Abstract
INTRODUCTION
The unplanned re-admission rate is a national key performance indicator employed by the UK Department of Health. An adjusted figure, based on admission information data on the hospital electronic Patient Administration System (PAS), but adjusted to take account of case mix is compared with a calculated ‘expected’. While previous studies have investigated unplanned re-admission rates in age-, procedure- or process-specific conditions, ‘all-cause’ general surgical re-admission rate is yet to be studied. The aim of this study was to assess the accuracy of hospital unplanned re-admission data, and identify patterns or possible causes of unplanned general surgical re-admissions.
PATIENTS AND METHODS
Retrospective audit of case note records of all patients identified from the hospital electronic PAS as unplanned, general surgical re-admissions over a period of 4 consecutive months.
RESULTS
Of all 161 re-admissions in this study, 46 (29%) were unrelated to the index admission, planned or involved patient self-discharge during the index admission. Of the ‘genuine’, unplanned re-admissions, 80 (78%) followed an emergency index admission, 58 (56%) had chronic or recurrent symptoms, for which 26 (25%) were on waiting lists. Fourteen (14%) were multiple admissions of 4 patients, while 8 (8%) re-admissions required further surgery for significant postoperative complications.
CONCLUSIONS
Unplanned. general surgical re-admission rates collated from hospital PAS systems may be inaccurate. Nearly half of ‘genuine’, unplanned re-admissions involved patients with chronic and/or recurrent symptoms, which are predictable and may be preventable. Significant postoperative complications accounted for few re-admissions in this study.
Keywords: Unplanned re-admissions, General surgery re-admissions, Re-admission, General surgery, Patient Administration System, PAS
Assessment of quality of care by unplanned admission rates is controversial.1–3 It is, however, a national key performance indicator employed by the UK Department of Health, and contributes to ‘star’ status.
While there are several studies of unplanned re-admissions, most have tended to be age specific,4 procedure specific, e.g. after hip fractures,5 or process specific, e.g. day-surgery or early mobilisation after major surgery.6–8 This is the first study of ‘all-cause’, unplanned general surgical re-admissions.
The primary aim of this study was to establish the accuracy of the hospital information database (PAS) generated unplanned re-admissions data. The secondary aim was to identify predictable and, therefore, potentially preventable causes of unplanned, general surgical re-admission.
Patients and Methods
Adjusted, unplanned, re-admission rates (adjusted to allow for varying case-mix, out of hospital trust re-admissions, etc.) are employed as relative indicators of performance. The data presented in this study are the ‘raw’ unplanned re-admission rates prior to ‘adjustment’ for central analysis.
An unplanned re-admission is defined by clinical governance as any re-admission within the trust occurring within the 28 days of the previous admission. A list of all such re-admissions to the University Hospital Birmingham between April and July 2003 was generated from the hospital database (Patient Administration System, PAS) system by the health informatics team. This 4-month period was selected for study because ‘adjusted’, unplanned re-admission rates were higher than the ‘expected’.
The accuracy of the retrieved data was analysed in two stages. The PAS recorded data was reviewed by the admitting consultant. A specialist registrar (DA) then reviewed the case records of all the re-admitted patients. Information data relevant to the aims of this study were recorded on a pre-designed form.
Re-admissions with recurrent or chronic problems were defined as those where the same symptoms/clinical problems had been managed by hospital consultants for at least 6 months prior to index admission.
Results
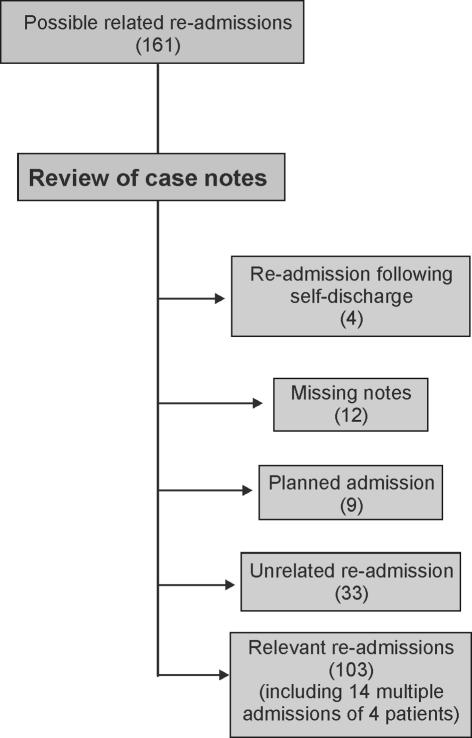
From an initial total of 161 ‘PAS coded’ re-admissions, 46 (29%) re-admissions were excluded because they were planned (9), unrelated (33) or had self-discharged (4) at the index admission. Table 1 lists re-admission diagnoses unrelated to index admission. Twelve re-admissions were excluded because the relevant notes were incomplete or missing.
Table 1.
Unrelated index and re-admission diagnoses obtained from individual case notes
| Re-admission diagnosis | Index admission |
|---|---|
| Epileptic seizure | Hydrocoele repair |
| Domestic tendon injury | Appendicectomy |
| Arthritis/Truncal cutaneous abscess/Pericardial effusion | OGD |
| MI/Lobar pneumonia/Asthma attack/Painful hip | 2 weeks post-OGD |
| Constipation | Cholangitis |
| Sebaceous cyst abscess | Dyspepsia |
| Peri-anal abscess/Alcohol intoxication | Neck sebaceous cyst excision |
| Haemoptysis | Haemorrhoidectomy |
| Angina attack | 3 weeks cholecystectomy |
| Atrial fibrillation/MI/Angina | 3 weeks post-varicose vein surgery |
| Pulmonary embolism/Fractured neck of femur/Back pain | 3 weeks after non-specific abdominal pain |
| Ileostomy flux/Asthma attack | I&D cutaneous abscess |
| Acute exarc. COPD/hernia repair | Colonoscopy |
| Left axillary abscess | I&D right axillary abscess |
| Fractured neck of femur/angina | Inguinal hernia repair |
Re-admission diagnosis between slash marks represents a different patient.
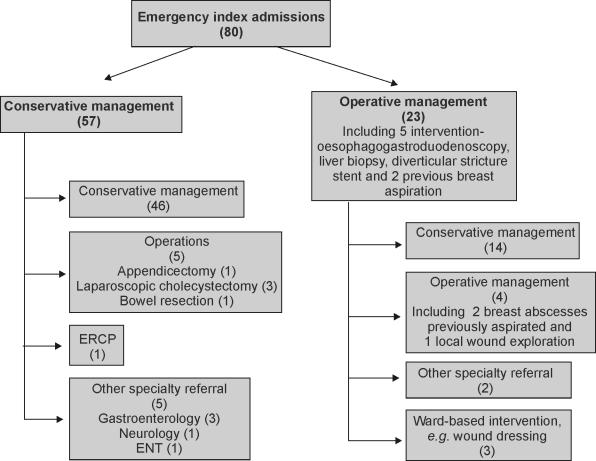
There were 103 ‘genuine’, unplanned re-admissions, consisting of 55 men and 48 women, average age 45.5 years (Fig. 1). Of these, 80 re-admissions occurred after an index emergency admission, during which 57 patients had non-operative management and 23 had operative management. The 42 re-admissions after non-operative emergency admission management involved patients who had chronic or recurrent symptoms (Table 2), of whom 19 were on waiting lists for definitive intervention. On re-admission, 7 patients had definitive operative management (bowel resection, appendicectomy, ERCP, endoscopic stricture dilatation, laparoscopic cholecystectomy [3]; Fig. 2).
Figure 1.
Distribution of all PAS-generated unplanned general surgical re-admissions generated after case note review.
Table 2.
Management of patients re-admitted with recurrent/chronic problems after non-operative index emergency index admission.
| Index admission diagnosis | n | Re-admission management |
|---|---|---|
| Non-specific abdominal pain | 11 | Appendicectomy (1), other specialties (3) |
| Diverticulitis | 1 | |
| Adhesive small bowel obstruction | 3 | Laparotomy and small bowel resection (1) |
| Inflammatory bowel disease – colitis | 1 | |
| Constipation | 1 | |
| Dyspepsia | 1 | OGD |
| Fistula-in-ano | 1 | |
| Gallstones | 9 | Laparoscopic cholecystectomy (2), ERCP) (1) |
| Hepatitis/abdominal pain and mild jaundice | 2 | Liver biopsy |
| Pancreatitis | 7 | Laparoscopic cholecystectomy (1) |
| Pseudo-obstruction | 2 | |
| Chronic colostomy symptoms | 1 | Laparotomy (1) |
| Ileostomy complications | 1 | |
| Crohn's perineum | 1 |
Blank spaces indicate non-operative/conservative management.
Figure 2.
Management pathway of re-admitted patients after an index emergency admission.
Theatre-based procedures were required for 4 re-admissions, non-theatre-based procedures (e.g. wound dressings, etc.) for 3 re-admissions, while the rest had symptom management only (Table 3).
Table 3.
Diagnosis and management of patients re-admitted after operative index admission
| Index operation | n | Re-admission diagnosis | Re-admission management |
|---|---|---|---|
| OGD | 2 | For observation ?perforation | |
| APPENDICECTOMY | 5 | Wound infection, pain, DVT | Wound dressing (1) |
| AXILLARY ABSCESS (I & D) | 3 | ||
| Inguinal hernia repairs (1 recurrent) | 3 | Scrotal haematoma (1), wound ooze (1), pneumonia (1) | |
| BREAST ABSCESS I & D | 2 | Review post-aspiration | 2 Incision & drainage |
| Breast lumpectomy | 1 | Haematoma | |
| DIVERTICULAR STRICTURE STENTING | 1 | Perforation | Hartmann's procedure (1) |
| Cholecystectomy | 4 | Choledochoduodenal fistula (1), postoperative pain (3) | 1 Re-exploration |
| Haemorrhoidectomy | 2 | Postoperative pain | |
| INCISIONAL HERNIA REPAIR | 1 | Seroma | |
| Lipoma excision | 2 | Wound infection | Wound drainage (1) |
| REPAIR OF PERFORATED DUODENAL ULCER | 2 | Wound infection | Wound dressing (1) |
| PERI-ANAL ABSCESS (I & D) | 2 | Recurrence | EUA + drainage (1) |
| Perineal sinus | 1 | Discharge | EUA (1) |
| Pilonidal sinus | 3 | Wound infection | Abscess drainage (1) |
| PILONIDAL ABSCESS (I & D) | 1 | Wound discharge | |
| Delormes procedure | 1 | Urinary retention | |
| Umbilical hernia repair | 1 | Wound infection | |
| LAPAROTOMY | 4 | Wound infection, pain, sinus (1) | Wound dressing (1) |
| Colostomy | 1 | Colostomy prolapse | Manipulation (1) |
| Parathyroidectomy | 1 | Hypocalcaemia | |
| Liver biopsy | 1 | Post-liver biopsy sepsis | |
| Colectomy | 1 | Small bowel obstruction | |
| Laparotomy/adhesiolysis | 1 | Colicky abdominal pain |
Emergency admissions in uppercase.
Non-theatre intervention at re-admission in italics.
There were 23 re-admissions following an index elective admission. Of these, 4 required operating theatre based intervention, 1 had ward-based intervention and the rest had symptom management only.
Overall, 58 (56%) of all ‘genuine’ re-admissions had recurrent or chronic symptoms (in-patient or out-patient management of symptoms for at least a year), while almost a quarter {25 [24%]) occurred in patients who were already on waiting lists for operations, special pre-operative tests, or intervention. These included patients who were waiting for pre-operative investigations, special tests and/or surgical procedures, e.g. MRCP/ERCP/bile duct stent/cholecystectomy etc. for unresolved pre-/postoperative symptoms or complications.
Postoperative complications accounted for 46 (45%) of all ‘genuine’, unplanned re-admissions, of which 14 (14%) required further intervention. Operating theatre intervention occurred in 8 (8%).
Discussion
This study demonstrates that in its ‘raw’ form, hospital coded information database-generated data may not be accurate enough for unplanned re-admission data analysis.
It unfortunately allows inclusion of unrelated admissions (including accidents, and early planned investigations/surgery) occurring within the 28-day post-discharge period. For example, admission for fractured neck of femur within 28 days of elective inguinal hernia repair or planned emergency ward reviews, e.g. ‘early’ planned hernia repair and endoscopy.
While it is likely that these errors in the information database are wide-spread in the NHS, the magnitude may vary between hospital trusts (perhaps even with time) and may lead to breach(es) of set targets and (any consequent) penalties.
Our study also confirms previous reports8 of low re-admission rates (< 2% during the period of this study) after elective surgery (including day-case surgery and accelerated discharge following major surgery).
Re-admissions after emergency index admission as a whole, and after an operative emergency index admission were significantly higher at 7% and 6%, respectively, in this study (see Table 4 for breakdown of total general surgical during admissions during study period). This may be partly explained by the fact that many patients did not have definitive management on index emergency admission. For example, cholecystectomy at emergency index admission may have reduced re-admissions among patients with acute pancreaticobiliary disease (at 12, the commonest single cause of re-admissions).9
Table 4.
Distribution of all general surgical admissions during study period
| Elective | Day-case | Emergency | |
|---|---|---|---|
| Operative | 887 | 565 | 357 |
| Non-operative | 843 | ||
| Total | 1452 | 1200 | |
Closer scrutiny of the higher re-admission rate (6%) following operative management at index emergency admission is also revealing. It shows that the majority (18 of 23) probably required no re-admission, as only symptom or minor non-interventional management (e.g. general or specialist nursing advice, analgesia, antibiotics or wound dressing change) was undertaken.
It is, therefore, arguable that timely investigations, easier access to symptom and/or definitive management may significantly reduce re-admissions after index emergency admissions, and of patients with recurrent or chronic symptoms.
Perhaps general surgical patients operated on during emergency admission may also be less prepared (re-assurance, information, telephone access, definitive treatment, etc.) for discharge than after elective admissions.
There was no evidence in this study to suggest that age or sex, discharge from non-surgical ward (outliers), history of psychiatric disease and number of drugs on discharge could be used to predict unplanned re-admission at discharge after a general surgical admission.
References
- 1.Weissman JS, Ayanian JZ, Chasan-Taber S, Sherwood MJ, Roth C, Epstein AM. Hospital re-admissions and quality of care. Med Care. 1999;37:490–501. doi: 10.1097/00005650-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Jimenez-Puente A, Garcia-Alegria J, Gomez-Aracena J, Hidalgo-Rojas L, Lorenzo-Nogueiras L, Perea-Milla-Lopez E, et al. Readmission rate as an indicator of hospital performance: the case of Spain. Int J Technol Assess Health Care. 2004;20:385–91. doi: 10.1017/s0266462304001230. [DOI] [PubMed] [Google Scholar]
- 3.Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–24. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 4.Roland M, Dusheiko M, Gravelle H, Parker S. Follow up of people aged 65 and over with a history of emergency admissions: analysis of routine admission data. BMJ. 2005;330:289–92. doi: 10.1136/bmj.330.7486.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boockvar KS, Halm EA, Litke A, Silberzweig SB, McLaughlin M, Penrod JD, et al. Hospital re-admissions after hospital discharge for hip fracture: surgical and nonsurgical causes and effect on outcomes. J Am Geriatr Soc. 2003;51:399–403. doi: 10.1046/j.1532-5415.2003.51115.x. [DOI] [PubMed] [Google Scholar]
- 6.Mezei G, Chung F. Return hospital visits and hospital re-admissions after ambulatory surgery. Ann Surg. 1999;230:721–7. doi: 10.1097/00000658-199911000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and re-admissions after same day surgery and associated costs. J Clin Anesth. 2002;14:349–53. doi: 10.1016/s0952-8180(02)00371-9. [DOI] [PubMed] [Google Scholar]
- 8.Delaney CP, Fazio VW, Senagore AJ, Robinson B, Halverson AL, Remzi FH. ‘Fast track’ postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg. 2001;88:1533–8. doi: 10.1046/j.0007-1323.2001.01905.x. [DOI] [PubMed] [Google Scholar]
- 9.Lai PB, Kwong KH, Leung KL, Kwok SP, Chan AC, Chung SC, et al. Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 1998;85:764–7. doi: 10.1046/j.1365-2168.1998.00708.x. [DOI] [PubMed] [Google Scholar]