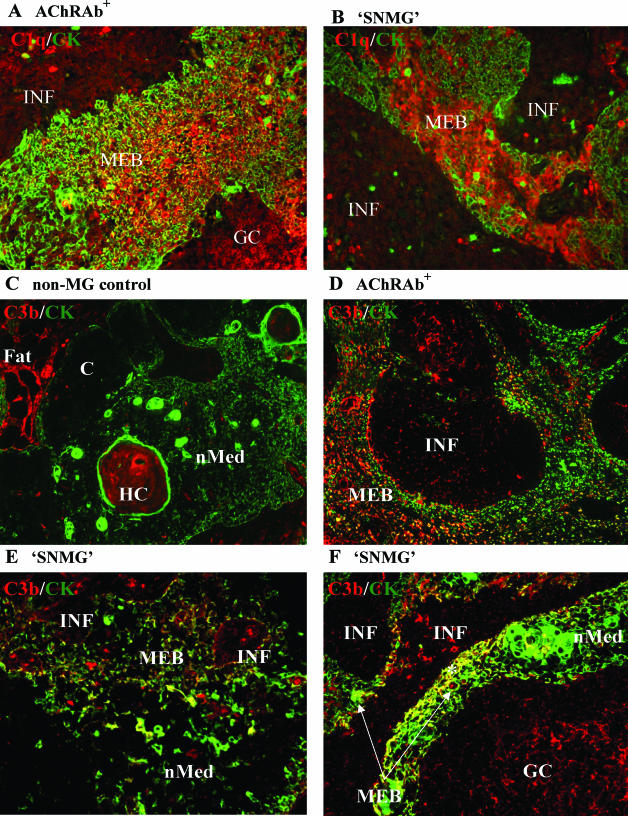
In control thymi, labeling for C1q and C3b was largely restricted to the Hassall’s corpuscles,36 blood vessel endothelium, and connective tissue and was otherwise minimal in both cortex and medulla (Table 2, Figure 3C). In MG, by contrast, we saw clear signs of activation of the classical complement pathway; surprisingly, most samples with infiltrates showed substantial labeling for C1q on patches of densely packed mTECs in samples with infiltrates (Figure 3, A and B). Many such mTECs also labeled strongly for C3b (Figure 3, D–F), which sometimes showed a linear laminin-like pattern (Figure 3D). However, other apparently similar areas in the same sections were negative for either C1q or C3b (Figure 3D), as was the nMed (Figure 3, E and F; except for C3b in three AChRAb+ cases). Within the infiltrates, labeling for C1q, and especially for C3b, was strongest/most consistent in the GCs (on follicular dendritic cells and B cells as expected35; Figure 3, A and F; see also Figure 5C) but was also evident on some B lymphocytes and macrophages (Figure 3, D and E).
Figure 3.
Labeling for C1q and C3b complement fragments (both in red) in epithelial areas and infiltrates in MG and control thymi. Cytokeratin (CK, green). A and B: In MG, there is extensive patchy labeling for C1q in mTECs and other cells in MEBs and in infiltrates and GC in AChRAb+ (A) or SNMG (B) samples. C: In controls, C3b labeling is seen in Hassall’s corpuscles (HC), fat, and connective tissue septa and blood vessels. In MG, whether AChRAb+ or SNMG, it is most evident in MEBs (focally in D and F), in the adjacent infiltrates (D and E), and in their GC (F). The nMed areas are negative for C3b in most MG thymi (E and F). (Donors all female: A, 16 years of age; *B, 38 years of age; C, 24 years of age; *D, 24 years of age; E, 43 years of age; and F, 28 years of age; *on steroids). Original magnifications, ×200.
Figure 5.
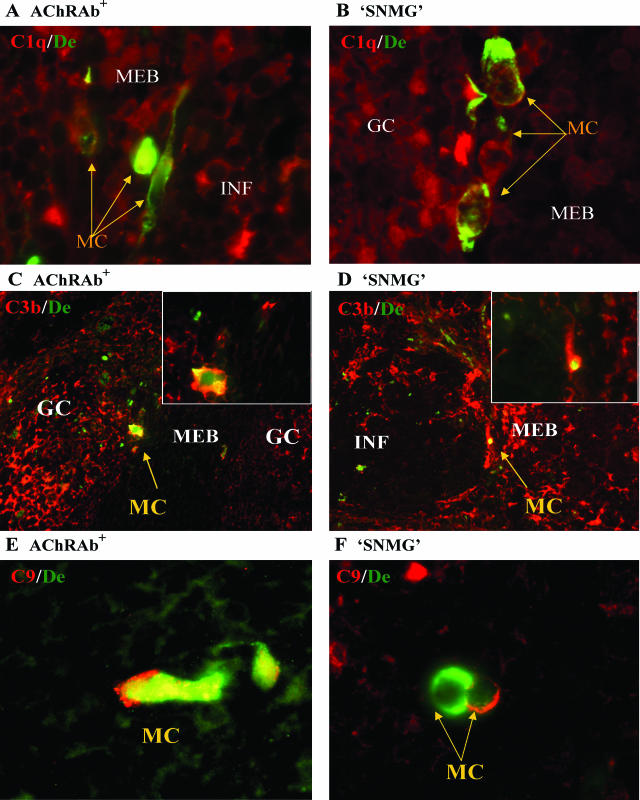
Labeling for C1q, C3b, or C9 (all in red) on exposed myoid cells (MC) in MG thymi. Desmin (De, green). A and B: Some exposed myoid cells label for C1q in AChRAb+ (A) or SNMG (B) MG samples, in which many of them label for C3b (C and D; enlarged in insets) and some for C9 in AChRAb+ (E) or SNMG (F) samples. Note aggregation of desmin (B and E). (Donors all female: A, 16 years of age; *B, 33 years of age; C, 20 years of age; *D, 38 years of age; E, 35 years of age; and *F, 33 years of age; *on steroids). Original magnifications: ×200 (C and D); ×1000 (A, B, E, F, and insets).
Staining for C9/MAC was generally weak and was not seen on either TECs or even C3b+ follicular dendritic cells (not shown), implying a bias toward earlier stages of complement activation. Thus, C9/MAC showed an inverse distribution to that of CD59 in reactive GC. Overall, as in our previous studies, these thymic GCs show labeling essentially identical to that in reactive tonsillar GC for all of the markers we have now applied for the first time in MG.
Again, all such labeling was rare in the relatively normal thymi but was broadly similar in any MG sample with infiltrates, regardless of the subgroup (as summarized in Tables 2 and 3), although it did vary in degree. Moreover, C3b deposition on mTECs was equally prevalent in thymi from the most recent onset and the longer-standing AChRAb+ and apparently SNMG patients (Supplemental Figure A at http://ajp.amjpathol.org).
Table 3.
Numbers of Samples Showing C3b Deposition in the MEBs, in the Infiltrates, and on Myoid Cells Exposed to the Infiltrates in Each Subgroup, and Estimated Percentages of the Myoid Cells Positive for C3b in Each Compartment Median (Range)
| C3b in MEB | C3b in infiltrates | C3b on exposed myoid cells | % of the myoid cells in nMed that labeled for C3b | % of the exposed myoid cells that labeled for C3b | |
|---|---|---|---|---|---|
| Controls (n = 11) | 2 (18%)* | NA | NA | 0 | NA |
| AChRAb+ (n = 23) | 20 (87%) | 17 (74%) | 18 (78%) | 3.8% (0.7 to 5.6) | 38% (8 to 48) |
| AChRAblo (n = 8) | 4 (50%) | 4 (50%) | 4 (50%) | 3.3% (1.9 to 5.1) | 25% (14 to 27) |
| SNMG (n = 30) | 20 (67%) | 15 (50%) | 19 (63%) | 2.7% (0.4 to 3.7) | 24% (4 to 33) |
| MuSKAb+ (n = 14) | 3 (21%) | 2 (14%) | 2 (14%) | 1.2% | 14% (11,17) |
The same individual samples in each MG subgroup showed C3b labeling on exposed myoid cells and in the MEB or infiltrates.
Occasional areas of mTEC adjacent to small perivascular expansions. NA, not applicable.
Involvement of Myoid Cells
In general, myoid cells (desmin+) were haphazardly distributed in the nMed, often near the Hassall’s corpuscles, and were sometimes clustered. In any thymi with infiltrates, other very typical locations were at the edges of MEBs, ie, where they interfaced with infiltrates (Figures 4B and 5, A, B, and D), especially where there were GCs nearby, or even wholly within the infiltrates (Figures 4A and 5C); together, these are designated exposed myoid cells.
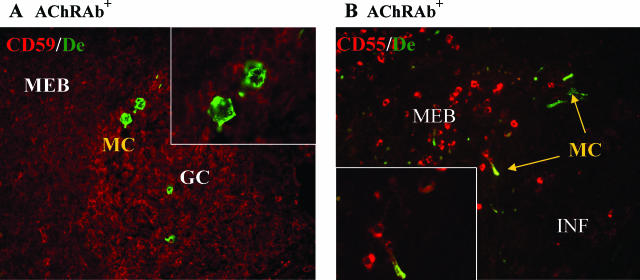
Figure 4.
Rarity of complement regulators on myoid cells. In both control (not shown) and MG thymi (A), myoid cells (MC) are uniformly CD59− (red), even when exposed to infiltrates, but ∼5% of the latter express detectable CD55 (red) (B, inset). (Donors both female: A, 20 years of age; B, 16 years of age). Desmin (De, green). Original magnifications: ×200; ×1000 (insets).
Complement Regulators and Receptors
We never observed significant staining in any of the control or MG samples for CD59 on any of the many thousands of myoid cells we examined (Figure 4A, Table 2). Likewise, they showed no labeling for CD46 or CD55 in the two controls tested, but these regulators were clearly detectable on ∼10 and 5%, respectively, of the exposed myoid cells in the seven representative MG thymi from each subgroup with infiltrates (Figure 4B). Nearly all myoid cells must also be negative for CR1 because it was confined to the GC. In one control, they also appeared negative for C3aR and C5aR; however, in two AChRAb+ thymi, up to 5% of the exposed myoid cells were C3aR+ and up to 10% were C5aR+ (not shown). Hence, in general, myoid cells appear relatively deficient in complement regulators and therefore vulnerable to complement attack, for which we checked next.
Complement Components
In the control thymi, myoid cells very rarely showed any detectable C1q or C3b (Table 3). In MG, both were rare in thymi without infiltrates and uncommon in the nMed (Tables 2 and 3). In sharp contrast, ∼10% of the exposed myoid cells showed clear C1q labeling (Figure 5, A and B), which implicates the classical pathway in activation. More strikingly, in almost every MG thymus with infiltrates, C3b labeling was seen clearly and strongly on many of the exposed myoid cells (Figure 5, C and D), up to 48% of them in some samples (Table 3). At lower frequency, we also saw clear staining for C9/MAC on some of the exposed myoid cells (Figure 5, E and F). Although the C3b+ myoid cells showed no terminal dUTP nick-end labeling staining (for apoptosis; not shown), a few showed signs of damage (eg, desmin aggregation; Figure 5, B and E).
Exposed myoid cells were much more frequent in AChRAb+ than control thymi (Figure 6), and were also more common in most AChRAblo and many apparently SNMG thymi, whereas they were rare in the MuSKAb+ subgroup (Figure 6). Moreover, the frequencies of myoid cells under complement attack (by C3b) showed a parallel hierarchy, reaching up to 48% in the AChRAb+, 27% in the AChRAblo, and 33% in some SNMG samples (Table 3B) but only 17% in two of the three MuSKAb+ samples with occasional small infiltrates. Remarkably, this attack was already evident in the most recent-onset cases, in fact, regardless of MG duration at thymectomy (Supplemental Figure B at http://ajp.amjpathol.org), and also in some thymi with very modest infiltrates and few GC, ie, with signs of atrophy/burnout.
Discussion
This article reports three novel findings in the MG thymus. First, we found unexpected up-regulation of complement receptors and regulators on the hyperplastic medullary epithelial cells (mTECs), and evidence of early and persistent complement attack on them. These findings are consistent with the proposed roles of mTECs in autosensitizing AChR-specific helper T cells15,16,17 and in attracting the lymph node-type infiltrates.37 Second, the general lack of CD46, CD55, and especially CD59 on myoid cells indicates vulnerability to complement-mediated damage. Moreover, the deposition of C3b on many exposed myoid cells (often near GCs), and even of the terminal C5b-9 (MAC) complex on some, strongly supports their proposed role in provoking GC formation and thus in autoantibody diversification. Third, the changes in many patients with apparently seronegative (SNMG), and most with borderline AChRAb titers (AChRAblo), are very similar to those in EOMG (although somewhat milder). This argues strongly that these subgroups belong to the EOMG spectrum; it therefore also implicates AChR autoantibodies in both, which are evidently underestimated in standard assays with native AChR in dilute solution (M.I. Leite, S. Jacob, S. Viegas, J. Cossins, D. Beeson, B.P. Morgan, N. Willcox, and A. Vincent, in preparation). The rarity of similar thymic changes in MuSKAb+ MG again emphasizes the distinctness of this subgroup.
Involvement of mTECs
In our previous studies, the mTECs appeared hyperplastic because of their dense packing and more uniform staining for several integrins, especially αVβ516; to that we can now add increased expression of C5aR, CD46, and CD55 and CD59. As with other epithelial (and endothelial) cells,38,39,40 this up-regulation could be a result of attack by autoantibodies triggering the classical complement pathway, as indicated by the labeling for C1q, and especially for C3b. This, in turn, agrees very well with the previously reported autoantibodies against mTECs in EOMG,41 whereas our failure to detect factor B (not shown) argues against any major concomitant role for the alternative pathway. Expression of peripheral tissue-specific autoantigens by mTECs is often focal,42 as with AChR subunits,17 which could explain the patchy labeling we observed for C5aR and complement regulators. Furthermore, sublytic MAC deposition can stimulate epithelial, endothelial, and Schwann cell proliferation,43,44,45,46,47 which might contribute to the mTECs’ hyperplastic appearance in MG.16 Their up-regulation of CXCL13 may be an important factor in provoking the nearby infiltrates in MG.37
Involvement of Myoid Cells
In experimental MG in mice, cd55 or cd59 alone can each protect against motor endplate damage.48,49,50 However, unlike the mTECs, few myoid cells expressed CD46 or CD55 and none were CD59+, even when there was marked local infiltration, implying general vulnerability to complement. Indeed, a remarkably high proportion of the exposed myoid cells in MG labeled for C1q, more for C3b, and a few even for the terminal membrane attack complex. That implies that GC, and adjacent infiltrates, develop in response to complement deposition on myoid cells. Their subsequent killing and/or proliferation might explain their variable numbers (Figure 6), or even virtual absence, in some EOMG samples15; C9/MAC+ myoid cells might be underestimated if they are killed in some cases. In fact, it would be surprising if myoid cells escaped such attack because complement-mediated damage is such an important cause of the AChR loss at the muscle endplates in MG.4 Indeed, the lower expression of complement regulators in extraocular than other muscles apparently contributes to their susceptibility in MG,51,52 as it does on neurons and oligodendrocytes in MS.53
This variability in myoid cells, and in complement deposition, within and between MG subgroups also suggests that complement dysregulation might be another factor influencing pathogenesis in MG. Notably, the genes for CR1, CR2, CD46, CD55, and factor H map to the complement regulatory gene cluster (chromosome 1q32),54 which might prove a fertile region to screen for genetic susceptibility in MG. Indeed, associations with factor H are now being recognized in inflammatory diseases.54
One consistent finding is that, very frequently, the GCs were associated with myoid cells positive for C1q and C3b, implicating them still more deeply in formation of GCs. Because these are the sites of somatic hypermutation,55 and because many of the thymic GCs and their B cells are specific for AChR,56 including the fetal isoform that myoid cells express,57 they must both be important in diversifying the autoantibodies in EOMG56,57,58 so that they recognize AChR in its native conformation (even if other cell types prove also to be involved in this epitope spreading). Their resulting heterogeneity must, in turn, enhance both their pathogenicity and their ability to bind solubilized AChR at high dilution in standard assays.
Correlating Thymic Changes with Autoantibody Serology
That all of the above findings were so similar, if milder, in the majority of the apparently SNMG as well as the AChRAblo thymi argues very strongly that many patients in these subgroups belong to the same spectrum as those with AChRAb+ MG. Indeed, we are now able to detect anti-AChR antibodies, in ∼50% of previously SNMG patients, by their binding to AChRs densely clustered on transfected human embryonic kidney cells.59 Interestingly, positivity in this new assay correlates with thymic infiltrates and C3b+-exposed myoid cells in these patients’ thymi.59 The contrasting rarity of similar thymic changes in MuSKAb+ cases fits with the predominance of noncomplement-activating IgG4 anti-MuSK antibodies; the few patients with infiltrates might be the ones who also have some complement-activating IgG1 anti-MuSK.8
There is one final notable correlate. The GCs were fewer and smaller in these low-affinity (SNMG) patients’ thymi, which might well imply more limited diversity of their autoantibodies than in typical AChRAb+ MG, which might, in turn, make them harder to detect in standard assays, and possibly less pathogenic. Indeed, the MG in these patients does seem to be less severe than in the MuSKAb+ subgroup and more responsive to standard therapies.6,7,8,60 These may include thymectomy, which, if done early, could act by interrupting the processes we have observed.
Supplementary Material
Acknowledgments
We thank Dr. A. Martins Silva, Dr. E. Dulmet, Dr. V.T. De Montpreville, the patients and controls for access to thymus samples, J.B. de Sousa for advice, and Dr. H. Shiono and Dr. I. Roxanis for crucial groundwork.
Footnotes
Address reprint requests to Nick Willcox, Neuroscience Group, Dept. of Clinical Neurology, Weatherall Institute for Molecular Medicine, Headington, Oxford, OX3 9DS, UK. E-mail: nick.willcox@imm.ox.ac.uk.
Supported by the Fundação para a Ciência e a Tecnologia, Portugal (to M.I.L.); the Leukaemia Research Fund (to M.J.); the Deutsche Krebshilfe (grants 101740 and 106430 to P.S. and A.M.); the Princess Beatrix Fonds (to E.N. and J.J.G.M.V.); the Association Française contre les Myopathies (to S.B.-A.); the Wellcome Trust Programme (grant 068590 to B.P.M.); the United Kingdom Medical Research Council (to A.V. and N.W.); the Muscular Dystrophy Campaign (to A.V. and N.W.); the Myasthenia Gravis Association (to A.V. and N.W.); and the European Union (grant QLK3-CT-2001-00225).
Supplemental material for this article can be found on http://ajp. amjpathol.org.
A.V. receives royalties and consultancy fees for antibody assays against AChR and MuSK.
References
- Vincent A. Unravelling the pathogenesis of myasthenia gravis. Nat Rev Immunol. 2002;2:797–804. doi: 10.1038/nri916. [DOI] [PubMed] [Google Scholar]
- Tzartos SJ, Barkas T, Cung MT, Mamalaki A, Marraud M, Orlewski P, Papanastasiou D, Sakarellos C, Sakarellos-Daitsiotis M, Tsantili P, Tsikaris V. Anatomy of the antigenic structure of a large membrane autoantigen, the muscle-type nicotinic acetylcholine receptor. Immunol Rev. 1998;163:89–120. doi: 10.1111/j.1600-065x.1998.tb01190.x. [DOI] [PubMed] [Google Scholar]
- Drachman DB, Adams RN, Josifek LF, Self SG. Functional activities of autoantibodies to acetylcholine receptors and the clinical severity of myasthenia gravis. N Engl J Med. 1982;307:769–775. doi: 10.1056/NEJM198209233071301. [DOI] [PubMed] [Google Scholar]
- Engel AG, Lambert EH, Howard FM. Immune complexes (IgG and C3) at the motor end-plate in myasthenia gravis: ultrastructural and light microscopic localization and electrophysiologic correlations. Mayo Clin Proc. 1977;52:267–280. [PubMed] [Google Scholar]
- Hoch W, McConville J, Helms S, Newsom-Davis J, Melms A, Vincent A. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat Med. 2001;7:365–368. doi: 10.1038/85520. [DOI] [PubMed] [Google Scholar]
- Evoli A, Tonali PA, Padua L, Monaco ML, Scuderi F, Batocchi AP, Marino M, Bartoccioni E. Clinical correlates with anti-MuSK antibodies in generalized seronegative myasthenia gravis. Brain. 2003;126:2304–2311. doi: 10.1093/brain/awg223. [DOI] [PubMed] [Google Scholar]
- Sanders DB, El-Salem K, Massey JM, McConville J, Vincent A. Clinical aspects of MuSK antibody positive seronegative MG. Neurology. 2003;60:1978–1980. doi: 10.1212/01.wnl.0000065882.63904.53. [DOI] [PubMed] [Google Scholar]
- McConville J, Farrugia ME, Beeson D, Kishore U, Metcalfe R, Newsom-Davis J, Vincent A. Detection and characterization of MuSK antibodies in seronegative myasthenia gravis. Ann Neurol. 2004;55:580–584. doi: 10.1002/ana.20061. [DOI] [PubMed] [Google Scholar]
- Ohta K, Shigemoto K, Kubo S, Maruyama N, Abe Y, Ueda N, Fujinami A, Ohta M. MuSK Ab described in seropositive MG sera found to be Ab to alkaline phosphatase. Neurology. 2005;65:1988. doi: 10.1212/01.wnl.0000188881.46043.44. [DOI] [PubMed] [Google Scholar]
- Plested CP, Tang T, Spreadbury I, Littleton ET, Kishore U, Vincent A. AChR phosphorylation and indirect inhibition of AChR function in seronegative MG. Neurology. 2002;59:1682–1688. doi: 10.1212/01.wnl.0000041625.41937.ff. [DOI] [PubMed] [Google Scholar]
- Zhang X, Yang M, Xu J, Zhang M, Lang B, Wang W, Vincent A. Clinical and serological study of myasthenia gravis in HuBei Province, China. J Neurol Neurosurg Psychiatry. 2007;78:386–390. doi: 10.1136/jnnp.2006.100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spreadbury I, Kishore U, Beeson D, Vincent A. Inhibition of acetylcholine receptor function by seronegative myasthenia gravis non-IgG factor correlates with desensitization. J Neuroimmunol. 2005;162:149–156. doi: 10.1016/j.jneuroim.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Berrih S, Morel E, Gaud C, Raimond F, Le Brigand H, Bach JF. Anti-AChR antibodies, thymic histology, and T cell subsets in myasthenia gravis. Neurology. 1984;34:66–71. doi: 10.1212/wnl.34.1.66. [DOI] [PubMed] [Google Scholar]
- Schluep M, Willcox N, Ritter MA, Newsom-Davis J, Larche M, Brown AN. Myasthenia gravis thymus: clinical, histological and culture correlations. J Autoimmun. 1988;1:445–467. doi: 10.1016/0896-8411(88)90067-4. [DOI] [PubMed] [Google Scholar]
- Roxanis I, Micklem K, McConville J, Newsom-Davis J, Willcox N. Thymic myoid cells and germinal center formation in myasthenia gravis; possible roles in pathogenesis. J Neuroimmunol. 2002;125:185–197. doi: 10.1016/s0165-5728(02)00038-3. [DOI] [PubMed] [Google Scholar]
- Roxanis I, Micklem K, Willcox N. True epithelial hyperplasia in the thymus of early-onset myasthenia gravis patients: implications for immunopathogenesis. J Neuroimmunol. 2001;112:163–173. doi: 10.1016/s0165-5728(00)00415-x. [DOI] [PubMed] [Google Scholar]
- Shiono H, Roxanis I, Zhang W, Sims GP, Meager A, Jacobson LW, Liu JL, Matthews I, Wong YL, Bonifati M, Micklem K, Stott DI, Todd JA, Beeson D, Vincent A, Willcox N. Scenarios for autoimmunization of T and B cells in myasthenia gravis. Ann NY Acad Sci. 2003;998:237–256. doi: 10.1196/annals.1254.026. [DOI] [PubMed] [Google Scholar]
- Flores KG, Li J, Sempowski GD, Haynes BF, Hale LP. Analysis of the human thymic perivascular space during aging. J Clin Invest. 1999;104:1031–1039. doi: 10.1172/JCI7558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castleman B, Norris EH. The pathology of the thymus in myasthenia gravis: a study of 35 cases. Medicine. 1949;28:27–58. doi: 10.1097/00005792-194902000-00002. [DOI] [PubMed] [Google Scholar]
- Wakkach A, Guyon T, Bruand C, Tzartos S, Cohen-Kaminsky S, Berrih-Aknin S. Expression of acetylcholine receptor genes in human thymic epithelial cells: implications for myasthenia gravis. J Immunol. 1996;157:3752–3760. [PubMed] [Google Scholar]
- MacLennan CA, Beeson D, Willcox N, Vincent A, Newsom-Davis J. Muscle nicotinic acetylcholine receptor mRNA expression in hyperplastic and neoplastic myasthenia gravis thymus. Ann NY Acad Sci. 1998;841:407–410. doi: 10.1111/j.1749-6632.1998.tb10954.x. [DOI] [PubMed] [Google Scholar]
- Schluep M, Willcox N, Vincent A, Dhoot GK, Newsom-Davis J. Acetylcholine receptors in human thymic myoid cells in situ: an immunohistological study. Ann Neurol. 1987;22:212–222. doi: 10.1002/ana.410220205. [DOI] [PubMed] [Google Scholar]
- Wekerle H, Ketelsen UP. Intrathymic pathogenesis and dual genetic control of myasthenia gravis. Lancet. 1977;1:678–680. doi: 10.1016/s0140-6736(77)92118-3. [DOI] [PubMed] [Google Scholar]
- Nakano S, Engel AG. Myasthenia gravis: quantitative immunocytochemical analysis of inflammatory cells and detection of complement membrane attack complex at the end-plate in 30 patients. Neurology. 1993;43:1167–1172. doi: 10.1212/wnl.43.6.1167. [DOI] [PubMed] [Google Scholar]
- Leite MI, Strobel P, Jones M, Micklem K, Moritz R, Gold R, Niks EH, Berrih-Aknin S, Scaravilli F, Canelhas A, Marx A, Newsom-Davis J, Willcox N, Vincent A. Fewer thymic changes in MuSK antibody-positive than in MuSK antibody-negative MG. Ann Neurol. 2005;57:444–448. doi: 10.1002/ana.20386. [DOI] [PubMed] [Google Scholar]
- Lauriola L, Ranelletti F, Maggiano N, Guerriero M, Punzi C, Marsili F, Bartoccioni E, Evoli A. Thymus changes in anti-MuSK-positive and -negative myasthenia gravis. Neurology. 2005;64:536–538. doi: 10.1212/01.WNL.0000150587.71497.B6. [DOI] [PubMed] [Google Scholar]
- Beeson D, Jacobson L, Newsom-Davis J, Vincent A. A transfected human muscle cell line expressing the adult subtype of the human muscle acetylcholine receptor for diagnostic assays in myasthenia gravis. Neurology. 1996;47:1552–1555. doi: 10.1212/wnl.47.6.1552. [DOI] [PubMed] [Google Scholar]
- Pratt JR, Basheer SA, Sacks SH. Local synthesis of complement component C3 regulates acute renal transplant rejection. Nat Med. 2002;8:582–587. doi: 10.1038/nm0602-582. [DOI] [PubMed] [Google Scholar]
- Monsinjon T, Gasque P, Chan P, Ischenko A, Brady JJ, Fontaine MC. Regulation by complement C3a and C5a anaphylatoxins of cytokine production in human umbilical vein endothelial cells. FASEB J. 2003;17:1003–1014. doi: 10.1096/fj.02-0737com. [DOI] [PubMed] [Google Scholar]
- Hsi BL, Yeh CJ, Fenichel P, Samson M, Grivaux C. Monoclonal antibody GB24 recognizes a trophoblast-lymphocyte cross-reactive antigen. Am J Reprod Immunol Microbiol. 1988;18:21–27. doi: 10.1111/j.1600-0897.1988.tb00228.x. [DOI] [PubMed] [Google Scholar]
- Adams EM, Brown MC, Nunge M, Krych M, Atkinson JP. Contribution of the repeating domains of membrane cofactor protein (CD46) of the complement system to ligand binding and cofactor activity. J Immunol. 1991;147:3005–3011. [PubMed] [Google Scholar]
- Davies CS, Harris CL, Morgan BP. Glycation of CD59 impairs complement regulation on erythrocytes from diabetic subjects. Immunology. 2005;114:280–286. doi: 10.1111/j.1365-2567.2004.02086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan BP. Complement membrane attack on nucleated cells: resistance, recovery and non-lethal effects. Biochem J. 1989;264:1–14. doi: 10.1042/bj2640001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan BP, Meri S. Membrane proteins that protect against complement lysis. Springer Semin Immunopathol. 1994;15:369–396. doi: 10.1007/BF01837366. [DOI] [PubMed] [Google Scholar]
- Lampert IA, Schofield JB, Amlot P, Van Noorden S. Protection of germinal centres from complement attack: decay-accelerating factor (DAF) is a constitutive protein on follicular dendritic cells. A study in reactive and neoplastic follicles. J Pathol. 1993;170:115–120. doi: 10.1002/path.1711700204. [DOI] [PubMed] [Google Scholar]
- French LE, Sappino AP, Tschopp J, Schifferli JA. Distinct sites of production and deposition of the putative cell death marker clusterin in the human thymus. J Clin Invest. 1992;90:1919–1925. doi: 10.1172/JCI116069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meraouna A, Cizeron-Clairac G, Panse RL, Bismuth J, Truffault F, Tallaksen C, Berrih-Aknin S. The chemokine CXCL13 is a key molecule in autoimmune myasthenia gravis. Blood. 2006;108:432–440. doi: 10.1182/blood-2005-06-2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprott H, Muller-Ladner U, Distler O, Gay RE, Barnum SR, Landthaler M, Scholmerich J, Lang B, Gay S. Detection of activated complement complex C5b-9 and complement receptor C5a in skin biopsies of patients with systemic sclerosis (scleroderma). J Rheumatol. 2000;27:402–404. [PubMed] [Google Scholar]
- van Beek J, van Meurs M, t Hart BA, Brok HP, Neal JW, Chatagner A, Harris CL, Omidvar N, Morgan BP, Laman JD, Gasque P. Decay-accelerating factor (CD55) is expressed by neurons in response to chronic but not acute autoimmune central nervous system inflammation associated with complement activation. J Immunol. 2005;174:2353–2365. doi: 10.4049/jimmunol.174.4.2353. [DOI] [PubMed] [Google Scholar]
- Mason JC, Yarwood H, Sugars K, Morgan BP, Davies KA, Haskard DO. Induction of decay-accelerating factor by cytokines or the membrane-attack complex protects vascular endothelial cells against complement deposition. Blood. 1999;94:1673–1682. [PubMed] [Google Scholar]
- Safar D, Aime C, Cohen-Kaminsky S, Berrih-Aknin S. Antibodies to thymic epithelial cells in myasthenia gravis. J Neuroimmunol. 1991;35:101–110. doi: 10.1016/0165-5728(91)90165-4. [DOI] [PubMed] [Google Scholar]
- Kyewski B, Klein L. A central role for central tolerance. Annu Rev Immunol. 2006;24:571–606. doi: 10.1146/annurev.immunol.23.021704.115601. [DOI] [PubMed] [Google Scholar]
- Daveau M, Benard M, Scotte M, Schouft MT, Hiron M, Francois A, Salier JP, Fontaine M. Expression of a functional C5a receptor in regenerating hepatocytes and its involvement in a proliferative signaling pathway in rat. J Immunol. 2004;173:3418–3424. doi: 10.4049/jimmunol.173.5.3418. [DOI] [PubMed] [Google Scholar]
- Fosbrink M, Niculescu F, Rus V, Shin ML, Rus H. C5b-9-induced endothelial cell proliferation and migration are dependent on Akt inactivation of forkhead transcription factor FOXO1. J Biol Chem. 2006;281:19009–19018. doi: 10.1074/jbc.M602055200. [DOI] [PubMed] [Google Scholar]
- Rus HG, Niculescu FI, Shin ML. Role of the C5b-9 complement complex in cell cycle and apoptosis. Immunol Rev. 2001;180:49–55. doi: 10.1034/j.1600-065x.2001.1800104.x. [DOI] [PubMed] [Google Scholar]
- Cole DS, Morgan BP. Beyond lysis: how complement influences cell fate. Clin Sci (Lond) 2003;104:455–466. doi: 10.1042/CS20020362. [DOI] [PubMed] [Google Scholar]
- Dashiell SM, Rus H, Koski CL. Terminal complement complexes concomitantly stimulate proliferation and rescue of Schwann cells from apoptosis. Glia. 2000;30:187–198. doi: 10.1002/(sici)1098-1136(200004)30:2<187::aid-glia8>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Lin F, Kaminski HJ, Conti-Fine BM, Wang W, Richmonds C, Medof ME. Markedly enhanced susceptibility to experimental autoimmune myasthenia gravis in the absence of decay-accelerating factor protection. J Clin Invest. 2002;110:1269–1274. doi: 10.1172/JCI16086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski HJ, Kusner LL, Richmonds C, Medof ME, Lin F. Deficiency of decay accelerating factor and CD59 leads to crisis in experimental myasthenia. Exp Neurol. 2006;202:287–293. doi: 10.1016/j.expneurol.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Morgan BP, Chamberlain-Banoub J, Neal JW, Song W, Mizuno M, Harris CL. The membrane attack pathway of complement drives pathology in passively induced experimental autoimmune myasthenia gravis in mice. Clin Exp Immunol. 2006;146:294–302. doi: 10.1111/j.1365-2249.2006.03205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski HJ, Li Z, Richmonds C, Lin F, Medof ME. Complement regulators in extraocular muscle and experimental autoimmune myasthenia gravis. Exp Neurol. 2004;189:333–342. doi: 10.1016/j.expneurol.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Navenot JM, Villanova M, Lucas-Heron B, Malandrini A, Blanchard D, Louboutin JP. Expression of CD59, a regulator of the membrane attack complex of complement, on human skeletal muscle fibers. Muscle Nerve. 1997;20:92–96. doi: 10.1002/(sici)1097-4598(199701)20:1<92::aid-mus12>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Gasque P, Neal JW, Singhrao SK, McGreal EP, Dean YD, Van BJ, Morgan BP. Roles of the complement system in human neurodegenerative disorders: pro-inflammatory and tissue remodeling activities. Mol Neurobiol. 2002;25:1–17. doi: 10.1385/mn:25:1:001. [DOI] [PubMed] [Google Scholar]
- Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI, Hageman JL, Stockman HA, Borchardt JD, Gehrs KM, Smith RJ, Silvestri G, Russell SR, Klaver CC, Barbazetto I, Chang S, Yannuzzi LA, Barile GR, Merriam JC, Smith RT, Olsh AK, Bergeron J, Zernant J, Merriam JE, Gold B, Dean M, Allikmets R. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA. 2005;102:7227–7232. doi: 10.1073/pnas.0501536102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLennan IC. Germinal centers. Annu Rev Immunol. 1994;12:117–139. doi: 10.1146/annurev.iy.12.040194.001001. [DOI] [PubMed] [Google Scholar]
- Sims GP, Shiono H, Willcox N, Stott DI. Somatic hypermutation and selection of B cells in thymic germinal centers responding to acetylcholine receptor in myasthenia gravis. J Immunol. 2001;167:1935–1944. doi: 10.4049/jimmunol.167.4.1935. [DOI] [PubMed] [Google Scholar]
- Matthews I, Sims G, Ledwidge S, Stott D, Beeson D, Willcox N, Vincent A. Antibodies to acetylcholine receptor in parous women with myasthenia: evidence for immunization by fetal antigen. Lab Invest. 2002;82:1407–1417. doi: 10.1097/01.lab.0000032379.63784.9c. [DOI] [PubMed] [Google Scholar]
- Graus YF, de Baets MH, Parren PW, Berrih-Aknin S, Wokke J, van Breda Vriesman PJ, Burton DR. Human anti-nicotinic acetylcholine receptor recombinant Fab fragments isolated from thymus-derived phage display libraries from myasthenia gravis patients reflect predominant specificities in serum and block the action of pathogenic serum antibodies. J Immunol. 1997;158:1919–1929. [PubMed] [Google Scholar]
- Leite M, Cossins J, Clover L, Beeson D, Willcox N, Vincent A: Antibodies to clustered AChR and thymic changes in seronegative myasthenia gravis (abstract). J Neurol Neurosurg Psychiatry (in press) [Google Scholar]
- Vincent A, Lang B, International Seronegative Myasthenia Gravis Survey The prevalence of MuSK antibody positive myasthenia gravis worldwide. J Neuroimmunol. 2006;178:233. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.