Abstract
Objective To investigate the benefit of adding acupuncture to a course of advice and exercise delivered by physiotherapists for pain reduction in patients with osteoarthritis of the knee.
Design Multicentre, randomised controlled trial.
Setting 37 physiotherapy centres accepting primary care patients referred from general practitioners in the Midlands, United Kingdom.
Participants 352 adults aged 50 or more with a clinical diagnosis of knee osteoarthritis.
Interventions Advice and exercise (n=116), advice and exercise plus true acupuncture (n=117), and advice and exercise plus non-penetrating acupuncture (n=119).
Main outcome measures The primary outcome was change in scores on the Western Ontario and McMaster Universities osteoarthritis index pain subscale at six months. Secondary outcomes included function, pain intensity, and unpleasantness of pain at two weeks, six weeks, six months, and 12 months.
Results Follow-up rate at six months was 94%. The mean (SD) baseline pain score was 9.2 (3.8). At six months mean reductions in pain were 2.28 (3.8) for advice and exercise, 2.32 (3.6) for advice and exercise plus true acupuncture, and 2.53 (4.2) for advice and exercise plus non-penetrating acupuncture. Mean differences in change scores between advice and exercise alone and each acupuncture group were 0.08 (95% confidence interval −1.0 to 0.9) for advice and exercise plus true acupuncture and 0.25 (−0.8 to 1.3) for advice and exercise plus non-penetrating acupuncture. Similar non-significant differences were seen at other follow-up points. Compared with advice and exercise alone there were small, statistically significant improvements in pain intensity and unpleasantness at two and six weeks for true acupuncture and at all follow-up points for non-penetrating acupuncture.
Conclusion The addition of acupuncture to a course of advice and exercise for osteoarthritis of the knee delivered by physiotherapists provided no additional improvement in pain scores. Small benefits in pain intensity and unpleasantness were observed in both acupuncture groups, making it unlikely that this was due to acupuncture needling effects.
Trial registration Current Controlled Trials ISRCTN88597683.
Introduction
Knee pain in older adults is a common disabling problem, managed in the United Kingdom mostly within primary care.1 Osteoarthritis is the most likely underlying diagnosis and has been shown by radiography to be present in 70% of community dwelling adults aged 50 or more with knee pain.2 Structural changes before radiography are common in the remainder.3 Practice guidelines from the United Kingdom and mainland Europe emphasise the role of education, exercise, and drugs.4 5 6 The recommendations for exercise are underpinned by clinical trials.7 8 9 A recent best evidence summary of systematic reviews concluded that exercise therapy (strengthening, stretching, and functional exercises) compared with no treatment is effective for patients with knee osteoarthritis.10 Long term use of oral non-steroidal inflammatory drugs is discouraged11 and studies show that patients generally do not like taking drugs.12 People with knee osteoarthritis want non-pharmacological options for pain relief13 and often choose complementary medicine.14
The concept of integrated health care that incorporates conventional and complementary therapies has been promoted.15 Between 30% and 40% of general practices in England provide access to some form of complementary therapy for their patients,16 and acupuncture is one of the most popular options. Each week about 10% of general practitioners refer patients to acupuncture, or practise it themselves.16 More than 10% of chartered physiotherapists in the United Kingdom (n=4300) are members of an acupuncture group (personal communication, business manager of the Acupuncture Association of Chartered Physiotherapists, January 2007). Despite growing enthusiasm to provide complementary therapy within the UK National Health Service framework and the positive consensus statement from the National Institutes of Health,17 the place of acupuncture within mainstream health care remains controversial. Clinical trials of acupuncture have been criticised for small sample sizes, inadequate blinding, and lack of credible sham controls and long term follow-up.18 19 20 21 Recent trials have gone some way to tackling these limitations22 23 24 25 26 and systematic reviews conclude that acupuncture is more effective than placebo for osteoarthritis of the knee.20 21 However, questions about the benefit of adding acupuncture to mainstream, recommended treatments for this population remain unanswered. We have shown that exercise based physiotherapy is more effective than usual primary care for older adults with knee pain,9 but no high quality trial has investigated the additional benefit of integrating acupuncture with a recommended treatment such as exercise based physiotherapy for this population. Since physiotherapists, in addition to providing exercise and advice, are one of the largest groups of acupuncture providers within the National Health Service, they are an appropriate group with whom to investigate the effectiveness of integrating acupuncture into mainstream health care.
We carried out a prospective randomised controlled trial within primary care to investigate whether acupuncture is a useful adjunct to exercise based physiotherapy for knee pain in older adults.
Methods
Full details of the methods, recruitment, and outcome measures have been published.27 Participants were recruited from 37 NHS physiotherapy centres providing services for general practices within the Midlands and Cheshire regions of the United Kingdom between November 2003 and October 2005. Adults aged 50 years or more with knee pain and a clinical diagnosis of knee osteoarthritis were invited to participate. They were referred to physiotherapy by their general practitioner between November 2003 and October 2005 and they had not had acupuncture previously.
We screened referral letters and sent potential participants information leaflets about the study by post. They were subsequently telephoned to make an appointment, further explain the study, confirm eligibility, and obtain consent to participate. The leaflet explained that participants would receive physiotherapy advice and exercise and “may receive acupuncture, using one of two different types of acupuncture needle” without specifying the needles' mode of action (penetrating compared with non-penetrating) to maximise the effectiveness of blinding. After consent had been obtained the study nurse carried out a baseline research assessment. Participants then received an initial physiotherapy assessment during which affected knees were examined and conditions other than osteoarthritis (for example, referred pain from the hip or back) were ruled out. Potential acupuncture points were selected and recorded on a form. The first session of advice and exercise was delivered. After this the physiotherapist telephoned an administrator at the research centre to record the selected acupuncture points and to receive a computed generated randomisation group for the patient. This process ensured that the selection of initial acupuncture points, the assessment, and the first advice and exercise session were carried out blind to subsequent treatment allocation.
Using random permuted blocks of 12 (blocked by treatment centre) the participants were randomised to advice and exercise, advice and exercise plus true acupuncture, or advice and exercise plus non-penetrating acupuncture. Researchers who collected, entered, and analysed data were unaware of treatment allocation. By necessity the physiotherapists delivering the interventions were not blind to allocation.
Interventions
Interventions were delivered within 10 working days of randomisation by 67 physiotherapists trained in acupuncture to at least minimum national standards for membership of the Acupuncture Association of Chartered Physiotherapists. Two thirds of the physiotherapists had been qualified for more than 10 years and over half had been using acupuncture for more than three years. The treatment procedures were agreed and the use of the non-penetrating needle28 standardised during training before the trial.
Advice and exercise
Participants allocated to the advice and exercise group received advice supplemented by a leaflet modelled on the Arthritis Research Campaign leaflet on knee osteoarthritis (www.arc.org.uk). Participants who were receiving non-steroidal anti-inflammatory drugs were permitted to continue with their stable dose. The advice and exercise package was developed from reviews of best evidence, clinical guidelines, a survey of physiotherapy practice for knee pain,29 and a consensus workshop. Exercises were individualised using PhysioTools (www.physiotools.net), oriented towards lower limb strengthening, stretching, and balance. This could include concentric, eccentric, and isometric exercise; non-weight bearing exercise; and weight bearing exercise plus a home exercise programme. Intensity was progressed, when appropriate, at each supervised exercise session. The package consisted of up to six sessions of 30 minutes (including the prerandomisation session) over six weeks. Data on participants' self reported adherence to exercise were collected.
Advice and exercise plus true acupuncture
Participants allocated to advice and exercise plus true acupuncture received acupuncture on traditional Chinese acupuncture points. The acupuncture protocol was based on the concept of adequacy of treatment,21 survey results,30 a consensus workshop, and recommendations from traditional Chinese protocols. We did not allow moxibustion, cupping, herbs, or electroacupuncture. For each individualised treatment session between six and 10 acupuncture points from 16 commonly used local and distal points were selected. Local points were Sp 9, Sp 10, St 34, St 35, St 36, Xiyan, Gb 34, and trigger points. Distal points were LI 4, TH 5, Sp 6, Liv 3, St 44, Ki 3, BI 60, and Gb 41. Sterilised disposable steel needles (30×0.3 mm) were used; the depth of insertion was between 5 mm and 25 mm, depending on the points selected. Needles were manipulated to achieve the de qi sensation (for example, aching, warm or tingling sensation) and the therapists recorded the sensations that patients reported. The protocol permitted 25 to 35 minutes between insertion of the last needle and stopping treatment. The therapists revisited and manipulated the needles as appropriate. If the de qi sensation was no longer present the therapists were expected to use stronger manipulation, either rotation or thrust and withdraw techniques, to elicit it. In addition to the prerandomisation advice and exercise session the package consisted of up to six treatment sessions over three weeks, during which both the true acupuncture and the advice and exercise treatments were delivered.
Advice and exercise plus non-penetrating acupuncture
Participants randomised to receive advice and exercise plus non-penetrating acupuncture28 had acupuncture delivered through needles with a blunt tip. The shaft of these needles collapses into the handle, creating an illusion of insertion. They meet the recommendations for acceptable controls for acupuncture research18 and have been used in previous trials.22 31 Some authors believe that a small acupressure effect may be induced by this method.31 The same protocol was used as for true acupuncture, thus all criteria for harnessing non-specific effects were included (same contact time and interaction between therapist and patient, manual contact during the search for acupuncture points, and attention to elicited sensations). No attempt was made to elicit the de qi sensation but participants were told they may experience sensations and to report what they felt. In addition to the prerandomisation advice and exercise session the package consisted of up to six treatment sessions over three weeks, during which both the non-penetrating acupuncture and the advice and exercise treatments were delivered.
Outcomes
Full details of the outcome measures are published elsewhere.27 Follow-up was at two weeks (by telephone), six weeks, and six and 12 months (by postal questionnaire) after randomisation. The primary outcome measure was change at six months in the pain subscale score of the Western Ontario and McMaster Universities osteoarthritis index (Likert 3.0).32 This subscale has been shown to be reliable for use within postal surveys.33 Secondary outcomes at six months included the function subscale score of the Western Ontario and McMaster Universities osteoarthritis index, participants' global assessment of change compared with baseline, pain severity and unpleasantness, severity of patient nominated main functional problem, arthritis self efficacy, satisfaction with care, and adherence with exercises, and all measures at six weeks and 12 months. Side effects of treatment, adverse events, and use of cointerventions were also recorded. We identified the proportion of each group who achieved a clinically significant response according to criteria from the outcome measures in Rheumatology and Osteoarthritis Research Society international initiative (OMERACT-OARSI).34 35
Physiotherapists recorded the number and duration of treatment sessions, the exercises prescribed, the location and number of acupuncture points (when applicable), and any adverse reactions. In the acupuncture groups, therapists recorded the sensations that participants reported. This information was subsequently categorised by four acupuncture experts (three independent of the study team), blinded to treatment allocation, to identify those most likely to represent the de qi sensation. Acceptability and credibility of the intervention groups were evaluated during a telephone call two weeks after the start of treatment and at six weeks by questionnaire, using items adapted from previous literature.36
Statistical analysis
We assumed a 45% improvement in pain measured by the pain subscale at six months in participants randomised to the advice and exercise group. The sample size calculation was based on the ability to detect a 65% improvement in the two groups also receiving acupuncture (an additional improvement of 20%).37 A minimum of 270 participants with data at six months would be sufficient to detect these effects with 80% power at a 5% significance level (two tailed).38 To allow for dropouts we inflated this value by 30% and hence aimed to randomise 350 participants.
Analysis was by intention to treat. Estimates of the treatment effects for numerical data are presented as difference in mean change, with 95% confidence intervals (advice and exercise plus acupuncture groups minus advice and exercise alone group) and χ2 tests (heterogeneity test for binary data or linear trend test for ordinal data). We carried out exploratory sensitivity analyses of the mean pain subscale scores by adjusting for baseline characteristics using multiple linear regression. A priori subgroup analyses included comparing those participants in the advice and exercise plus true acupuncture group who had 50% or more treatment sessions in which the de qi sensation was elicited with those with less than 50%, and comparing the effect of treatment in those who had severe knee pain or disability at baseline. External validity was assessed by comparing demographic characteristics of patients not randomised with those of participants and the participants' recruitment characteristics and treatment allocation across high and low recruiting centres.
ET carried out statistical analyses using Stata 7.0. The trial was monitored by an independent steering and data monitoring committee and no interim analyses were undertaken.
Results
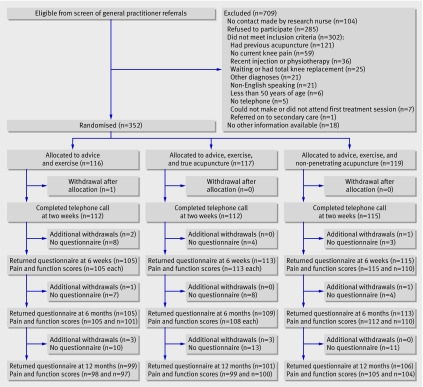
Overall, 1061 potentially eligible participants were identified, of whom 709 (66.8%) were ineligible or did not want to participate (figure). In total 352 (33.2%) patients were randomised: 116 to advice and exercise, 117 to advice and exercise plus true acupuncture, and 119 to advice and exercise plus non-penetrating acupuncture. Thirty seven physiotherapy centres recruited at least one patient (maximum 29 per site). Baseline characteristics of participants (mean age 63 years, 61% women) were similar between the groups (table 1).
Flow of participants through trial
Table 1.
Baseline characteristics of participants, by treatment group. Values are numbers (percentages) of participants unless stated otherwise
| Variables | Advice and exercise (n=116) | Advice, exercise, and true acupuncture (n=117) | Advice, exercise, and non-penetrating acupuncture (n=119) |
|---|---|---|---|
| Personal details | |||
| Mean (SD) age (years) | 63.8 (8.3) | 63.1 (8.7) | 62.8 (9.4) |
| Women | 79 (68) | 71 (61) | 66 (55) |
| Body mass index: | |||
| Underweight or normal (<25.0) | 26 (22) | 25 (22) | 22 (18) |
| Overweight (25.0-29.9) | 55 (47) | 54 (47) | 49 (41) |
| Obese (>29.9) | 35 (30) | 35 (31) | 48 (40) |
| Socioeconomic classification*: | |||
| Higher managerial or professional | 9 (9) | 11 (10) | 9 (9) |
| Lower managerial or professional | 19 (18) | 20 (18) | 18 (16) |
| Intermediate occupations | 22 (21) | 15 (14) | 20 (17) |
| Self employed | 5 (5) | 10 (9) | 8 (7) |
| Lower supervisory or technical | 3 (3) | 6 (5) | 11 (10) |
| Semiroutine occupations | 23 (22) | 29 (26) | 29 (25) |
| Routine occupations | 24 (23) | 19 (17) | 20 (17) |
| Currently employed | 37 (32) | 53 (45) | 48 (40) |
| Knee pain and function | |||
| Mean (SD) pain score† | 9.1 (3.7) | 9.3 (4.0) | 8.9 (3.3) |
| Mean (SD) function score† | 29.0 (12.9) | 30.8 (13.9) | 31.1 (12.8) |
| Total duration of knee pain (years): | |||
| <1 | 47 (41) | 53 (45) | 48 (40) |
| 1 to <5 | 38 (33) | 41 (35) | 35 (29) |
| 5 to <10 | 14 (12) | 8 (6) | 18 (15) |
| ≥10 | 17 (15) | 15 (13) | 18 (15) |
| Onset of current problem: | |||
| Sudden | 54 (47) | 51 (44) | 55 (46) |
| Gradual | 62 (53) | 66 (56) | 64 (54) |
| Mean (SD) pain severity in past 7 days‡ | 5.6 (2.2) | 6.0 (2.3) | 6.1 (2.1) |
| Mean (SD) pain unpleasantness in past 7 days‡ | 5.6 (2.3) | 6.0 (2.4) | 6.2 (2.2) |
| Mean (SD) severity of main problem‡ | 6.3 (2.1) | 6.3 (2.1) | 6.5 (2.0) |
| Self efficacy and drugs | |||
| Mean (SD) pain§ | 29.0 (9.4) | 27.2 (8.6) | 27.3 (9.0) |
| Mean (SD) other symptoms§ | 36.3 (10.5) | 34.5 (10.8) | 33.7 (9.9) |
| Used drugs: | |||
| Non-steroidal anti-inflammatory drugs | 55 (47) | 57 (49) | 63 (53) |
| Analgesia | 49 (42) | 49 (42) | 49 (41) |
Not all numbers add up to totals owing to missing data.
*Office for National Statistics.39 40
†Western Ontario and McMaster Universities osteoarthritis index.
‡Numerical rating scale (0-10).
§Arthritis self efficacy scale.
Those patients who were screened but not randomised (n=709) were slightly older than those randomised (65 v 63 years), but both groups had 61% of women. Treatment allocation and recruitment characteristics were similar between the higher (≥18 patients; n=177 patients) and the lower (≤17 patients; n=175 patients) recruiting centres (data not shown).
Four participants in the advice and exercise group and two in the advice and exercise plus non-penetrating acupuncture group withdrew permission for further contact in the period up to the six months' follow-up. In the 346 eligible for contact at six months the response rate was 94% for advice and exercise, 93% for advice and exercise plus true acupuncture, and 97% for advice and exercise plus non-penetrating acupuncture. Nineteen participants did not return the questionnaire at six months. Non-responders were more likely to be men (47% v 39%), to be younger (mean age 60 v 63 years), and to have slightly lower baseline scores for pain and function (pain: 8.7 v 9.2, function: 27.8 v 30.5).
Treatments were in line with the study protocols. A few participants violated the protocol: three in the advice and exercise group and two in the advice and exercise plus non-penetrating acupuncture group. No adverse events occurred in the advice and exercise group or in the advice and exercise plus non-penetrating acupuncture group. Five adverse events were reported for participants receiving true acupuncture (pain, sleepiness, fainting, nausea, and swelling around the treated knee).
The median (range) number of treatment sessions was in line with the study protocols: 6 (1-9) in the advice and exercise group, 7 (4-9) in the advice and exercise plus true acupuncture group, and 7 (1-8) in the advice and exercise plus non-penetrating acupuncture group. In both acupuncture groups the acupuncture treatment was used in a median of six sessions. The de qi sensation was reported at least once for 95 (83%) participants receiving true acupuncture and 65 (55%) receiving non-penetrating acupuncture. Of these, 67 (71%) and 29 (45%) reported de qi during at least half of their treatment sessions.
Intervention credibility and exercise compliance
Table 2 summarises treatment credibility two weeks after treatment started. Participants receiving either acupuncture intervention were significantly more confident that treatment could help their knee problem than those receiving advice and exercise alone.
Table 2.
Outcome and credibility of treatment* at two weeks. Values are numbers (percentages) of participants
| Patient's response | Advice and exercise (n=112) | Advice, exercise, and true acupuncture (n=112) | P value (χ2 test for trend)† | Advice, exercise, and non-penetrating acupuncture (n=115) | P value (χ2 test for trend)‡ |
|---|---|---|---|---|---|
| Confident that treatment can help problem?: | |||||
| Very | 26 (23) | 27 (24) | 0.01 | 38 (33) | 0.0001 |
| Quite | 44 (39) | 64 (57) | 60 (53) | ||
| Neither | 18 (16) | 12 (11) | 10 (9) | ||
| Not very | 21 (19) | 7 (6) | 5 (4) | ||
| Not at all | 3 (3) | 2 (2) | 1 (1) | ||
| Missing data | 0 | 0 | 1 | ||
| Recommend treatment to friend with similar knee problem?: | |||||
| Very confident | 29 (26) | 34 (30) | 0.2 | 41 (36) | 0.03 |
| Quite confident | 61 (54) | 58 (52) | 62 (54) | ||
| Neither | 8 (7) | 15 (13) | 4 (4) | ||
| Not very confident | 12 (11) | 5 (4) | 5 (4) | ||
| Not at all confident | 2 (2) | 0 (0) | 2 (2) | ||
| Missing data | 0 | 0 | 1 | ||
| Does treatment make sense to you?: | |||||
| Very logical | 46 (41) | 32 (29) | 0.006 | 45 (39) | 0.4 |
| Quite logical | 53 (47) | 54 (48) | 51 (45) | ||
| No opinion | 5 (4) | 6 (5) | 4 (4) | ||
| Not very logical | 7 (6) | 18 (16) | 13 (11) | ||
| Not at all logical | 1 (1) | 2 (2) | 1 (1) | ||
| Missing data | 0 | 0 | 1 | ||
| Do you think treatment would be successful in treating other problems? | |||||
| Very | 17 (15) | 17 (15) | 0.3 | 29 (25) | 0.03 |
| Quite | 61 (55) | 68 (61) | 56 (49) | ||
| No opinion | 27 (24) | 25 (22) | 29 (25) | ||
| Not very | 5 (5) | 1 (1) | 0 (0) | ||
| Not at all | 2 (2) | 1 (1) | 0 (0) | ||
| Missing data | 0 | 0 | 1 |
*Adapted from Vincent and Lewith.36
†Advice and exercise compared with advice, exercise, and true acupuncture.
‡Advice and exercise compared with advice, exercise, and non-penetrating acupuncture.
Most participants had treatment sessions that included supervised exercises (85% for advice and exercise, 77% for advice and exercise plus true acupuncture, and 78% for advice and exercise plus non-penetrating acupuncture) and a home exercise programme (89%, 91%, and 95%). Self reported compliance with exercise at two weeks was 63%, 70%, and 64% (table 3). Compliance remained above 50% in each group over the 12 months' follow-up.
Table 3.
Compliance with exercise at two weeks. Values are numbers (percentages) of participants unless stated otherwise
| Variable | Advice and exercise (n=112) | Advice, exercise, and true acupuncture (n=112) | P value* (χ2 test for trend) | Advice, exercise, and non-penetrating acupuncture (n=115) | P value† (χ2 test for trend) |
|---|---|---|---|---|---|
| I have been doing my exercises as often as advised: | |||||
| Strongly agree | 35 (32) | 41 (37) | 0.2 | 44 (39) | 0.7 |
| Agree | 34 (31) | 37 (33) | 27 (24) | ||
| Not sure | 0 (0) | 2 (2) | 0 (0) | ||
| Disagree | 40 (36) | 31 (28) | 41 (36) | ||
| Strongly disagree | 2 (2) | 1 (1) | 2 (2) | ||
| Missing data | 1 | 0 | — | 1 | — |
*Advice and exercise compared with advice, exercise, and true acupuncture.
†Advice and exercise compared with advice, exercise, and non-penetrating acupuncture.
Outcome measures
At six months no statistically significant differences were found in change on the pain subscale from baseline between the groups receiving acupuncture in addition to advice and exercise compared with the group receiving advice and exercise alone (table 4).
Table 4.
Change in pain and function scores.* Values are means (standard deviations) unless stated otherwise
| Advice and exercise | Advice, exercise, and true acupuncture | Mean difference† (95% CI) | P value‡ | Advice, exercise, and non-penetrating acupuncture | Mean difference† (95% CI) | P value‡ | |
|---|---|---|---|---|---|---|---|
| Pain | |||||||
| Six weeks: | |||||||
| No analysed | 105 | 113 | 115 | ||||
| Absolute score | 6.86 (4.2) | 6.38 (4.1) | 5.98 (4.3) | ||||
| Crude change score§ | 2.10 (3.5) | 2.83 (4.0) | 0.74 (−0.3 to 1.7) | 0.1 | 3.02 (3.6) | 0.93 (0.0 to 1.9) | 0.05 |
| Adjusted change score¶ | 0.69 (−0.2 to 1.6) | 0.1 | 0.88 (0.0 to 1.8) | 0.06 | |||
| Six months: | |||||||
| No analysed | 105 | 108 | 112 | ||||
| Absolute score | 6.78 (4.5) | 7.07 (4.4) | 6.50 (4.8) | ||||
| Crude change score§ | 2.28 (3.8) | 2.32 (3.6) | 0.04 (−1.0 to 1.0) | 0.9 | 2.53 (4.2) | 0.25 (−0.8 to 1.3) | 0.6 |
| Adjusted change score¶ | −0.08 (−1.0 to 0.9) | 0.9 | 0.25 (−0.8 to 1.3) | 0.6 | |||
| 12 months: | |||||||
| No analysed | 98 | 99 | 105 | ||||
| Absolute score | 6.29 (4.7) | 6.84 (4.7) | 6.16 (4.8) | ||||
| Crude change score§ | 2.57 (4.3) | 2.37 (4.2) | −0.20 (−1.4 to 1.0) | 0.7 | 2.82 (4.1) | 0.25 (−0.9 to 1.4) | 0.7 |
| Adjusted change score¶ | −0.42 (−1.5 to 0.7) | 0.5 | 0.23 (−0.9 to 1.3) | 0.7 | |||
| Function | |||||||
| Six weeks: | |||||||
| No analysed | 105 | 113 | 110 | ||||
| Absolute score | 22.34 (14.9) | 22.38 (14.5) | 22.14 (15.7) | ||||
| Crude change score§ | 6.21 (11.4) | 8.18 (11.5) | 1.97 (−1.1 to 5.0) | 0.2 | 9.32 (11.4) | 3.11 (0.0 to 6.2) | 0.05 |
| Adjusted change score¶ | 1.46 (−1.5 to 4.4) | 0.3 | 2.49 (−0.6 to 5.5) | 0.1 | |||
| Six months: | |||||||
| No analysed | 101 | 108 | 110 | ||||
| Absolute score | 24.36 (15.6) | 24.93 (16.0) | 23.83 (16.9) | ||||
| Crude change score§ | 4.60 (11.4) | 6.25 (12.1) | 1.66 (−1.5 to 4.9) | 0.3 | 7.13 (13.1) | 2.54 (−0.8 to 5.9) | 0.1 |
| Adjusted change score¶ | 0.92 (−2.2 to 4.0) | 0.6 | 2.39 (−0.9 to 5.6) | 0.2 | |||
| 12 months: | |||||||
| No analysed | 97 | 100 | 104 | ||||
| Absolute score | 23.16 (15.8) | 23.83 (16.5) | 22.47 (16.7) | ||||
| Crude change score§ | 5.36 (11.9) | 6.61 (13.8) | 1.24 (−2.3 to 4.5) | 0.5 | 8.24 (13.5) | 2.87 (−0.7 to 6.4) | 0.1 |
| Adjusted change score¶ | 0.23 (−3.2 to 3.6) | 0.9 | 2.52 (−0.9 to 6.0) | 0.2 | |||
*Scores on Western Ontario and McMaster Universities osteoarthritis index.
†Difference in mean scores (advice and exercise plus acupuncture group minus advice and exercise group).
‡Derived from linear regression.
§Change in score from baseline.
¶Mean difference adjusted for recruitment age, sex, duration of pain, and scores for pain or function.
At six weeks the advice and exercise plus non-penetrating acupuncture group reported small but significantly greater improvements in pain than did the advice and exercise group (mean difference 0.88, 95% confidence interval 0.0 to 1.8). At 12 months no statistically significant differences were found between the groups (table 4). At two weeks statistically significant trends were found in favour of better global outcome for each of the acupuncture groups compared with the advice and exercise alone group (table 5).
Table 5.
Global assessment at follow-up. Values are numbers (percentages) of participants unless stated otherwise
| Variables | Advice and exercise | Advice, exercise, and true acupuncture | P value* (χ2 test for trend) | Advice, exercise, and non-penetrating acupuncture | P value† (χ2 test for trend) |
|---|---|---|---|---|---|
| Two weeks: | |||||
| Much better | 14 (13) | 25 (22) | 0.02 | 29 (25) | 0.008 |
| Better | 55 (49) | 58 (52) | 53 (46) | ||
| No change | 34 (30) | 25 (22) | 28 (25) | ||
| Worse | 7 (6) | 2 (2) | 4 (4) | ||
| Much worse | 2 (2) | 2 (2) | 0 (0) | ||
| Missing data | 0 | 0 | 1 | ||
| Six weeks: | |||||
| Complete recovery | 4 (4) | 1 (1) | 4 (4) | ||
| Much better | 25 (24) | 33 (30) | 0.3 | 42 (37) | 0.2 |
| Better | 42 (40) | 52 (46) | 36 (32) | ||
| No change | 24 (23) | 23 (21) | 25 (22) | ||
| Worse | 8 (8) | 2 (2) | 5 (4) | ||
| Much worse | 1 (1) | 1 (1) | 2 (2) | ||
| Missing data | 1 | 1 | 1 | ||
| Six months: | |||||
| Complete recovery | 4 (4) | 3 (3) | 6 (5) | ||
| Much better | 24 (23) | 23 (21) | 0.9 | 38 (34) | 0.2 |
| Better | 28 (27) | 33 (31) | 23 (21) | ||
| No change | 33 (31) | 33 (31) | 29 (26) | ||
| Worse | 12 (11) | 12 (11) | 13 (12) | ||
| Much worse | 4 (4) | 4 (4) | 3 (3) | ||
| Missing data | 0 | 1 | 1 | ||
| 12 months: | |||||
| Complete recovery | 11 (11) | 4 (4) | 5 (5) | ||
| Much better | 19 (19) | 20 (20) | 0.7 | 31 (29) | 0.8 |
| Better | 21 (21) | 39 (39) | 26 (25) | ||
| No change | 30 (30) | 15 (15) | 25 (24) | ||
| Worse | 12 (12) | 17 (17) | 14 (13) | ||
| Much worse | 6 (6) | 6 (6) | 5 (5) | ||
| Missing data | 0 | 0 | 0 |
*Advice and exercise compared with advice, exercise, and true acupuncture.
†Advice and exercise compared with advice, exercise, and non-penetrating acupuncture.
No other statistically significant differences were found in the changes in function scores, global assessment, or response status according to the OMERACT-OARSI criteria between the three groups at any follow-up points, or in the adjusted analyses (tables 5 and 6).
Table 6.
Response to criteria from the outcome measures in Rheumatology and Osteoarthritis Research Society international initiative at follow-up. Values are numbers (percentages) of participants unless stated otherwise
| Variables | Advice and exercise | Advice, exercise, and true acupuncture | P value* (χ2 test for trend) | Advice, exercise, and non-penetrating acupuncture | P value† (χ2 test for trend) |
|---|---|---|---|---|---|
| Six weeks: | |||||
| High | 30 | 39 | 0.1 | 51 | 0.1 |
| Improvement | 24 | 31 | 20 | ||
| Total response | 54 (51) | 70 (62) | 71 (62) | ||
| Six months: | |||||
| High | 31 | 29 | 0.4 | 38 | 0.2 |
| Improvement | 14 | 26 | 21 | ||
| Total response | 45 (43) | 55 (50) | 59 (52) | ||
| 12 months: | |||||
| High | 37 | 31 | 0.6 | 41 | 0.3 |
| Improvement | 11 | 22 | 18 | ||
| Total response | 48 (48) | 53 (52) | 59 (56) |
*Advice and exercise compared with advice, exercise, and true acupuncture.
†Advice and exercise compared with advice, exercise, and non-penetrating acupuncture.
Statistically significant differences were found between the groups in pain intensity and unpleasantness (table 7). The results at two and six weeks for pain intensity and at six weeks for change in pain unpleasantness favoured both groups receiving acupuncture. The results at six and 12 months for both pain intensity and pain unpleasantness favoured the group receiving advice and exercise plus non-penetrating acupuncture. Satisfaction with care was significantly greater for participants receiving advice and exercise plus non-penetrating acupuncture than for those receiving advice and exercise alone (table 8). No statistically significant differences were seen between advice and exercise plus true acupuncture and advice and exercise plus non-penetrating acupuncture for any other of the outcomes measured (data not shown).
Table 7.
Change in knee pain and function and psychological measures at follow-up. Values are means (standard deviations) unless stated otherwise
| End point | Advice and exercise | Advice, exercise, and true acupuncture | Difference (95% CI)* | P value | Advice, exercise, and non-penetrating acupuncture | Difference (95% CI)* | P value |
|---|---|---|---|---|---|---|---|
| Knee pain and function | |||||||
| Change in pain intensity†: | |||||||
| 2 weeks | 0.27 (2.2) | 1.31 (2.2) | 1.12 (0.5 to 1.7) | <0.0001 | 1.51 (2.1) | 1.24 (0.7 to 1.8) | <0.0001 |
| 6 weeks | 0.90 (2.5) | 1.81 (2.4) | 0.98 (0.3 to 1.6) | 0.004 | 2.18 (2.5) | 1.27 (0.6 to 1.9) | <0.0001 |
| 6 months | 0.95 (2.6) | 1.28 (2.4) | 0.32 (−0.4 to 1.0) | 0.4 | 1.95 (2.6) | 1.01 (0.3 to 1.7) | 0.006 |
| 12 months | 1.21 (2.9) | 1.60 (2.6) | 0.34 (−0.4 to 1.1) | 0.4 | 2.02 (2.6) | 0.84 (0.1 to 1.6) | 0.03 |
| Change in pain unpleasantness†: | |||||||
| 6 weeks | 1.08 (2.5) | 1.91 (2.4) | 0.90 (0.2 to 1.6) | 0.007 | 2.23 (2.5) | 1.09 (0.4 to 1.8) | 0.002 |
| 6 months | 0.94 (2.6) | 1.22 (2.5) | 0.30 (−0.4 to 1.0) | 0.4 | 2.07 (2.8) | 1.12 (0.4 to 1.9) | 0.003 |
| 12 months | 1.20 (3.0) | 1.66 (2.8) | 0.43 (−0.4 to 1.2) | 0.3 | 2.15 (2.8) | 0.94 (0.2 to 1.7) | 0.02 |
| Change in severity of main problem†: | |||||||
| 6 weeks | 1.39 (2.6) | 1.88 (2.4) | 0.58 (−0.1 to 1.3) | 0.09 | 2.13 (2.4) | 0.72 (0.1 to 1.4) | 0.04 |
| 6 months | 1.13 (2.7) | 1.23 (2.5) | 0.12 (−0.6 to 0.8) | 0.7 | 1.76 (2.8) | 0.66 (−0.1 to 1.4) | 0.08 |
| 12 months | 1.36 (2.6) | 1.60 (2.7) | 0.15 (−0.6 to 0.9) | 0.7 | 1.89 (2.7) | 0.52 (−0.2 to 1.3) | 0.2 |
| Psychological measures | |||||||
| Change in pain on arthritis self efficacy scale†: | |||||||
| 6 weeks | 0.71 (9.5) | −1.46 (9.3) | −2.19 (−4.8 to 0.4) | 0.1 | −2.54 (10.4) | −2.99 (−5.7 to -0.3) | 0.03 |
| 6 months | 1.64 (11.1) | −0.62 (9.8) | −2.36 (−5.3 to 0.5) | 0.1 | −1.43 (11.3) | −2.77 (−5.9 to 0.3) | 0.08 |
| 12 months | 0.91 (12.1) | 0.33 (12.0) | −0.64 (−4.2 to 2.9) | 0.7 | 0.08 (10.3) | −0.71 (−3.9 to 2.5) | 0.7 |
| Change in other symptoms on arthritis self efficacy scale†: | |||||||
| 6 weeks | −0.32 (10.0) | −1.83 (10.1) | −1.42 (−4.2 to 1.3) | 0.3 | −3.38 (10.4) | −2.74 (−5.5 to 0.02) | 0.05 |
| 6 months | 0.38 (11.2) | −0.68 (11.2) | −1.01 (−4.1 to 2.1) | 0.5 | −1.88 (12.0) | −2.09 (−5.3 to 1.1) | 0.2 |
| 12 months | 0.55 (11.5) | −0.12 (13.9) | −0.47 (−4.2 to 3.3) | 0.8 | −1.93 (11.5) | −2.48 (−5.8 to 0.8) | 0.1 |
*Mean difference (advice and exercise plus acupuncture group minus advice and exercise group) adjusted for recruitment age, sex, and duration of pain.
†Change in score from baseline.
Table 8.
Change in satisfaction with care at follow-up. Values are numbers (percentages) of participants
| Variables | Advice and exercise | Advice, exercise, and true acupuncture | P value* (χ2 test for trend) | Advice, exercise, and non-penetrating acupuncture | P value† (χ2 test for trend) |
|---|---|---|---|---|---|
| Six weeks: | |||||
| Very satisfied | 47 (45) | 62 (55) | 0.07 | 71 (62) | 0.008 |
| Quite satisfied | 39 (37) | 37 (33) | 35 (30) | ||
| No opinion | 10 (10) | 8 (7) | 3 (3) | ||
| Not very satisfied | 8 (7) | 5 (4) | 6 (5) | ||
| Not at all satisfied | 1 (1) | 0 (0) | 0 (0) | ||
| Missing data | 1 | 0 | 0 | ||
| Six months: | |||||
| Very satisfied | 32 (31) | 38 (35) | 0.5 | 56 (50) | 0.006 |
| Quite satisfied | 44 (42) | 46 (43) | 39 (35) | ||
| No opinion | 15 (14) | 11 (10) | 6 (5) | ||
| Not very satisfied | 10 (10) | 11 (10) | 9 (8) | ||
| Not at all satisfied | 3 (3) | 2 (2) | 1 (1) | ||
| Missing data | 1 | 1 | 2 | ||
| 12 months: | |||||
| Very satisfied | 28 (29) | 33 (33) | 0.2 | 47 (44) | 0.009 |
| Quite satisfied | 37 (38) | 45 (45) | 40 (38) | ||
| No opinion | 20 (20) | 12 (12) | 7 (7) | ||
| Not very satisfied | 8 (8) | 9 (9) | 12 (11) | ||
| Not at all satisfied | 5 (5) | 2 (2) | 0 (0) | ||
| Missing data | 1 | 0 | 0 |
*Advice and exercise compared with advice, exercise, and true acupuncture.
†Advice and exercise compared with advice, exercise, and non-penetrating acupuncture.
Exploratory subgroup analyses showed no significant differences in change scores for pain or function between participants in the advice and exercise plus true acupuncture group reporting de qi during more than 50% of treatment sessions compared with those who reported de qi less often. Those with severe pain or disability at baseline showed similar change scores in each of the treatment groups (data not shown). No significant differences were found between groups in the number of reported general practitioner consultations over six months (advice and exercise 25%, advice and exercise plus true acupuncture 19%, and advice and exercise plus non-penetrating acupuncture 20%) or in the use of non-steroidal anti-inflammatory or simple analgesics.
Discussion
Acupuncture delivered by physiotherapists as part of an integrated package of health care with advice and exercise, for older adults with osteoarthritis of the knee, provided no additional improvement in pain scores compared with advice and exercise alone measured on the Western Ontario and McMaster Universities osteoarthritis index at six and 12 months. Small benefits were shown for pain intensity and unpleasantness but these effects were greater and sustained for longer in the group receiving non-penetrating acupuncture than in the group receiving true acupuncture. This finding makes it unlikely that the observed effects were due to needling effects of needle penetration, manual stimulation throughout treatment, and elicitation of the de qi sensation.
Comparison with other studies
Our trial is important for two reasons. Firstly, it provides new information on the effectiveness of acupuncture for knee osteoarthritis in older adults, delivered in addition to an evidence based package of physiotherapy care within mainstream health care. Previous trials of acupuncture for knee osteoarthritis have compared true acupuncture with sham acupuncture (including off-point needling),22 ongoing stable medication,41 waiting list controls,24 or education alone.23 We decided not to include a no treatment group as this would be difficult to justify given that guidelines and previous trials recommend advice and exercise for older adults with knee osteoarthritis. Our procedures differed in several important ways from those in previous trials. We used fewer treatment sessions: six acupuncture treatments compared with 10, 12, 15, and 24 in previous studies.23 24 25 26 Although it can be argued that this may have rendered the true acupuncture intervention suboptimal, we found no differences between true and non-penetrating acupuncture after six treatments. We included participants with a clinical diagnosis of knee osteoarthritis, who are the patients seen in primary care, rather than those with a confirmed radiological diagnosis only, as used in other trials.24 25 26 We also used the credible acupuncture control of non-penetrating acupuncture at the same points as the true acupuncture rather than minimal depth needling at predefined distant non-acupuncture points. There is much debate within the acupuncture literature about the validity of sham acupuncture, and given that a considerable proportion of participants in our non-penetrating acupuncture group reported sensations fitting the normal descriptions of de qi we cannot consider this intervention as inert. Only one high quality trial included physiotherapy in an integrated package with acupuncture.25 In that trial all treatment groups (true acupuncture, minimal needling acupuncture, and conservative therapy consisting of visits to a general practitioner and drugs) could have up to six sessions with a physiotherapist although these were actually received by only a minority of participants. Although procedural differences make direct comparisons between trials difficult, the treatment response in our control group (a course of advice and exercise) was considerably higher (51% at six weeks, 43% at six months, and 48% at 12 months) than in the control groups of previous trials (29%, 6.5%, and 30% at six months or equivalent).23 25 26 Thus it is clear that the course of six sessions of advice plus individualised and supervised exercise in the current trial was considerably more effective than the control interventions used in previous acupuncture studies. We have shown that acupuncture offers limited additional benefits when delivered alongside an effective package of physiotherapy led advice and exercise.
Secondly, this trial adds to the debate about acupuncture's mechanisms of action. Participants were not told they may receive a sham intervention (rather they were told they may receive one of two forms of acupuncture), the credibility of the interventions was high, and participants were not asked to guess the treatment they had received. We have shown that there are no differences when a credible, non-penetrating acupuncture treatment, delivered under strict participant blinded conditions, and true acupuncture, involving needle penetration, manual stimulation, and elicitation of the de qi sensation are added to a course of advice and exercise. Indeed patient satisfaction, credibility of intervention at six weeks, and reduction in pain intensity and unpleasantness were significantly greater for the advice and exercise plus non-penetrating acupuncture group than for the advice and exercise group but not for the advice and exercise plus true acupuncture group. We cannot explain these findings. One possibility is that non-penetrating acupuncture harnesses some of the benefits of acupuncture, such as acupressure or participants' expectations of benefit, without any adverse or unpleasant side effects, such as minor bleeding, bruising, or pain. Our findings make it difficult to sustain the argument that the observed effects of acupuncture are explained by specific physiological mechanisms of needling and eliciting de qi sensations.42 Other possible mechanisms could include placebo effects, effects on the limbic system, light touch stimulating mechanoreceptors thus alleviating pain unpleasantness,43 or patients' expectations of pain relief.44 45 We also excluded other possible explanations of acupuncture's effects suggested by previous trials, such as the intensity of provider contact or the physiological effects of needling. One study showed no difference between true acupuncture over minimal shallow needling for knee osteoarthritis.25 Our trial adds to this important finding by showing no difference between true acupuncture and a non-penetrating acupuncture intervention in patients with no experience of true acupuncture who are expecting to receive acupuncture to help their knee problem.
Strengths and weaknesses of the study
Our trial engaged experienced physiotherapists trained to national standards. The treatment protocols were developed from available evidence, using information about traditional Chinese acupuncture points, previous surveys of practice, and consensus workshops. Treatment could be adjusted according to individual patients' needs within boundaries set and agreed within the treatment protocols. We ensured that treatments met the criteria of adequacy for acupuncture, that many more participants in the true acupuncture group reported the de qi sensation during treatment, and that all adverse reactions were linked to the group receiving the true acupuncture intervention. We had successful concealed randomisation, had sufficient power, excellent follow-up rates, and high adherence to the protocol, achieved good credibility and blinding of participants receiving the non-penetrating acupuncture intervention, and successful blinding of the research team.
A potential limitation of this trial is that we used fewer treatment sessions than in previous studies of acupuncture practice, such as those from the United States23 and Germany.24 25 26 We developed the acupuncture protocols to fit within current physiotherapy practice in the United Kingdom, however, and the protocols met the minimum criteria for adequacy of acupuncture.
Our trial failed to show that acupuncture is a useful adjunct to a course of individualised, exercise based physiotherapy for older adults with knee osteoarthritis. This adds to the existing body of evidence as acupuncture was compared with an effective comparison treatment.
Conclusion
Our trial addressed the three important questions recommended by the House of Lords report on complementary and alternative medicine in 2000.46 Firstly, true acupuncture did not show any greater therapeutic benefit than a credible control procedure in patients with a clinical diagnosis of knee osteoarthritis. Secondly, acupuncture was safe, with few, minor adverse events. Thirdly, acupuncture provided no additional improvement in pain scores compared with a course of six sessions of physiotherapy led advice and exercise. The small additional benefits from acupuncture were unlikely to be clinically significant, were limited to pain intensity and unpleasantness, were mostly short lived, and could not be attributed to specific acupuncture needling effects. Further research is needed to investigate the possible mechanisms of acupuncture, particularly the role of expectancy effects.
What is already known on this topic
Guidelines for the management of knee osteoarthritis emphasise patient education and exercise
Acupuncture alongside mainstream healthcare interventions has been advocated
What this study adds
Acupuncture did not provide greater reduction in pain scores when added to a course of advice and exercise delivered by physiotherapists
Benefits from acupuncture were limited to pain intensity and unpleasantness, were unlikely to be clinically significant, were mostly short lived, and could not be attributed to needling effects
Supplementary Material
We thank Chan Vohora, Hannah Yates, Rhian Hughes, Jo Bailey, Gail White, Sue Weir, Claire Calverley, Wendy Clow, Peter Croft, and Krysia Dziedzic (Primary Care Musculoskeletal Research Centre); the physiotherapists based at the following NHS trusts: Amber Valley Primary Care Trust, South, Eastern, Heart of, and North Birmingham primary care trusts, East and South Staffordshire primary care trusts, Mid Staffordshire General Hospitals NHS Trust, East Cheshire Primary Care Trust, Mid Cheshire Hospitals NHS Trust, East Cheshire NHS Trust, Derby Hospitals NHS Foundation Trust, Worcestershire Acute Hospitals NHS Trust, Shrewsbury and Telford Hospital NHS Trust, Shropshire Community Primary Care Trust, Burton Hospitals NHS Trust, Robert Jones and Agnes Hunt Orthopaedic Hospital NHS Trust, South Warwickshire Primary Care Trust, South Warwickshire Hospitals NHS Trust, North Stoke, and Staffordshire Moorlands primary care trusts; and Adrian White, Michael Cummings, and Hugh MacPherson for categorising patients on the de qi sensation.
Contributors: All authors participated in the interpretation of the results and drafting of the article. NEF contributed to the design, funding application, advice and exercise intervention, training of the therapists, and management of the trial. ET contributed to the outcomes measured, data management, and analysis. PB contributed to the design, funding application, acupuncture interventions, and training of the therapists. JCH and EM contributed to the management of the trial, data collection, and training of the therapists. JY contributed to the recruitment procedures, data collection, and management. EMH contributed to the design, funding application, and management of the trial. NEF and EMH are guarantors.
Funding: This study was supported by a project grant from the Arthritis Research Campaign, UK (grant H0640) and Support for Science funding secured by the North Staffordshire Primary Care Research Consortium for NHS service support costs. NEF is funded by a primary care career scientist award from the Department of Health and NHS research and development, UK. JCH is funded by a lecturership in physiotherapy from the Arthritis Research Campaign, UK.
Competing interests: None declared.
Ethical approval: This study was approved by the West Midlands multicentre research ethics committee and by 13 local ethics committees.
References
- 1.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis—it all depends on your point of view. Rheumatology 2006;45:757-60. [DOI] [PubMed] [Google Scholar]
- 3.Cibere J, Trithart S, Koec JA, Thorne A, Zhang H, Singer J, et al. Pre-radiographic knee osteoarthritis is common in people with knee pain: results from a population-based study. Arthritis Rheum 2005;52(9 suppl):S509 (Abstract). [Google Scholar]
- 4.Primary Care Rheumatology Society. The management of osteoarthritis—guidelines. .www.library.nhs.uk/musculoskeletal/ViewResource.aspx?resID=5317
- 5.Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JWJ, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roddy E, Zhang W, Doherty M, Arden NK, Barlow J, Birrell F, et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee—the MOVE consensus. Rheumatology 2005;44:67-73. [DOI] [PubMed] [Google Scholar]
- 7.Van Baar ME, Assendelft WJJ, Dekker J, Oostendorp RAB, Bijlsma JWJ. Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee. Arthritis Rheum 1999;42:1361-9. [DOI] [PubMed] [Google Scholar]
- 8.Thomas KS, Miller P, Doherty M, Muir KR, Jones AC, O'Reilly SC. Cost-effectiveness of a two-year home exercise program for the treatment of knee pain. Arthritis Rheum 2005;53:388-94. [DOI] [PubMed] [Google Scholar]
- 9.Hay EM, Foster NE, Thomas E, Peat G, Phelan M, Yates HE, et al. Pragmatic randomized clinical trial of the effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in older people presenting to primary care. BMJ 2006;333:995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smidt N, de Vet HCW, Bouter LM, Dekker J. Effectiveness of exercise therapy: a best-evidence summary of systematic reviews. Aust J Physiother 2005;51:71-85. [DOI] [PubMed] [Google Scholar]
- 11.Oxford Pain Site. NSAIDS and adverse effects. Bandolier. .www.jr2.ox.ac.uk/bandolier/booth/painpag/nsae/nsae.html
- 12.Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med 2005;61:133-55. [DOI] [PubMed] [Google Scholar]
- 13.Arthritis Care. Osteoarthritis nation: the most comprehensive UK report of people with osteoarthritis London: Arthritis Care, 2004
- 14.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life and treatment. Eur J Pain 2006;10:287-333. [DOI] [PubMed] [Google Scholar]
- 15.Vickers A. Complementary medicine. BMJ 2000;321:683-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas KJ, Nicholl JP, Fall M. Access to complementary medicine via general practice. Br J Gen Pract 2001;51:25-30. [PMC free article] [PubMed] [Google Scholar]
- 17.NIH Consensus Conference. Acupuncture. JAMA 1998;280:1518-24. [PubMed] [Google Scholar]
- 18.White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complement Ther Med 2001;9:237-45. [DOI] [PubMed] [Google Scholar]
- 19.Derry CJ, Derry S, McQuay HJ, Moore RA. Systematic review of systematic reviews of acupuncture published 1996-2005. Clin Med 2006;6:381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ezzo J, Hadhazy V, Birch S, Lao L, Kaplan G, Hochberg M, et al. Acupuncture for osteoarthritis of the knee: a systematic review. Arthritis Rheum 2001;44:819-25. [DOI] [PubMed] [Google Scholar]
- 21.White AR, Foster NE, Cumming M, Barlas P. Acupuncture for chronic knee pain: a systematic review. Rheumatology 2007;46:384-90. [DOI] [PubMed] [Google Scholar]
- 22.Vas J, Mendez C, Perea-Milla E, Vega E, Panadero MD, Leon JM, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomized controlled trial. BMJ 2004;329:1216-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AMK, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med 2004;141:901-10. [DOI] [PubMed] [Google Scholar]
- 24.Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomized trial. Lancet 2005;366:136-43. [DOI] [PubMed] [Google Scholar]
- 25.Scharf HP, Mansmann U, Streitberger K, Witte S, Kramer J, Maier C, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med 2006;145:12-20. [DOI] [PubMed] [Google Scholar]
- 26.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomised arm. Arthritis Rheum 2006;54:3485-93. [DOI] [PubMed] [Google Scholar]
- 27.Hay E, Barlas P, Foster N, Hill J, Thomas E, Young J. Is acupuncture a useful adjunct to physiotherapy for older adults with knee pain? The “Acupuncture, Physiotherapy and Exercise” (APEX) study. BMC Musculoskelet Disord 2004;5:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352:364-5. [DOI] [PubMed] [Google Scholar]
- 29.Foster NE, Barlas P, Dziedzic K, Daniels J, Gray R. Current physiotherapy management of knee osteoarthritis informs a clinical trial [abstract]. Rheumatology 2000;39(suppl 1):166 [Google Scholar]
- 30.Foster NE, Barlas P, Daniels J, Dziedzic K, Gray R. Use of acupuncture by physiotherapists in the treatment of osteoarthritis of the knee: current trends inform a clinical trial. Birmingham, UK: Proceedings of the Chartered Society of Physiotherapy Congress, Oct 1999;27.
- 31.Kleinhenz J, Streitberger K, Windeler J, Güssbacher A, Mavridis G, Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain 1999;83:235-41. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy N. WOMAC osteoarthritis index. A user's guide Ontario: University of Western Ontario, 1996.
- 33.Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities osteoarthritis index (WOMAC). Pain 2002;100:55-64. [DOI] [PubMed] [Google Scholar]
- 34.Pham T, Van der Heijde D, Lassere M, Altman RD, Anderson JJ, Bellamy N, et al. Outcome variables for osteoarthritis clinical trials: the OMERACT-OARSI set of responders criteria. J Rheumatol 2003;30:1648-54. [PubMed] [Google Scholar]
- 35.Pham T, Van der Heijde D, Altman RD, Anderson JJ, Bellamy N, Hochberg M, et al. OMERACT-OARSI initiative: Osteoarthritis Research Society International set of responder criteria for osteoarthritis clinical trials revisited. Osteo Cartilage 2004;12:389-99. [DOI] [PubMed] [Google Scholar]
- 36.Vincent CA, Lewith G. Placebo controls for acupuncture studies. J R Soc Med 1995;88:199-202. [PMC free article] [PubMed] [Google Scholar]
- 37.O'Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis 1999;58:15-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Norman GR, Streiner DL. Biostatistics: the bare essentials St Louis: Mosby, 1994:160.
- 39.Office for National Statistics. Standard occupational classification 2000, vol. 2 The coding index. London: Stationery Office, 2000:4.
- 40.Office for National Statistics. The national statistics socio-economic classification user manual Version 1. ONS: London, 2002:4.
- 41.Berman BM, Singh BB, Lao L, Langenberg P, Li H, Hadhazy V, et al. A randomized trial of acupuncture as an adjunctive therapy in osteoarthritis of the knee. Rheumatology 1999;38:346-54. [DOI] [PubMed] [Google Scholar]
- 42.Campbell A. Point specificity of acupuncture in the light of recent clinical and imaging studies. Acupunct Med 2006;24:118-22. [DOI] [PubMed] [Google Scholar]
- 43.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 2006;24:13-5. [DOI] [PubMed] [Google Scholar]
- 44.Bausell RB, Lao L, Bergman S, Berman BM. Is acupuncture analgesia an expectancy effect? Preliminary evidence based on participants' perceived assignments in two placebo-controlled trials. Eval Health Prof 2005;28:9-26. [DOI] [PubMed] [Google Scholar]
- 45.Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage 2005;25:1161-7. [DOI] [PubMed] [Google Scholar]
- 46.House of Lords Science and Technology Committee. Sixth report: complementary and alternative medicine. London: Stationery Office, 2000. .www.parliament.thestationeryoffice.co.uk/pa/ld199900/ldselect/ldsctech/123/12301.htm
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.