Abstract
INTRODUCTION
Information regarding early morbidity, pain and patient satisfaction following band ligation of haemorrhoids is limited. This is the first report to address these issues specifically.
PATIENTS AND METHODS
A total of 183 patients underwent the procedure over a 10-month period. Prospective data were collected using a detailed structured questionnaire regarding symptoms, analgesia requirements and patient satisfaction in the following week.
RESULTS
The response rate was 74% (135/183). Pain scores were highest 4 h following the procedure. At 1 week, 75% of patients were pain-free, with 9 (7%) still experiencing moderate-to-severe pain. About 65% required oral analgesia, most frequently on the day of procedure. Rectal bleeding occurred in 86 patients (65%) on the day after banding, persisting in 32 (24%) at 1 week. Vaso-vagal symptoms occurred in 41 patients (30%) and were commonest at the time of banding. Eighty patients (59%) were satisfied with their experience and would undergo the procedure again. Patients requiring oral analgesia and those experiencing bleeding or vaso-vagal symptoms were significantly less likely to be satisfied with the procedure. Only 57% of the patients surveyed would recommend the procedure to a friend.
CONCLUSIONS
Data from this large cohort of patients suggest that discomfort and bleeding may persist for a week or more following banding of haemorrhoids. Patients should be aware of this in order to make an informed decision as to whether to undergo the procedure, and surgeons should investigate ways of reducing it. Patient satisfaction may be further improved by more accurate counselling regarding the incidence of specific complications.
Keywords: Haemorrhoids, Symptoms, Patient care, Band ligation
Rubber band ligation (RBL) is the most commonly performed out-patient treatment for symptomatic haemorrhoids and provides a cure for the majority of patients.1 In about 30% of patients for whom initial RBL is unsuccessful, the treatment may be repeated, resulting in a long-term success rate of approximately 80%.2 The base of the haemorrhoid is visualised by anoscopy and controlled by either a suction device or forceps. A band is then applied to the base of the haemorrhoid, leading to necrosis and sloughing of the haemorrhoidal tissue. The commonest complications of RBL are pain and rectal bleeding; however, the reported incidence of these varies considerably.2–4 Vaso-vagal symptoms, urinary dysfunction, haemorrhoid thrombosis, mucosal ulceration and septic complications may also occur. We conducted a prospective audit of patient outcomes and satisfaction in the first week following RBL of symptomatic haemorrhoids. This is the first report to address these issues specifically, and will allow more accurate counselling of patients undergoing the procedure.
Patients and Methods
Over a 10-month study period, all patients undergoing RBL for symptomatic haemorrhoids were invited to participate in the study. The total number of patients eligible was 183. Treatment was performed on an out-patient basis at our institution and at the local community hospital. All patients were referred to colorectal surgical clinics, and the procedures were performed by all grades of surgeon (SHO, SpR, staff grade and consultant) and nurse practitioner. Prior to the procedure, informed consent was obtained through verbal counselling together with the use of preprinted information sheets. Information sheets regarding the procedure constituted dietary advice regarding avoidance of constipation, together with advice to seek medical assistance in cases of fever, excessive rectal blood loss, difficulty in passing urine or swelling of the anus. No specific written advice regarding driving vehicles or returning to work was given. Patients were also given a detailed structured questionnaire on which to record symptoms, analgesia requirements and their overall satisfaction with the procedure. They were asked to return this after 1 week in a prepaid envelope. Verbal informed consent was taken for the study, and no patients declined to participate. Responses were anonymous; therefore, no attempt was made to contact non-responders. The study was registered with the hospital audit department. Statistical analysis was performed using SPSS for Windows v 11.0, and P-values < 0.05 considered significant.
Results
Of 183 patients issued with questionnaires, 135 were returned (response rate 74%). Of the responders, 51% were male, and the median age was 58 years (range, 22–85 years). For 102 patients (76%) this was their first experience of RBL. In total, 90% of patients read the information sheet regarding the procedure, and of these only 10% felt that it could be improved. The median number of bands applied per patient was 2 (range, 1–4).
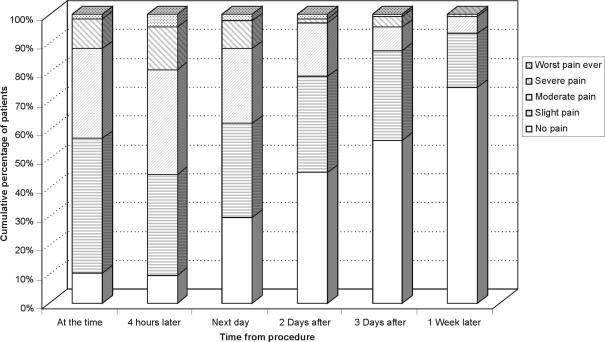
Pain
The commonest symptom experienced following RBL was pain, which occurred in almost 90% of patients. Pain at different time-points over the course of the week was assessed on a 5-point scale from (1) no pain at all, to (5) the worst pain ever experienced (Fig. 1). The median pain score was found to be significantly worse at 4 h after banding compared with the pain experienced at the time of the procedure (paired samples t-test −2.813; P = 0.006), declining steadily thereafter. At 1 week, 75% of patients reported themselves as being pain-free; however, 9 patients (7%) were still experiencing moderate-to-severe pain.
Figure 1.
Incidence and severity of pain following RBL.
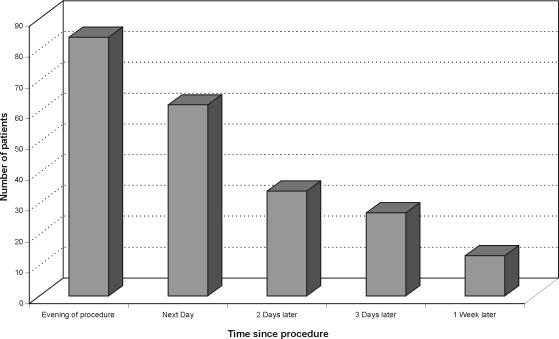
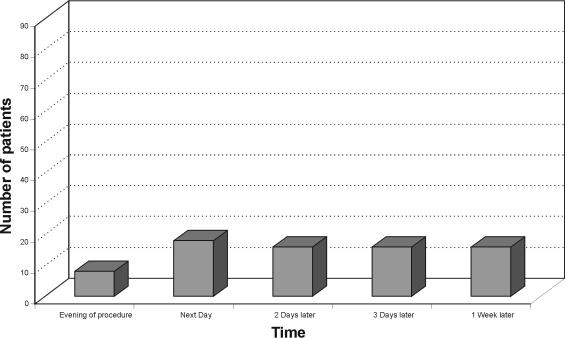
Use of oral analgesia and topical anaesthetic agents
A total of 88 patients (65%) required oral analgesia during the week following RBL, most frequently on the day of the procedure (Fig. 2). Of the total, 20% required oral analgesia for 3 or more days, with 10% still requiring analgesia at 1 week. We did not enquire specifically about use of topical agents prior to the banding procedure. These were used by a total of 38 patients (28%) at some point during the following week (Fig. 3).
Figure 2.
Patient use of oral analgesia following RBL.
Figure 3.
Patient use of topical anaesthetic agents following RBL.
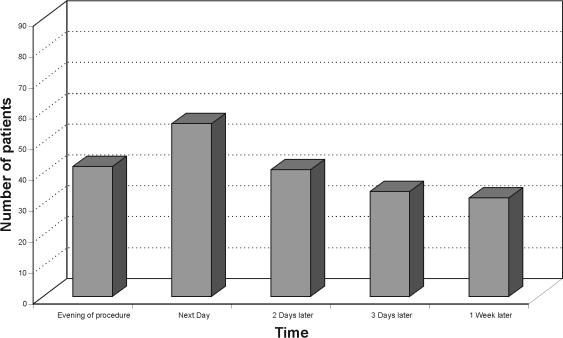
Rectal bleeding
In total, 86 patients (65%) experienced rectal bleeding after RBL, most frequently on the day after the procedure (Fig. 4). Thirty-two patients (24%) were still experiencing bleeding at 1 week.
Figure 4.
Incidence of bleeding following RBL.
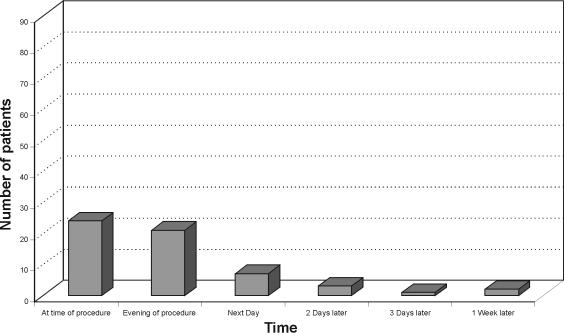
Vaso-vagal symptoms
Vaso-vagal symptoms (dizziness or fainting) were reported by 41 patients (30%). These were commonest at the time of the procedure and in the evening of that day (Fig. 5), occurring infrequently over the remaining week.
Figure 5.
Incidence of vaso-vagal symptoms following RBL.
Major complications
No major complications were noted over the duration of the study. No patient who suffered post-procedure bleeding required blood transfusion. We did not specifically enquire about urinary symptoms post-RBL; however, no patient required hospital treatment for these. A single patient required parenteral (intramuscular) analgesia from their general practitioner due to severe pain on the second day post RBL.
Satisfaction with the procedure
In total, 80 patients (59%) were satisfied with their procedure at 1 week and would undergo further RBL in the future if their symptoms persisted or recurred. However, 25 patients (15%) were dissatisfied and would not undergo RBL again. The remaining 30 (22%) were undecided. Only 76 patients (56%) reported that they would recommend the procedure to a friend.
On univariate chi-square analysis, patients requiring oral analgesia (χ2 = 16.954; P = 0.049), topical anaesthetic agents (χ2 = 20.796; P = 0.002), experiencing bleeding (χ2 = 17.862; P = 0.007), and those experiencing vaso-vagal symptoms (χ2 = 20.864; P = 0.002), were significantly less likely to report satisfaction with their treatment. There was no association between having read the printed information and satisfaction with RBL (χ2 = 1.775; P = 0.620); however, a trend was noted towards dissatisfaction with the procedure in patients who thought that the printed information could be improved (χ2 = 15.540; P = 0.077). No association was seen between satisfaction and the number of bands applied (single versus multiple; χ2 = 5.601; P = 0.133).
Discussion
Previous reports concerning RBL of haemorrhoids have suggested that the procedure is associated with less pain and fewer complications than surgical haemorrhoidectomy.5 Findings from this study suggest that up to 90% of patients experience some pain following RBL. Discomfort during the first week was maximal at 4 h post-procedure, when over 55% of patients complained of moderate pain or worse. This proportion diminished to 38%, 21%, 13% and 7% on days 1, 2, 3 and 7 following RBL, respectively. It is frequently suggested that pain after RBL may be more severe if the band is applied too low in the anal canal, and that this may be an operator-dependent factor. We were not able to analyse pain scores by the experience of the operator. However, in our study, procedures were performed by all grades of surgeon and by nurse practitioners, and this is likely to reflect accurately the situation in most hospitals in the UK.
Oral analgesia was used by 65% of patients following RBL, and only one patient was noted to require supplementary parenteral analgesia. Despite this, our results suggest that patients who require oral analgesia and/or topical anaesthetic agents after RBL report less satisfaction with the procedure. Strategies to decrease post-procedure pain may thus improve patient satisfaction, although no reduction in pain was seen in a randomised trial combining RBL with synchronous local anaesthetic injection.6
Rates of significant rectal bleeding (requiring hospital admission or transfusion) following RBL are around 1–2%.2 No patient in our study experienced these complications. The reported incidence of any bleeding was highest on the day after the procedure (41% of patients); whilst the incidence was seen to decline over the first week, this persisted in 24% of cases. Patients experiencing bleeding in the week after RBL reported less satisfaction with the procedure. This is likely to reflect a (perceived or actual) treatment failure in patients for whom bleeding was the predominant symptom prior to RBL. Application of multiple rather than single bands may prove more effective in these patients;7 however, our data did not allow for this subgroup analysis.
We found the incidence of vaso-vagal symptoms following RBL to be higher than in previous studies.3 These were reported by 18% of patients at the time of the procedure and by 16% later on the same day. Experience of vaso-vagal symptoms was strongly associated with lower patient satisfaction. A warning of the possibility of these symptoms occurring was not part of the written patient information sheet, and our findings suggest that they are a sufficiently common occurrence to warrant inclusion in the future.
Conclusions
Haemorrhoidal banding is painful for the majority of patients and may persist for a week or more following the procedure. Patients should be aware of this in order to make an informed decision as to whether to undergo the procedure, and surgeons should investigate ways of reducing it. We have also found that patients who require oral analgesia, topical anaesthetic agents, who experience rectal bleeding or who experience vaso-vagal symptoms in the week after haemorrhoidal banding tend to report lower satisfaction with the procedure. This situation may be improved by providing more accurate patient counselling.
References
- 1.Nisar PJ, Scholefield JH. Managing haemorrhoids. BMJ. 2003;327:847–51. doi: 10.1136/bmj.327.7419.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum. 2004;47:1364–70. doi: 10.1007/s10350-004-0591-2. [DOI] [PubMed] [Google Scholar]
- 3.Lee HH, Spencer RJ, Beart RW. Multiple hemorrhiodal bandings in a single session. Dis Colon Rectum. 1994;37:37–41. doi: 10.1007/BF02047212. [DOI] [PubMed] [Google Scholar]
- 4.Bat L, Meltzer E, Koler M, Dreznick Z, Shemesh E. Complications of rubber band ligation of symptomatic internal hemorrhoids. Dis Colon Rectum. 1993;36:287–90. doi: 10.1007/BF02053512. [DOI] [PubMed] [Google Scholar]
- 5.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg. 1997;40:14–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Law WL, Chu KW. Triple rubber band ligation for hemorrhoids: prospective, randomised trial of use of local anaesthetic injection. Dis Colon Rectum. 1999;42:363–6. doi: 10.1007/BF02236354. [DOI] [PubMed] [Google Scholar]
- 7.Chaleoykitti B. Comparative study between multiple and single rubber band ligation in one session for bleeding internal hemorrhoids: a prospective study. J Med Assoc Thai. 2002;85:345–50. [PubMed] [Google Scholar]