Abstract
INTRODUCTION
This study was designed to: (i) determine if the priority of referral letters by general practitioners to a plastic surgery skin lesion clinic adhered to the national guidelines, what happened to these patients, and what was the histological diagnosis; and (ii) analyse whether the prognosis at diagnosis of malignant melanoma had improved since the introduction of the 2-week wait for patients with suspected cancer.
MATERIALS AND METHODS
The study involved a prospective audit questionnaire, retrospective note review and histology report review in the Plastic Surgery Department in a district general hospital and their ‘bespoke’ out-patient clinics.
RESULTS
Of 202 referral letters, 58 (29%) were referred as 2-week cancer referrals of which 13 (22%) suggested diagnoses that did not fall within the guidelines, and 11 gave no diagnosis. In addition, 84 (42%) had no indication of priority, though the text may suggest the need for it, either explicitly or implied. The prognostic indices for malignant melanoma have not altered since the 2-week wait rule has been implemented.
CONCLUSIONS
The guidelines are not being adhered to, thus patients with benign lesions are being given undue priority. The history and examination of skin lesions given in the referral letters is insufficient to allow the consultant to prioritise. Since the 2-week rule has be implemented, malignant melanomas have not been diagnosed at an earlier stage.
Keywords: Questionnaire, Skin lesion clinic, GP recommendations, Prioritisation
In June 2000, the UK Government published the NHS plan. One of its aims was to improve the quality of the cancer services. To this end, national standards were introduced which included the target of a hospital appointment being offered within 2 weeks of a general practitioner's decision to refer patients who may have cancer. The introduction was staged, and for skin malignancies the target started in October 2000. Basal cell carcinomas do not count as cancer in this context, so urgent referrals are appropriate only for patients with suspected squamous cell carcinoma (SCC) and malignant melanoma (MM). The system differs from the existing procedure in that the onus is on the GPs to decide if a 2-week-wait is appropriate, not the consultant who reads the referral letter.
The UK Department of Health (DH) has made information available on how to achieve these targets. For GPs, guidelines in the form of a booklet1 and wall-charts2 have been developed to indicate what signs and symptoms cause concern for referral within the 2-week-wait framework. For the trusts, referral forms have been devised that can be adapted locally and then distributed to GPs.
We were concerned about whether these targets were achievable. In particular, there was a perception that the referral rates were increasing and that this could put an unacceptable workload on the consultants, especially if the referrals were disproportionally 2-week-waiters. Although the onus is on the GP to decide whether the case is urgent or not, we wanted to see if there is enough information in the letters to decide on the priority, because frequently the priority is not explicitly requested in the referral letter. Coxon and others3 investigated GP referral letters to a urology department that stated that the patient had signs or symptoms that were included in the referral guidelines for criteria warranting urgent referral. Only 13% of those that complied with the criteria were marked as urgent or see within 2 weeks.
Patients and Methods
Our plastic surgery department has two consultants, who attend three dedicated skin lesion clinics each month. Additionally, they each have two or three general plastic surgery clinics every week. In an attempt to investigate the perception that the referral rate was increasing, the number of patients attending skin lesion clinics and the number of patients who were referred to plastic surgery out-patient clinics at the base hospital (Sandwell General Hospital) over the previous 4 years was found from the hospital computer system. The main study had three parts.
Prospective proforma
For a period of 3 months, a simple tick-box proforma was completed in clinic for every new patient who was seen regarding a skin lesion. The information included the patient's name and date of birth, date of the consultation, whether the referral letter stated or implied that the lesion was malignant or not, whether the consultant thought that the lesion was malignant or not, the outcome of the consultation, what the recommended treatment plan was and whether the priority request by the referral letter was appropriate. The study was held over 15 weeks, as we wished to have at least 100 patients seen by each of the consultants.
Case note review
To analyse the accuracy of the consultant's opinions, the case notes of the patients who had been seen in the prospective stage of the study were reviewed. If applicable, the following data were recorded: the date of surgery, histology results and any other notable information within the notes. Information missing from the notes was gleaned from the hospital or pathology information systems.
Histology review
As a final part of the study, data were gathered from the pathology department. The reports were reviewed of patients who had had a histology result of MM, as identified by the SNOMED (Systematized Nomenclature of Medicine) coding system, in the 30 months preceding and 30 months after October 2000. In particular, Clark's level and Breslow thickness were recorded.
Results
The number of patients being referred to plastic surgery out-patients' department (OPD) and those attending the skin lesion clinics is shown in Figure 1. The value of these figures is limited. The number of patients referred to the OPD includes patients who are not being seen regarding a skin lesion and the numbers do not include the clinics performed at peripheral hospitals. The number attending the skin lesion clinics are relatively static because the clinics have been full and often overbooked ever since their inception.
Figure 1.
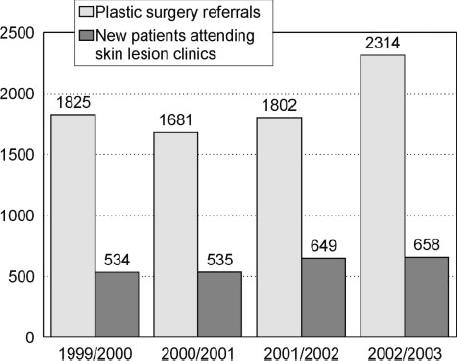
Number of patients each year.
Prospective proforma/case note review
A total of 210 proforma were received of which six were excluded from the study: two were referrals with recurrent lesions, one was filled in error, and three were too incomplete for analysis. The notes could not be found for two patients, but sufficient information was gained from the hospital letters on computer, the completed proforma and pathology reports.
The average age was 58 years and there were 83 males and 121 females. The recommended outcome of the consultation is shown in Table 1. Of the 204 patients, 56 (27%) had clearly benign lesions, were re-assured and discharged with information about skin lesions and sun advice. However, 139 (68%) were recommended to have surgical intervention, of whom nine patients had a biopsy taken in the clinic.
Table 1.
Recommendations at initial consultation
| Recommendation | n | |
|---|---|---|
| Surgery recommended | 130 | |
| For diagnosis | 89 | |
| For symptoms | 37 | |
| For cosmesis | 4 | |
| Biopsy in clinic | 9 | |
| Medical treatment | 9 | |
| 5-Fluorouracil | 4 | |
| Cryotherapy | 3 | |
| Other | 2 | |
| Reassured and discharged | 56 | |
The proforma recorded the implied or explicit diagnosis given by the GP in the referral letter. The options were stated to be malignant, stated to be benign, implicitly malignant, implicitly benign or no diagnosis suggested. When comparing the GP's implied or explicit diagnosis in the referral letter, of the 69 patients where the GP thought the lesion was benign, 16 were re-assured and discharged. Forty-three patients had surgery with the specimen being sent for analysis by a histopathologist. The results showed that all but five were benign. There were three malignant, and two pre-malignant specimens. Six of the remaining 10 patients did not attend the day-surgery appointment or declined to go ahead when admitted.
In contrast, of the 123 patients where the GP thought the lesion was malignant, 69 were thought to be clinically benign by the consultants of whom 7 had medical treatment and 36 were simply re-assured and discharged. The remaining 80 were recommended for surgery of whom 15 were for symptomatic lesions. Seven patients did not attend for their surgery. The histology results showed 42 benign lesions, 20 malignant, and 11 premalignant (for further details see Table 2).
Table 2.
Consultant's diagnosis versus that of GP
| Consultant's diagnosis | |||||
|---|---|---|---|---|---|
| GP letter | No lesion | Lesion benign | Lesion malignant | Unable to classify | Total |
| Stated to be benign | 51 | 3 | 4 | 58 | |
| Implicitly benign | 9 | 1 | 1 | 11 | |
| Stated to be malignant | 5 | 27 | 31 | 11 | 74 |
| Implicitly malignant | 3 | 34 | 5 | 7 | 49 |
| No diagnosis | 1 | 5 | 5 | 1 | 12 |
The case note review found 202 referral letters, of which 73 were on the locally produced skin lesion referral form. The priority of the referral was not explicit on 84; furthermore, 21 (10% of all referrals) of these letters simply did not have enough information to allocate a priority. There was neither a suggested differential diagnosis, nor enough history to gather one. Of patient referral letters, 58 were labelled as urgent or under the 2-week rule. Of these, 40 (69%) were considered inappropriate by the consultants, that is, the lesion was clearly benign or a classical BCC. Of the 58 urgent and 2-week-wait patient referral letters, 11 did not give a suggested diagnosis, and 13 had suggested diagnoses that do not fall within the guidelines for urgent referral (such as a BCC, see Table 3). In the context of an urgent request, a changing mole could be interpreted as a possible MM. In this series, there were 26 patients referred urgently with a possible MM. Fifteen of these 26 patients have had their lesions excised; the rest had clinically benign lesions and were re-assured. There were no melanomas, nor SCCs, just two excised BCCs in this group. A further 41 letters, with a priority other than urgent, gave a history of changing, itchy or bleeding mole, or questioned whether the patient had a malignant melanoma. Ten of these had an explicit 6-week priority requested, seven were routine requests and the remaining 24 had no priority indicated (more details in Table 3). Table 4 shows the ideal referral priority (once the histology is known, or from the consultant's clinical diagnosis where no surgery has been done) against referral priority requested by the GP.
Table 3.
The GP's most significant diagnosis versus the priority requested
| GP priority request | ||||
|---|---|---|---|---|
| GP diagnosis | 2-weeks/urgent | 6-weeks/other | Routine | None |
| MM/?MM | 20 | 8 | 1 | 1 |
| Cancer | 2 | 1 | ||
| SCC/?SCC | 6 | 5 | 2 | |
| Bowen's/?Bowen's | 1 | 1 | 2 | |
| BCC/?BCC | 9 | 13 | 14 | |
| Worrying mole | 6 | 2 | 6 | 23 |
| Benign | 3 | 8 | 7 | 20 |
| No information | 11 | 6 | 3 | 21 |
Table 4.
Expected referral priority in light of histology or consultant's diagnosis versus the priority requested by GP
| GP priority request | ||||
|---|---|---|---|---|
| Final diagnosis | 2-weeks urgent | 6-weeks/other | Routine | None |
| MM/SCC/keratoacanthoma | 2 | 1 | 4 | |
| BCC/other malignancy/premalignancy | 13 (4) | 15 (3) | – | 13 (1) |
| Benign lesion/gone by OPA | 43 (18) | 27 (14) | 17 (10) | 69 (32) |
Overall, 139 patients were recommended to have surgery or a biopsy in clinic for diagnosis. Of these, 124 patients had histology results available, as seen in Table 5. Two of the remaining 15 patients had had skin tags removed with no histology requested; nine did not attend the unit for their surgery and four refused to come back because the lesion had ‘dropped off’.
Table 5.
Histology results
| Histology | n |
|---|---|
| SCC | 5 |
| BCC | 18 |
| Bowen's disease | 9 |
| Malignant, other | 3 |
| Naevus | 25 |
| Seborrhoeic keratosis | 24 |
| Actinic keratosis | 3 |
| Viral wart | 3 |
| Cyst | 4 |
| KA | 2 |
| Naevus sebaceous | 1 |
| Benign, other | 27 |
The consultants' diagnoses (categorised in the proforma as ‘malignant’, ‘benign’ or ‘unable to classify’) compared with the histological results is shown in Table 6.
Table 6.
Consultant diagnosis against histology
| Consultant's diagnosis | |||
|---|---|---|---|
| Histology | Lesion benign | Lesion malignant | Unable to classify |
| Malignant | 3 | 20 | 5 |
| Benign | 56 | 11 | 16 |
| Premalignant | 2 | 10 | 1 |
Histology review
Using the SNOMED system, 94 patients were identified as having had malignant melanoma in the 30 months prior to and after October 2000. Of these, 10 patients were excluded: five patients had had their surgery prior to referral to Sandwell General Hospital, two were incision or biopsies of very large lesions and had their definitive surgery elsewhere, and three patients had only melanoma in situ.
Of the remaining, 44 patients were identified as having had a primary MM excised in the 30 months before October 2000, and 40 patients in the 30 months after October 2000. Demographic data and the median Breslow and Clark's thicknesses are illustrated in Table 7. There was no statistical difference in the demographic or prognostic indicators following the introduction of the 2-week-wait.
Table 7.
Results of histological review
| Before October 2000 | After October 2000 | |
|---|---|---|
| Number | 44 | 40 |
| Male:female | 18:26 | 16:24 |
| Median Clark's | 3 | 4 |
| Mean (SD) Clark's | 3.9 (0.9) | 3.51 (1.0) |
| Median Breslow | 1.2 | 2.5 |
| Mean (SD) Breslow | 2.3 (2.8) | 3.51 (4.2) |
Discussion
While it is laudable to have established aims within the NHS, it is difficult to believe that some of these are not open to abuse. This study has shown that a large proportion (29%) of referrals to our unit had been requested as urgent. The pathological diagnoses showed only 35 malignancies, of which only five were a cancer appropriate for the 2-week-wait according to the NHS guidelines.1 The NHS plan gives the responsibility for deciding the clinical priority to the referring GP. This is appropriate, since they are the clinician who has the greatest information about the patient. However, it also gives rise to a few concerns. First, it assumes that the diagnostic accuracy of the referring practitioner is acceptable. Other studies have shown a diagnostic accuracy of skin lesions referred to skin cancer clinic as high as 100%4 for melanoma, but our sample showed a diagnostic accuracy of only 41% (to the simple categories of benign or malignant). The false negative rate being a manageable 1.6%, but the false positive rate of 84% makes this system difficult to manage. The DH have estimated that 1 in 24 referrals would be a MM or SCC and that an average district general hospital would have 12 such referrals each week.1 This in itself represents a significant workload, but is sometimes shared between plastic surgeons and dermatologists. Our department saw 58 two-week referrals over 15 weeks, i.e. four each week. This does not seem excessive until one understands that the consultants have clinic time for only one skin lesion clinic each a month, and not enough personnel to cope with the surgical implications of these extra patients.
A second concern of this referral system is that it could lead to confusion of clinical responsibilities. For example, if the referral letter suggests a significant pathology, such as a MM, but there is no request for urgency, where does the responsibility for that patient while he/she is awaiting an out-patient appointment lie? Should a consultant increase the priority of a young adult referred with a history of, for example, a bleeding mole, when the GP has requested none, or marked the letter as routine? If this had been the case in our series, an even higher proportion of referrals would have to be treated as 2-week-waiters. This could overwhelm our service and no doubt many others, as Coxon et al.3 have discussed.
Locally-produced specific guidelines for urgent referrals may reduce the inappropriate referral rate. However, the system has to be fine-tuned so that it picks up the patients with cancer early, without being overwhelmed by the worried well, which again would lead to excessive waits with inevitable increased patient anxiety.5 Guidelines that are simple enough to use will always include patients that may later seem inappropriately referred and miss patients with more subtle signs that prove to have malignancy.6 These routine patients may have to wait longer than with the previous system.7 As in our study, others have shown that a significant proportion of urgent referrals do not meet the criteria or guidelines for such a priority.8,9
Our study showed no change in the stage of MM at diagnosis following the introduction of the 2-week rule. The evidence for improved survival rates when the patient is seen within 2 weeks is flimsy,6,10,11 though there must be a limit to this and it has been shown that a 3-month delay with symptoms of breast cancer does significantly alter survival.12 In many cases, most of the delay is prior to presentation to a clinician, so patient education is crucial for overall cancer survival rates to improve.
Osborne et al.13 have shown how difficult it is to diagnose malignant melanoma with any accuracy, and recommended the use of MacKie's seven-point check-list score to ensure an acceptable pickup rate for MM.14 The DH skin lesion referral form uses most of the seven points in its tick-boxes, but does not go as far as dividing the system into major and minor signs and accounting a score.15 Interestingly, the DH Guidelines for Urgent Referral of Patients with Suspected Cancer suggests that urgent referral should be made for patients with pigmented lesions with simply one or more signs of a list that includes simple inflammation.1,2
It has been estimated that 10–25% of a GP's workload is relating to skin conditions, and yet few GPs have had any time in dermatology training within the hospital setting. As a result 60–95% of referrals to dermatologists under the 2-week cancer rule are benign.16 The report from the All Party Parliamentary Group on Skin published in 2003 repeatedly reports GP's lack of ability to manage skin disease and malignancies appropriately and it emphasised the lack of training available within GP training schemes.16 It also states that: ‘Clinicians are generally dismayed by the quality of referrals from GPs in primary care …[and that] a lack of training in dermatology means that GPs have poor diagnostic skill in this area’. Also, ‘GPs are referring patients with a condition they think might be skin cancer although a proper case history may suggest otherwise. …GPs may be referring people with benign lesions in order to avoid complaints by patients’. Our study concurs with all these points.
Conclusions
This study has demonstrated that although there is a locally-produced referral form, its uptake is poor, and the DH cancer referral guidelines are disregarded. Freehand letters tend to have insufficient information to establish whether the guidelines have been considered, and often there is a request for specific priority thus preventing the consultant deciding when to see the patient. A cancer referral will aim to be seen within 2 weeks, but this requires the GP to request an urgent referral and to get it to the hospital within 24 h. In many cases, urgency is not requested in the referral despite the guidelines being met. By leaving the decision to the consultant, unless sufficient information is in the referral letter, the patient will not be seen within 2 weeks. Furthermore, the 2-week priority is being abused to refer patients outside the guidelines. This probably means that appointments are delayed for patients with non-urgent conditions and, more disturbingly, delaying patients with malignant conditions but whose referral letter was sent without a request for urgency.
Acknowledgments
The authors thank Mr Michael Porter, Consultant Plastic, Hand and Reconstructive Surgeon, for his ideas and for contributing his patients, Penny Harrison of clinical effectiveness and Karen McLeod of histopathology, for her IT skills.
References
- 1. Referral Guidelines for Suspected Cancer at < http://www.dh.gov.uk/assetRoot/04/01/44/21/04014421.pdf> [accessed 19 November 2005]
- 2. Guidelines for Urgent Referral of Patients with Suspected Cancer < http://www.dh.gov.uk/assetRoot/04/01/44/22/04014422.pdf> [accessed 19 November 2005]
- 3.Coxon JP, Harris HJ, Watkin NA. A prospective audit of the implementation of the 2-week rule for assessment of suspected urological cancers. Ann R Coll Surg Engl. 2003;85:347–50. doi: 10.1308/003588403769162486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen SC, Bravata DM, Weil E, Olkin I. A comparison of dermatologists' and primary care physicians' accuracy in diagnosing melanoma. Arch Dermatol. 2001;137:1627–34. doi: 10.1001/archderm.137.12.1627. [DOI] [PubMed] [Google Scholar]
- 5.Williams RW, Hughes W, Felmingham S, Irvine GH. An audit of two week wait referrals for head and neck cancer. Ann R Coll Surg Engl (Suppl) 2002;84:304–6. [Google Scholar]
- 6.Jones R, Rubin G, Hungin P. Is the two week rule for cancer referrals working? BMJ. 2001;322:1555–6. doi: 10.1136/bmj.322.7302.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreea S, Green J, MacFie J, Mitchell CJ. Impact of the two week waiting time standard on the gastroenterology service of a district general hospital (abstract) Gut. 2001;48(Suppl 1):A3. [Google Scholar]
- 8.Eccersley AJ, Wilson EM, Makris A, Novell JR. Referral guidelines for colorectal cancer – do they work? Ann R Coll Surg Engl. 2003;85:107–10. doi: 10.1308/003588403321219885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adair A, Bennis M, Clifton MA. Referral guidelines for colorectal cancer – do they work? Ann R Coll Surg Engl. 2004;86:144. doi: 10.1308/003588404322827581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiran PR, Glass RE. Duration of symptoms and spread of colorectal cancer. A short history does not mean early disease. Ann R Coll Surg Engl. 2002;84:381–5. doi: 10.1308/003588402760978157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cancer Guidelines Sub–Group of the COG. Guidance on commissioning cancer services: Improving outcomes in colorectal cancer: the manual. Leeds: NHS Executive; 1997. [Google Scholar]
- 12.Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999;353:1119–26. doi: 10.1016/s0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- 13.Osborne JE, Bourke JF, Graham-Brown RAC, Hutchinson PE. False negative clinical diagnoses of malignant melanoma. Br J Dermatol. 1999;140:902–8. doi: 10.1046/j.1365-2133.1999.02823.x. [DOI] [PubMed] [Google Scholar]
- 14.MacKie RM. Skin Cancer: An Illustrated Guide to the Aetiology, Clinical Features, Pathology and Management of Benign and Malignant Cutaneous Tumours. 2nd edn. London: Martin Dunitz; 1996. [Google Scholar]
- 15. Blankshire Cancer Network: Suspected Skin Cancer Referral Form at < http://www.dh.gov.uk/assetRoot/04/06/67/08/04066708.pdf> [accessed 19 November 2005]
- 16.All Party Parliamentary Group on Skin. Report on the enquiry into the treatment, management and prevention of skin cancer. London: All-Party Parliamentary Group on Skin; 2003. pp. 4.9–4.12. paragraphs. [Google Scholar]


