Abstract
The coexistence of thyroid diseases with primary hyperparathyroidism (PHPT) can present a challenge in the clinical diagnosis and management for these patients. This study aims to determine the frequency of coexisting thyroid gland lesions in a consecutive series patients with PHPT, and to analyze the clinical features, diagnosis and treatment of these patients. Twenty-two cases of a total of 52 PHPT patients who had synchronous thyroid and parathyroid pathology were surgically managed in this study. Thirteen patients had ipsilateral thyroid nodules, and 9 patients had thyroid nodules in contralateral or bilateral side. Seven patients underwent direct parathyroidectomy and hemithyroidectomy via a mini-incision (about 3 cm), while other 15 procedures were converted to Kocher incision. Seventeen nodular goiter (32.7%), 2 thyroiditis (3.8%), 2 thyroid adenoma (3.8%) and 1 thyroid carcinoma (1.9%) coexisting with parathyroid adenoma were pathologically diagnosed. The sensitivity of preoperative ultrasonography (US) and methoxy-isobutyl-isonitrile (MIBI) scintigraphy for parathyroid lesions was 63.6% and 85.7%; and the overall positive predictive values for MIBI and US were 100% and 95.5% respectively. A high incidence of thyroid diseases that coexisted with PHPT in literatures was briefly reviewed. Our study illustrated the need for clinical awareness of concomitant PHPT and thyroid disease. A combination of US, computed tomography (CT) and MIBI scintigraphy would be recommended for preoperative localization of enlarged parathyroid adenoma and for evaluation of thyroid lesions. Synchronous treatment of associated thyroid abnormalities is desirable, and open minimally invasive surgical approach with additional resection of isolated ipsilateral thyroid nodules is possible in some of these patients.
Keywords: Hyperparathyroidism, Thyroid diseases, Imaging diagnosis, Surgical treatment
INTRODUCTION
Although primary hyperparathyroidism (PHPT) is a common disease in Caucasians (Kaplan et al., 1992), it is relatively rare in Chinese. On our previous studies on the preoperative localization and surgical management of this entity, we concluded that PHPT is caused by a solitary adenoma in 95% of patients, and that the simple resection of the affected parathyroid gland through a mini-incision is a safe and effective alternative to conventional bilateral neck exploratory (BNE) operation (Xu et al., 2001).
Synchronous thyroid pathology found in patients presenting PHPT has been observed (Kosem et al., 2004; Sidhu and Campbell, 2000). This coexistence can present a challenge in the clinical decision making and management for these patients. The purpose of the current study is to determine the frequency of coexisting thyroid gland lesions in a consecutive series of 52 patients operated for PHPT, and to analyze the clinical features, diagnosis and treatment of these patients. In particular, the preoperative localization and minimal invasive surgical procedures related to these two diseases are discussed.
MATERIALS AND METHODS
Patients
A total of 52 consecutive patients with biochemically diagnosed PHPT were referred to our department between Jan. 1968 and July 2006. Among them, 22 cases of them who had synchronous thyroid and parathyroid pathology were surgically managed and included in this study. We examined the patient demographics, preoperative symptoms and examination findings, preoperative investigations (including blood tests and radiological investigations), intraoperative findings, histology, and postoperative follow-up.
Preoperative imaging study
All patients underwent neck ultrasonography (US) before surgery. Suspected parathyroid glands as well as thyroid lobes were evaluated by high-resolution (8~14 MHz) transducer (Acuson-Sequoia 512, Germany) or (5~12 MHz) transducer (ALT-HD I5000, USA). In 14 patients, single-tracer, dual-phase scintigraphy (e.Camduet, Siemens, Germany) was followed by the double-tracer visual subtraction technique. Anterior planar images of the neck and chest were acquired for 5 min, starting at 15 min and at 120 min after intravenous injection of 20 mCi 99mTc-MIBI (methoxy-isobutyl-isonitrile) (sestamibi) using a large field-of-view gamma camera equipped with a parallel-hole collimator. Plain and enhanced computed tomography (CT) scans were performed in 8 patients, using a rapid injection of a high dose of contrast medium taken at 5 mm intervals by a scanner (Somatom Plus, Siemens, Germany). The results of localization procedures were compared with intraoperative findings.
Operative procedures
Standard surgical protocol was used for all patients during the study period. We proceeded with focal exploration through a mini-incision about 3 cm long. A conventional collar incision was then required if necessary. Thyroid exploration was performed through the same incision. Suspected lesions (parathyroid adenomas and thyroid nodules) were excised and sent for frozen section examination during surgery. Bilateral exploration and thyroidectomy with modified radical neck dissection were performed when malignant thyroid nodules were proved. If the intraoperative pathology confirmed parathyroid lesions or the serum parathyroid hormone (PTH) level showed a decline of more than 50% from the preoperative levels 10 min after the resection, single-gland disease was assumed and the operation was terminated. The clinical cure was defined when the parathyroid lesion was confirmed to be an adenoma on paraffin section and the serum calcium level was subsequently normalized and sustained within the normal range for at least 6 months following surgery. The removed parathyroid glands and thyroid nodules of all patients had a histopathologic examination for comparison with the preoperative imaging results.
RESULTS
Patients
This group was composed of 6 men and 16 women, with mean age of 46.5 (range 24~72) years. Patient histories were collected. Bone and joint pain was the most frequently reported symptom (16/22, 72.7%) and bone fracture was the most common physical affliction (6/22, 27.3%). Neck mass could be palpated in 12 patients. Thirteen patients had thyroid lesions in ipsilateral thyroid, and 9 in contralateral or bilateral side of thyroid. We summarized the patient demographics, examination findings, and preoperative biochemical parameters in Table 1.
Table 1.
Patient characteristics
| Parameter | Mean | Range | Normal value |
| Age (year) | 46.5 | 24~72 | − |
| Male/female | 6/16 | − | − |
| Serum calcium (mmol/L) | 3.2 | 2.9~4.0 | 2.1~2.6 |
| Alkaline phosphatase (U/L) | 254.5 | 85~540 | 30~140 |
| Serum PTH (pg/ml) | 1180.5 | 385~4257 | 8.0~65.0 |
| Thyrotropin (TSH, IRMA) (mIU/L) | 1.22 | 0.60~2.35 | 0.49~4.67 |
Operative findings and outcome
Exploration of the neck was started at the presumed site. The median mini-incision (3 cm) was chosen in order to be able to convert to a standard Kocher incision if necessary. In 7 patients, hemithyroidectomy was performed on the same side as the enlarged parathyroid gland via the original mini-incision. In other 15 patients, procedures were converted to Kocher incision (7~10 cm) because of technical difficulties related to ensuring adequate resection of thyroid (n=9), uncertainty of intraoperative localization (n=4), an intrathyroid parathyroid adenoma (n=1) and further modified radical neck dissection (n=1).
Twenty-one parathyroid adenomas were confirmed by frozen section examination during the surgery. Serum PTH level was measured intraoperatively in 12 patients and an adequate decline was proved in all these patients. The operative procedures and pathology of 22 PHPT patients with concomitant thyroid disease are shown in Table 2. None of patients suffered recurrent laryngeal nerve palsy. None of them showed any sign of hypocalcemia during 3 months of follow-up.
Table 2.
Operative procedures and pathology of PHPT patients with concomitant thyroid disease
| Number | |
| Concomitant thyroid nodules | 22 |
| Ipsilateral | 13 |
| Contralateral | 7 |
| Bilateral | 2 |
| Operative procedure | |
| Minimally invasive parathyroid exploration and hemithyroidectomy via the original mini-incision | 7 |
| Conversion to thyroid exploration with a standard Kocher incision | 15 |
| Pathology of thyroid | |
| Nodular goiter | 17 |
| Thyroiditis | 2 |
| Adenoma | 2 |
| Papillary carcinoma | 1 |
Sensitivity and positive predictive value of preoperative imaging studies
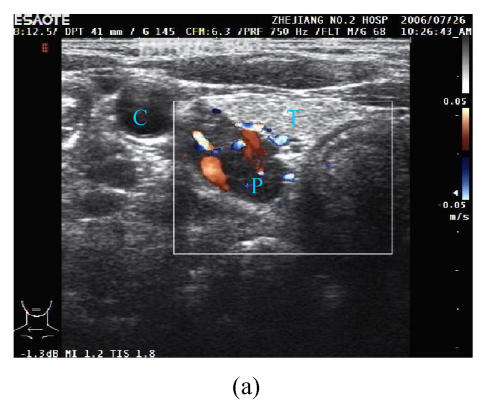
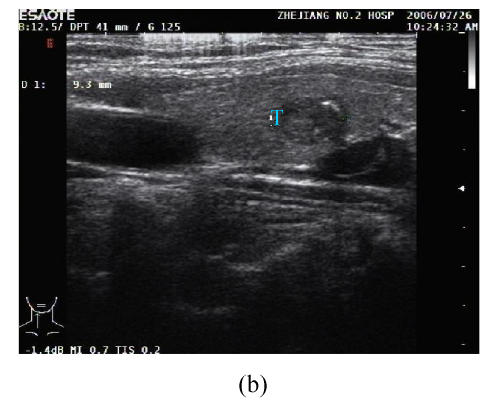
Longitudinal and axial neck US scans were obtained from the angle of the mandible to the sternal notch. The parathyroid adenoma was identified on grey-scale imaging as a hypo-echoic nodule distinct from the thyroid gland, posterior or lateral to the thyroid lobe, with echogenicity less than that of the thyroid glands, oval or oblique in shape, and nonadherent to the surrounding tissues. In addition to this, the thyroid lobes were evaluated by US as well (Fig.1).
Fig. 1.
(a) Transverse US section at the right lower neck showed a hypoechoic nodule (P) posterior to the lower pole of the right thyroid lobe (T) and medial to the common carotid artery (C); (b) Longitudinal section of the same patient as in (a) showed a hypoechoic nodule in the right thyroid lobe
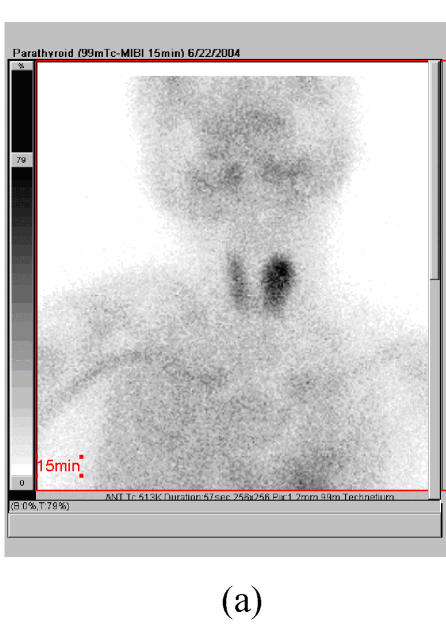
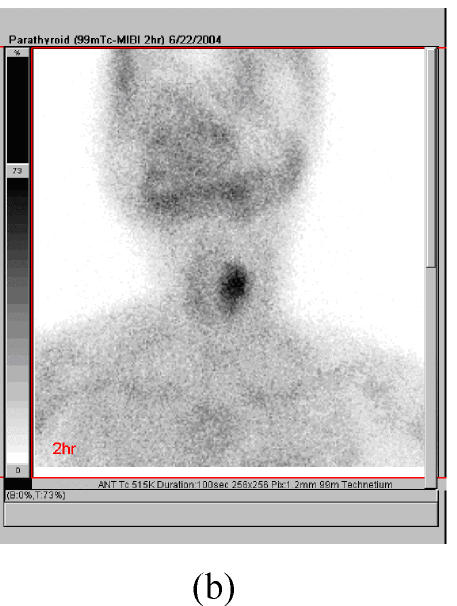
The initial scintigraphic images were compared with delayed views after MIBI administration. A distinct focus of increased or separate MIBI uptake, relative to the thyroid gland on either an early or a late image (or both) was considered positive for abnormal parathyroid tissue (Fig.2).
Fig. 2.
(a) Early anterior 99mTc-sestamibi scintigraphy (MIBI) image; (b) Delayed image demonstrated distinct focus of increased MIBI uptake in a right lower parathyroid adenoma
Spiral CT of the neck revealed a homogeneous mild-hypodensity lesion. The lesion showed a slightly homogeneous enhancement following bolus injection of intravenous contrast. CT films could provide the anatomical orientation for surgeons.
The preoperative imaging data were compared with the operative and pathological findings. The sensitivity and positive predictive value (PPV) of three preoperative imaging methods are presented in Table 3. Prior to surgery, US correctly localized 14 parathyroid adenomas in the whole study group of 22 patients (63.6%), while it was falsely positive in one patient. Preoperative MIBI scintigraphy localized 12 parathyroid adenomas in 14 patients (85.7%). Therefore the sensitivity of US and MIBI scintigraphy for parathyroid lesions was 63.6% and 85.7%. The overall PPV for MIBI and US were 100% and 95.5% respectively. Nineteen abnormal thyroids diagnosed by US were correlated correctly with intraoperative findings. Therefore the sensitivity of US for correct localization of abnormal thyroid nodules was 86.4% with a false positive rate of 18.2%.
Table 3.
Sensitivity and positive predictive value (PPV) of preoperative imaging studies
| US | MIBI | CT | |
| Parathyroid | |||
| PPV | 95.5% (21/22) | 100% (12/12) | 100% (4/4) |
| Sensitivity | 63.6% (14/22) | 85.7% (12/14) | 66.7% (4/6) |
| Thyroid | |||
| PPV | 100% (19/19) | 57.1% (4/7) | 100% (2/2) |
| Sensitivity | 86.4% (19/22) | 28.6% (4/14) | 33.3% (2/6) |
DISCUSSION
Recently, thyroid disease concomitant with PHPT has been reported. The pathological association between these two endocrine glands is not rare, with a prevalence ranging from 18% to 84.3%. Moreover, thyroid carcinoma has been reported in 3.1%~15% of patients with PHPT. These wide variations are attributed to association with the different methods of examination, the surgical indications, and the patient selection process. The characters of thyroid pathology associated with PHPT from these literatures are shown in Table 4 (Bentrem et al., 2002; Kosem et al., 2004; Masatsugu et al., 2005; Sidhu and Campbell, 2000).
Table 4.
Thyroid pathology associated with PHPT
| Authors | Number [T/P (%)] | Nodular goiter | Thyroiditis | Adenoma | Carcinoma | Graves’ |
| Sidhu and Campbell (2000), Australia | 26/65 (40.0%) | 17 (26.2%) | 3 (4.6%) | 3 (4.6%) | 3 (4.6%) | |
| Bentrem et al.(2002), USA | 103/580 (17.8%) | 49 (8.4%) | 8 (1.4%) | 31 (5.3%) | 12 (2.1%) | |
| Kosem et al.(2004), Turkey | 43/51 (84.3%) | 24 (47.0%) | 9 (17.6%) | 2 (3.9%) | 9 (17.6%) | |
| Masatsugu et al.(2005), Japan | 61/110 (55.4%) | 20 (18.2%) | 12 (10.9%) | 7 (6.4%) | 20 (18.2%) | 2 (1.8%) |
| Present series | 22/52 (42.3%) | 17 (32.7%) | 2 (3.8%) | 2 (3.8%) | 1 (1.9%) |
T: Thyroid diseases; P: Hyperparathyroidism
To our knowledge, no study on the coexistence of thyroid and parathyroid diseases has been reported in China. Xiao et al.(2002) described the first case of concomitant Graves’ disease and PHPT in China, which was considered to be coincidental. We have focused on the preoperative diagnosis and surgical management of patients with PHPT since 1980 (Xu et al., 2001). Lesions of the thyroid gland were found in 42.3% of all patients with PHPT, which was similar as other study. Pathology of thyroid lesions involved almost all the common thyroid diseases but Graves’. It is of interest that the frequency of concomitant thyroid malignancy is lower than that in other studies. This could be explained partly by the fact that the relatively rarer use of neck irradiation therapy in China than in western country (Seehofer et al., 2005).
On the other hand, Wagner et al.(1999) reported if all patients with thyroid diseases (13387 cases) were screened for PHPT, the frequency would be higher (55.5%). Pino Rivero et al.(2003) also measured serum calcium concentration in a series of patients with thyroid diseases and demonstrated that a high occurrence of PHPT in those patients (0.29%) as compared to persons without thyroid dysfunction (0.09%).
The cause of this association remains unclear. Some authors considered it to be coincidental, whereas others suggested that some connections might exist between both disorders, such as increased endogenous calcium concentrations, growth factors, epithelial growth factor, and goitrogenic factors. In addition, the concomitance might occur as a part of the syndrome of multiple endocrine adenomas, resulting from the presence of the abnormal gene responsible for this syndrome (Prinz et al., 1982; van der Schaar and Mulder, 1985).
For patients with PHPT, surgical removal of an enlarged parathyroid gland is thought to be a curative treatment. The surgical approach to PHPT has changed since the last decade, moving from bilateral neck exploration (BNE) to unilateral or limited neck exploration, followed by minimally invasive approach which depends on preoperative imaging (Schiffmann et al., 2003). Our group therefore introduced a minimally invasive surgical approach for PHPT since 1993, wherein only a localized area of the neck is explored according to the preoperative imaging evaluation, and the adenoma is resected without histological sampling from the other parathyroid glands (Xu et al., 2006). Several groups have recently reported that concomitant thyroid nodules are main hazard to minimally invasive procedures (Eigelberger and Clark, 2000; Prager et al., 2003). In our setting, open minimally invasive parathyroid exploration is favorable because additional resection of isolated ipsilateral thyroid nodules is possible. In 59.1% (13/22) of our patients nodules were located ipsilateral to the parathyroid adenoma and 53.8% (7/13) of them could still be resected via the original mini-incision.
For successful minimally invasive approaches for PHPT, it is essential to (1) establish whether the parathyroid adenoma is solitary, (2) precisely locate the position of the parathyroid adenoma, and (3) evaluate the presence of possible concomitant nodular thyroid diseases. When thyroid disease coexists, the diagnostic accuracy of PHPT is probably abated. This can result in a challenge in the clinical decision making and management of these patients. Since the first report (Coakley et al., 1989), it has been shown that MIBI scintigraphy is useful for localization of enlarged parathyroid glands. However, the sensitivity and PPV for MIBI were unsatisfactory in the patients with concomitant thyroid disease, due to confusion from enlarged thyroid glands or nodules (Arici et al., 2001). Apart from parathyroid localization studies, an exact thyroid work-up with confirmation of number and localization of all thyroid nodules is necessary preoperatively in the endemic goiter region. US, as a standard modality for evaluation of thyroid lesions, not only detects the presence, site, number, and size of thyroid nodules, but also clearly depicts the characteristics of these nodules. In the present study, concordant preoperative MIBI and US findings represent a reliable localization technique when used together. In addition to planar parathyroid scintigraphy, single photon emission computed tomography (SPECT) and image fusion with computed tomography/magnetic resonance (CT/MR) improve adenoma detection in PHPT, and might be helpful for patients for whom conventional US and other scintigraphic methods have failed for intrinsic reasons due to the concomitant presence of multinodular goitre or ectopic parathyroid gland (d′Amico et al., 2006). In fact, anatomical information provided by CT enables precise localization of the functional abnormalities highlighted by MIBI, and both are essential to a correct surgical approach.
The diagnosis and timely treatment of associated thyroid abnormalities is desirable because a delay in operating would result in increased morbidity associated with a second neck exploration. Other reasons include removal of thyroid goiter for access to an adenoma, worrisome thyroid injury during parathyroidectomy, and an intrathyroid parathyroid adenoma. Therefore, it is quite favorable in evaluating the thyroid gland prior to parathyroid gland operations. A combination of various imaging methods helps surgeons to make an optimal operative strategy before surgery, not only preoperative localization of parathyroid adenoma, but also evaluation of concomitant thyroid lesions.
Footnotes
Project (No. 2007C34001) supported by the Science and Technology Research Foundation of Zhejiang Province, China
References
- 1.Arici C, Cheah WK, Ituarte PH, Morita E, Lynch TC, Siperstein AE, Duh QY, Clark OH. Can localization studies be used to direct focused parathyroid operation? Surgery. 2001;129(6):720–729. doi: 10.1067/msy.2001.114556. [DOI] [PubMed] [Google Scholar]
- 2.Bentrem DJ, Angelos P, Talamonti MS, Nayar R. Is preoperative investigation of the thyroid justified in patients undergoing parathyroidectomy for hyperparathyroidism? Thyroid. 2002;12(12):1109–1112. doi: 10.1089/105072502321085207. [DOI] [PubMed] [Google Scholar]
- 3.Coakley AJ, Kettle AG, Wells CP, O'Doherty MJ, Collins RE. 99mTc sestamibi—a new agent for parathyroid imaging. Nucl Med Commun. 1989;10(11):791–794. doi: 10.1097/00006231-198911000-00003. [DOI] [PubMed] [Google Scholar]
- 4.d′Amico A, Szczucka K, Borys D, Gorczewski K, Steinhof K. SPECT-CT fusion: a new diagnostic tool for endocrinology. Endokrynol Pol. 2006;57(Suppl. A):71–74. [PubMed] [Google Scholar]
- 5.Eigelberger MS, Clark OH. Surgical approaches to primary hyperparathyroidism. Endocrinol Metab Clin North Am. 2000;29(3):479–502. doi: 10.1016/S0889-8529(05)70147-X. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan E, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s. Choice of surgical procedures for this disease. Ann Surg. 1992;215(4):300–317. doi: 10.1097/00000658-199204000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kosem M, Algun E, Kotan C, Harman M, Ozturk M. Coexistent thyroid pathologies and high rate of papillary cancer in patients with primary hyperparathyroidism: controversies about minimal invasive parathyroid surgery. Acta Chir Belg. 2004;104(5):568–571. doi: 10.1080/00015458.2004.11679616. [DOI] [PubMed] [Google Scholar]
- 8.Masatsugu T, Yamashita H, Noguchi S, Nishii R, Watanabe S, Uchino S, Kuroki S, Tanaka M. Significant clinical differences in primary hyperparathyroidism between patients with and those without concomitant thyroid disease. Surg Today. 2005;35(5):351–356. doi: 10.1007/s00595-004-2952-9. [DOI] [PubMed] [Google Scholar]
- 9.Pino Rivero V, Marques Rebollo L, Ambel Albarran A, Trinidad Ruiz G, Pardo Romero G, Blasco Huelva A. Hyperparathyroidism associated with thyroid disease. Retrospective study of 15 patients treated in 11 years. An Otorrinolaringol Ibero Am. 2003;30(5):459–466. [PubMed] [Google Scholar]
- 10.Prager G, Czerny C, Ofluoglu S, Kurtaran A, Passler C, Kaczirek K, Scheuba C, Niederle B. Impact of localization studies on feasibility of minimally invasive parathyroidectomy in an endemic goiter region. J Am Coll Surg. 2003;196(4):541–548. doi: 10.1016/S1072-7515(02)01897-5. [DOI] [PubMed] [Google Scholar]
- 11.Prinz RA, Barbato AL, Braithwaite SS, Brooks MH, Emanuele MA, Gordon DL, Lawrence AM, Paloyan E. Simultaneous primary hyperparathyroidism and nodular thyroid disease. Surgery. 1982;92(3):454–458. [PubMed] [Google Scholar]
- 12.Schiffmann L, Mann B, Hotz H, Buhr HJ. Minimal invasive surgery for pHPT—which patients will profit? Zentralbl Chir. 2003;128(7):561–565. doi: 10.1055/s-2003-40813. (in German) [DOI] [PubMed] [Google Scholar]
- 13.Seehofer D, Rayes N, Klupp J, Nussler NC, Ulrich F, Graef KJ, Schindler R, Steinmuller T, Frei U, Neuhaus P. Prevalence of thyroid nodules and carcinomas in patients operated on for renal hyperparathyroidism: experience with 339 consecutive patients and review of the literature. World J Surg. 2005;29(9):1180–1184. doi: 10.1007/s00268-005-7859-0. [DOI] [PubMed] [Google Scholar]
- 14.Sidhu S, Campbell P. Thyroid pathology associated with primary hyperparathyroidism. Aust N Z J Surg. 2000;70(4):285–287. doi: 10.1046/j.1440-1622.2000.01799.x. [DOI] [PubMed] [Google Scholar]
- 15.van der Schaar H, Mulder H. Lesions of the thyroid gland in patients with primary hyperparathyroidism. Surg Gynecol Obstet. 1985;160(5):407–408. [PubMed] [Google Scholar]
- 16.Wagner B, Begic-Karup S, Raber W, Schneider B, Waldhausl W, Vierhapper H. Prevalence of primary hyperparathyroidism in 13387 patients with thyroid diseases, newly diagnosed by screening of serum calcium. Exp Clin Endocrinol Diabetes. 1999;107(7):457–461. doi: 10.1055/s-0029-1212138. [DOI] [PubMed] [Google Scholar]
- 17.Xiao H, Yu B, Wang S, Chen G. Concomitant Graves’ disease and primary hyperparathyroidism: the first case report in mainland of China and literature review. Chin Med J (Engl) 2002;115(6):939–941. [PubMed] [Google Scholar]
- 18.Xu S, Wang P, Zheng YX, Yu ZG, Chen J. Clinical research of primary hyperparathyroidism. Natl Med J China. 2001;81(23):1453–1455. (in Chinese) [PubMed] [Google Scholar]
- 19.Xu SM, Wu ZR, Wang P, Chen J, Liu YB. Minimally invasive direct parathyroidectomy for primary hyperparathyroidism in 34 cases. Chin J Surg. 2006;44(5):337–338. (in Chinese) [Google Scholar]