Abstract
Objectives. We studied failure and delay in making initial treatment contact after the first onset of a mental or substance use disorder in Mexico as a first step to understanding barriers to providing effective treatment in Mexico.
Methods. Data were from the Mexican National Comorbidity Survey (2001–2002), a representative, face-to-face household survey of urban residents aged 18 to 65 years. The age of onset for disorders was compared with the age of first professional treatment contact for each lifetime disorder (as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition).
Results. Many people with lifetime disorders eventually made treatment contact, although the proportions varied for mood (69.9%), anxiety (53.2%), and substance use (22.1%) disorders. Delays were long: 10 years for substance use disorders, 14 years for mood disorders, and 30 years for anxiety disorders. Failure and delay in making initial treatment contact were associated with earlier ages of disorder onset and being in older cohorts.
Conclusions. Failure to make prompt initial treatment contact is an important reason explaining why there are unmet needs for mental health care in Mexico. Meeting these needs will likely require expansion and optimal allocation of resources as well as other interventions.
Mental and substance use disorders account for enormous burdens worldwide. In developing countries, these disorders are already leading causes of disability and their number is expected to increase.1 Many affected individuals in both developed and developing countries fail to receive effective treatment; determining the reasons for this failure is imperative.2
An essential first step in obtaining effective treatment is making prompt contact with a health care provider after the first onset of a mental or substance use disorder.3,4 Unfortunately, little is known about the barriers people face in taking this crucial first step. The few studies of this issue have found that although approximately 80% of people with mental disorders eventually make treatment contact, they typically delay for a decade.5,6
These troubling results come from studies that examined the United States6,7 and other developed countries.8,9 The situation may be far worse in developing countries such as Mexico.10 Indirect evidence supporting this possibility comes from a 2004 Pan-American Health Organization report that documented Mexico’s widespread lack of mental health services and limited treatment options even when services were available.11 Initial results from the World Health Organization (WHO) World Mental Health (WMH) Survey Initiative being implemented in developed and developing countries worldwide showed that respondents in Mexico had one of the lowest rates of prevalence of mental health service use (4.2% vs 15.3% in the United States) among the countries studied.2 A more detailed analysis found that fewer than 1 in 5 respondents with a current, active psychiatric disorder during the previous 12 months used any services during the same period, and only 1 in every 2 of those who used services received care that met minimal standards for adequacy.12
We used data from the recent Mexican National Comorbidity Survey13 to examine the extent to which people with mental and substance use disorders fail and delay in seeking initial treatment. We hypothesized that the situation in a developing country such as Mexico would be worse than that observed in developed countries such as the United States and would illustrate the urgency of intervening to ensure that individuals in need receive prompt and effective initial treatment.
METHODS
Sample and Assessments
The WMH Survey Initiative consists of nationally or regionally representative household surveys carried out in different countries around the world, including Mexico.2 The Mexican National Comorbidity Survey was a stratified, multistage area probability sample of household residents aged 18 to 65 years in Mexico who live in areas with a population of at least 2500 people. Interviews were conducted from September 2001 through May 2002. The response rate was 76.6%. A total of 5826 respondents were interviewed, and 5782 interviews were completed. The interview had 2 parts: part 1, which was administered to all respondents, assessed anxiety, mood, and substance use disorders along with information about basic sociodemographic variables, and part 2, which was administered to all of the part 1 respondents with mental or substsance use disorders and to a probability subsample of other part 1 respondents, assessed other disorders (such as impulse-control disorders) and a wide range of correlates. We used data pertaining to the 5782 respondents who were included in the part 1 sample. More details of the survey and results on the 12-month prevalence of disorders in Mexico are available elsewhere.13
We assessed mental and substance use disorders defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)14 with version 3.0 of the WHO Composite International Diagnostic Interview (CIDI), a fully structured, lay-administered diagnostic questionnaire used in face-to-face interviews.15 The WHO translation protocol was used to translate the instrument and all training materials into Spanish. We report on service use for lifetime cases of psychiatric and substance use disorders, defined according to DSM-IV criteria for diagnoses. All disorders were considered with the exclusion of disorders caused by physical causes and those without diagnostic hierarchy rules (classifying persons by their most serious disorder). The disorders were grouped into the following categories: mood disorders (major depressive episode, bipolar I and II disorder, and dysthymia), anxiety disorders (panic disorder, social phobia, specific phobia, and generalized anxiety disorder), and substance use disorders (alcohol and drug abuse and dependence).
Lifetime Service Use and Predictors
The characteristics of current service use (i.e., previous 12 months) in Mexico were reported by Borges et al.12 We assessed service use by asking respondents, near the end of each CIDI diagnostic section, whether they ever in their life “talked to a medical doctor or other professional” about the disorder under investigation. The interviewer clarified that the term “other professional” was meant to apply broadly to include “psychologists, counselors, spiritual advisors, herbalists, acupuncturists, and any other healing professionals.” Respondents who reported ever talking to any of these professionals about the disorder in question were then asked how old they were the first time they did so. The response to this question was used to define age of first treatment contact.
Predictor variables included the age at onset of the focal disorder (categorized into 25th, 50th, and 75th percentiles), cohort (categorized as ages 18–29, 30–44, and ≥ 45 years at the time of interview), and respondent’s gender.
Statistical Analyses
We used survival analysis to estimate the cumulative lifetime probability of treatment contact from year of disorder onset.16 We estimated ages of disorder onset and first use of mental health services with a 2-part actuarial survival method implemented in SAS version 8.2 (SAS Institute Inc, Cary, NC). We used the actuarial method rather than the more familiar Kaplan–Meier method because it provides a more accurate estimate of disorder onset or service use within a given year.17
The typical duration of delay in initial treatment contact was defined as the median number of years from disorder onset to first treatment contact among individuals who eventually made treatment contact. Discrete-time survival analysis18 with person-year as the unit of analysis was used to examine correlates of treatment contact separately for each disorder. Predictors included both time-invariant predictors (i.e., age at onset of the disorder, cohort, and gender) and a time-varying predictor (i.e., number of years since first onset of the disorder). Standard errors and significance tests were estimated using the Taylor series linearization method18 implemented in SUDAAN version 9.0.1 (Research Triangle Institute, Research Triangle Park, NC) to adjust for the weighting and clustering of data. Multivariate significance of predictor sets was evaluated with Wald χ2 tests derived from design-corrected coefficient variance–covariance matrices. Statistical significance was evaluated with 2-tailed tests, with α = .05.
RESULTS
Most mental disorders in Mexico have an early age of onset. The median age of onset (50th percentile) was age 14 years for anxiety disorders (interquartile range [IQR]: age 8–28 years), age 26 years for substance use disorders (IQR: age 21–38 years), and age 41 years for mood disorders (IQR: age 25–59 years). The first column of Table 1 ▶ presents the proportion of persons with a disorder who made treatment contact in the year of disorder onset. The proportion for persons with any anxiety disorder was 3.6% and ranged from a high of 17.0% for panic disorder to a low of 1.2% for social phobia. For any mood disorder, the percentage was 16.0% and ranged from 19.0% for major depressive episode to 6.5% for bipolar disorder. The lowest proportions were recorded for substance use disorders (0.9%).
1.
Proportional Treatment Contact in the Year of Disorder Onset and Median Duration of Delay Among Patients Who Subsequently Made Treatment Contact: Mexico National Comorbidity Survey, 2001–2002
| Treatment Contact Made in Year of Onset, % | Treatment Contact Made by Age 50 Years, % | Median Duration of Delay, y | Total Number | |
| Anxiety disorders | ||||
| Panic disorder | 17.0 | 79.2 | 16 | 65 |
| Generalized anxiety disorder | 12.7 | 38.6 | 2 | 78 |
| Specific phobia | 1.6 | 25.2 | 26 | 412 |
| Social phobia | 1.2 | 43.9 | 22 | 203 |
| Any anxiety disorders | 3.6 | 53.2 | 30 | 610 |
| Mood disorders | ||||
| Major depressive episode | 19.0 | 70.4 | 13 | 531 |
| Dysthymia | 11.7 | 75.5 | 18 | 89 |
| Bipolar disorder (broad) | 6.5 | 53.1 | 13 | 106 |
| Any mood disorders | 16.0 | 69.9 | 14 | 598 |
| Substance use disorders | ||||
| Alcohol abuse | 2.4 | 24.3 | 12 | 367 |
| Alcohol abuse with dependence | 2.8 | 16.8 | 8 | 141 |
| Drug abuse | 2.9 | 56.9 | 4 | 74 |
| Drug abuse with dependencea | . . . | . . . | . . . | . . . |
| Any substance-use disorders | 0.9 | 22.1 | 10 | 378 |
Note. We assessed mental and substsance use disorders defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition14 with version 3.0 of the WHO Composite International Diagnostic Interview, a fully structured, lay-administered diagnostic questionnaire used in face-to-face interviews.15
aDisorder omitted because of insufficient cases (n < 30) but included in the “any substance use disorders” category.
The proportion of persons with a disorder who made treatment contact by age 50 years is shown in the second column of Table 1 ▶. The proportion for persons with any anxiety disorders was 53.2%; the range was 79.2% for panic disorder to 25.2% for specific phobia. For mood disorders, the proportion was 69.9%, ranging from 75.5% for dysthymia to 53.1% for bipolar disorder. The lowest proportion was observed for substance use disorders (22.1%).
The median duration of delay among persons with a disorder who eventually made treatment contact is shown in the third column of Table 1 ▶. Among the fraction of patients making treatment contacts for the 3 types of disorders, delays were shortest for persons with substance use disorders (median delay of 10 years). Delays were longer for persons with mood disorders (median delay of 14 years) and longest for persons with anxiety disorders (median delay of 30 years). Some large differences were seen within disorder categories; for example, among anxiety disorders, the shortest (2 years for generalized anxiety disorder) and longest (26 years for specific phobia) median delays for an individual disorder were observed. Figure 1 ▶ shows the typical durations of delay in the cumulative lifetime probability of treatment contact among patients who eventually made treatment contact.
FIGURE 1—
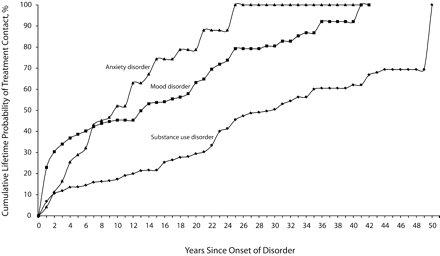
Percentage of respondents who received initial treatment contact since the first onset of a mental or substance use disorder, by group of disorders: Mexico National Comorbidity Survey, 2001–2002.
Results from the discrete-time survival models of lifetime treatment contact are shown in Table 2 ▶. Compared with older cohorts (aged 45–65 years), younger cohorts (aged 18–29 and aged 30–44 years) had higher lifetime probabilities of making a treatment contact for anxiety disorders; there were no statistically significant differences between age cohorts in the probability of making treatment contact for mood or substance use disorders. There were significant differences in the probability of making initial treatment contact according to the age of first onset of mood and anxiety disorders. For example, compared with the group with a late age of onset of the disorder (being in the 75th percentile), all other patients were about 0.2 times as likely to make treatment contact for anxiety disorders and about 0.3 to 0.9 times less likely to make contact for a mood disorder. There were no differences between late- and earlier-onset patients (25th percentile) with substance use disorders. Gender was associated with the likelihood of making initial treatment contact for any mood disorder only, with women more likely to make contact than men.
2.
Sociodemographic Predictors of Lifetime Treatment Contact for Specific Disorders: Mexico National Comorbidity Survey, 2001–2002
| Gender (Female) | Cohort (Age at Interview, y)a | Age of Onseta | |||||||
| OR (95% CI) | P | 18–29, OR (95% CI) | 30–44, OR (95% CI) | P | Early (ages 18–29y), OR (95% CI) | Early Average (ages 30–44y), OR (95% CI) | Late Average (ages 45–65y) OR (95% CI) | P | |
| Anxiety disorders | |||||||||
| Panic disorder | 0.6 (0.2, 1.8) | .337 | 1.1 (0.3, 4.6) | 1.2 (0.3, 4.7) | .978 | 0.3* (0.1, 0.9)b | .025 | ||
| Generalized anxiety disorder | 5.8 (0.8, 40.5) | .070 | 2.4 (0.4, 13.9)b | .318 | 0.2* (0.0, 0.7)b | 0.6 (0.1, 3.1) | .047 | ||
| Specific phobia | 1.1 (0.5, 2.5) | .766 | 2.5 (0.8, 7.9) | 1.2 (0.6, 2.7) | .230 | 0.2* (0.1, 0.5)b | < .001 | ||
| Social phobia | 0.6 (0.3, 1.1) | .096 | 4.3 (0.9, 19.3) b | .055 | 0.4* (0.1, 1.0)b | 1.1 (0.3, 3.3) | .046 | ||
| Any anxiety disorders | 1.1 (0.7, 1.9) | .623 | 2.2* (1.1, 4.5) b | .024 | 0.2* (0.1, 0.2)b | < .001 | |||
| Mood disorders | |||||||||
| Major depressive episode | 1.5 (0.9, 2.5) | .078 | 1.8* (1.0, 3.4) | 1.3 (0.7, 2.2) | .105 | 0.4* (0.2, 0.8)b | 1.0 (0.5, 2.0) | < .001 | |
| Dysthymia | 0.7 (0.3, 2.0) | .504 | 1.3 (0.4, 4.7) | 1.2 (0.4, 3.6) | .912 | 1.0 (0.3, 4.1) | 0.8 (0.2, 3.9) | 1.5 (0.3, 7.5) | .767 |
| Bipolar disorder (broad) | 1.6 (0.5, 5.7) | .457 | 1.5 (0.2, 10.4) | 0.9 (0.2, 4.7) | .735 | 0.3* (0.1, 0.9) b | 1.0 | .030 | |
| Any mood disorders | 1.6* (1.0, 2.4) | .033 | 1.7 (0.9, 3.3) | 1.3 (0.8, 2.4) | .244 | 0.3* (0.2, 0.6) | 0.5* (0.3, 0.9) | 0.9 (0.4, 1.7) | < .001 |
| Substance use disorders | |||||||||
| Alcohol abuse | 2.2 (0.7, 6.6) | .165 | 3.4* (1.1, 10.7) | 1.2 (0.4, 4.1) | .063 | 0.4 (0.2, 1.3) | 1.0 | 1.0 | .135 |
| Alcohol abuse with dependence | 1.2 (0.2, 9.7) | .840 | 4.0 (0.4, 37.2) | 1.1 (0.3, 3.8) | .444 | 0.9 (0.0, 23.2) | 0.7 (0.1, 9.9) | 2.5 (0.3, 17.8) | .393 |
| Drug abusec | . . . | . . . | 0.1* (0.0, 0.9) | 0.1* (0.0, 0.5) | .012 | 1.2 (0.2, 7.7) | 0.7 (0.2, 2.8) | 1.0 (0.2, 4.3) | .892 |
| Any substance-use disorders | 2.3 (0.7, 7.9) | .159 | 2.4 (0.8, 7.3) | 1.2 (0.4, 3.6) | .257 | 1.1 (0.3, 4.4) | 1.9 (0.4, 8.1) | 1.9 (0.6, 5.8) | .568 |
Note. OR = odds ratio; CI = confidence interval. We assessed mental and substsance use disorders as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition14 with version 3.0 of the WHO Composite International Diagnostic Interview, a fully structured, lay-administered diagnostic questionnaire used in face-to-face interviews.15 Drug abuse with dependence disorder category was omitted because of insufficient lifetime cases (n < 30) but included in the “any substance-use disorders” category.
aReference category is age 45–65 years.
bGroups in this row were collapsed.
cGender was used as a control variable in the model except for drug abuse (because of insufficient cases of women).
*Significant at the 0.05 level in a 2-sided test.
DISCUSSION
These findings should be interpreted in light of several potential limitations. Some of these limitations are the result of conducting research on the lifetime occurrence of mental disorders and the lifetime use of services (see Wang et al. for a more detailed discussion19). They include possible recall failure of events and a possible inaccuracy of dating of the disorder onset and first treatment contacts. Furthermore, we lacked information on whether any therapeutic treatment actually took place as the result of initial contacts and on the nature, intensity, and duration of treatment. We also had only a limited set of potential predictor variables that could be retrospectively dated and therefore studied. Finally, one potential limitation specific to the Mexican National Comorbidity Survey is that respondents were drawn only from areas with a population of at least 2500 people but not from more rural areas. A likely effect of this limitation is that our current estimates of initial treatment seeking for mental disorders in Mexico may be overestimates.
Despite these limitations, our results identify a large source of unmet need for mental health care in developing countries such as Mexico. First, many people appear to never make treatment contacts for mental and substance use disorders. Only 1 in 5 persons with a substance use disorder made initial treatment contact by age 50 years, and just over half of persons with an anxiety disorder made initial contact by age 50 years. As we initially hypothesized, these proportions were considerably smaller than those observed in a developed country such as the United States, where the vast majority of persons with a disorder at any age eventually make initial treatment contact.19
Furthermore, even patients who made eventual treatment contact delayed doing so for long periods. Even for persons with substance use disorders, who had the shortest delays, a decade typically elapsed before initial treatment contact was made. For mood and anxiety disorders, these delays were typically more than 1 and 3 decades, respectively. The magnitude of these delays was larger than has been observed in developed countries such as the United States.19 Reasons for the variation among disorders are unclear but may have to do with the relative severity and impairments from disorders, their associated stigma, and the availability of appropriate treatments in Mexico.20–22
In addition to the differences among disorders, we found other predictors of making initial treatment contact. The higher probability of eventual treatment contact in younger cohorts, statistically significant for anxiety disorders only, may have resulted from the de-stigmatization and increased awareness of mental disorders, screening and outreach initiatives, expansion of some insurance programs, and even the introduction of direct-to-consumer advertising for treatments in Mexico.23–25
Substance use disorders were a notable exception to this general pattern of increased lifetime treatment in recent cohorts; whether this was the result of our methods (e.g., failure to capture contacts with self-help groups, which now play increasingly important roles in the treatment of substance use disorders) or substantive processes (e.g., changes in funding of treatment programs or changes in public attitudes toward substance use disorders) requires further investigation.
By contrast, early-onset disorders were associated with lower probabilities of initial treatment contact, perhaps because minors need help from adults to obtain treatment,26,27 and early-onset mental disorders are associated with a normalization of symptoms (e.g., a person appearing “normal” by not exposing themselves to situations in which their symptoms would be obvious) or coping strategies (e.g., social withdrawal) that often interferes with seeking help later.
Obtaining treatment for mental health and substance use disorders in Mexico remains a relatively rare event. Only 5% of persons with an active disorder and 24% of persons with severe mental illness received any form of care within the previous 12 months in our study.12 In the country’s many rural areas, where obtaining treatment can require more than a day’s journey to facilities or personnel, rates of service use are even lower.22,28 This tremendous unmet need for treatment is explained at least in part by structural realities such as a severe shortage of qualified mental health personnel capable of delivering effective care.11,29
As recently as 1976, there were only 507 psychiatrists in Mexico, mostly concentrated in the largest cities; although by 2005 there were 1451 psychiatrists registered with the National Board of Psychiatrists, that still only represented between 1.5 and 2.7 psychiatrists per 100 000 population.30 Similarly, the number of available psychiatric nurses was fewer than 1 per 100 000 population.30 Even the largest health provider in Mexico, the Mexican Institute of Social Security, covering 42 993 343 beneficiaries, employed only 244 psychiatrists in 2004, clearly reflecting grossly insufficient resources for the mental health needs in Mexico. It has been estimated that the number of psychologists working in health sectors in Mexico was approximately 1600 in 1998.31 Furthermore, it is not clear in what capacities these psychologists were functioning, what types of interventions they were delivering, or whether their interventions were adequate.
The challenge is not simply overcoming inadequate infrastructure and a shortage of mental health personnel. Throughout Mexico, the large financial burdens of treatment on individuals or their families, as well as cultural and often linguistic gaps between those needing services and those providing services (caregivers), can create formidable barriers to obtaining treatment. Increased public awareness of mental disorders, effective treatments, and destigmatization efforts are all needed to increase demand for treatment. Furthermore, changes in resource allocation and mental health policy in Mexico will be needed to ensure that increases in demand and availability of resources are matched to patients’ needs. The recent implementation of new government-funded programs for the provision of mental health to 11 million of the poorest and often sickest members of society (Seguro Popular, or Popular Insurance)32 represents one opportunity for policymakers and other stakeholders in Mexico to translate epidemiological data such as those presented here into action.
Our results shed light on the enormous challenges facing persons with mental illness and substance abuse disorders and those who deliver or seek to improve mental health care in developing countries such as Mexico. Large proportions of people with lifetime mental and substance use disorders in Mexico remain untreated, and even those who are eventually treated delay for decades before seeking care. Ensuring prompt, effective treatment and recovery for these patients will clearly require interventions at many levels. New government investments in the mental health infrastructure will be required to increase the availability of services.11 Clinics and clinicians need to recognize disorders and initiate treatments more quickly, which may require implementing screening, demand management for treatment, and other outreach strategies.33,34 Finally, at the population level, programs that increase awareness and change attitudes toward mental and substance use disorders and their treatments are needed.23
Acknowledgments
The Mexican National Comorbidity Survey was supported by the National Institute of Psychiatry Ramon de la Fuente (grant INPRFM-DIES 4280) and by the National Council on Science and Technology (grant CONACyT-G30544-h), with supplemental support from the Pan American Health Organization. The Mexican National Comorbidity Survey was carried out in conjunction with the World Health Organization World Mental Health Survey Initiative, which is supported by the US National Institute of Mental Health (grant R01MH070884); the John D. and Catherine T. MacArthur Foundation; the Pfizer Foundation; the US Public Health Service (grants R13-MH066849, R01-MH069864, and R01 DA016558); the Fogarty International Center (grant FIRCA R01-TW006481); the Pan American Health Organization; Eli Lilly and Company; Ortho-McNeil Pharmaceutical, Inc; Glaxo-SmithKline; and Bristol-Myers Squibb.
We thank the World Mental Health staff for assistance with instrumentation, fieldwork, and data analysis.
Human Participant Protection The institutional review board of the National Institute of Psychiatry, Mexico City, Mexico, approved this study.
Peer Reviewed
Contributors G. Borges originated the study, collected data in Mexico City, analyzed the data, and wrote drafts and the final version of the article. M. E. Medina-Mora originated the study, collected data in Mexico City, and reviewed the final version of the article. P. S. Wang originated the study, participated in planning and data analyses, wrote drafts, and reviewed the final version of the article. C. Lara originated the study, collected data in Mexico City, and reviewed the final version of the article. W. T. Chiu participated in planning and data analyses and reviewed the final version of the article.
References
- 1.Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass: Harvard University Press; 1996.
- 2.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization. World Mental Health Surveys. JAMA. 2004;291: 2581–2590. [DOI] [PubMed] [Google Scholar]
- 3.Gallo JJ, Marino S, Ford D, Anthony JC. Filters on the pathway to mental health care: II. Sociodemographic factors. Psychol Med. 1995;25:1149–1160. [DOI] [PubMed] [Google Scholar]
- 4.Rogler LH, Cortes DE. Help-seeking pathways: a unifying concept in mental health care. Am J Psychiatry. 1993;150:554–561. [DOI] [PubMed] [Google Scholar]
- 5.Johnstone EC, Crow TJ, Johnson AL, MacMillan JF. The Northwick Park study of first episodes of schizophrenia: I. Presentation of the illness and problems relating to admission. Br J Psychiatry. 1986;148: 115–120. [DOI] [PubMed] [Google Scholar]
- 6.Wang PS, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv Res. 2004;39:393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am J Psychiatry. 1998;155:62–69. [DOI] [PubMed] [Google Scholar]
- 8.Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL, Olfson M, Kessler RC. Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: an international survey of members of mental health patient advocate groups. Psychol Med. 2000;30:693–703. [DOI] [PubMed] [Google Scholar]
- 9.Olfson M, Kessler RC, Berglund PA, Lin E. Psychiatric disorder onset and first treatment contact in the United States and Ontario. Am J Psychiatry. 1998;155: 1415–1422. [DOI] [PubMed] [Google Scholar]
- 10.Joska J, Flisher AJ. The assessment of need for mental health services. Soc Psychiatry Psychiatr Epidemiol. 2005;40:529–539. [DOI] [PubMed] [Google Scholar]
- 11.Pan-American Health Organization. The Evaluation of Mental Health Services in the Republic of Mexico [in Spanish]. Mexico City, Mexico: Organizacion Panamericana de la Salud; 2004:42.
- 12.Borges G, Medina-Mora ME, Wang PS, Lara C, Berglund P, Walters E. Treatment and adequacy of treatment for mental disorders in the Mexico National Comordity Survey. Am J Psychiatry. 2006;163: 1371–1378. [DOI] [PubMed] [Google Scholar]
- 13.Medina-Mora ME, Borges G, Lara C, et al. Prevalence, service use, and demographic correlates of 12-month DSM-IV psychiatric disorders in Mexico: results from the Mexican National Comorbidity Survey. Psychol Med. 2005;35:1–11. [DOI] [PubMed] [Google Scholar]
- 14.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC; American Psychiatric Association; 1994.
- 15.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Mental Health (WHO) Compositive International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13: 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halli SS, Rao KV. Advanced Techniques of Population Analysis. New York, NY: Plenum; 1992.
- 17.Efron B. Logistic regression, survival analysis, and the Kaplan–Meier curve. J A Stat Assoc. 1988;83: 414–425. [Google Scholar]
- 18.Wolter K. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1985.
- 19.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62:603–613. [DOI] [PubMed] [Google Scholar]
- 20.Berenzon S, Juarez F. Mental health services to poor patients with affective disorders in Mexico City [in Spanish]. Rev Saude Publica. 2005;39:619–626. [DOI] [PubMed] [Google Scholar]
- 21.Berenzon SG, Medina-Mora ME, Lara MA. Mental health services: twenty five years of research [in Spanish]. Salud Mental. 2003;26:61–72. [Google Scholar]
- 22.Caraveo J, Martínez N, Rivera E, Polo A. Life prevalence of depressive episodes and the use of specialized services [in Spanish]. Salud Mental. 1997;20: 15–23. [Google Scholar]
- 23.Barry MM, Domitrovich C, Lara MA The implementation of mental health promotion programmes. Promot Educ. 2005(suppl 2):30–36. [DOI] [PubMed]
- 24.CONADIC. Action programs: mental health [in Spanish]. Available at: http://www.conadic.gob.mx/interior/menu_principal/programas.html. Accessed June 15, 2007.
- 25.Lara MA, Navarro C, Acevedo M, Berenzon S, Mondragon L, Rubi NA. A psycho-educational intervention for depressed women: a qualitative analysis of the process. Psychol Psychother. 2004;77:429–447. [DOI] [PubMed] [Google Scholar]
- 26.Janicke DM, Finney JW, Riley AW. Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care. 2001;39:990–1001. [DOI] [PubMed] [Google Scholar]
- 27.Morrisey-Kane E, Prinz RJ. Engagement in child and adolescent treatment: the role of parental cognitions and attributions. Clin Child Fam Psychol Rev. 1999;2:183–198. [DOI] [PubMed] [Google Scholar]
- 28.Salgado VN, Díaz-Pérez MJ. Emotional disorders in rural population [in Spanish]. Salud Mental. 1999; 22:68–74. [Google Scholar]
- 29.World Health Organization. The World Health Report 2006—Working Together for Health. Geneva, Switzerland: World Health Organization; 2006.
- 30.World Health Organization. World Mental Health Atlas. Geneva, Switzerland: World Health Organization; 2005;314–317.
- 31.López JAP. Psychology and psychologists in the health sector in Mexico: some disturbing realities [in Spanish]. Int J Clin Health Psychol. 2004;4:191–205. [Google Scholar]
- 32.Office of Human and Social Development. Development Objectives of the Millenium in Mexico: Advance Report 2005 [in Spanish]. Mexico City, Mexico: Secretaria de Desarrollo Social; 2005.
- 33.Carleton RA, Bazzarre T, Drake J, et al. Report of the expert panel on awareness and behavior change to the board of directors, American Heart Association. Circulation. 1996;93:1768–1772. [DOI] [PubMed] [Google Scholar]
- 34.Velicer WF, Hughes SL, Fava JL, Prochaska JO, DiClemente CC. An empirical typology of subjects within stage of change. Addict Behav. 1995;20: 299–320. [DOI] [PubMed] [Google Scholar]


