Abstract
Mesenteric haematomas are a rare surgical presentation and are associated with trauma, pancreatitis or anticoagulation treatment. We report two cases diagnosed as spontaneous mesenteric haematomas. In both cases, MRI was diagnostic of a mesenteric haematoma and both cases were managed conservatively with interval imaging until complete resolution of the haematomas. We discuss the clinical features, diagnostic modalities and management options of mesenteric haematomas in the light of the literature. We emphasise the importance of radiological imaging to delineate the underlying pathology and appropriate management strategies. In the absence of obvious underlying pathology, spontaneous mesenteric haematomas can be managed conservatively.
Keywords: Mesentery, Haematoma, Pseudo-aneurysm
Mesenteric haematoma is a rare clinical condition often associated with early or delayed blunt abdominal trauma,1,2 acute pancreatitis,3 visceral artery aneurysm rupture4 and complication of anticoagulation treatment.5 We describe two case reports diagnosed as spontaneous mesenteric haematomas and discuss the imaging modalities employed and treatment implications.
Case report 1
A 53-year-old Caucasian man with no history of significant alcohol consumption or biliary tract pathology was admitted to the acute surgical admission unit at the Bradford Royal Infirmary, UK, for sudden-onset, left upper quadrant pain, vomiting and a history of influenza-like illness. The patient was a fit marathon runner with no history of recent trauma. Clinical examination revealed a palpable epigastric mass and laboratory findings except for haemoglobin of 12.9 g/dl (normal 14–17 g/dl) were all within normal range. An abdominal computer tomography (CT) scan revealed a well-defined cystic lesion measuring 5.5 × 4.5 × 3.3 cm lying inferior to the uncinate process of the pancreas and in close relation to the third part of the duodenum. This case was referred to the pancreatobiliary unit at our institution as a possible pseudo-aneurysm or pseudocyst complicating acute pancreatitis. A subsequent contrast magnetic resonance imaging (MRI) scan of the pancreas demonstrated a 4 × 2.1 × 2.6 cm mass, in keeping with a mesenteric haematoma separate from the pancreas and duodenum. No vascular malformation was noted and the source was unclear. Follow-up ultrasound scan of the abdomen at 4 months showed the haematoma had completely resolved. As the patient remained asymptomatic at 7-month follow-up, he was discharged.
Case report 2
A 62-year-old Caucasian man presented with a history of non-specific abdominal pain and vomiting. Physical examination was unremarkable. Laboratory investigations were all within normal range. CT examination of the abdomen revealed a mixed attenuation mass containing features of haemorrhage in the small bowel mesentery surrounding the superior mesenteric pedicle and measuring up to 10 cm in size. This was causing compression of the third part of the duodenum and a diagnosis of a pseudo-aneurysm was considered. No inflammatory abdominal aortic aneurym or pancreatitis was noted. A MRI scan performed at 2 weeks revealed a haematoma in the small bowel mesentery measuring 8.6 × 5.9 cm extending up to the uncinate process and lying posterior to the superior mesenteric vessels separate to the duodenum and pancreas (Fig. 1). A repeat CT scan at 3 weeks confirmed this and reported inflammatory changes adjacent to the uncinate process of the pancreas which were secondary to the haematoma. The patient was symptom-free during the follow-up period and a CT examination at 5 months demonstrated complete resolution of the mesenteric haematoma.
Figure 1.
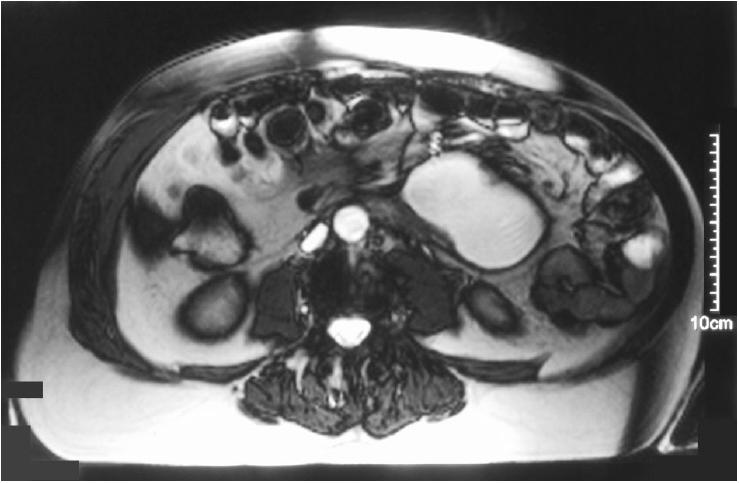
MRI scan of the abdomen of case 2 performed at 2 weeks after presentation. The scan revealed a haematoma in the small bowel mesentery measuring 8.6 × 5.9 cm extending up to the uncinate process of the pancreas, separate from the duodenum and pancreas.
Discussion
Due to its varied and non-specific clinical presentation and the rarity of the condition, mesenteric haematomas are difficult to diagnose clinically and radiologically. The clinical features are predominantly determined by the cause, size and site of the haematoma. If bleeding into the mesentery is a dominant feature, an abdominal mass may be palpated on clinical examination. Mesenteric haematomas can also exhibit extrinsic compression of the gastrointestinal tract leading to partial or complete obstruction.6 Both our patients presented with abdominal pain and vomiting and the CT examination revealed a compressed duodenum secondary to a mesenteric haematoma in one patient.
In the absence of an obvious underlying condition, i.e. pancreatitis, peptic ulcer disease or trauma, an urgent CT examination of the abdomen is an ideal first-line investigation as it enables clinicians to exclude differential diagnoses such as abdominal aortic aneurysm, pseudo-aneurysms and tumours, including leiomyoma, leiomyosarcoma, mesenteric tumours and lymphoma. CT scans have been diagnostic for mesenteric haematomas in previous reports.1,3,4 Contradicting other reports, CT findings in both our patients suggested a pseudo-aneurysm, although subsequent MRI of the abdomen confirmed the diagnosis of mesenteric haematoma. Hence, in cases where CT scan findings are indeterminate, a contrast MRI of the abdomen should be performed to confirm the diagnosis of mesenteric haematomas as it is a sensitive investigation and also assists in determining vascular or biliary tract involvement. An ultrasound scan of the abdomen was a first-line investigation in some reports;2,7,8 however, this test lack sensitivity although its additional feature of colour Doppler studies enables the vascularity status of such lesions to be determined.8 In cases where an arterial aneurysm or pseudo-aneurysm is suspected, an angiography is indicated,4 both to clinch the diagnosis and allow for definitive therapy by transcatheter embolisation of the causative artery.3
The management of mesenteric haematoma is determined by the underlying pathology. In both our cases where a diagnosis of spontaneous haematoma was made, a conservative approach was employed. Surgical intervention in the form of laparotomy and haematoma evacuation for a mesenteric haematoma has been described.9 In that case, the mesenteric haematoma was diagnosis on CT scan but no definite findings were seen on angiography and gallium scintigraphy; hence, a laparotomy was performed.9 In cases where an underlying pathology cannot be elucidated on radiological modalities, conservative management with interval imaging is an appropriate option as described in both our cases.
Conclusions
Based on the literature, mesenteric haematoma can be spontaneous or associated with trauma. The diagnosis can be achieved radiologically by MRI as demonstrated in our cases. Imaging is crucial to delineate the underlying pathology, risk of complications and appropriate management strategies. In the absence of obvious underlying pathology, these mesenteric haematomas can be managed conservatively.
References
- 1.Yoshiki A, Shunichi M, Takuro I, Naonobu K, Hideaki N. A case of traumatic mesenteric bleeding controlled by only transcatheter arterial embolization. Cardiovasc Intervent Radiol. 2005;28:256–8. doi: 10.1007/s00270-003-9108-y. [DOI] [PubMed] [Google Scholar]
- 2.Taskin A. Chronic duodenal stenosis and periduodenal fibrosis secondary to a intramesenteric cyst arising from an old traumatic hematoma: a case report. Ulus Travma Derg. 2005;11:162–4. [PubMed] [Google Scholar]
- 3.Takayuki T, Sakae N, Kennoki O, Morisuke N, Toshihiko S, Takahiro O, et al. Case of a bleeding pseudoaneurysm of the middle colic artery complicating acute pancreatitis. Hepatogastroenterology. 2002;49:1141–3. [PubMed] [Google Scholar]
- 4.Skudder PA, Jr, Craver WL. Mesenteric hematoma suggests rupture of visceral artery aneurysm. Arch Surg. 1984;119:863. doi: 10.1001/archsurg.1984.01390190099023. [DOI] [PubMed] [Google Scholar]
- 5.Becker A, Berlin Y, Sayfan J. Spontaneous rupture of mesenteric hematoma with hemorrhagic shock as a complication of oral anticoagulant treatment. Isr Med Assoc J. 1999;1:196–7. [PubMed] [Google Scholar]
- 6.Weinstock LB, Wu JS, Malden ES, Garcia KM, Rubin BG, Brunt LM. Small bowel obstruction resulting from mesenteric hematoma caused by spontaneous rupture of a jejunal branch artery. Gastrointest Endosc. 1999;49:537–40. doi: 10.1016/s0016-5107(99)70061-1. [DOI] [PubMed] [Google Scholar]
- 7.Raghavendra BN, Grieco AJ, Balthazar EJ, Megibow AJ, Subramanyam BR. Diagnostic utility of sonography and computed tomography in spontaneous mesenteric hematoma. Am J Gastroenterol. 1982;77:570–3. [PubMed] [Google Scholar]
- 8.Chao HC, Kong MS. Sonographic diagnosis of mesenteric hematoma. J Clin Ultrasound. 1999;27:284–6. doi: 10.1002/(sici)1097-0096(199906)27:5<284::aid-jcu9>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 9.Aoki T, Nishizono M, Niina H, Inatsu H, Komidori H, Itano T, et al. A case of spontaneous mesenteric hematoma and a review of 17 cases in Japan. Gastroenterol Jpn. 1990;25:768–73. doi: 10.1007/BF02779194. [DOI] [PubMed] [Google Scholar]


