Abstract
INTRODUCTION
Injuries to the origin of the hamstring muscles usually occur in athletes and can result in an avulsion fracture of the ischium, an avulsion of the ischial apophysis, or a pure avulsion of the hamstring tendons themselves, depending on the patient' sage. These are rare injuries in the general population and are often initially misdiagnosed as a simple ‘hamstring pull’, leading to the development of chronic pain and disability.
PATIENTS AND METHODS
We present a retrospective case series of the 12 patients with such injuies who presented or were referred consecutively to the senior author between 1997 and 2006.
RESULTS
There was a significant delay (5 months to 12 years) in the diagnosis of the injury in 8 of the 12 patients. Five of these 8 patients required more extensive surgery than would otherwise have been required as a result of this delay, but all recovered well. The sporting career of one of the remaining three patients had already been brought to an end by her injury and the subsequent disability, and she elected not to have surgery. Of the four patients who were diagnosed acutely, three required surgery, and all four had an excellent result.
CONCLUSIONS
Injuries to the hamstring origin are rare and are often initially misdiagnosed as a simple ‘hamstring pull’, leading to the development of chronic pain and disability. Displaced injuries of the ischial apophysis and pure tendon avulsions are probably best treated surgically in the acute setting. As a result of our experience with these patients, we have produced a management algorithm.
Keywords: Hamstring, Avulsion injury, Management algorithm
Injury to the hamstring origin usually occurs when sudden forcible contraction of the hamstring muscles against resistance causes excessive eccentric overload, as in sporting activities such as gymnastics and sprinting. However, the nature of the injury to this area of the hamstring muscles and the adjacent skeleton depends on the skeletal maturity of the patient. The ischial apophysis, a secondary ossification centre, appears at puberty and does not fuse until the late teenage years or early twenties.
During this interval between the appearance of the apophysis and its fusion, a sudden forcible hamstring contraction may cause avulsion of the apophysis itself, at a time when the link between apophysis and bone is weaker than that between tendon and apophysis.1 After skeletal maturity has been reached, an avulsion is more likely to occur at the tendon–bone interface. In rare instances, a skeletally mature patient may avulse a significant fragment of ischium.
Injuries at the hamstring origin are rare when considered alongside mid-substance hamstring muscle ruptures,2 and it may be for this reason that, both in the authors’ experience and in the cases of several patients cited in the literature,3–6 a delay in diagnosis is common. While a muscle rupture is treated with non-operative measures, we feel that displaced fractures of the ischium or ischial apophysis are best treated operatively in the acute setting. A pure avulsion of the hamstring tendon origin is particularly unusual, but it has been shown that an athlete is unlikely to return to previous levels of sporting activity unless this is re-attached surgically and allowed to heal.7
We report 12 consecutively treated patients who illustrate the spectrum of injury possible at the hamstring origin and, as a result of our experience, have formulated a management algorithm.
Results
The patients were all referred to the senior author (MDB) between 1997 and 2006, except for one patient who presented directly to a fracture clinic. They were treated both operatively and non-operatively, and at varying times post-injury. Details of the 12 patients’ histories are summarised in Table 1. Each of the patients gave informed consent to data concerning their cases being included in this study.
Table 1.
Summary of the case histories of the 12 patients
| No/sex | Referral source | Age at time of injury | Age at time of diagnosis | Injury to surgery | Mechanism of injury | Diagnosis | Management | Outcome |
|---|---|---|---|---|---|---|---|---|
| Group A | Ischial | Apophysis | Avulsions | |||||
| 1M | St George's clinic | 16 | 16 | N/A | Martial arts, high kick | Undisplaced avulsion | Non-operative | Good |
| 2F | Orthopaedic specialist | 15 | 17 | 30 months | Gymnastics, ‘did the splits’ | Displaced avulsion, > 3 cm | Operative (Recon plate and bone graft) | Good |
| 3M | Rheumatology specialist | 14 | 16 | 36 months | Sprinting | Displaced avulsion, > 3 cm | Operative (Recon plate and bone graft) | Good |
| 4M | Orthopaedic specialist | 15 | 18 | 30 months | Football, ‘lunged for ball’ | Displaced avulsion, > 3 cm | Operative (Recon plate and bone graft) | Screws broke, revised, good outcome (see text) |
| 5M | General practitioner | 12 | 15 | N/A | Rugby tackle and fall | Chronic avulsion 3 cm and acute bone bruise | Non-operative | Satisfactory |
| 6M | General practitioner | 9 | 9 | 3 months | Bad landing after a ski jump | Laterally displaced avulsion, 2 cm | Operative (Recon plate, no bone graft) | Good |
| Group B | Hamstring | Tendon | Avulsions | |||||
| 7M | Orthopaedic specialist | 30 | 30 | 5 months | Karate kick, swivelled on back leg | Avulsion of hamstring origin, 3 cm | Operative (4 bone anchors used) | Good (75% strength) |
| 8M | Orthopaedic specialist | 23 | 24 | 14 months | Football, ‘did the splits’ | Avulsion of hamstring origin, 10 cm | Operative (4 bone anchors used) | Good |
| 9M | General practitioner | 19 | 31 | 12 years | Martial arts kick | Avulsion of hamstring origin, 2 cm | Operative (4 bone anchors used) | Good |
| 10F | St George's orthopaedic specialist | 51 | 51 | 10 weeks | Running, slipped on wet surface | Avulsion of hamstring origin, 4 cm | Operative (6 bone anchors used) | Good (70% strength) |
| 11F | Orthopaedic specialist | 20 | 22 | N/A | Tennis, ‘lunged to reach ball’ | Avulsion of hamstring origin, 6 cm | Declined surgery | Poor (unable to compete) |
| Group C | Ischial | Avulsion | Fracture | |||||
| 12M | Orthopaedic specialist | 32 | 32 | < 1 week | Water-skiing, leading leg | Avulsion of large part of ischium | Operative (Recon plate, no bone graft) | Good |
Case studies
GROUP A (PATIENTS 1–6): AVULSION OF THE ISCHIAL APOPHYSIS IN THE SKELETALLY IMMATURE
The six patients in this group were between the ages of 9–16 years at the time of their injuries; in all but patient 6, there was a significant delay in diagnosis. All the injuries occurred during sporting activities in which a sudden eccentric loading of the hamstrings had occurred, and all but patient 6 were treated over a prolonged period for a presumed mid-substance tear of the hamstring muscles.
The histories of all six patients were similar in that a combination of time, rest and analgesia, followed usually by physiotherapy, led to an improvement in their acute symptoms of pain. All regained the ability to walk without pain, but continued to experience either occasional (patient 5) or persisting discomfort on running and sitting. Examination tended to demonstrate wasting of the hamstring muscles and weakness of knee flexion, a palpable gap at the hamstring origin and, in some cases, persisting ischial tenderness. One of the patients (patient 3) had symptoms suggestive of sciatica and was referred to a rheumatology specialist for imaging of the lumbar spine, before a plain radiograph of the pelvis was obtained. This patient required a neurolysis as part of the operative procedure to release the sciatic nerve from surrounding scar tissue. The common feature, in all but patient 6, was a delay in obtaining an anteroposterior X-ray of the pelvis.
Patient 5 presented, following a recent rugby injury, complaining of similar acute symptoms. Magnetic resonance imaging confirmed a chronic apophyseal avulsion which was thought to have occurred 3 years’ previously, and acute bone bruising at the posterior aspect of the acetabulum. Acute symptoms settled with rest and were attributed to the bone bruising. However, unlike the other patients in this group, the limited chronic symptoms were not considered severe enough to embark upon surgery.
Operative treatment, where undertaken, was essentially the same for all. The operative approach used was similar to the ‘Kocher–Langenbeck’ approach for posterior column acetabular fractures, but sited a little more posteriorly. The only exception to this was for patient 2, the only female in this group, where a transverse incision in the gluteal crease was used for cosmetic reasons. In all but patient 6, the fixation was augmented with bone graft, taken either from the greater trochanter of the femur or the posterior aspect of the iliac crest. Pelvic reconstruction plates and screws were used for fixation. No splintage was needed postoperatively, although patients were asked to touch weight-bear on the affected side for about 8 weeks.
In patient 4, full reduction of the displaced fragment had been difficult to achieve medially. The fixation failed (Fig. 1) with breakage of the inferior screws, but was revised successfully. All the operated patients returned to their previous levels of sports between 6 months and 1 year postoperatively.
Figure 1.
One patient experienced complications following reduction and fixation of a widely displaced non-union: (A) Patient 4: a widely displaced non-union of the left ischial apophysis. (B) Patient 4: failure of fixation requiring second operation in a still symptomatic patient. (C) Patient 4: union of the fracture was achieved after revision of the fixation.
GROUP B (PATIENTS 7–11): AVULSION OF THE HAMSTRING ORIGIN IN THE SKELETALLY MATURE
The five patients in this group were aged 19–51 years at the time of injury. Again, in all but one (patient 10), there was a significant delay to diagnosis, in one case as long as 12 years. Persisting symptoms included pain on attempting to run or exercise. Examination findings were also similar to the adolescent group, with a palpable gap, wasting and weakness apparent in all five patients. Confirmation of the diagnosis was achieved by magnetic resonance imaging (Fig. 2).
Figure 2.
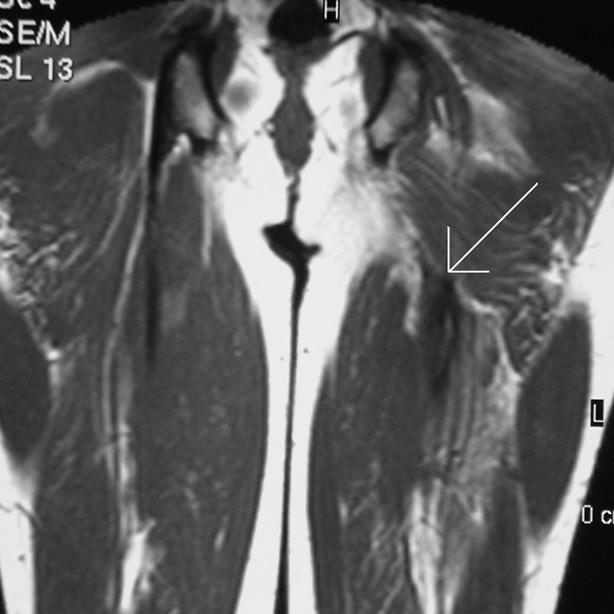
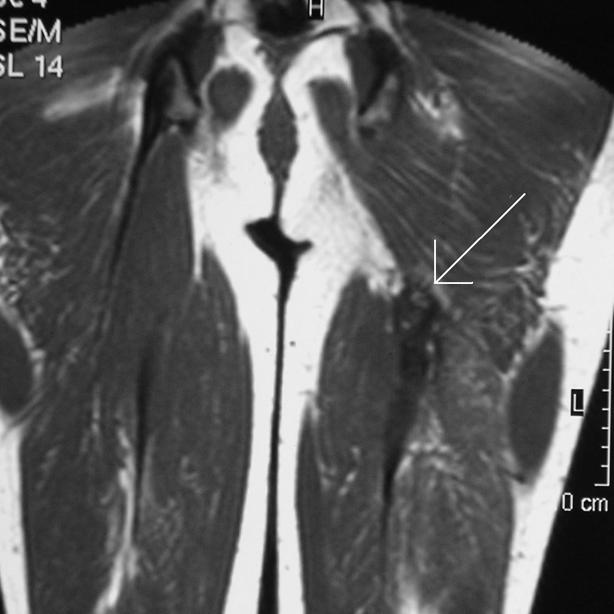
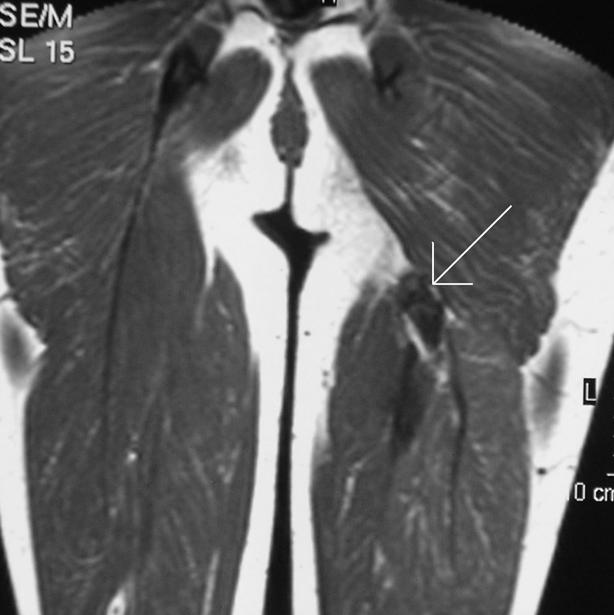
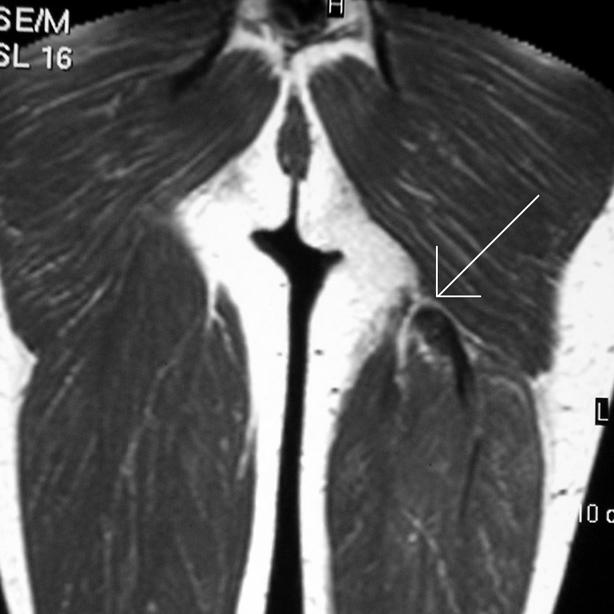
(A–D) Patient 7: four consecutive coronal MRI images (T1-weighted spin echo sequences) clearly demonstrate the left hamstring avulsion.
The amount of avulsion varied from 2 cm to as much as 10 cm. Neurolysis of the sciatic nerve was required in all the chronically retracted cases. The same operative approach was used as for Group A patients, and 4–6 large bone anchors were required to effect a repair. Splintage of the knee in a brace was used, starting at 90° of flexion for 6 weeks and then gradually reducing over the following 6 weeks. This was followed by an intense programme of physiotherapy to restore muscle length and strength. In two patients, measurements of peak muscle torque were made at 6 months using a Kin-Com dynamometer and comparing strength to the contralateral hamstrings (Table 1). Patient 11 declined surgery, having already ceased a semiprofessional tennis career at national level. Patients 7–10 have been successful in returning to their previous levels of sporting endeavours.
GROUP C (PATIENT 12): AVULSION OF THE ISCHIUM IN THE SKELETALLY MATURE
This 32-year-old man was transferred from a hospital in the same region having presented to the accident and emergency department. He was unable to walk and in severe pain after an injury to his leading leg whilst water-skiing. Radiographs were diagnostic, showing a large segment of the ischium and ischiopubic ramus which had been avulsed, leaving the tendons intact. A Kocher–Langenbeck approach was used to achieve reduction and plate fixation. No splintage was needed. The patient made a full recovery and returned to water-skiing within 9 months.
Discussion
These cases demonstrate the spectrum of possible injuries to the proximal hamstring complex, affecting patients from adolescence through to full skeletal maturity. While this is a heterogeneous group, it should be noted that the essential mechanism of injury was the same throughout – sudden excessive eccentric overload of the hamstrings, in disciplines as diverse as water-skiing and martial arts.
These cases demonstrate the importance of maintaining a high index of suspicion for serious injury to the hamstring origin, either tendinous or bony, in the presence of ischial tenderness. While a palpable gap at the hamstring origin may be present, conclusive physical examination of these patients in the acute setting may be difficult because of the pain and swelling associated with this injury.6,8 Indeed, for 8 of the 12 patients, a significant delay occurred before the correct diagnosis was made. Awareness is probably only high amongst those working specifically with competitive sportsmen and women, in whom such injuries are probably more frequent.9
Four of the first six patients, all adolescents or younger, were not correctly diagnosed for some time after their injury. All of these patients developed established non-unions, and three had chronic symptoms of pain on sitting, and inability to run or take part in sports. This delay would have been reduced or prevented in these cases if an anteroposterior radiograph of the pelvis had been taken at the time of initial presentation.10 Presence of a significantly displaced avulsion of the ischial apophysis may be considered an indication for surgical fixation in the acute setting, because of the likelihood of developing chronic symptoms; however, it is impossible to estimate how many patients who have sustained a displaced avulsion go on to make a full functional recovery (such as patient 5), as the studies documenting large numbers of avulsed ischial apophyses have been radiological, rather than clinical, and do not comment on degrees of displacement.9 Even in the case of the undisplaced fracture (patient 1), recognition of the true nature of the injury is important, as a longer period of rehabilitation will be necessary,2 and hamstring stretching may have to be avoided for a period of weeks. While this is too uncommon an injury to propose a randomised prospective study, there are a few other examples of similar cases in the literature where operative treatment has been carried out for displaced non-unions with good results.4,11
Patients 7–11 demonstrate clearly that a normal X-ray does not exclude serious injury to the hamstring origin, especially in the older, skeletally mature patient. MRI scanning has been shown to be a sensitive test for hamstring avulsion,12,13 and should be carried out expeditiously so as not to delay surgery. Patients 7 and 10 regained hamstring muscle strength comparable to other published results of repairs of both acute and chronic injuries,14 and were able to return to practicing their sports of choice.
There have been at least five other reports in the recent literature also showing good outcome from surgical reattachment of the hamstring origin, both in the acute and the delayed setting.5,6,8,14–16 However, two studies have demonstrated a superior outcome in cases where surgery was undertaken ‘acutely’, within 2–3 months of the injury.8,15 Neurolysis of the sciatic nerve may be required, particularly in cases where the surgery is delayed.5,6 In one case of delayed repair, the use of a polypropylene ligament augmentation device was required.3 An important feature of these patients’ management postoperatively in some centres has been the use of splintage whilst maintaining knee flexion to protect the repair for a period of 3–8 weeks.3,5,16 Conservative treatment of this injury may allow retraction of the hamstring musculature and, therefore, prevent patients returning to their previous level of sporting prowess, as in patient 11 and other specific cases cited in the literature.7,16
Patient 12, again, demonstrates the role of an anteroposterior radiograph in the acute setting, on this occasion in the skeletally mature patient. An excellent outcome was obtained from operative fixation of the large avulsed fragment, without any requirement for immobilisation of the knee.
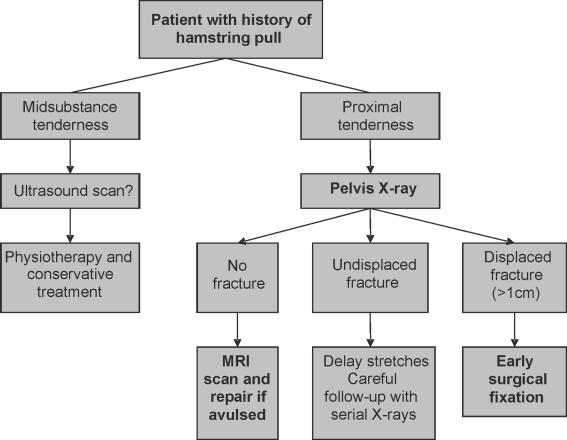
The cases presented above represent a consecutive series of patients with hamstring origin injury presenting to one specialist. While definite conclusions about the efficacy of operative versus non-operative treatment cannot be drawn from this group, we believe that a logical approach to patients with such injuries can be suggested on the basis of our experience (Fig. 3).
Figure 3.
An algorithm for the management of injuries to the hamstring origin.
All patients with a history of a hamstring injury should first be examined for the site of maximal tenderness. Patients with mid-substance tenderness may be further assessed with an ultrasound scan which, in the acute stage, has been shown to be as sensitive as MRI.17 The presence of proximal tenderness is an indication for pelvic radiography to exclude the presence of a fracture. Patients without a fracture should be investigated further with an MRI scan to detect a possible avulsion of the hamstring origin. Ultrasonography has been clearly shown to be less reliable in the diagnosis of such injuries.13 In this series, patients who underwent surgical repair of a displaced fracture of the ischium or an avulsion of the hamstring origin had a good outcome.
References
- 1.Mattick AP, Beattie TF, Macnicol MF. Just a pulled hamstring? Emerg Med J. 1999;16:457–8. doi: 10.1136/emj.16.6.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kujala UM, Orava S, Jarvinen M. Hamstring injuries. Current trends in treatment and prevention. Sports Med. 1997;23:397–404. doi: 10.2165/00007256-199723060-00005. [DOI] [PubMed] [Google Scholar]
- 3.Thomsen NO, Jensen TT. Late repair of rupture of the hamstring tendons from the ischial tuberosity – a case report. Acta Orthop Scand. 1999;70:89–91. doi: 10.3109/17453679909000967. [DOI] [PubMed] [Google Scholar]
- 4.Wootton JR, Cross MJ, Holt KWG. Avulsion of the ischial apophysis. The case for open reduction and internal fixation. J Bone Joint Surg Br. 1990;72:625–7. doi: 10.1302/0301-620X.72B4.2380217. [DOI] [PubMed] [Google Scholar]
- 5.Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26:785–8. doi: 10.1177/03635465980260060801. [DOI] [PubMed] [Google Scholar]
- 6.Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742–7. doi: 10.1177/03635465020300051901. [DOI] [PubMed] [Google Scholar]
- 7.Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130–6. doi: 10.1177/036354659602400202. [DOI] [PubMed] [Google Scholar]
- 8.Johnson AE, Granville RR, DeBerardino TM. Avulsion of the common hamstring tendon origin in an active duty airman. Mil Med. 2003;168:40–2. [PubMed] [Google Scholar]
- 9.Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127–31. doi: 10.1007/s002560000319. [DOI] [PubMed] [Google Scholar]
- 10.Gidwani S, Jagiello J, Bircher M. Lesson of the week. Avulsion fracture of the ischial tuberosity in adolescents – an easily missed diagnosis. BMJ. 2004;329:99–100. doi: 10.1136/bmj.329.7457.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Servant CT, Jones CB. Displaced avulsion of the ischial apophysis: a hamstring injury requiring internal fixation. Br J Sports Med. 1998;32:255–7. doi: 10.1136/bjsm.32.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandser EA, El-Khoury GY, Kathol MH, Callaghan JJ, Tearse DS. Hamstring injuries: radiographic, CT and MR imaging characteristics. Radiology. 1995;197:257–62. doi: 10.1148/radiology.197.1.7568833. [DOI] [PubMed] [Google Scholar]
- 13.Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–9. doi: 10.1007/s00256-003-0674-5. [DOI] [PubMed] [Google Scholar]
- 14.Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13:411–8. doi: 10.1007/s00167-004-0563-z. [DOI] [PubMed] [Google Scholar]
- 15.Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23:702–5. doi: 10.1177/036354659502300612. [DOI] [PubMed] [Google Scholar]
- 16.Kurosawa H, Nakasita K, Nakasita H, Sasaki S, Takeda S. Complete avulsion of the hamstring tendons from the ischial tuberosity. A report of two cases sustained in judo. Br J Sports Med. 1996;30:72–4. doi: 10.1136/bjsm.30.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975–84. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]