Abstract
Metastatic Crohn's disease is an uncommon complication of Crohn's disease defined as granulomatous inflammation not contiguous with inflammatory disease in bowel. We report on the presentation and management of a 36-year-old man, who had undergone panproctocolectomy 11 years ago, with complex fistulous disease in his perineum, which demonstrated granulomas histologically after resection. We review six similar case reports. Optimal treatment would appear to be by surgical debridement.
Keywords: Perineal sepsis, Crohn's disease, Surgical management
Patients with Crohn's disease may exhibit a variety of cutaneous disorders such as pyoderma gangareneosum, erythaema multiformae, aphthous ulcers, erythema nodosum and necrotising vasculitis.1 While these skin pathologies can be found in diseases other than Crohn's disease, skin lesions demonstrating characteristic granulomas of Crohn's histologically, are specific to Crohn's disease and are termed metastatic Crohn's disease if not contiguous with bowel inflammatory change. This was first described in 1976.2
Metastatic Crohn's disease of the perineum is uncommon and can manifest several years after an apparently successful proctectomy. Medical treatment of this condition appears to have a poorer outcome than surgical debridement. We report on a case that was treated by aggressive surgical debridement and intensive specialist nurse input.
Case report
A 39-year-old male presented as an out-patient in July 2005 with a 12-month history of pain and discharge from the perineum. He had been diagnosed with Crohn's disease 24 years previously. This had initially been managed with medical therapy but his symptoms progressed and, in 1986, he underwent a subtotal colectomy with an ileorectal anastomosis. Postoperatively, he continued to have discharge from his perineum. A colonoscopy at that time showed a proctitis with an ulcerated lesion at his anastomosis. Medical therapy again was tried but failure of this led to a completion proctectomy the following year. Unfortunately, he was still troubled with occasional episodes of perineal discharge and was, therefore, maintained on oral steroids and salazopyrine. Five years later, he was relatively symptom-free and had discontinued all medications.
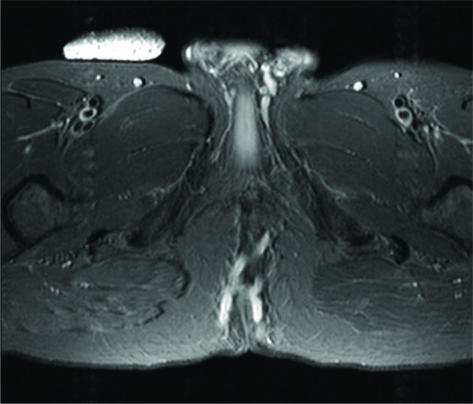
On presentation to out-patient clinic, he had multiple openings in his scrotum extending round to his perineum. His inflammatory markers were mildly elevated and MRI showed a complex H-shaped perineal fistula, giving rise to external openings in the perineum and up to the coccyx via a tract in the ischiorectal fossa. While awaiting an urgent review appointment, he required emergency deroofing of perineal sepsis. Despite this intervention, he was still troubled with perineal pain and discharge. A couple of weeks later, he underwent an examination under anaesthesia which largely confirmed the MRI findings (Fig. 1). Extensive debridement of the perineum was performed removing all affected tissue down to healthy tissue. Microbiological review of pus grew a group B streptococcus. Skin and granulation tissue was sent to pathology which demonstrated chronic inflammation with abscess formation along the sinus tracts with evidence of several non-caseating granulomas in keeping with Crohn's disease. The extensive wound was allowed to heal by secondary intention with expertise from a specialist tissue nurse. When he was reviewed 2 weeks later, there was significant improvement in his symptoms and the wound was healing well. To date, the wound has healed and he has required no further surgical input.
Figure 1.
MRI scan of perineal fistula track.
Discussion
The terms ‘metastatic Crohn's disease’, ‘perineum’ and review of relevant references yielded six case reports in adults. Our patient was included in the review. Details of all cases are displayed in Table 1. The median age was 36 years and male:female ratio was 5:2. One patient presented with perineal ulceration responding to steroids. The remaining patients presented with perineal discharge and sinuses that did not respond to medical therapy and requiring surgical debridement, three with skin or flap graft. The outcome from surgery was good with no patient requiring further intervention.
Table 1.
Review of case reports in literature
| Reference | Williams et al. (1993)3 |
| Age (years) | 25 |
| Sex | M |
| Presentation | Perineal discharge and sinuses. Previous panproctocolectomy 5 years before |
| Symptom duration (years) | 5 |
| Initial management | Prednisolone, azathioprine, dapsone, antibiotics, hyperbaric oxygen failed |
| Treatment | Extensive surgical debridement |
| Outcome | At 1 year, few sinuses remain but healed well |
| Reference | Williams et al. (1993)3 |
| Age (years) | 50 |
| Sex | M |
| Presentation | Chronic perineal discharge from sinuses |
| Symptom duration (years) | 3–4 |
| Initial management | Proctectomy failed |
| Treatment | Extensive debridement and split skin graft |
| Outcome | Healed with no sepsis 16 months later |
| Reference | Williams et al. (1993)3 |
| Age (years) | 54 |
| Sex | M |
| Presentation | Chronic perineal sinus |
| Symptom duration (years) | 26 |
| Initial management | Conservative debridement of sinuses but sepsis continued. Azathioprine/cyclosporin failed |
| Treatment | Debridement and split skin graft 3 years post-presentation |
| Outcome | Good – minimal discharge 10 months later |
| Reference | Williams et al. (1993)3 |
| Age (years) | 48 |
| Sex | F |
| Presentation | Perineal discharge. Panproctocolectomy and ileostomy for Crohn's disease 13 years before |
| Symptom duration (years) | 5 |
| Initial management | Cyclosporin/metronidazole initial improvement then failed |
| Treatment | Extensive debridement down to deep fascia. Closure – secondary intention |
| Outcome | Complete healing 1 year later |
| Reference | Williams et al. (1993)3 |
| Age (years) | 23 |
| Sex | F |
| Presentation | Peri-anal Crohn's disease – subtotal colectomy and ileostomy. Developed peri-anal discharge |
| Symptom duration (years) | 7 |
| Initial management | Steroids, azathioprine, metronidazole and mercaptopurine |
| Treatment | Extensive perineal and vaginal excision with reconstruction flap |
| Outcome | Good results at 6 months |
| Reference | Sangueza and Davis(1997)4 |
| Age (years) | 24 |
| Sex | N |
| Presentation | Perineal ulceration. Past history of perirectal abscess (4 years previously) |
| Symptom duration (years) | 1 |
| Initial management | Prednisolone |
| Treatment | Prednisolone – no surgical management needed |
| Outcome | Good |
| Reference | This case |
| Age (years) | 36 |
| Sex | M |
| Presentation | Perineal sepsis. Previous panproctocolectomy 18 years ago |
| Symptom duration (years) | 1 |
| Initial management | |
| Treatment | Extensive surgical debridement |
| Outcome | Good |
Conclusions
Perineal sepsis containing granulomas characteristic of Crohn's disease can occur at a long interval following proctectomy. Medical therapy would only appear to be useful in very mild disease and treatment should be extensive surgical debridement with specialist nursing wound care. No cases have been published since Infliximab came into use and this may be of benefit, but the purpose of this report is to highlight the possibility of metastatic Crohn's disease and allow such patients to be considered for surgery rather than a lengthy period of medical therapy.
References
- 1.Burgdorf W. Cutaneous manifestations of Crohn's disease. J Am Acad Dermatol. 1981;5:689–95. doi: 10.1016/s0190-9622(81)70130-0. [DOI] [PubMed] [Google Scholar]
- 2.McCallum DI, Gray WM. Metastatic Crohn's disease. Br J Dermatol. 1976;95:551–4. doi: 10.1111/j.1365-2133.1976.tb00868.x. [DOI] [PubMed] [Google Scholar]
- 3.Williams N, Scott NA, Watson JS, Irving MH. Surgical management of perineal and metastatic cutaneous Crohn's disease. Br J Surg. 1993;80:1596–8. doi: 10.1002/bjs.1800801235. [DOI] [PubMed] [Google Scholar]
- 4.Sangueza OP, Davis LS. Metastatic Crohn's disease. Southern Med J. 1997;90:897–8. doi: 10.1097/00007611-199709000-00006. [DOI] [PubMed] [Google Scholar]