Abstract
INTRODUCTION
Preputial problems are a common reason for referral to the paediatric surgical out-patient department. Many boys referred do not need surgical intervention. One indication for intervention is balanitis xerotica obliterans (BXO), a potentially serious condition previously considered rare in childhood.
PATIENTS AND METHODS
Consecutive boys referred to a paediatric general surgical out-patient department with problems relating to their prepuce during a period of 4 years were included. The out-patient diagnosis and management was recorded. All foreskins excised were sent for histological analysis.
RESULTS
A total of 422 boys were referred, median age 6 years 2 months (range, 3 months to 16 years). Over half the boys referred simply required re-assurance that all was normal with their penis. However, 186 boys (44.1%) were listed for surgical procedures – 148 circumcision, 33 preputial adhesiolysis, and 5 frenuloplasty. There were histological abnormalities in 110 specimens (84.8%); chronic inflammation (n = 69; 46.6%), BXO (n = 51; 34.5%), and fibrosis(n = 4; 2.7%). Nineteen (12.8%) specimens were reported as histologically normal. The overall prevalence of BXO in the boys referred was 12.1%.
CONCLUSIONS
In this series, the percentage of boys circumcised and the prevalence of BXO were both higher than in other published series. BXO may be more common and present at a younger age than previously thought.
Keywords: Circumcision, Balanitis xerotica obliterans, Out-patients
Problems with the prepuce (relating to pain, micturition, nonretractibility or cosmesis) are common reasons for referral to the paediatric surgical out-patients. Circumcision is one of the most commonly performed surgical procedures in childhood with nearly 11,000 boys under the age of 14 years circumcised between April 2003 and March 2004 on the NHS in England alone. In addition, over 2500 boys under 14 years underwent other surgery to their prepuce during the same period.1 Surgeons from many different specialties see boys with preputial problems including specialist paediatric surgeons, general surgeons, urologists and plastic surgeons. In addition to the operative workload, a considerable amount of outpatient work is involved, often seeing children who do not need surgical intervention.2
Despite its popularity, the indications for circumcision are controversial, often exciting emotive responses in the literature.3,4 The Royal College of Surgeons of England guidelines on circumcision state that the only absolute indication for circumcision is a pathological phimosis, with recurrent balanoposthitis being a relative indication.5
One cause of pathological phimosis is balanitis xerotica obliterans (BXO), a progressive fibrosis of unknown aetiology.6 BXO is generally, although not universally, accepted as an indication for circumcision.4,7–11 Whether or not BXO is considered a reason to circumcise, it is a significant condition that, if not recognised and treated appropriately, can result in a tight phimosis and lead to meatal or urethral stenosis. Published series of boys under 18 and 15 years, respectively, presenting for circumcision have found BXO in 5–6%.2,12
We examined a consecutive series of boys presenting for consideration for circumcision to determine the nature of the work-load created and the management decisions made. We also reviewed the histological findings in the foreskins of those boys who were circumcised.
Patients and Methods
Consecutive boys under 16 years of age referred between May 2000 and May 2004 for consideration of circumcision to a single general surgeon with an interest in paediatric surgery were included. The out-patient diagnosis made was recorded as was the management plan formulated. The diagnoses made were: BXO, phimosis (implying a pathological condition but not including those suspected of having BXO), preputial adhesions, short frenulum, physiological phimosis (referring to boys with a non-retractile foreskin considered normal for their age and stage of development), or normal. The management plans available were to: discharge, offer an open appointment, arrange a follow-up appointment, divide preputial adhesions, perform a frenuloplasty or circumcise. An open appointment refers to cases where follow-up was not deemed essential but the parents were given access to the clinic directly should they have any concerns.
All boys were followed to discharge. All foreskins excised were sent for histological analysis and the histological diagnosis obtained.
Results
A total of 422 boys were seen in the clinic, median age 6 years 2 months (range, 3 months to 16 years). No boys in this series presented for circumcision for religious reasons although one boy requested circumcision because all the other male members of his family were circumcised.
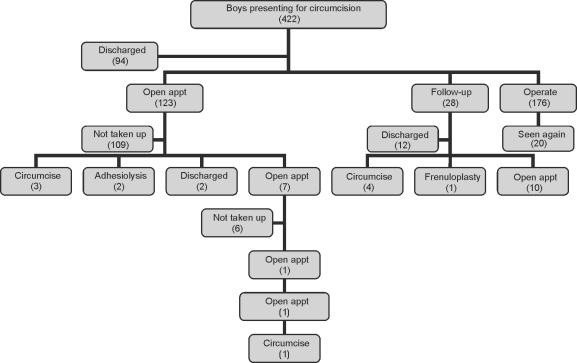
Figure 1 shows a flow diagram of the management of these boys indicating the final outcome and the steps taken to get there. In total, 186 boys had surgery: circumcision (n = 148), adhesiolysis (n = 33), and frenuloplasty (n = 5). The majority (93.6%) of boys who were operated on were only seen once in clinic pre-operatively. All boys who had a diagnosis of BXO made in clinic were circumcised after their first presentation, others circumcised on a single presentation had a diagnosis of phimosis. Those circumcised after follow-up were predominantly diagnosed as having a phimosis; three, however, had been diagnosed as having physiological phimosis. Boys diagnosed as having preputial adhesions underwent adhesiolysis in 73.4% of cases, usually performed using topical local anaesthetic in clinic, most of these at first presentation although two boys had failed to improve by the time they were followed up and underwent adhesiolysis at their second presentation. Six of the eight boys diagnosed as having a short frenulum underwent a frenuloplasty, all but one after their first presentation; one was circumcised.
Figure 1.
Management pathway for boys presenting for circumcision.
The vast majority of the other boys attending out-patients simply required re-assurance, being either discharged or offered an open appointment; for some parents, re-assurance took more than one clinic visit. Indeed, one boy's parents were so concerned they took up the offer of three open appointments, the decision to circumcise being taken at their fourth clinic visit; the foreskin was normal on histological analysis. A few boys had a follow-up appointment arranged; these boys either had diagnoses that may have improved with time (such as preputial adhesions or a physiological phimosis) or were unsure at their initial presentation whether they wanted surgery for their preputial problems.
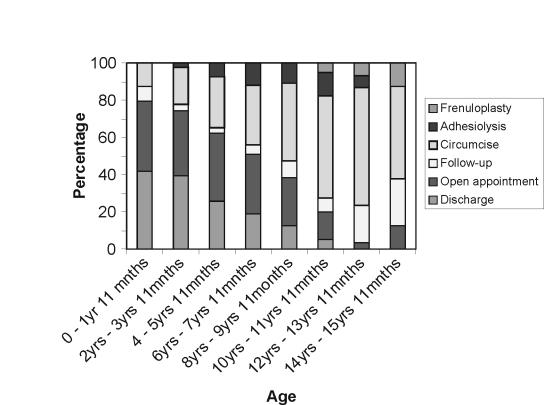
The initial management plan for each boy by age group is shown in Figure 2. As can be seen, the younger the boy at presentation, the more likely they were to be discharged or offered an open appointment. However, in the older age ranges, fewer boys were simply discharged, with the majority either being given follow-up appointments or offered a surgical procedure. Adhesiolysis was most commonly performed between the ages of 6 and 10 years while frenuloplasty was only contemplated for boys over the age of 10 years.
Figure 2.
Initial management decision by age.
It is normal to find a number of chronic inflammatory cells in the prepuce; however, foreskins were only reported as showing chronic inflammation when there was a significant inflammatory infiltrate, consistent with active inflammation.
Of foreskins excised, 84.8% showed significant histological abnormalities with 34.5% of specimens having evidence of BXO. The prevalence of BXO in the population of boys studied was 12.1%. Twenty-seven boys were suspected of having BXO at their out-patient appointment; 24 (88.9%) of these were subsequently confirmed to have evidence of BXO on histological analysis. Of the five boys for whom no histological diagnosis was available, two had their surgery performed elsewhere and the other three had no histology report on their foreskin available.
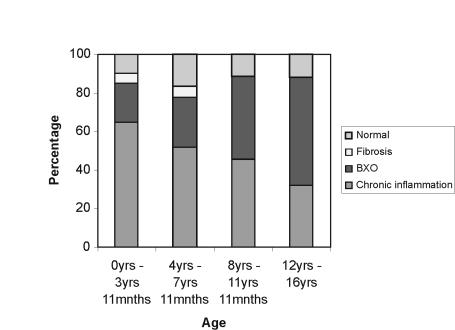
Figure 3 shows the histological diagnoses as a proportion of each age group (having excluded those with no pathological report available; n = 143). It can be clearly seen that in the younger age groups chronic inflammation was the predominant finding, this giving way to BXO as the most common pathological finding in older boys. However, BXO was found in all age groups; the youngest boy with confirmed BXO in the excised specimen was 2 years 6 months old. Isolated fibrosis was an unusual finding restricted to those between the ages of 3 and 6 years. The proportion of normal foreskins remained constant throughout the age groups.
Figure 3.
Histological findings by age.
Discussion
In common with other similar series, the majority of boys referred did not need any surgical procedure,2,12–15 with re-assurance being sufficient intervention. The decision as to how to follow-up the boys reveals how readily parents could be reassured that their child's prepuce was normal. Those discharged were content with simple re-assurance whilst those given open appointments tended to have some residual concerns. The younger the boy at presentation, the more likely simple re-assurance was all that was required; older boys were far more likely to have problems warranting intervention. This is probably due to a combination of wide-spread misunderstanding of normal development early in the life of the prepuce and the fact that older boys will present because they are subjectively experiencing a problem rather than because of the concerns of a third party, most usually a parent but occasionally another health worker such as the GP or health visitor. If primary-care physicians could gain greater understanding of the normal development of the prepuce,16 many referrals to paediatric surgical out-patients and the attendant anxieties could be avoided.
Abnormal pathology was demonstrated in over 85% of those boys circumcised for whom a histology report was available. This was despite circumcising more boys than other authors have reported. Specifically, in our series, the prevalence of BXO was more than double that in previous, comparable series (12.1% versus 5–6%) whilst circumcising a greater proportion of boys (35.1% versus 9–25%).2,12 Other published series from British centres have reported circumcising boys presenting with preputial problems in similar proportions to our series (28–34%) series but these give no figures for the prevalence of BXO.14,15 The number of young children circumcised was, however, higher than in other series, 11% of those presenting under 2 years and 20% of those between 2–4 years. Despite this, the highest proportion of foreskins showing significant histological abnormalities was in those under 4 years (90%), predominantly chronic inflammation but significant numbers of these young boys were found to have evidence of BXO. This is in contrast to other series where authors report finding no cases of pathological phimosis in boys under 5 years of age.14
BXO has traditionally been considered a rare condition that most commonly presents in adulthood.17 In our series, however, it was a common histological finding overall and found frequently in boys of a very young age. There are various possible reasons for these findings. First, there may be a more selective referral pattern from GPs locally. On appointment, the senior author engaged with GPs and gave clear guidelines for referral for circumcision. If this initial engagement had an effect, it could reasonably be expected to wane over time; however, the proportion of boys found to have BXO remained constant throughout the 4 years of the series suggesting our findings cannot be wholly attributed to a more selective referral practice. The prevalence of BXO in the local population of Plymouth may be higher than elsewhere in the country, accounting for our findings. There is no obvious reason for this. Whilst BXO is known to occur more commonly in Black and Hispanic patients,17 the patients in our series were overwhelmingly of Caucasian origin. It may be that BXO is generally more common or that it occurs at a younger age than previously thought. This would have significant implications for the boys developing BXO in childhood. Circumcision is potentially curative for BXO, even when extending onto the glans,7 and timely treatment could prevent the complications that can occur later in life.
Conclusions
If awareness and understanding of the normal development of the prepuce was improved, many referrals to paediatric surgical out-patients and their attendant anxieties could be avoided. All clinicians seeing boys of any age with problems relating to their prepuce should consider BXO in the differential diagnosis and have a low threshold for intervention, be it surgical or otherwise.
References
- 1.Department of Health. Hospital Episode Statistics 2003–2004. London: Department of Health; 2005. [Google Scholar]
- 2.Griffiths D, Frank JD. Inappropriate circumcision referrals by GPs. J R Soc Med. 1992;85:324–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Scheon EJ. ‘Ode to the circumcised male’. Am J Dis Child. 1987;141:128. doi: 10.1001/archpedi.1987.04460020018014. [DOI] [PubMed] [Google Scholar]
- 4.Dalton JD. BXO does not require treatment by circumcision [Letter] BMJ. 2000 Rapid response pages. [Google Scholar]
- 5.The Royal College of Surgeons of England. Statement on Male Circumcision [Press release] London: RCSE; 2001. Mar 6, [Google Scholar]
- 6.Freeman C, Laymon CW. Balanitis xerotica obliterans. Arch Derm Syph. 1941;44:547–59. [Google Scholar]
- 7.Meuli M, Briner J, Hanimann B, Sacher P. Lichen sclerosus et atrophicus causing phimosis in boys: a prospective study with five year follow up after complete circumcision. J Urol. 1994;152:987–9. doi: 10.1016/s0022-5347(17)32638-1. [DOI] [PubMed] [Google Scholar]
- 8.Hrebinko RL. Circumferential laser vaporization for severe meatal stenosis secondary to balanitis xerotica obliterans. J Urol. 1996;156:1735–6. [PubMed] [Google Scholar]
- 9.Jorgensen ET, Svensson A. Problems with the penis and prepuce in children: lichen sclerosus should be treated with corticosteroids to reduce need for surgery. BMJ. 1996;313:692. doi: 10.1136/bmj.313.7058.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Depasquale I, Park AJ, Bracka A. The treatment of balanitis xerotica obliterans. BJU Int. 2000;86:459–65. doi: 10.1046/j.1464-410x.2000.00772.x. [DOI] [PubMed] [Google Scholar]
- 11.Dickson AP. Common non-obstructive urological problems. In: Postlethwaite RJ, editor. Clinical Paediatric Nephrology. 2nd edn. Oxford: Butterworth-Heineman; 1994. [Google Scholar]
- 12.Huntley JS, Bourne MC, Munro FD, Wilson-Storey D. Troubles with the foreskin: one hundred consecutive referrals to paediatric surgeons. J R Soc Med. 2003;96:449–51. doi: 10.1258/jrsm.96.9.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams N, Chell J, Kapila L. Why are children referred for circumcision? BMJ. 1993;306:28. doi: 10.1136/bmj.306.6869.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rickwood AMK, Walker J. Is phimosis overdiagnosed in boys and are too many circumcisions performed in consequence? Ann R Coll Surg Engl. 1989;71:275–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Williams N, Offer GJ, Williams S, Everson N. Parental attitude in children referred for circumcision. Br J Surg. 1997;84:1722–3. [PubMed] [Google Scholar]
- 16.Gairdner D. The fate of the foreskin. BMJ. 1949;ii:1433–7. doi: 10.1136/bmj.2.4642.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kizer WS, Prarie T, Morey AF. Balanitis xerotica obliterans: epidemiological distribution in an equal access health care system. South Med J. 2003;96:9–11. doi: 10.1097/00007611-200301000-00004. [DOI] [PubMed] [Google Scholar]