Abstract
INTRODUCTION
Accurate written communication is essential in orthopaedic surgery. Incomplete and poorly structured letters can lead to poor knowledge of a patient's diagnosis.
MATERIALS AND METHODS
Structured and traditional letter formats were compared for speed of reading and preference by general practitioners (GPs), consultants, registrars and out-patient nursing staff. In addition, out-patient clinic letters and notes were analysed and compared for speed of reading and ease of assimilating information and content.
RESULTS
There was overwhelming preference for the structured letter format. This style of letter could be read significantly more quickly with information better assimilated and relevant data included more frequently. However, only 26% of letters generated contained a complete set of information sought by GPs and hospital staff.
CONCLUSIONS
Structured letters are better in orthopaedics because it is easier to access the contents. The structured format disciplines medical staff to address essential information. Even with a structured format the majority of letters omitted essential information. Training in letter writing is necessary. A structured letter format next to dictating machines might improve the quality of letters generated.
Keywords: Communication, Orthopaedic surgery, Education
Communication by letter is essential in high-volume practice such as orthopaedics. We were interested in establishing the style of consultation note that communicates information most rapidly and completely.
We aimed to ascertain which clinic letter format allowed information to be most rapidly assimilated by general practitioners (GPs) and consultants, registrars and nurses in out-patient clinics.
Materials and Methods
Two separate letters were created describing the same clinical scenario. Sample Letter A (Appendix 1) used a traditional letter format with paragraphs whilst sample Letter B (Appendix 2) was structured and used subheadings. The two sample letters were given to GPs, orthopaedic registrars and fracture clinic nurses. All participants were asked to record the time taken to read each letter, their preferred format and which letter they felt contained the most information. They were also asked to prioritise which items of information they would most like to see in the letter.
The pack was given to a random selection of 73 GPs, 15 orthopaedic registrars and 11 out-patient clinic nurses.
In addition, in two follow-up fracture clinics, the notes of 115 patients were analysed by registrars and consultants. The style of letter and the time taken to find the relevant information in the notes using the most recent letter before seeing the patient was recorded. Staff also identified if the relevant information including date of injury, side of injury, mechanism, initial treatment, subsequent treatment and reason for attendance was present in the last clinic letter.
Results
Time to read letter
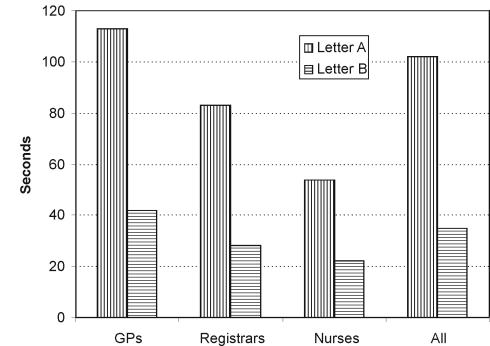
The mean time for GPs to read letter A (Fig. 1) was 113 s (range, 23–420 s) and letter B, 42 s (range, 5–180 s), registrars 84 s (range, 20–300 s) and 28 s (range, 7–60 s) and nurses 54 s (range, 24–65 s) and 22 s (range, 5–40 s). The difference in reading times for both registrars and nurses was significant (P < 0.001). There was no significant difference in reading times for the GPs. The mean time for the three groups to read letter A was 102 s (range, 20–420 s) and letter B 35 s (range, 5–180 s), the difference in reading times between the three groups combined was not statistically significant.
Figure 1.
Mean times to read sample letters.
Preferred format
Of GPs, 92% and all the registrars and nurses preferred the structured letter.
Perceived amount of information
Overall, 47% of GPs, 67% of registrars and 91% of nurses thought the structured letter contained more information (Table 1), 13% of GPs and 13% of registrars felt the content was the same and 40% of GPs, 20% of registrars and 9% of nurses thought the traditional style letter contained more information.
Table 1.
Impression of which sample letter contained the most information
| Impression of which letter contained the most information | |||
|---|---|---|---|
| Group | A | B | Equal |
| GPs | 21/53 | 25/53 | 7/53 |
| Registrars | 3/15 | 10/15 | 2/15 |
| Nurses | 1/11 | 10/1 | 0/11 |
Preferred items of information
In descending order of importance of items that should be included in the letter, GPs prioritised diagnosis, treatment, plan of management, date of injury, present state/examination findings, radiographic findings and history whilst orthopaedic registrars prioritised diagnosis, date of injury, treatment and examination findings/present state and plan of management (Table 2).
Table 2.
Priority of information required in clinic letters by different medical staff
| Item of information | GPs (n = 53) | Registrars (n = 15) | Nurses (n = 11) |
|---|---|---|---|
| Diagnosis | 53 | 11 | 4 |
| Date of injury | 19 | 13 | |
| History/mechanism of injury | 4 | 4 | 3 |
| Treatment | 47 | 11 | 2 |
| Present state/examination | 17 | 11 | |
| Management plan | 41 | 10 | 9 |
| Radiographic findings | 7 | 2 | |
| Medical history | 2 | ||
| Social history | 2 | ||
| Patient details | 2 | 1 | |
| Complications | 1 | ||
| Other investigations | 1 | 4 | |
| Consultation (e.g to see consultant) | 2 | ||
| Side/reason for X-ray | 3 | ||
| Date of last appointment | 1 |
Fracture clinic nurses prioritised plan of management which included the need for X-ray on arrival, plaster room intervention or wound care procedures, grade of surgeon to see patient, diagnosis, investigations awaited, e.g blood results, CT/MRI scan results, history, treatment, reason for X-ray, side of X-ray, patient details and date of last appointment.
Desired information
GPs preferred more detailed letters in complex cases and wanted to know of time needed off work, details of medical certification and feed-back on their referrals.
Registrars preferred the structured letter and requested that a complex history or operative details should be included where appropriate.
The nurses preferred letters in a consistent style and suggested that the secretaries have a set template for typing letters. The structured letter facilitated access to the plan of management.
Assimilation of information in fracture clinics
Of 115 sets of notes in fracture clinics, 19 (17%) had a paragraphed (type A letter), 90 (78%) had a structured (type B letter) and 6 (5%) had no letter at all. The mean time to find the information required in the type A letters was 27 s (range, 7–100 s) and in the type B letter was 20 s (range, 5–60 s). The difference was not statistically significant.
Content of clinic letters
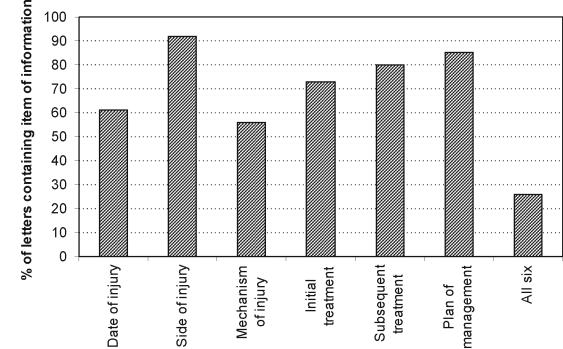
Staff identified (Figs 2 and 3): side of injury (92%), plan of management (85%), subsequent treatment (80%), initial treatment (73%), date of injury (61%), mechanism of injury (56%) and all six items (26%).
Figure 2.
Information present in clinic letters.
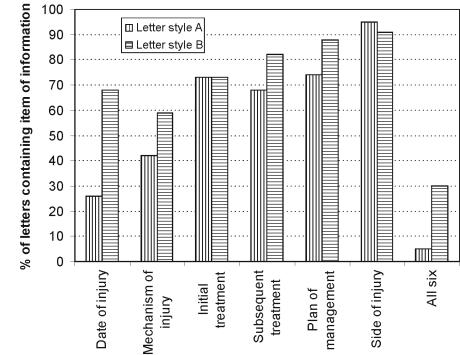
Figure 3.
Information content of the different styles of letter.
Structured letters contained more information (mean, 4.54 ± 1.47) than the traditional style letters (mean, 3.83 ± 1.09; P = 0.05).
Discussion and Conclusions
Letters are the main method of contact and communication between GPs and hospital staff. They should be clear, concise and contain sufficient relevant information to satisfy all parties involved in the patient's care1 and to ensure smooth management of their problem. Past correspondence is the main source of information used by hospital doctors.2 Letters are often the sole communication between specialists and GPs and act as a means of education.3
Structured referral letters impart more information without increasing the length of the letter1 as do structured replies. GPs prefer structured, headed letters4 with problem lists as they are generally shorter and the contents more easily transferable to computerised patient records.5,6 Few hospital doctors write such letters and, therefore, communication with GPs is less effective than it could be.2,5 In this study, the majority of GPs preferred the structured reply letter although this format is not standard throughout our department.
Useful information is often missed in both referral and reply letters. The content of such letters is often poor and the level of mutual education is low, with most questions posed by GPs going unanswered.7 Our letter content was poor with only 26% of letters having a complete data set despite a well-staffed fracture clinic with 1–2 consultants present. Time was wasted searching for missing data in previous records. There was little or no consideration of important diagnostic or therapeutic considerations, information given to the patient or relatives8 or sickness certification. This problem is not confined to our practice; elsewhere, it has been reported that only 50–60% of the time are details of the patient's problem, diagnosis and management clearly communicated.9
Written communication is not easy and training in letter writing is necessary. An opinion section in the structured letter would allow for detailed response to questions posed and provide an opportunity for educating both GPs and hospital staff.
Appendix 1 Sample Letter A
Dear Doctor
Re: Mr Patient, d.o.b.
Address
Thank you for asking me to see this 30-year-old gentleman who presents with a history of an acute injury to his right knee two months ago.
Whilst playing football, he was tackled by another player, resulting in a valgus strain to the knee. He heard a loud snap and developed immediate swelling. He was unable to continue playing and had to be carried off the field. He attended the Accident and Emergency Department at Southmead Hospital where X-rays showed an acute haemarthrosis but no bony injury. The haemarthrosis was aspirated and he was placed in a backslab, a review appointment was made for the trauma clinic two weeks later.
On initial review in the fracture clinic, he still had a tense haemarthrosis and was in a back slab and was walking with crutches partial weight bearing. He had full extension of the knee and could flex to 40°. Collateral ligaments felt stable but the cruciate could not be examined. In his past history, he had sustained an osteochondral fracture of the patella in 1989 which was fixed with screws, with satisfactory results.
An emergency arthroscopy was performed showing a large haemarthrosis. After thoroughly washing out the knee, it was evident that he had sustained a rupture of his anterior cruciate ligament with an associated medial meniscal tear. The knee was thoroughly irrigated and all the haematoma removed. The unstable medial meniscus was left with a view to repair at definitive surgery. He was then mobilised with physiotherapy supervision until review today.
On review today, he has a reduced quadriceps bulk on the right and a small effusion with a positive bulge test. He was tender over the medial joint line. He had full extension but lacked hyperextension. The collateral ligaments were stable in extension and 20° of flexion. The Lachman test was Grade II positive and the anterior drawer test revealed 2 cm of travel, consistent with the diagnosis of anterior cruciate deficiency. McMurray's testing was positive for pain and clicking.
After discussion today with Mr Patient, we have organised to bring him into Southmead Hospital on 25 December for Anterior Cruciate Ligament Reconstruction and Medial Meniscal Repair. We will keep you informed of his progress.
Yours sincerely
Orthopaedic Surgeon FRCS
Consultant – Southmead Hospital
Appendix 2 Sample Letter B
Dear Doctor
Knee PATIENT dob 25/12/68
Address
| Diagnosis: | Right ACL Deficient Knee and Medial Meniscal Tear |
| Date of Injury: | 15/9/99 |
| History: | Tackled whilst playing football. He heard a loud snap, had immediate swelling and was unable to walk afterwards. A haemarthrosis was aspirated in A&E. |
| Treatment: | EUA and Arthroscopic Washout 16/9/99. |
| Present State: | Continued painful stiff knee with sensation of instability. |
| On Examination: | Reduced quadriceps bulk on the right and a small effusion. Tender medial joint line. ROM: 0–0–100°. Stable collaterals. Grade II positive Lachman, no end point. Grade III pivot shift. McMurray's positive for pain and clicking. |
| Radiographs: | No bony injury. |
| Plan: | For Hamstring ACL Reconstruction and Meniscal Repair 25/12/99. |
Yours sincerely
Orthopaedic Surgeon, FRCS
Consultant – Southmead Hospital
References
- 1.Jenkins S, Arroll B, Hawken S, Nicholson R, et al. Referral letters: are form letters better? Br J Gen Pract. 1997;47:107. [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd B, Barnett P, et al. Use of problem lists in letters between hospital doctors and general practitioners. BMJ. 1993;306:247. doi: 10.1136/bmj.306.6872.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newton J, Eccles M, Hutchinson A, et al. Communication between general practitioners and consultants: what should their letters contain? BMJ. 1992;304:821–4. doi: 10.1136/bmj.304.6830.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salathia K, Mcllwaine W, et al. General practitioners and hospital letters. Ulster Med J. 1995;64:46–50. [PMC free article] [PubMed] [Google Scholar]
- 5.Rawal J, Barnett P, Lloyd B, et al. Use of structured letters to improve communication between hospital doctors and general practitioners. BMJ. 1993;307:1044. doi: 10.1136/bmj.307.6911.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cross X, Gaunt M, et al. Dictating an outpatient clinic letter. BMJ. 2002;(Career Suppl):92. [Google Scholar]
- 7.Jacobs L, Pringle M, et al. Referral letters and replies from orthopaedic departments: opportunities missed. BMJ. 1990;301:470–3. doi: 10.1136/bmj.301.6750.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grol R, Rooijackers-Lemmers N, Van Kaathoven L, Wollersheim H, Mokkink H, et al. Communication at the interface: do better referral letters produce better consultant replies? Br J Gen Pract. 2003;53:217–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Westerman R, Hull F, Bezemer P, Gort G, et al. A study of communication between general practitioners and specialists. Br J Gen Pract. 1990;40:445–9. [PMC free article] [PubMed] [Google Scholar]