Abstract
Dupuytren's disease is a progressive fibroproliferative disorder of an unknown origin affecting the hands causing permanent flexion contracture of the digits. Significant risk factors for development of Dupuytren's disease include old age, male sex, white northern European extraction, presence of positive family history of Dupuytren's disease, and diabetes mellitus. The disease also seems to deteriorate rapidly in those cases showing young age of onset and additional fibromatosis affecting the back of the hands, soles of the feet and the penis. Although there is no cure, patients with Dupuytren's disease of the hand may gain a significant functional benefit following surgical improvement or correction of the deformity. With realistic expectations, timely and appropriate surgical technique in a specialist centre, and attention to postoperative recovery and rehabilitation (occupational therapy and physiotherapy support), a beneficial outcome can be achieved in most cases.
Keywords: Dupuytren's disease, Contracture, Diagnosis, Assessment, Treatment, Referral
Dupuytren's disease is so common that every doctor will encounter it and yet there is confusion about what to tell the patient, when to refer and what treatment is best. Dupuytren's disease is a benign nodular fibromatosis, affecting the hands, named after Baron Guillaume Dupuytren who was the first to operate on the condition.1 Dupuytren's disease leads to shortening of the skin anchoring ligaments of the palm (palmar fascia), which may lead to contracture of the digits. Dupuytren's disease may be familial and is extremely common in northern Europeans.2,3 Treatment is by surgery, the main indications being progression of contracture, or functional disability. There is a high rate of recurrence.4
This article is based on the authors' personal scientific and clinical experiences in the investigation and treatment of Dupuytren's disease and on a comprehensive review of the literature of the condition in the English language. Key terms including, Dupuytren's disease, Dupuytren contracture, palmar fibromatosis, diagnosis, prevention, management and treatment were used to search for relevant articles in the peer-reviewed medical literature.
What to tell the patient?
Demographics of Dupuytren's disease
The results of various epidemiological studies on Dupuytren's disease have produced conflicting evidence as to causative factors and links to other disease processes.
IS DUPUYTREN'S DISEASE INHERITED?
The incidence certainly seems to be highest in patients of northern European extraction, and rare in dark-skinned individuals,5–7 the prevalence ranging from 2% to 42% in diverse Caucasian populations.7 Dupuytren's disease may be a familial disorder with reports in identical twins2 although many patients are unable to identify an affected relative. With different inheritance patterns and variable levels of penetrance and gene expression, it is unclear whether Dupuytren's disease is a simple monogenic or polygenic condition.2 In one study, the incidence in relatives when reported by patients was 16%, but this increased to 68% following examination of family members.8 Little statistical value can, therefore, be placed on the familial incidence of Dupuytren's disease as suggested by history alone.
POSSIBLE NORDIC ORIGIN OF THE DISEASE
The known geographical distribution has suggested that the Norsemen in the Viking age were responsible for spreading Dupuytren's disease. The Nordic theory of origin is supported by high incidence of the condition in Denmark and those parts of the UK which faced the Norsemen, namely north of England and the north and west of Scotland, both of which were invaded and subsequently colonised.9
EFFECT OF AGE AND SEX
Dupuytren's disease is very uncommon in the teens and twenties but the incidence rises in each decade thereafter.10 Consequently, one can expect an increasing incidence as the ageing population increases. Early age of onset of Dupuytren's disease is less favourable and generally has a higher rate of disease progression and recurrence, but there are no exact rules and some early-onset cases have a relatively benign course. Although the incidence of Dupuytren's disease is higher (5–15 times) in men, the disease is less severe in women; therefore, it may go unnoticed until later in life.11,12 A number of authors have questioned these gender differences and stated that the difference in prevalence is age-dependent and, by the eighth and ninth decade of life, the sex ratio for affected individuals approaches one.12
IS THERE AN IDENTIFIABLE CAUSE?
Dupuytren's disease has been variously reported to be associated with a host of causative factors and diseases but, in most cases, the evidence is disputed by different studies. There seems to be a fairly well-established link with diabetes mellitus, although such cases tend to have more nodules and less contraction.13 There is no evidence that Dupuytren's disease is associated with liver disease.14,15 The literature is evenly split as to whether there is an association with epilepsy (or epileptic medication), alcohol intake or cigarette smoking. There is certainly no evidence that a modification in these factors will influence the course of the patient's disease. Over the past 180 years since Dupuytren, suggested links between Dupuytren's disease and the fashionable pathological concepts at the time (including syphilis, tuberculosis, high serum lipids and HIV positivity) can chart the history of medicine during this period. There is clearly no simple answer. There are many teetotal, non-smoking Dupuytren's disease patients who will be offended by indelicate enquiries! And there is no indication to investigate the patient for any of the reported associated conditions unless otherwise indicated.
Nor is there any clear link to work-related activities, including (much quoted but not substantiated) frequent use of heavy, vibrating machinery, and increased risk of developing Dupuytren's disease.16,17 Patients can, therefore, be re-assured that the problem is not due to something they are doing – whether at work or play. In addition, it is not part of a systemic disease process; however, a worrying statistical finding in recent studies has been an increased general mortality of individuals with advanced Dupuytren's disease when reviewed some years later, where 42% of the excess in mortality could be attributed to cancer deaths.18,19 This needs further investigation. At present patients should simply be advised that we do not know the cause of this condition.
WHAT IS THE KNOWN DISEASE PROCESS?
The disease mainly affects the bands of fascial fibres running longitudinally in the subcutaneous tissues of the palm. The palmar fascia or aponeurosis (the normal anatomical bands which anchor the skin of the palm) become thick fibrous cords causing digital contractures.20
The basic pathophysiological process in Dupuytren's disease is similar to wound healing involving fibroblast proliferation, collagen deposition and myofibroblast contraction driven by various growth factors such as transforming growth factor beta. Dupuytren's disease does display features in common with a neoplastic process, including distinct chromosomal abnormalities,21,22 high rates of recurrence following surgery, but it is not a cancer or premalignant disease.21–24
Dupuytren's disease can be associated with other fibromatoses including plantar fibromatosis (Ledderhose disease), penile fibromatosis (Peyronie disease), and fibromatosis of the dorsum of the proximal interphalangeal (PIP) joints (Garrod's nodules or knuckle pads). The histopathological appearances are indistinguishable from those observed in Dupuytren's disease. It has been suggested that patients with such additional fibromatosis have more recurrences and extensions (new occurrence of disease beyond the area of operation) after surgery.25
When to refer?
The insidious disease process in Dupuytren's disease is often unnoticed by the patient until the disease has suddenly progressed from a simple painless nodule to a severely contracted digit (Fig. 1).
Figure 1.
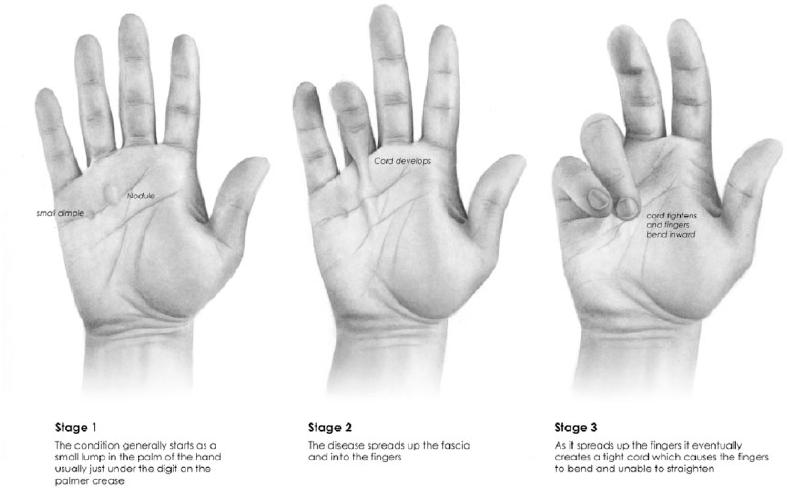
Diagrammatic illustration of clinical presentation in Dupytren's disease; from simple nedule to thick fibrous band formation and finally to finger contracture.
Figure 2.
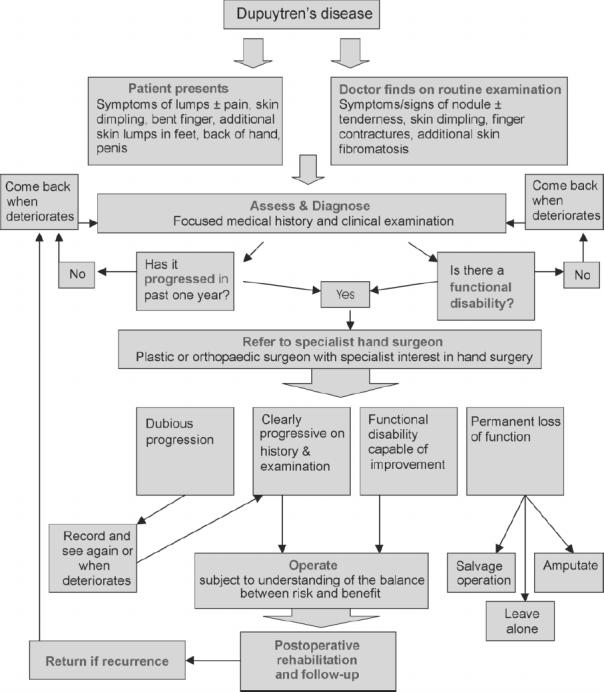
Flow chart for managing patients with Dupuytren's disease from diagnosis to treatment.
The key indications for referral and treatment are:
Definite progression of the contracture, as demonstrated by history (what has happened in the past year?) or repeated examination.
Functional disability, which can manifest at different stages depending on how exacting the patient's hand use may be.
Once contracture develops, the fingers get in the way affecting simple everyday tasks such as face washing (poking the eye with affected digit), combing hair, putting the hand in a pocket or glove, driving or playing sports. Dupuytren's disease often develops in both hands (hand dominance is unrelated) and most commonly affects the ring fingers and the little fingers, followed by the index, the middle fingers and the thumb. disease severity and impact on life is variable but worse in young individuals with aggressive disease. The term diathesis is often applied to such young individuals ± additional sites of fibromatosis and ± family history of Dupuytren's disease, but defies precise definition.23
Early referral is beneficial as it allows the surgeon to judge the rate of progression of the disease or, alternatively, the GP may monitor progress over a period of time. Metacarpal phalangeal joint (MCPJ) contracture can be corrected even at a late stage but the PIPJ is likely to remain stiff if it is allowed to progress too far.
Assessment of patient with suspected Dupuytren's disease
In the primary care setting, the diagnosis is generally a spot diagnosis, which experience of referral letters has often shown to be correct. While there are other causes of hand contracture, they do not develop nodules in the palm.
A thorough patient assessment starts with a focused medical history taking note of the following relevant information: age, gender, ethnicity, profession, manual hobbies, handedness, family history of Dupuytren's disease, age of onset, symptoms, rate and course of disease progression, previous treatments by other practitioners, recurrence, and patient's medical history (particularly ask for presence of diabetes mellitus, epilepsy, drug history and psychosocial history). This information is not to establish a cause but to predict how Dupuytren's disease will affect the patient's occupational and recreational pursuits; family history will reveal the expectations of surgical outcome.
Physical examination is the mainstay of diagnosis for determining the presence of Dupuytren's disease. The following features should be noted on clinical examination of the patient:
Sites of nodules (tender/non-tender) and bands/contracted cords, skin pitting and dimpling in palm and digits.
Degree of skin involvement.
In palmar/digital contracture, measure MCPJ angle (active and passive range of motion).
In palmar/digital contracture, measure PIPJ angle (active and passive range of motion).
Knuckle pads (Garrod's nodes) – firm dermal nodule located on the extensor aspect of the PIP joint or MCPJ.
Plantar nodule(s) (Ledderhose's disease) – tender/non-tender in the foot.
Secondary Boutonniere, swan neck or other deformity.
In case of disease recurrence: also note the following:
-
8.
Previous surgical scars.
-
9.
Sensation in palm and tips/sides of digits.
-
10.
Digital Allen's test (if suspicion of previous vascular injury, warn about possibility of finger loss peri- or postoperatively).
The Hueston Table Top Test is a useful, quick and simple test to stage the disease. Ask the patient to put the hand and fingers prone on a table. The test is positive when the hand will not go flat in active or moderate stage of the disease. The development of Dupuytren's disease can be slow and insidious and is, therefore, difficult to diagnose in its early stages. As the disease is frequently symptomless in its early stages, the doctor may not be consulted until the later stages of disease. Patients presenting with Dupuytren's disease in its advanced stage are much easier to diagnose, although it may already be too late to salvage a severely contracted digit.
How to treat?
Current management of Dupuytren's disease
Although there is no cure for Dupuytren's disease, most patients can gain significant functional improvement following corrective surgery, which is the mainstay of treatment. Indeed, hand function is worsened by increasing deformity in Dupuytren's disease and improved by correction of the deformity.26,27 Satisfactory outcome does not only depend on degree of extension achieved but also on surgical complications and maintenance of some flexion for a functionally useful hand rather than a stiff, straight digit or a vascularly compromised finger requiring amputation. Many surgical operations of different magnitudes are available. One common surgical approach is a limited fasciectomy removing involved fascia. For less extensive cases, fasciotomy (simple division) of contracted fascia may be performed by an open operation or a closed technique. The closed technique has been advocated using a blade or as percutaneous needle fasciotomy. This last technique should only be performed in selected cases and by a surgeon with detailed knowledge of hand anatomy. For more extensive cases or recurrences, both skin and fascia may be removed en bloc (dermofasciectomy) and the wound skin grafted. This may reduce disease recurrence but not its extension.25 There are no routine procedures; therefore, the choice of these three general approaches should be tailored to the needs of individual cases. Distraction devices may be useful in conjunction with surgery to treat Dupuytren's disease, although their effectiveness has not been proven.27 There are few non-surgical options. Corticosteroid injections are sometimes used to treat painful nodules. The medication is injected directly into the affected area.28 Radiotherapy has also been used to prevent disease progression for early stage Dupuytren's disease.29
Non-surgical enzymatic fasciotomy using clostridial collagenase injection into the affected area has shown encouraging clinical results in early trials but is not yet available.30 Recently, despite positive in vitro use of 5-fluorouracil (inhibits myofibroblast activity), a prospective clinical trial showed no significant difference between control and 5-fluorouracil treated digits.31
Postoperative complications include haematoma, skin necrosis, infection, nerve injury, vascular injury, prolonged oedema, reflex sympathetic dystrophy and, rarely, finger loss. However, the most common complication is postoperative joint stiffness and loss of pre-operative flexion, further emphasising the importance of a postoperative rehabilitation programme. There are no proven ways to prevent Dupuytren's disease or limit its progress. Hand therapy and rehabilitation using thermoplastic night splints and regular physiotherapy exercises may aid in the postoperative recovery period. Regardless of the technique, there is a high rate of recurrence following surgical correction, and the patient and general practitioner should be aware of this and not attribute problems to surgical competence.
Conclusions and future perspectives
Dupuytren's disease is a very common condition, which can be diagnosed on the basis of clinical features. Many studies have noted the familial as well as the sporadic nature of Dupuytren's disease, but the exact nature and type of the gene–environment interaction remains unclear. Despite numerous previous studies, the aetiopathogenesis of Dupuytren's disease remains obscure and debate regarding the exact cause of the disease continues. Recent genetic studies have demonstrated a polymorphism in a transcription factor and a novel mitochondrial gene mutation to be associated with development of Dupuytren's disease.32,33 Future non-operative therapies utilising localised novel gene therapies may hold promise for eradication of this disabling disorder. However, until these treatments are proven to be therapeutic, surgery remains the main therapeutic option. More objective and scientific data are certainly needed as many empirical views highlight the muddled thinking which still prevail on pathogenesis and treatment.34
Acknowledgments
Research summarised in this manuscript has been supported by a variety of grants including the Medical Research Council (UK) for which we are grateful.
References
- 1.Dupuytren BG. Permanent retraction of the fingers, produced by an affection of the palmar fascia. Lancet. 1834;ii:222–5. [Google Scholar]
- 2.Burge P. Genetics of Dupuytren's disease. Hand Clin. 1999;15:63–72. [PubMed] [Google Scholar]
- 3.Gudmundsson KG, Arngrimsson R, Jonsson T. Eighteen year follow-up study of the clinical manifestations and progression of Dupuytren's disease. Scan J Rheumatol. 2001;30:31–4. doi: 10.1080/030097401750065292. [DOI] [PubMed] [Google Scholar]
- 4.Leclercq C. Results of surgical treatment. In: Tubiana, et al., editors. Dupuytren's disease. 1st edn. London: Martin Dunitz; 2000. pp. 239–50. [Google Scholar]
- 5.Gudmundsson KG, Arngrimsson R, Sigfusson N, Bjornsson A, Jonsson T. Epidemiology of Dupuytren's disease: clinical, serological, and social assessment. The Reykjavik Study. J Clin Epidemiol. 2000;53:291–6. doi: 10.1016/s0895-4356(99)00145-6. [DOI] [PubMed] [Google Scholar]
- 6.Sladicka MS, Benfanti P, Raab M, Becton J. Dupuytren's contracture in the black population: a case report and review of the literature. J Hand Surg Br. 1996;21:898–9. doi: 10.1016/s0363-5023(96)80211-5. [DOI] [PubMed] [Google Scholar]
- 7.McFarlane RM, Botz FS, Cheung H. Epidemiology of surgical patients. In: McFarlane RM, McGrouther DA, Flint M, editors. Dupuytren's Disease Biology and Treatment. Edinburgh: Churchill Livingstone; 1990. pp. 201–13. [Google Scholar]
- 8.Ling RS. The genetic factor in Dupuytren's disease. J Bone Joint Surg Br. 1963;45:709–18. [PubMed] [Google Scholar]
- 9.Elliot D. The early history of contracture of the palmar fascia. Part 1: The origin of the disease: the curse of the MacCrimmons: the hand of benediction: Cline's contracture. J Hand Surg Br. 1988;13:246–53. doi: 10.1016/0266-7681_88_90078-2. [DOI] [PubMed] [Google Scholar]
- 10.Mikkelsen OA. The prevalence of Dupuytren's disease in Norway. Acta Chir Scand. 1972;138:695–700. [PubMed] [Google Scholar]
- 11.Wilbrand S, Ekbom A, Gerdin B. The sex ratio and rate of reoperation for Dupuytren's contracture in men and women. J Hand Surg Br. 1999;24:456–9. doi: 10.1054/jhsb.1999.0154. [DOI] [PubMed] [Google Scholar]
- 12.Ross DC. Epidemiology of Dupuytren's disease. Hand Clin. 1999;15:53–65. [PubMed] [Google Scholar]
- 13.Yi IS, Johnson G, Moneim M. Etiology of Dupuytren's disease. Hand Clin. 1999;15:43–52. [PubMed] [Google Scholar]
- 14.Attali P, Ink O, Pelletier G, Vernier C, Jean F, Moulton L, et al. Dupuytren's contracture, alcohol consumption, and chronic liver disease. Arch Intern Med. 1987;147:1065–7. [PubMed] [Google Scholar]
- 15.Noble J, Arafa M, Royle SG, McGeorge G, Crank S. The association between alcohol, hepatic pathology and Dupuytren's disease. J Hand Surg Br. 1992;17:71–4. doi: 10.1016/0266-7681(92)90015-t. [DOI] [PubMed] [Google Scholar]
- 16.Thurston AJ. Dupuytren's disease. J Bone Joint Surg Br. 2003;85:469–77. doi: 10.1302/0301-620x.85b4.14215. [DOI] [PubMed] [Google Scholar]
- 17.Burge CP. Dupuytren's disease. J Bone Joint Surg Br. 2004;86:1088. doi: 10.1302/0301-620x.86b7.15766. author reply 1088–9. [DOI] [PubMed] [Google Scholar]
- 18.Gudmundsson KG, Arngrimsson R, Sigfusson N, Jonsson T. Increased total mortality and cancer mortality in men with Dupuytren's disease: a 15-year follow-up study. J Clin Epidemiol. 2002;55:5–10. doi: 10.1016/s0895-4356(01)00413-9. [DOI] [PubMed] [Google Scholar]
- 19.Mikkelsen OA, Hoyeraal HM, Sandvik L. Increased mortality in Dupuytren's disease. J Hand Surg Br. 1999;24:515–8. doi: 10.1054/jhsb.1999.0229. [DOI] [PubMed] [Google Scholar]
- 20.Luck J. Dupuytren's contracture. A new concept of the pathogenesis correlated with surgical management. J Bone Joint Surg Am. 1959;41:635–64. [PubMed] [Google Scholar]
- 21.Sergovich FR, Botz JS, McFarlane RM. Nonrandom cytogenetic abnormalities in Dupuytren's disease. N Engl J Med. 1983;308:162–3. [PubMed] [Google Scholar]
- 22.Wurster-Hill DH, Brown F, Park JP, Gibson SH. Cytogenetic studies in Dupuytren contracture. Am J Hum Genet. 1988;43:285–92. [PMC free article] [PubMed] [Google Scholar]
- 23.Hueston JT. Lessons in Dupuytren's disease. Ann Chir Main Memb Super. 1992;11:349–54. doi: 10.1016/s0753-9053(05)80269-8. [DOI] [PubMed] [Google Scholar]
- 24.Leclercq C. Results of surgical treatment. In: Tubiana R, Mackin EJ, Hurst LC, Leclercq C, Badalamente MA, editors. Dupuytren's Disease. Taylor & Francis; 2000. pp. 239–265. [Google Scholar]
- 25.Abe Y, Rokkaku T, Ofuchi S, Tokunaga S, Takahashi K, Moriya H. An objective method to evaluate the risk of recurrence and extension of Dupuytren's disease. J Hand Surg Br. 2004;29:427–30. doi: 10.1016/j.jhsb.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Sinha R, Cresswell TR, Mason R, Chakrabarti I. Functional benefit of Dupuytren's surgery. J Hand Surgery Br. 2002;27:378–81. doi: 10.1054/jhsb.2002.0776. [DOI] [PubMed] [Google Scholar]
- 27.Messina A, Messina J. The continuous elongation treatment by the TEC device for severe Dupuytren's contracture of the fingers. Plast Reconstr Surg. 1993;92:84–90. doi: 10.1097/00006534-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Ketchum LD, Donahue TK. The injection of nodules of Dupuytren's disease with triamcinolone acetonide. J Hand Surg Am. 2000;25:1157–62. doi: 10.1053/jhsu.2000.18493. [DOI] [PubMed] [Google Scholar]
- 29.Adamietz B, Keilholz L, Grunert J, Sauer R. Radiotherapy of early stage Dupuytren disease. Long-term results after a median follow-up period of 10 years. Strahlenther Onkol. 2001;177:604–10. doi: 10.1007/pl00002371. [DOI] [PubMed] [Google Scholar]
- 30.Badalamente MA, Hurst LC, Hentz VR. Collagen as a clinical target: nonoperative treatment of Dupuytren's disease. J Hand Surg Am. 2002;27:788–98. doi: 10.1053/jhsu.2002.35299. [DOI] [PubMed] [Google Scholar]
- 31.Bulstrode NW, Bisson M, Jemec B, Pratt AL, McGrouther DA, Grobbelaar AO. A prospective randomised clinical trial of the intra-operative use of 5-fluorouracil on the outcome of Dupuytren's disease. J Hand Surg Br. 2004;29:18–21. doi: 10.1016/j.jhsb.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Bayat A, Watson JS, Stanley JK, Ferguson MWJ, Ollier WE. Genetic susceptibility to Dupuytren disease: association of Zf9 transcription factor gene. Plast Reconstr Surg. 2003;111:2133–9. doi: 10.1097/01.PRS.0000060531.98180.32. [DOI] [PubMed] [Google Scholar]
- 33.Bayat A, Walter J, Lambe H, Watson JS, Stanley JK, Marino M, et al. Identification of a novel mitochondrial mutation in Dupuytren's disease using multiplex DHPLC. Plast Reconstr Surg. 2005;115:134–41. [PubMed] [Google Scholar]
- 34.McGrouther DA. Dupuytren's disease. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green's Operative Hand Surgery. 5th edn. Vol I. New York: Churchill Livingstone; 2005. [Google Scholar]
Reading recommendations
- McFarlane R, McGrouther DA, Flint M, editors. Dupuytren's Disease, Biology & Treatment. Edinburgh: Churchill Livingstone; 1990. [Google Scholar]
- Tubiana R, Leclercq C, Hurst LC, Badalamente MA, Mackin EJ. Dupuytren's Disease. Martin Dunitz; 2000. [Google Scholar]
- McGrouther DA. Green DP, Hotchkiss RN, Pederson WC. Green's Operative Hand Surgery. 5th edn. Vol I. New York: Churchill Livingstone; 2004. Dupuytren's contracture. [Google Scholar]


